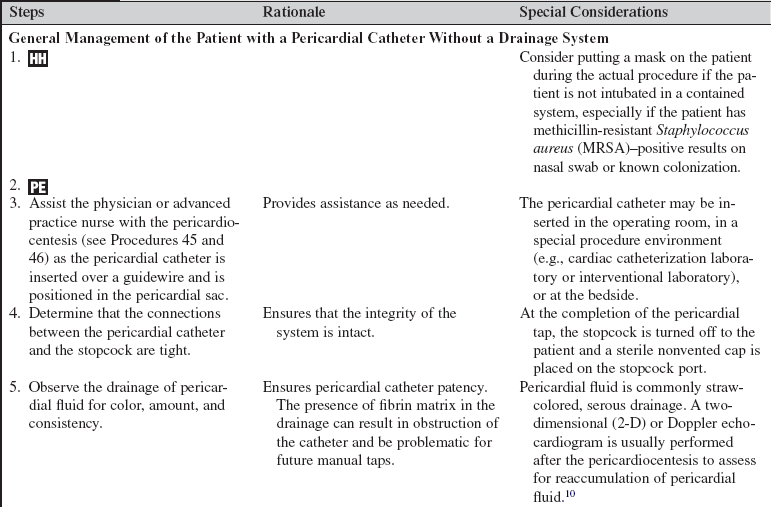
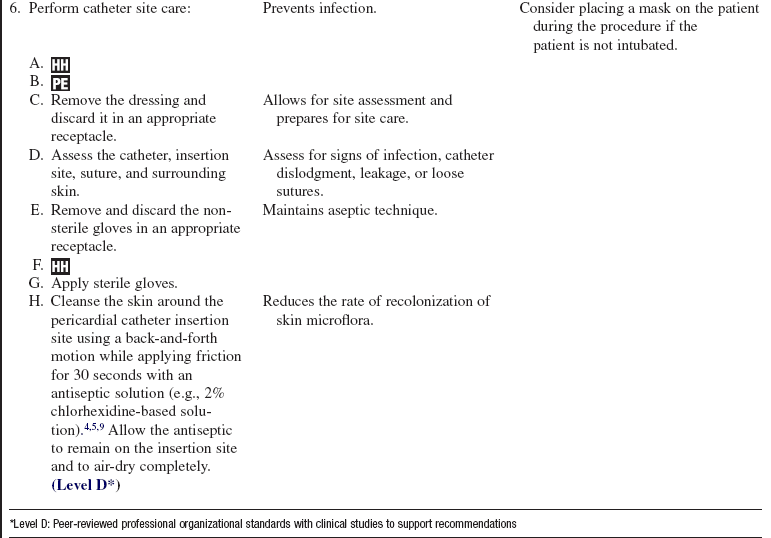
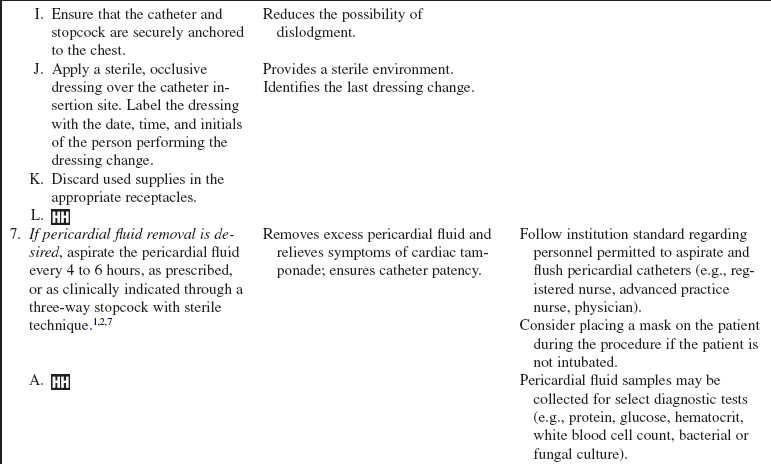
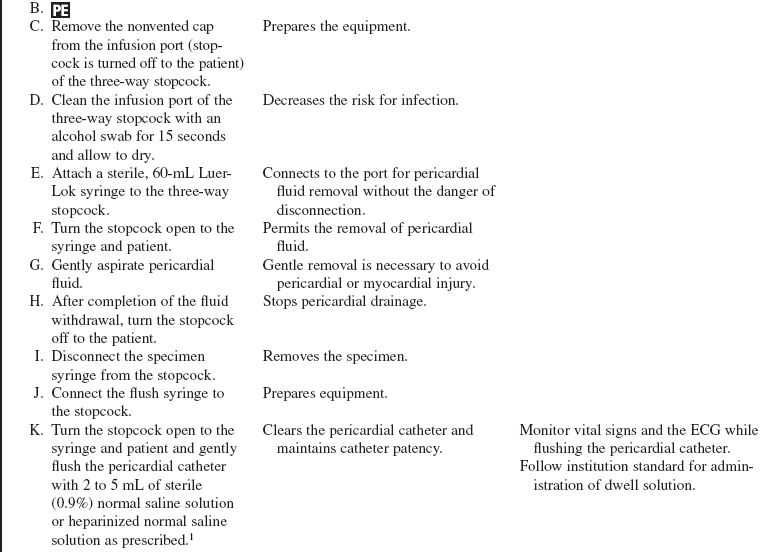
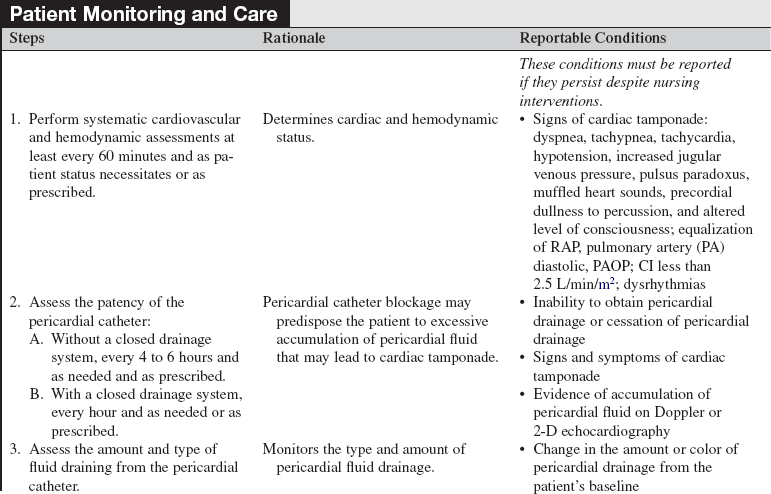
Pericardial Catheter Management
PREREQUISITE NURSING KNOWLEDGE
• Knowledge of the anatomy and physiology of the cardiovascular system, the principles of cardiac conduction, electrocardiogram (ECG) lead placement, basic dysrhythmia interpretation, and electrical safety is needed.
• Understanding of sterile technique is essential.
• Advanced cardiac life support knowledge and skills are needed.
• Pericardial effusion is an excessive collection of fluid in the pericardial space.
• The pericardial space normally contains 20 to 50 mL of fluid. Injury to the pericardium causes increased production of pericardial fluid, formation of fibrin, and cellular proliferation.2,13
• Pericardial fluid has electrolyte and protein profiles similar to plasma.13
• Causes of pericardial effusion are numerous and include infection, malignant neoplasms, autoimmune disorders, kidney failure, heart failure, acute myocardial infarction, trauma, radiation exposure, inflammatory disorders, and myxedema. Pericardial effusion may also be medication-induced, idiopathic, or a complication of invasive procedures.7,13,14
• Pericardiocentesis is an effective treatment for pericardial effusion (see Procedures 45 and 46). An indwelling pericardial catheter may be left in place after a pericardiocentesis to drain excess or continued excess production of pericardial fluid.
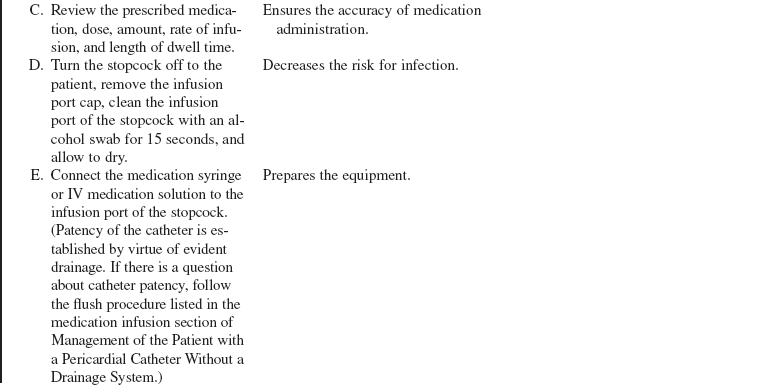
• The pericardial catheter may be connected to a closed drainage system (Fig. 78-1).
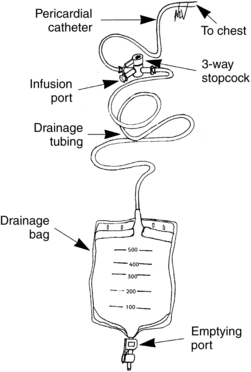
Figure 78-1 Indwelling pericardial catheter system. (From Hammel WJ: Care of patients with an indwelling pericardial catheter, Crit Care Nurse 18[5]:40-45, 1998.)
• The pericardial catheter may also be left in place to allow the instillation of certain medications (i.e., nonabsorbable corticosteroid or antineoplastic agents) depending on the patient’s underlying disease state.8,12
• The indwelling pericardial catheter is usually removed within 48 to 72 hours after placement to avoid the risk of infection or iatrogenic pericarditis.13,14 The indwelling pericardial catheter may be left in place for longer periods of time to promote the resolution of a pericardial effusion or cardiac tamponade.1 Pericardial catheters are immediately removed if there is an abrupt rise in the white blood cell (WBC) level.12
• Pericardial catheters are usually removed when the total amount of drainage has decreased to less than 25 to 30 mL over the preceding 24 hours.1,13,14
• Extended catheter drainage is associated with a reduction of the re-occurrence of cardiac tamponade compared with a single pericardiocentesis in patients with pericardial effusion related to malignancy.2,3
EQUIPMENT
• Sterile drapes: small drapes and a full-body drape
• Sterile and nonsterile gloves, gowns, masks, protective eyewear
• Sterile 0.9% normal saline solution for irrigation and sterile basin
• Anticoagulant flush available for dwell as prescribed (i.e., heparin)
• Sterile syringes: 3-, 5-, 30-, or 60-mL Luer-Lok
• Sterile 1000-mL vacuum bottle available for the initial procedure
• Antiseptic solution (e.g., 2% chlorhexidine-based preparation)
• Sterile transparent occlusive dressing
• Sterile three-way Luer-Lok stopcock with nonvented caps and replacement caps
PATIENT AND FAMILY EDUCATION
• Explain the need for the indwelling pericardial catheter and the reason for its insertion.  Rationale: The explanation decreases patient and family anxiety.
Rationale: The explanation decreases patient and family anxiety.
• Explain the need for frequent monitoring while the pericardial catheter remains in place.  Rationale: This information may decrease patient and family anxiety.
Rationale: This information may decrease patient and family anxiety.
• Explain that the catheter may be uncomfortable and may cause some discomfort at the insertion site, possibly with inspiration, and that pain medication will be available to administer at the time of the procedure and afterward to promote comfort.  Rationale: This explanation prepares and informs the patient of the pain management plan.
Rationale: This explanation prepares and informs the patient of the pain management plan.
• Describe the possible signs and symptoms of cardiac tamponade to the patient and family.  Rationale: Teaching the patient and family will help them to recognize a possible reoccurrence of pericardial effusion.
Rationale: Teaching the patient and family will help them to recognize a possible reoccurrence of pericardial effusion.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess the patient’s cardiovascular and hemodynamic status: heart rate and rhythm, blood pressure (BP), respiratory rate, heart sounds, peripheral pulses, and if available, pulmonary artery pressures (PAPs), pulmonary artery occlusion pressure (PAOP), right atrial pressure (RAP), cardiac output (CO), cardiac index (CI), and systemic vascular resistance (SVR).  Rationale: The patient’s baseline values are established for future comparison.
Rationale: The patient’s baseline values are established for future comparison.
• Assess the patient for dyspnea, tachypnea, tachycardia, muffled heart sounds, precordial dullness to percussion, or impaired consciousness; hypotension (systolic BP, <100 mm Hg or decreased from patient’s baseline); if available, cerebral perfusion pressure (CPP) of less than 70 mm Hg; increased jugular venous pressure/jugular distention; pulsus paradoxus (inspiratory fall in systolic BP sounds) greater than 12 to 15 mm Hg; equalization of RAP, PAOP, and pulmonary artery diastolic pressure; and decreased CO/CI.14  Rationale: Signs and symptoms of possible cardiac tamponade are assessed.
Rationale: Signs and symptoms of possible cardiac tamponade are assessed.
• Determine the patient’s allergy history (e.g., heparin, antiseptic solutions).  Rationale: This assessment decreases the risk for allergic reactions by avoiding known allergenic products.
Rationale: This assessment decreases the risk for allergic reactions by avoiding known allergenic products.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand preprocedural teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of previously taught information is evaluated and reinforced.
Rationale: Understanding of previously taught information is evaluated and reinforced.
• Ensure that in nonemergent situations, informed consent has been obtained.  Rationale: Informed consent protects the rights of the patient and makes a competent decision possible for the patient.
Rationale: Informed consent protects the rights of the patient and makes a competent decision possible for the patient.
• Perform a pre-procedure verification and time out, if non-emergent.  Rationale: Ensures patient safety.
Rationale: Ensures patient safety.
• Administer analgesia or anxiolytic as prescribed before pericardial catheter insertion.  Rationale: Comfort is promoted and anxiety is reduced.
Rationale: Comfort is promoted and anxiety is reduced.
References
1. Cornily, JC, et al, Cardiac tamponade in medical patients. a 10 year follow-up survey. Cardiology. 2008; 111(3):197–201.
2. Gandhi, S, et al. Has the clinical presentation and clinician’s index of suspicion of cardiac tamponade changed over the past decade. Echocardiography. 2008; 25(3):237–241.
![]() 3. Hammel, WJ. Care of patients with an indwelling pericardial catheter. Crit Care Nurse. 1998; 18:40–45.
3. Hammel, WJ. Care of patients with an indwelling pericardial catheter. Crit Care Nurse. 1998; 18:40–45.
4. Infusion Nurses Society. Policies and procedures for -infusion nursing, 3rd ed. Norwood, MA: Author; 2006.
5. Intravenous Nurses Society. Infusion nursing standards of practice. J Infus Nurs. 2006; 29(1S):S1–S90. [(2006)].
6. Johnson, KK, Soundarraj, D, Patel, P. Tenecteplase for -malignant pericardial effusion. Pharmacotherapy. 2007; 27(2):303–305.
7. Kolski, BC, et al. Echocardiographic assessment of the -accuracy of computed tomography in the diagnosis of -hemodynamically significant pericardial effusions. J Am Soc Echocardiogr. 2007; 21(4):377–379.
8. Maruyama, R, et al, Catheter drainage followed by the -instillation of bleomycin to manage malignant pericardial effusion in non-small cell lung cancer. a multi-institutional phase II trial. J Thorac Oncol. 2007; 2(1):65–68.
![]() 9. O’Grady, NP, et al, Guidelines for the prevention of intravascular catheter-related infections. Centers for Disease Control and Prevention. MMWR Recommend Rep. 2002; 51(RR-10):1–29.
9. O’Grady, NP, et al, Guidelines for the prevention of intravascular catheter-related infections. Centers for Disease Control and Prevention. MMWR Recommend Rep. 2002; 51(RR-10):1–29.
10. Seferovic, PM, et al. Management strategies in pericardial emergencies. Herz. 2006; 31(9):891–900.
11. Staltari, D, et al, Laparoscopic pericardio-peritoneal window. An alternative approach in the treatment of recurrent pericardial effusion, in-hospital evolution and survival. Surg Laparosc Endosc Percutan Tech. 2007; 17(2):116–119.
12. Swanson, N, Mirza, I, Wijesinghe, N, et al. Primary percutaneous balloon pericardiotomy for malignant pericardial effusion. Cath Cardiovasc Interv. 2008; 71(4):504–507.
13. Valley, VT, et al. Pericarditis and cardiac tamponade,. available at www.eMedicine.com, updated May 12, 2008.
14. Yarlagadda, C. Cardiac tamponade,. available at www.eMedicine.com, updated May 24, 2008.