Single-Pressure and Multiple-Pressure Transducer Systems
PREREQUISITE NURSING KNOWLEDGE
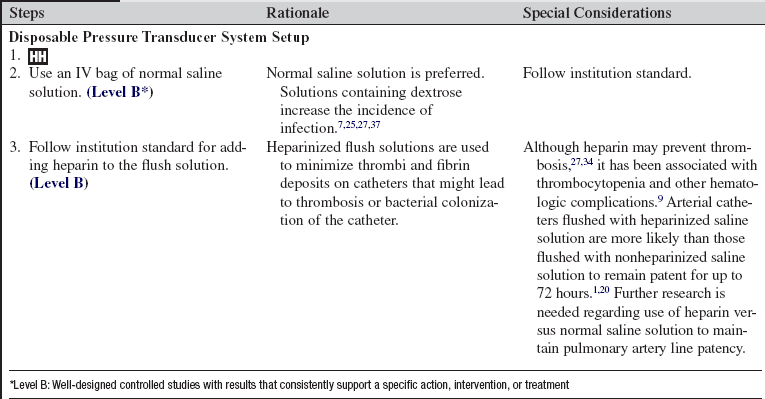
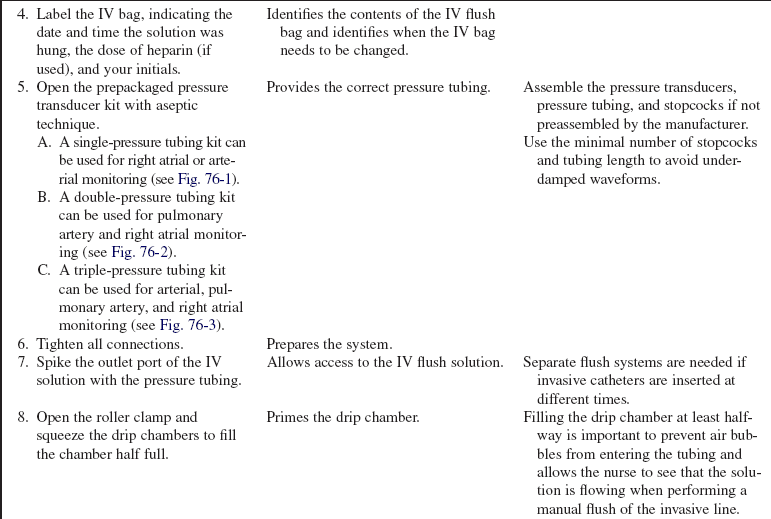
• Knowledge of the anatomy and physiology of the cardiovascular system is needed.
• Knowledge of principles of aseptic technique is necessary.
• Fluid-filled pressure monitoring systems used for bedside hemodynamic pressure monitoring are based on the principle that a change in pressure at any point in an unobstructed system results in similar pressure changes at all other points of the system.
• Pressure transducers detect the pressure waveform generated by ventricular ejection and convert that pressure wave into an electrical signal, which is transmitted to the monitoring equipment for representation as a waveform on the oscilloscope.
• Invasive measurement of intravascular (arterial) pressure requires insertion of a catheter into an artery.
• Invasive measurement of intracardiac (right atrial and pulmonary artery) pressures requires insertion of a catheter into the pulmonary artery.
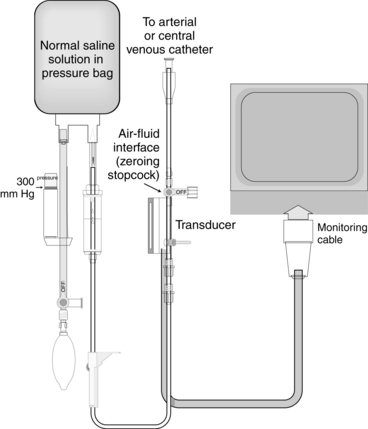
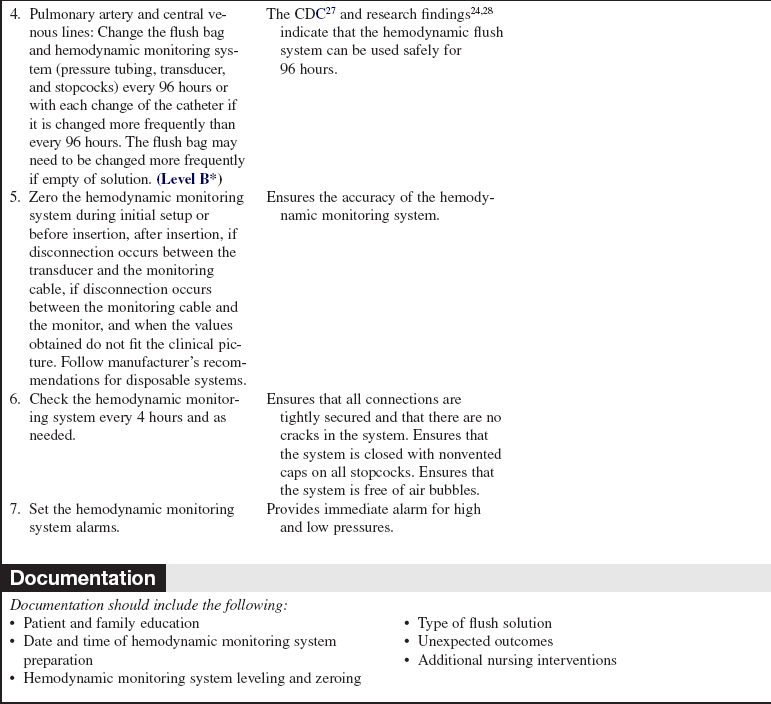
• A single-pressure transducer system is used to measure pressure from a single catheter (e.g., arterial catheter, central venous; Fig. 76-1).
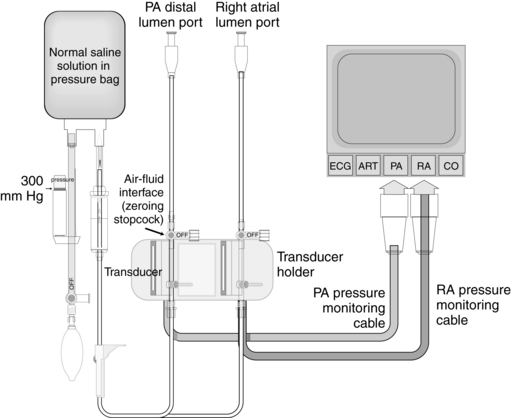
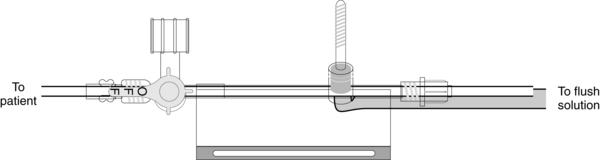
• A double-pressure transducer system is used to measure pressure from two catheters (e.g., arterial and central venous) or two ports (e.g., pulmonary artery and right atrial) from a single catheter (e.g., pulmonary artery catheter; Fig. 76-2).
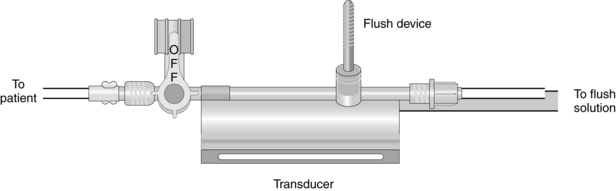
• A triple-pressure transducer system is commonly used to measure pressures from the arterial and pulmonary artery catheters. With this system, arterial pressures, pulmonary artery pressures, and right atrial pressures can be obtained (Fig. 76-3).
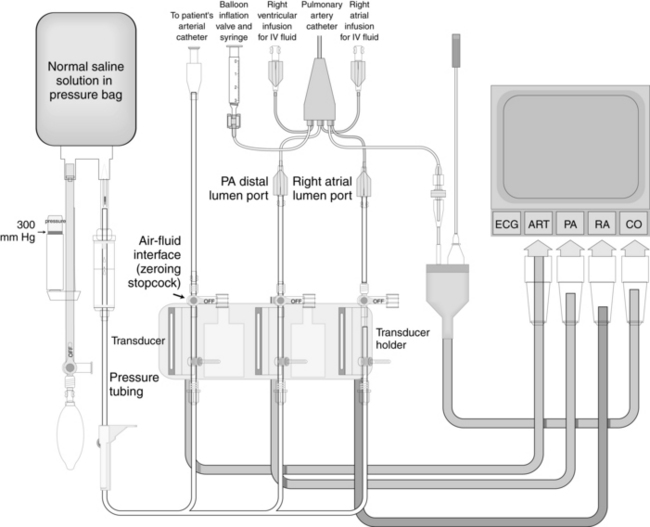
Figure 76-3 Triple-pressure transducer system. (Drawing by Paul W. Schiffmacher, Thomas Jefferson University, Philadelphia, PA.)
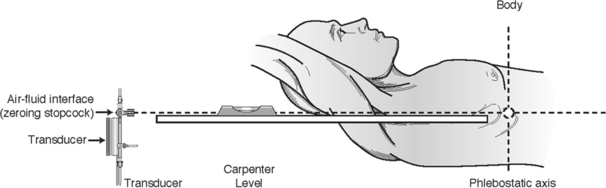
• For accuracy of the hemodynamic values obtained from any transducer system, leveling and zeroing are essential.
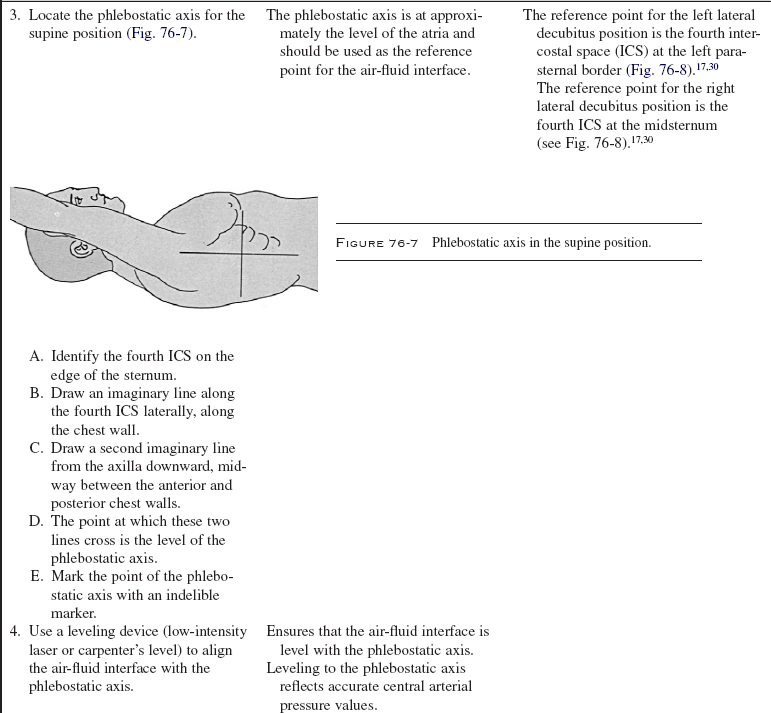
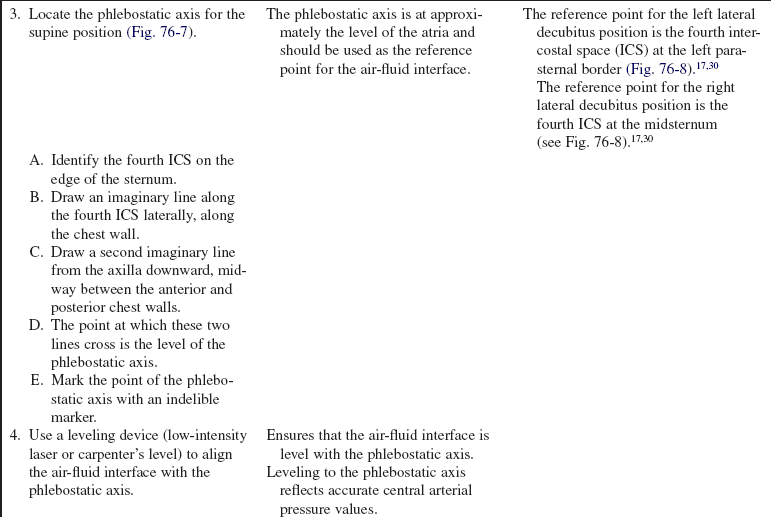
• All hemodynamic values (pulmonary artery, right atrial, and arterial) are referenced to the level of the atria. The external reference point of the atria is the phlebostatic axis.
EQUIPMENT
• Invasive catheter (e.g., arterial, pulmonary artery)
• Pressure modules and cables for interface with the monitor
• Cardiac output cable with a thermistor/injectate sensor for use with the pulmonary artery catheter
• Pressure transducer system, including flush solution recommended according to institution standard, a pressure bag or device, pressure tubing with transducers, and flush device
PATIENT AND FAMILY EDUCATION
• Assess patient and family understanding of hemodynamic monitoring and the reason for its use.  Rationale: Clarification or reinforcement of information is an expressed patient and family need.
Rationale: Clarification or reinforcement of information is an expressed patient and family need.
• Explain the procedure for hemodynamic monitoring.  Rationale: This information prepares the patient and the family for what to expect and may decrease anxiety.
Rationale: This information prepares the patient and the family for what to expect and may decrease anxiety.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess the patient for conditions that may warrant the use of a hemodynamic monitoring system, including hypotension or hypertension, cardiac failure, cardiac arrest, hemorrhage, respiratory failure, fluid imbalances, oliguria, anuria, and sepsis.  Rationale: Assessment provides data regarding signs and symptoms of hemodynamic instability.
Rationale: Assessment provides data regarding signs and symptoms of hemodynamic instability.
• Obtain the patient’s medical history of coagulopathies, use of anticoagulants, vascular abnormalities, and peripheral neuropathies.  Rationale: The medical history assists in determining the safety of the procedure and aids in site selection.
Rationale: The medical history assists in determining the safety of the procedure and aids in site selection.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and the family understand preprocedural teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of previously taught information is evaluated and reinforced.
Rationale: Understanding of previously taught information is evaluated and reinforced.
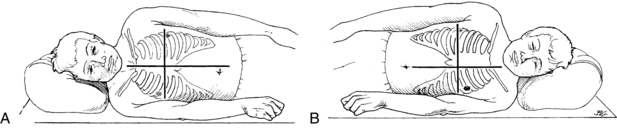
• Position the patient in the supine position with the head of bed flat or elevated up to 45 degrees.  Rationale: This positioning prepares the patient for hemodynamic monitoring.
Rationale: This positioning prepares the patient for hemodynamic monitoring.
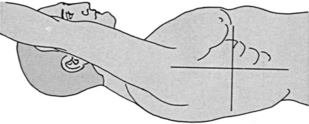
Figure 76-7 Phlebostatic axis in the supine position.
References
American Association of Critical-Care Nurses, Evaluation of the effects of heparinized and nonheparinized flush solutions on the patency of arterial pressure monitoring lines. the AACN Thunder Project. Am J Crit Care 1993; 2:3–15.
Bisnaire, D, Robinson, L. Accuracy of leveling hemodynamic transducer systems. CACCN. 1999; 10:16–19.
Blanch, L, et al. Short term effects of prone position -in critically ill patients with acute respiratory distress syndrome. Intensive Care Med. 1997; 23:1033–1039.
Bridges, EJ, et al. Effect of 30 degree lateral recumbent position on pulmonary artery and pulmonary artery wedge pressures in critically ill adult cardiac surgery patients. Am J Crit Care. 2000; 9:262–275.
Bridges, EJ, et al, Direct arterial vs. oscillometric monitoring of blood pressure. stop comparing and pick one . Crit Care Nurse 1997; 17:96–102. [[comment]].
Brussel, T, et al. Mechanical ventilation in the prone -position for acute respiratory failure after cardiac surgery. J Cardiothorac Vasc Anesth. 1993; 7:541–546.
Buxton, AE, et al. Failure of disposable domes to prevent septicemia acquired from contaminated pressure transducers. Chest. 1978; 74:508–513.
Cason, CL, et al. Effects of backrest elevation and -position on pulmonary artery pressures. Cardiovasc Nurs. 1990; 26:1–5.
Chong, BH. Heparin-induced thrombocytopenia. Br J Haematol. 1995; 89:431–439.
Chulay, M, Miller, T. The effect of backrest elevation on pulmonary artery and pulmonary capillary wedge pressures in patients after cardiac surgery. Heart Lung. 1984; 13:138–140.
Clochesy, J, Hinshaw, AD, Otto, CW. Effects of change of position on pulmonary artery and pulmonary capillary wedge pressure in mechanically ventilated patients. NITA. 1984; 7:223–225.
Dobbin, K, et al, Pulmonary artery pressure measurement in patients with elevated pressures. effect of backrest elevation and method of measurement. Am J Crit Care 1992; 1:61–69.
Fridrich, P, et al. The effects of long-term prone positioning in patients with trauma-induced adult respiratory distress syndrome. Anesth Analg. 1996; 83:1206–1211.
Groom, L, Frisch, SR, Elliot, M. Reproducibility and accuracy of pulmonary artery pressure measurement in supine and lateral positions. Heart Lung. 1990; 19:147–151.
Jolliet, P, Bulpa, P, Chevrolet, JC, Effects of prone position on gas exchange and hemodynamics in severe acute respiratory distress syndrome. Crit Care Med 1998; 26 :1977–1985.
Keating, D, et al. Effect of sidelying positions on pulmonary artery pressures. Heart Lung. 1986; 15:605–610.
Keckeisen, M, Protocols for practice. hemodynamic monitoring seriespulmonary artery pressure monitoring. 1997. American Association of Critical-Care Nurses: Aliso Viejo, CA.
Kennedy, GT, Bryant, A, Crawford, MH. The effects of lateral body positioning on measurements of pulmonary artery and pulmonary wedge pressures. Heart Lung. 1984; 13:155–158.
Kirkhoff, KT, Rebenson-Piano M, Mean arterial pressure readings. variations with positions and transducer level. Nurs Res 1984; 33:343–345.
Kulkarni, M, et al. Heparinized saline versus normal saline in maintaining patency of the radial artery catheter. Can J Surg. 1994; 37:37–42.
Lambert, CW, Cason, CL, Backrest elevation and pulmonary artery pressures. research analysis. Dimens Crit Care Nurs 1990; 9:327–335.
Langer, M, et al. The prone position in ARDS patients. Chest. 1988; 94:103–107.
Laulive, JL. Pulmonary artery pressures and position changes in the critically ill adult. Dimens Crit Care Nurs. 1982; 1:28–34.
Luskin, RL, et al, Extended use of disposable pressure transducers. a bacteriologic evaluation. JAMA 1986; 255 :916–920.
Maki, DG, Martin, WT, Nationwide epidemic of septicemia caused by contaminated infusion products. IV: growth of microbial pathogens in fluids for intravenous infusion. J Infect Dis 1975; 131:267–272.
McGhee, BH, Bridges, MEJ, Monitoring arterial blood pressure. what you may not know. Crit Care Nurse 2002; 22:60–79.
O’Grady, NP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.
O’Malley, MK, et al. Value of routine pressure monitoring system changes after 72 hours of use. Crit Care Med. 1994; 22:1424–1430.
Osika, C, Measurement of pulmonary artery pressures. supine verses side-lying head-elevated positions. Heart Lung 1989; 18:298–299.
Paolella, LP, et al, Topographic location of the left atrium by computed tomography. reducing pulmonary artery catheter calibration error. Crit Care Med 1988; 16:1154–1156.
Pappert, D, et al. Influence of positioning on ventilation-perfusion relationships in severe adult respiratory distress syndrome. Chest. 1994; 106:1511–1516.
Pauca, AL, et al. Does radial artery pressure accurately reflect aortic pressure. Chest. 1992; 102:1193–1198.
Pelosi, P, et al. Effects of the prone position on respiratory mechanics and gas exchange during acute lung injury. Am J Respir Crit Care Med. 1998; 157:387–393.
Randolph, AG, et al. Benefit of heparin in central venous and pulmonary artery catheters. Chest. 1998; 113:165–171.
Rice, WP, et al. A comparison of hydrostatic leveling methods in invasive pressure monitoring. Crit Care Nurse. 2000; 20:20–30.
Ross, CJ, Jones, R. Comparisons of pulmonary artery pressure measurements in supine and 30 degree lateral positions. Can J Cardiovasc Nurs. 1995; 6:4–8.
Solomon, SL, et al. Nosocomial fungemia in neonates associated with intravascular pressure-monitoring devices. Pediatr Infect Dis. 1986; 5:680–685.
Voggenreiter, G, et al. Intermittent prone positioning in the treatment of severe and moderate posttraumatic lung injury. Crit Care Med. 1999; 27:2375–2382.
Vollman, KM, Bander, JJ. Improved oxygenation utilizing a prone positioner in patients with acute respiratory distress syndrome. Intensive Care Med. 1996; 22:1105–1111.
Wild, L. Effect of lateral recumbent positions on measurement of pulmonary artery and pulmonary artery wedge pressures in critically ill adults. Heart Lung. 1984; 13:305.
Wilson, AE, et al. Effect of backrest position on hemodynamic and right ventricular measurements in critically ill adults. Am J Crit Care. 1996; 5:264–270.
Woods, SL, Mansfield, LW. Effect of body position upon pulmonary artery and pulmonary capillary wedge pressures in noncritically ill patients. Heart Lung. 1976; 5:83–90.
Darovic, GO, Hemodynamic monitoring. invasive and noninvasive clinical application. ed 3. Saunders, Philadelphia, 2002.
Imperial-Perez F, McRae, M, Protocols for practice. hemodynamic monitoring series: arterial pressure monitoring. American Association of Critical-Care Nurses, Aliso Viejo, CA, 1998.
Kee, LL, et al. Echocardiographic determination of valid zero reference levels in supine and lateral positions. Am J Crit Care. 1993; 2:72–80.
Mermel, LA, Maki, DG, Epidemic bloodstream infections from hemodynamic pressure monitoring. signs of the times. Infect Control Hosp Epidemiol 1989; 10:47–53.
Pearson, ML, Hospital infection control practices advisory committee. guideline for prevention of intravascular device-related infections. Infect Control Hosp Epidemiol 1996; 17:438–473.
Quaal, SJ, Weir, C, Effect of head of bed position on pulmonary artery pressure measurements. a review of the literature. Online J Knowledge Synthesis Nurs 1995; 2:1–10.
Shih, F. Patient positioning and the accuracy of pulmonary artery pressure measurements. Int J Nurs Studies. 1999; 36:497–505.
Vollman, KM. What are the practice guidelines for prone positioning of acutely ill patients? Specifically, what are the recommendations related to hemodynamic monitoring and tube feeding. Crit Care Nurse. 2001; 21:84–86.