Pulmonary Artery Catheter and Pressure Lines, Troubleshooting
PREREQUISITE NURSING KNOWLEDGE
• Knowledge of the cardiovascular anatomy and physiology is needed.
• Knowledge of the pulmonary anatomy and physiology is necessary.
• An understanding of basic dysrhythmia recognition and treatment of life-threatening dysrhythmias is important.
• Advanced cardiac life support knowledge and skills are needed.
• Knowledge of principles of aseptic technique is necessary.
• Understanding of the set-up of the hemodynamic monitoring system (see Procedure 76) is needed.
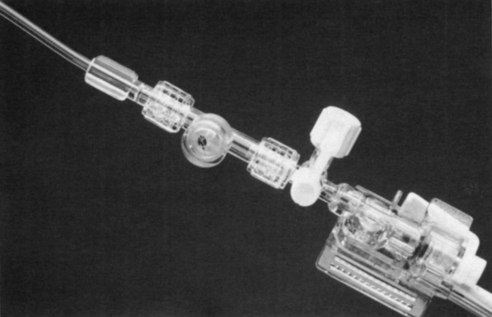
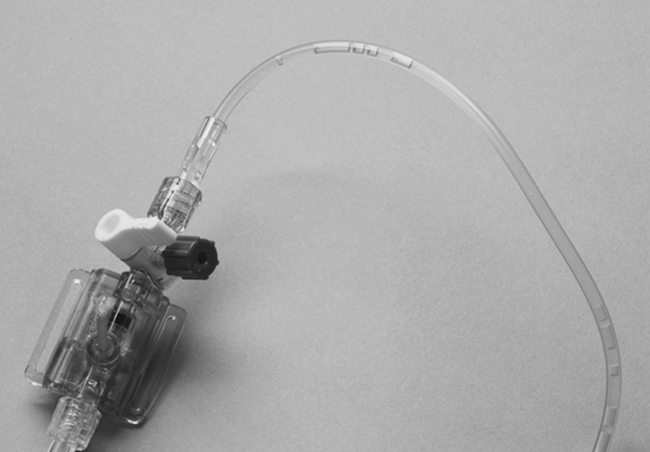
• Anatomy of the pulmonary artery (PA) catheter (see Fig. 73-1) and the location of the PA catheter in the heart and pulmonary artery (see Fig. 73-2) should be understood.
• Pulmonary artery occlusion pressure may be referred to as pulmonary artery wedge pressure.
• After wedging of the PA catheter, air is passively removed by disconnecting the syringe from the balloon-inflation port. Active withdrawal of air from the balloon is avoided because it can weaken the balloon, pull the balloon structure into the inflation lumen, and possibly cause balloon rupture.
• The pulmonary artery diastolic pressure (PADP) and the pulmonary artery occlusion pressure (PAOP) are indirect measures of left ventricular end-diastolic pressure (LVEDP). Usually, the PAOP is approximately 1 to 4 mm Hg less than the PADP. Because these two pressures are similar, the PADP is commonly followed, which minimizes the frequency of balloon inflation, thus decreasing the potential of balloon rupture.
• Differences between the PADP and the PAOP may exist for patients with pulmonary hypertension, chronic obstructive lung disease, adult respiratory distress syndrome, pulmonary embolus, and tachycardia.
• Pulmonary artery pressures (PAPs) may be elevated because of pulmonary artery hypertension, pulmonary disease, mitral valve disease, left ventricular failure, atrial or ventricular left-to-right shunt, pulmonary emboli, or hypervolemia.
• PAPs may be decreased because of hypovolemia or vasodilation.
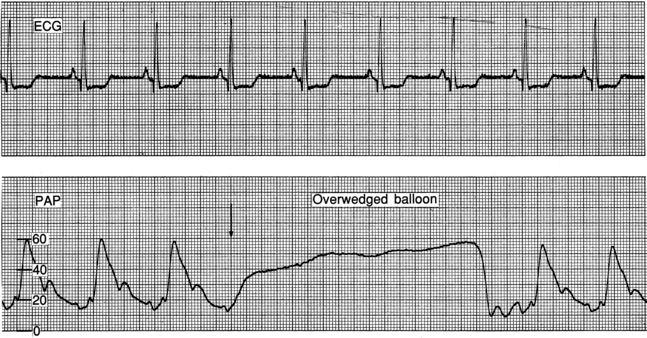
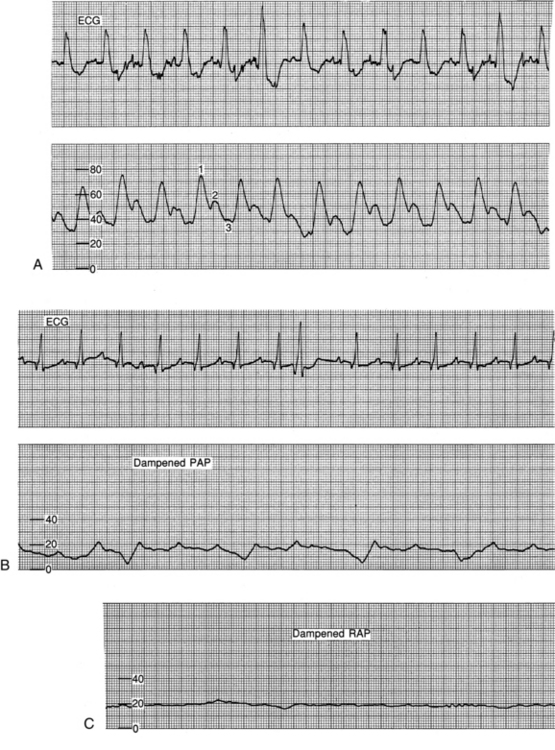
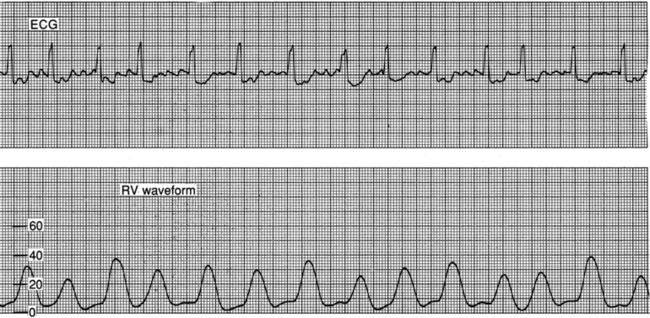
• The waveforms that occur during insertion should be recognized, including right atrial (RA), right ventricular (RV), PA, and pulmonary artery occlusion (PAO; see Fig. 73-3).
• a wave reflects atrial contraction. The c wave reflects closure of the atrioventricular valves. The v wave reflects passive filling of the atria during ventricular systole (see Figs. 73-4 and 73-5).
• Knowledge of normal hemodynamic values (see Table 67-1) is needed.
• Elevated a and v waves may be evident in RA or central venous pressure (CVP) and in PAO waveforms. These elevations may occur in patients with cardiac tamponade, constrictive pericardial disease, and hypervolemia.
• Elevated a waves in the RA or CVP waveform may occur in patients with pulmonic or tricuspid stenosis, right ventricular ischemia or infarction, right ventricular failure, pulmonary artery hypertension, and atrioventricular (AV) dissociation.
• Elevated a waves in the PAO waveform may occur in patients with mitral stenosis, acute left ventricular ischemia or infarction, left ventricular failure, and AV dissociation.
• Elevated v waves in the RA or CVP waveform may occur in patients with tricuspid insufficiency.
• Elevated v waves in the PAO waveform may occur in patients with mitral insufficiency or ruptured papillary muscle.
EQUIPMENT
• Needleless blood sampling access device
• Pressure transducer system, including flush solution recommended according to institution standard, a pressure bag or device, pressure tubing with transducers, and flush device
Additional equipment to have available as needed includes the following:
PATIENT AND FAMILY EDUCATION
• Explain the troubleshooting procedures to the patient and family.  Rationale: The patient and family are kept informed, and anxiety is reduced.
Rationale: The patient and family are kept informed, and anxiety is reduced.
• Explain the patient’s expected participation during the procedure.  Rationale: This explanation will encourage patient assistance.
Rationale: This explanation will encourage patient assistance.
• Inform the patient and family of signs and symptoms to report to the critical care nurse, including chest pain, palpitations, new cough, tenderness at the insertion site, and chills.  Rationale: The patient is encouraged to report signs of discomfort and potential PA catheter complications.
Rationale: The patient is encouraged to report signs of discomfort and potential PA catheter complications.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Monitor PA waveforms continuously.  Rationale: The PA catheter may migrate forward into a wedged position or may loop around and move back into the right ventricle.
Rationale: The PA catheter may migrate forward into a wedged position or may loop around and move back into the right ventricle.
• Assess the configuration of the PA catheter waveforms.  Rationale: Thrombus formation at the tip of the catheter lumen may be evidenced by an overdamped waveform.
Rationale: Thrombus formation at the tip of the catheter lumen may be evidenced by an overdamped waveform.
• Assess the patient’s hemodynamic and cardiovascular status.  Rationale: The patient’s clinical assessment should correlate with the PA catheter readings.
Rationale: The patient’s clinical assessment should correlate with the PA catheter readings.
• Assess the patient and the PA catheter site for signs of infection.  Rationale: Infection can develop because of the invasive nature of the PA catheter.
Rationale: Infection can develop because of the invasive nature of the PA catheter.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient understands preprocedural teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of previously taught information is evaluated and reinforced.
Rationale: Understanding of previously taught information is evaluated and reinforced.
• Determine the patency of the patient’s intravenous catheters.  Rationale: Access may be needed for administration of emergency medication or fluids.
Rationale: Access may be needed for administration of emergency medication or fluids.
References
![]() 1. Blanch, L, et al. Short term effects of prone position in critically ill patients with acute respiratory distress syndrome. Intensive Care Med. 1997; 23:1033–1039.
1. Blanch, L, et al. Short term effects of prone position in critically ill patients with acute respiratory distress syndrome. Intensive Care Med. 1997; 23:1033–1039.
![]() 2. Brussel, T, et al. Mechanical ventilation in the prone position for acute respiratory failure after cardiac surgery. J Cardiothorac Vasc Anesth. 1993; 7:541–546.
2. Brussel, T, et al. Mechanical ventilation in the prone position for acute respiratory failure after cardiac surgery. J Cardiothorac Vasc Anesth. 1993; 7:541–546.
![]() 3. Cason, CL, et al. Effects of backrest elevation and position on pulmonary artery pressures. Cardiovasc Nurs. 1990; 26:1–5.
3. Cason, CL, et al. Effects of backrest elevation and position on pulmonary artery pressures. Cardiovasc Nurs. 1990; 26:1–5.
![]() 4. Chulay, M, Miller, T. The effect of backrest elevation on pulmonary artery and pulmonary capillary wedge pressures in patients after cardiac surgery. Heart Lung. 1984; 13:138–140.
4. Chulay, M, Miller, T. The effect of backrest elevation on pulmonary artery and pulmonary capillary wedge pressures in patients after cardiac surgery. Heart Lung. 1984; 13:138–140.
![]() 5. Clochesy, J, Hinshaw, AD, Otto, CW. Effects of change of position on pulmonary artery and pulmonary capillary wedge pressure in mechanically ventilated patients. NITA. 1984; 7:223–225.
5. Clochesy, J, Hinshaw, AD, Otto, CW. Effects of change of position on pulmonary artery and pulmonary capillary wedge pressure in mechanically ventilated patients. NITA. 1984; 7:223–225.
![]() 6. Dobbin, K, et al, Pulmonary artery pressure measurement in patients with elevated pressures. effect of backrest -elevation and method of measurement. Am J Crit Care 1992; 1:61–69.
6. Dobbin, K, et al, Pulmonary artery pressure measurement in patients with elevated pressures. effect of backrest -elevation and method of measurement. Am J Crit Care 1992; 1:61–69.
![]() 7. Fridrich, P, et al. The effects of long-term prone positioning in patients with trauma-induced adult respiratory -distress syndrome. Anesth Analg. 1996; 83:1206–1211.
7. Fridrich, P, et al. The effects of long-term prone positioning in patients with trauma-induced adult respiratory -distress syndrome. Anesth Analg. 1996; 83:1206–1211.
![]() 8. Groom, L, Frisch, SR, Elliot, M. Reproducibility and accuracy of pulmonary artery pressure measurement in supine and lateral positions. Heart Lung. 1990; 19:147–151.
8. Groom, L, Frisch, SR, Elliot, M. Reproducibility and accuracy of pulmonary artery pressure measurement in supine and lateral positions. Heart Lung. 1990; 19:147–151.
![]() 9. Jolliet, P, Bulpa, P, Chevrolet, JC. Effects of prone position on gas exchange and hemodynamics in severe acute -respiratory distress syndrome. Crit Care Med. 1998; 26:1977.
9. Jolliet, P, Bulpa, P, Chevrolet, JC. Effects of prone position on gas exchange and hemodynamics in severe acute -respiratory distress syndrome. Crit Care Med. 1998; 26:1977.
![]() 10. Keating, D, et al. Effect of sidelying positions on pulmonary artery pressures. Heart Lung. 1986; 15:605–610.
10. Keating, D, et al. Effect of sidelying positions on pulmonary artery pressures. Heart Lung. 1986; 15:605–610.
![]() 11. Kennedy, GT, Bryant, A, Crawford, MH. The effects of lateral body positioning on measurements of pulmonary artery and pulmonary wedge pressures. Heart Lung. 1984; 13:155–158.
11. Kennedy, GT, Bryant, A, Crawford, MH. The effects of lateral body positioning on measurements of pulmonary artery and pulmonary wedge pressures. Heart Lung. 1984; 13:155–158.
![]() 12. Lambert, CW, Cason, CL, Backrest elevation and pulmonary artery pressures. research analysis. Dimens Crit Care Nurs 1990; 9:327–335.
12. Lambert, CW, Cason, CL, Backrest elevation and pulmonary artery pressures. research analysis. Dimens Crit Care Nurs 1990; 9:327–335.
![]() 13. Langer, M, et al. The prone position in ARDS patients. Chest. 1988; 94:103–107.
13. Langer, M, et al. The prone position in ARDS patients. Chest. 1988; 94:103–107.
![]() 14. Laulive, JL. Pulmonary artery pressures and position changes in the critically ill adult. Dimens Crit Care Nurs. 1982; 1:28–34.
14. Laulive, JL. Pulmonary artery pressures and position changes in the critically ill adult. Dimens Crit Care Nurs. 1982; 1:28–34.
![]() 15. O’Grady, NP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.
15. O’Grady, NP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.
![]() 16. Osika, C, Measurement of pulmonary artery pressures. supine verses side-lying head-elevated positions. Heart Lung 1989; 18:298–299.
16. Osika, C, Measurement of pulmonary artery pressures. supine verses side-lying head-elevated positions. Heart Lung 1989; 18:298–299.
![]() 17. Pappert, D, et al. Influence of positioning on ventilation-perfusion relationships in severe adult respiratory distress syndrome. Chest. 1994; 106:1511–1516.
17. Pappert, D, et al. Influence of positioning on ventilation-perfusion relationships in severe adult respiratory distress syndrome. Chest. 1994; 106:1511–1516.
![]() 18. Pelosi, P, et al. Effects of the prone position on respiratory mechanics and gas exchange during acute lung injury. Am J Respir Crit Care Med. 1998; 157:387–393.
18. Pelosi, P, et al. Effects of the prone position on respiratory mechanics and gas exchange during acute lung injury. Am J Respir Crit Care Med. 1998; 157:387–393.
![]() 19. Voggenreiter, G, et al. Intermittent prone positioning in the treatment of severe and moderate posttraumatic lung injury. Crit Care Med. 1999; 27:2375–2382.
19. Voggenreiter, G, et al. Intermittent prone positioning in the treatment of severe and moderate posttraumatic lung injury. Crit Care Med. 1999; 27:2375–2382.
![]() 20. Vollman, KM, Bander, JJ. Improved oxygenation utilizing a prone positioner in patients with acute respiratory distress syndrome. Intensive Care Med. 1996; 22:1105–1111.
20. Vollman, KM, Bander, JJ. Improved oxygenation utilizing a prone positioner in patients with acute respiratory distress syndrome. Intensive Care Med. 1996; 22:1105–1111.
![]() 21. Wild, L. Effect of lateral recumbent positions on measurement of pulmonary artery and pulmonary artery wedge pressures in critically ill adults. Heart Lung. 1984; 13:305.
21. Wild, L. Effect of lateral recumbent positions on measurement of pulmonary artery and pulmonary artery wedge pressures in critically ill adults. Heart Lung. 1984; 13:305.
![]() 22. Wilson, AE, et al. Effect of backrest position on hemodynamic and right ventricular measurements in critically ill adults. Am J Crit Care. 1996; 5:264–270.
22. Wilson, AE, et al. Effect of backrest position on hemodynamic and right ventricular measurements in critically ill adults. Am J Crit Care. 1996; 5:264–270.
![]() 23. Woods, SL, Mansfield, LW. Effect of body position upon pulmonary artery and pulmonary capillary wedge pressures in noncritically ill patients. Heart Lung. 1976; 5:83–90.
23. Woods, SL, Mansfield, LW. Effect of body position upon pulmonary artery and pulmonary capillary wedge pressures in noncritically ill patients. Heart Lung. 1976; 5:83–90.
Bridges, EJ, Pulmonary artery pressure monitoring. when, how, and what else to use. AACN Adv Crit Care 2006; 17:286–305.
![]() Darovic, GO, Hemodynamic monitoring. invasive and noninvasive clinical application. ed 3. Saunders, Philadelphia, 2002.
Darovic, GO, Hemodynamic monitoring. invasive and noninvasive clinical application. ed 3. Saunders, Philadelphia, 2002.
![]() Keckeisen, M, Protocols for practice. hemodynamic monitoring seriespulmonary artery pressure monitoring. American Association of Critical-Care Nurses, Aliso Viejo, CA, 1997.
Keckeisen, M, Protocols for practice. hemodynamic monitoring seriespulmonary artery pressure monitoring. American Association of Critical-Care Nurses, Aliso Viejo, CA, 1997.
Rauen, CA, Flynn, MB, Bridges, E, Evidence-based practice habits. transforming research into bedside practice. Crit Care Nurse 2009; 29:46–59.