Pulmonary Artery Catheter Removal
PREREQUISITE NURSING KNOWLEDGE
• Knowledge of the normal cardiovascular anatomy and physiology is necessary.
• Knowledge of normal values for intracardiac pressures is important.
• Knowledge of normal coagulation values is needed.
• Knowledge of normal waveform configurations for right atrial pressure (RAP), right ventricular pressure (RVP), pulmonary artery pressure (PAP), and pulmonary artery occlusive pressure (PAOP) is necessary.
• Venous access routes should be known.
• Principles of aseptic technique should be known.
• Advanced cardiac life support knowledge and skills are needed.
• Potential complications associated with removal of the pulmonary artery (PA) catheter should be understood.
• Clinical and technical competence in PA catheter removal is necessary.
• Knowledge of the state nurse practice act is important because some states do not allow this intervention to be performed by a registered nurse.
• Air embolism can occur during the removal of the catheter. Air embolism after the removal of the catheter is a result of air drawn in along the subcutaneous tract and into the vein. During inspiration, negative intrathoracic pressure is transmitted to the central veins. Any opening external to the body to one of these veins may result in aspiration of air into the central venous system. The pathologic effects depend on the volume and rate of air aspirated.
• Indications for the removal of the PA catheter include the following:
 The patient’s condition no longer necessitates hemodynamic monitoring.
The patient’s condition no longer necessitates hemodynamic monitoring.
 Complications occur because of the presence of the PA catheter.
Complications occur because of the presence of the PA catheter.
 The patient shows evidence of a catheter-related infection that may be associated with the PA catheter.
The patient shows evidence of a catheter-related infection that may be associated with the PA catheter.
• Contraindications to percutaneous removal of the PA catheter include the following:
EQUIPMENT
• Sterile and nonsterile gloves
• Fluid-shield face mask or goggles
Additional equipment to have available as needed includes the following:
PATIENT AND FAMILY EDUCATION
• Explain the procedure and the reason for removal of the catheter.  Rationale: This explanation provides information and decreases anxiety.
Rationale: This explanation provides information and decreases anxiety.
• Explain the importance of the patient lying still during the removal of the catheter.  Rationale: The explanation ensures patient cooperation and facilitates safe removal of the catheter.
Rationale: The explanation ensures patient cooperation and facilitates safe removal of the catheter.
• Instruct the patient and family to report any shortness of breath, bleeding, or discomfort at the insertion site after removal of the catheter.  Rationale: Identifies patient discomfort and early recognition of complications.
Rationale: Identifies patient discomfort and early recognition of complications.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess the electrocardiogram (ECG), vital signs, and neurovascular status of the extremity distal to the catheter insertion site.  Rationale: This assessment serves as baseline data.
Rationale: This assessment serves as baseline data.
• If the introducer will also be removed, assess the current coagulation values of the patient.  Rationale: If the patient has abnormal coagulation study results, hemostasis may be difficult to obtain after the introducer catheter is removed.
Rationale: If the patient has abnormal coagulation study results, hemostasis may be difficult to obtain after the introducer catheter is removed.
• Verify catheter position with waveform analysis or chest radiograph.  Rationale: Accuracy of catheter position is ensured.
Rationale: Accuracy of catheter position is ensured.
• Determine whether the patient has a permanent pacemaker, temporary transvenous pacemaker, or ICD.  Rationale: PA catheter removal by a critical care nurse is contraindicated in the presence of a permanent pacemaker, temporary transvenous pacemaker, or ICD. Entanglement of the PA catheter and the pacemaker electrodes can occur.
Rationale: PA catheter removal by a critical care nurse is contraindicated in the presence of a permanent pacemaker, temporary transvenous pacemaker, or ICD. Entanglement of the PA catheter and the pacemaker electrodes can occur.
• Assess the integrity of the PA catheter.  Rationale: The PA catheter should be removed by an advanced practice nurse or physician if the catheter or introducer is not intact (e.g., visible cracks are noted).
Rationale: The PA catheter should be removed by an advanced practice nurse or physician if the catheter or introducer is not intact (e.g., visible cracks are noted).
• Assess the catheter site for redness, warmth at the site, tenderness, or presence of drainage.  Rationale: Signs and symptoms of infection are assessed.
Rationale: Signs and symptoms of infection are assessed.
Patient Preparation
• In collaboration with the physician, determine when the PA catheter should be removed.  Rationale: The invasive catheter is removed when it is no longer indicated.
Rationale: The invasive catheter is removed when it is no longer indicated.
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand preprocedural teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of previously taught information is evaluated and reinforced.
Rationale: Understanding of previously taught information is evaluated and reinforced.
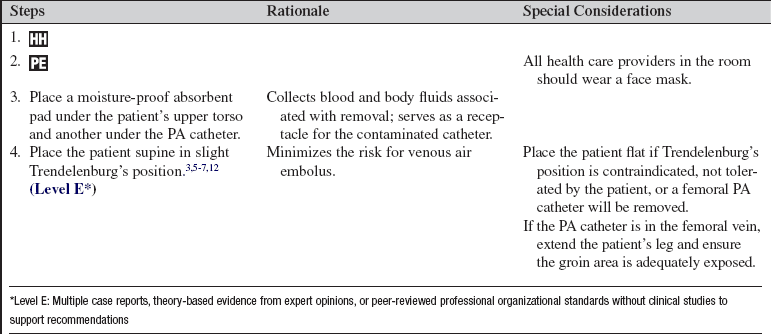
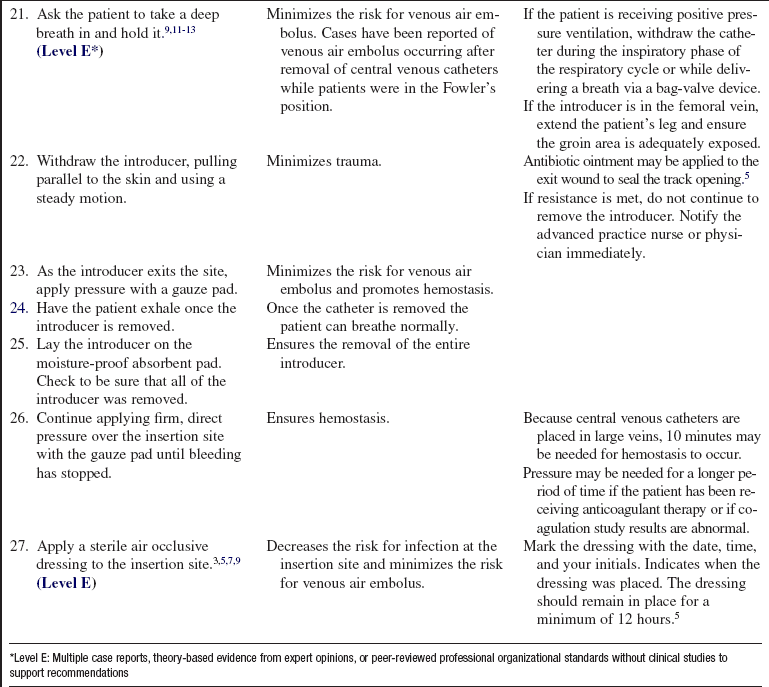
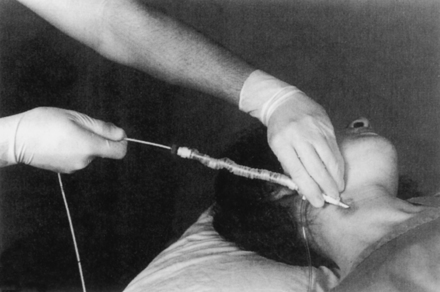
• Place the patient in a supine position with the head of the bed in a slight Trendelenburg’s position (or flat if Trendelenburg’s position is contraindicated or not tolerated by the patient).  Rationale: A normal pressure gradient exists between atmospheric air and the central venous compartment that promotes air entry if the compartment is open. The lower the site of entry below the heart, the lower the pressure gradient, thus minimizing the risk of venous air embolism.
Rationale: A normal pressure gradient exists between atmospheric air and the central venous compartment that promotes air entry if the compartment is open. The lower the site of entry below the heart, the lower the pressure gradient, thus minimizing the risk of venous air embolism.
References
![]() 1. Baldwin, IC, Heland, M. Incidence of cardiac dysrhythmias in patients during pulmonary artery catheter -removal after cardiac surgery. Heart Lung. 2000; 29:155–160.
1. Baldwin, IC, Heland, M. Incidence of cardiac dysrhythmias in patients during pulmonary artery catheter -removal after cardiac surgery. Heart Lung. 2000; 29:155–160.
![]() 2. Chen, Y, et al. Comparison between replacement at 4 days and 7 days on the infection rate for pulmonary artery -catheters in an intensive care unit. Crit Care Med. 2003; 31:1353–1358.
2. Chen, Y, et al. Comparison between replacement at 4 days and 7 days on the infection rate for pulmonary artery -catheters in an intensive care unit. Crit Care Med. 2003; 31:1353–1358.
![]() 3. Ely, EW, et al, Venous air embolism from central venous catheterization. a need for increased physician awareness. Crit Care Med 1999; 27:2113–2117.
3. Ely, EW, et al, Venous air embolism from central venous catheterization. a need for increased physician awareness. Crit Care Med 1999; 27:2113–2117.
![]() 4. Eyer, S, et al, Catheter-related sepsis. prospective, -randomized study of three methods of long-term -catheter maintainence. Crit Care Med 1990; 18:1073–1079.
4. Eyer, S, et al, Catheter-related sepsis. prospective, -randomized study of three methods of long-term -catheter maintainence. Crit Care Med 1990; 18:1073–1079.
![]() 5. Kim, DK, et al, The CVC removal distress syndrome. an unappreciated complication of central venous catheter removal. Am Surgeon 1998; 64:344–347.
5. Kim, DK, et al, The CVC removal distress syndrome. an unappreciated complication of central venous catheter removal. Am Surgeon 1998; 64:344–347.
![]() 6. McCarthy, PM, et al. Air embolism in single-lung transplant patients after central venous catheter removal. Chest. 1995; 107:1178–1179.
6. McCarthy, PM, et al. Air embolism in single-lung transplant patients after central venous catheter removal. Chest. 1995; 107:1178–1179.
![]() 7. Mennim, P, Cormac, FC, Taylor, JD. Venous air embolism associated with removal of central venous catheter. BMJ. 1992; 305:171–172.
7. Mennim, P, Cormac, FC, Taylor, JD. Venous air embolism associated with removal of central venous catheter. BMJ. 1992; 305:171–172.
![]() 8. O’Grady, NP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.
8. O’Grady, NP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.
9. Oztekin, DS, et al. Comparison of complications and procedural activities of pulmonary artery catheter removal by critical care nurses versus medical doctors. Nurs Crit Care. 2008; 13:105–115.
![]() 10. Peter, DA, Saxman, C, Preventing air embolism when removing CVCs. an evidence-based approach to changing practice. Medsurg Nurs 2003; 12:223–229.
10. Peter, DA, Saxman, C, Preventing air embolism when removing CVCs. an evidence-based approach to changing practice. Medsurg Nurs 2003; 12:223–229.
![]() 11. Rountree, WD, Removal of pulmonary artery catheters by registered nurses. a study in safety and complications. Focus Crit Care 1991; 18:313–318.
11. Rountree, WD, Removal of pulmonary artery catheters by registered nurses. a study in safety and complications. Focus Crit Care 1991; 18:313–318.
![]() 12. Turnage, WS, Harper, JV. Venous air embolism occurring after removal of a central venous catheter. Anesth Analg. 1991; 72:559–560.
12. Turnage, WS, Harper, JV. Venous air embolism occurring after removal of a central venous catheter. Anesth Analg. 1991; 72:559–560.
![]() 13. Wadas, TM. Pulmonary artery catheter removal. Crit Care Nurse. 1994; 14:62–72.
13. Wadas, TM. Pulmonary artery catheter removal. Crit Care Nurse. 1994; 14:62–72.
Arnaout, S, et al. Rupture of the chordae of the tricuspid valve after knotting of the pulmonary artery catheter. Chest. 2001; 120:1742–1744.
Darovic, GO, Hemodynamic monitoring. invasive and noninvasive clinical application. ed 3. Saunders, Philadelphia, 2002.
Mirski, MA, Lele, AV, Fitzsimmons, L, et al. Diagnosis and treatment of vascular air embolism. Anesthesiology. 2007; 106:164–177.
Woodrow, P. Central venous catheters and central venous pressure. Nursing Standard. 2002; 16:45–54.