Left Atrial Catheter: Care and Assisting with Removal
The left atrial catheter measures pressure from the left atrium for assessment of left ventricular function after cardiac surgery in the setting of severe left ventricular dysfunction, pulmonary hypertension, presence of circulatory assist devices, or cardiac transplantation.2 The left atrial catheter provides information about left-sided intracardiac pressure. Hemodynamic information obtained with the left atrial catheter is used to guide therapeutic interventions, including administration of fluids and medications and titration of vasoactive and inotropic medications.
PREREQUISITE NURSING KNOWLEDGE
• Knowledge of the cardiovascular anatomy and physiology is necessary.
• Understanding of basic dysrhythmia recognition and treatment of life-threatening dysrhythmias is needed.
• Advanced cardiac life support knowledge and skills are necessary.
• Understanding is needed of the setup of the hemodynamic monitoring system (see Procedure 76).
• Understanding of hemodynamic monitoring is necessary (see Procedure 73).
• Principles of aseptic technique should be understood.
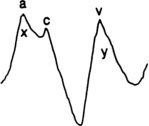
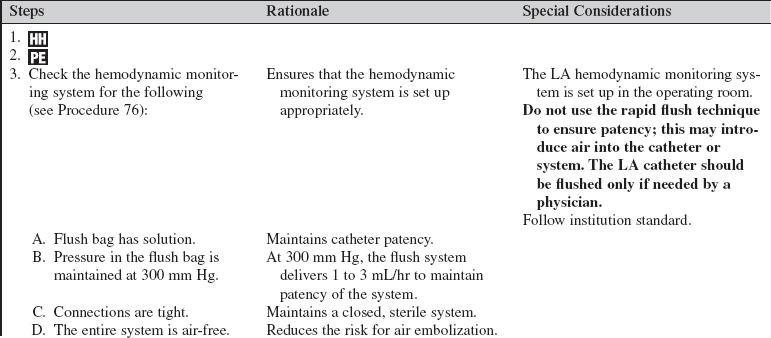
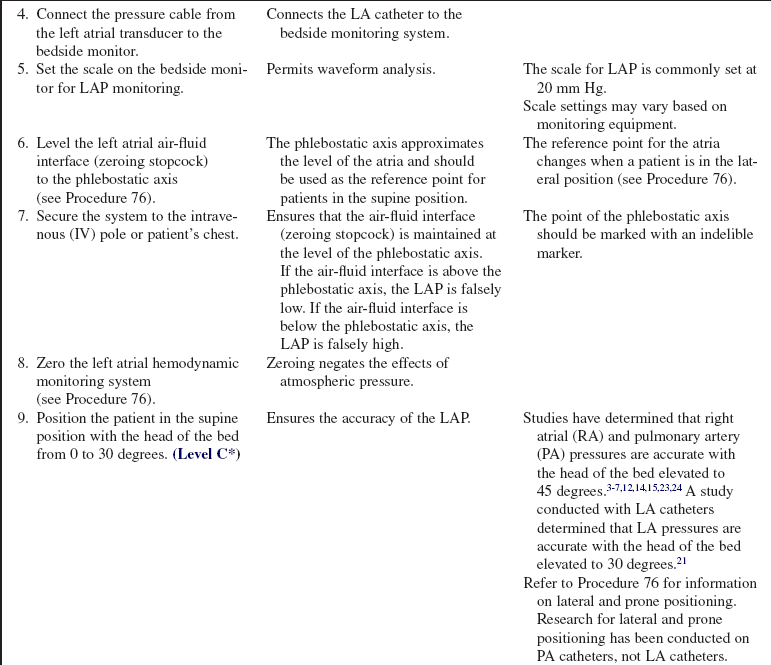
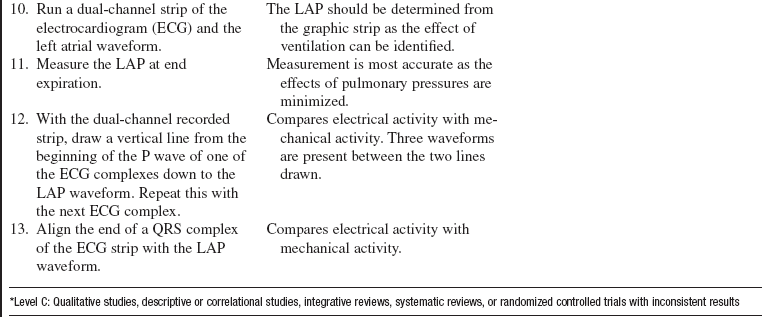
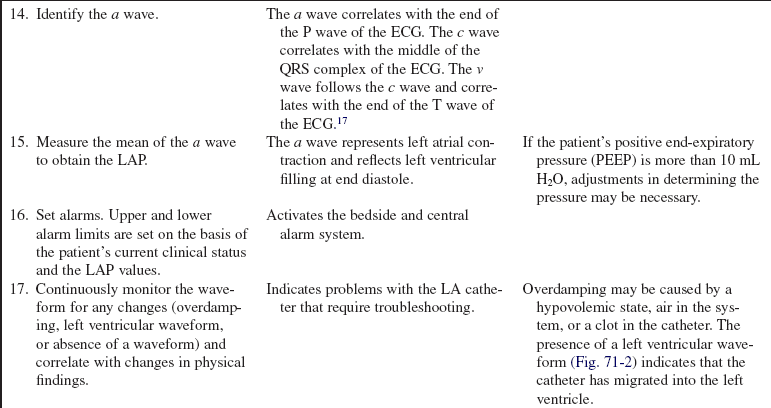
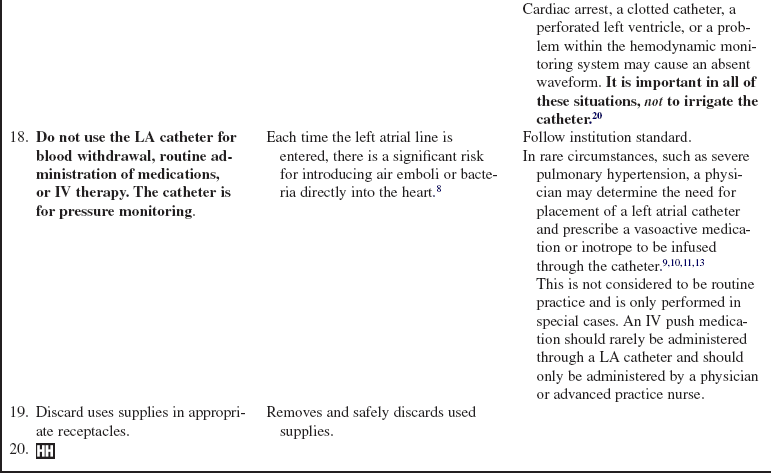
• The left atrial pressure (LAP) waveform is configured similarly to that of a pulmonary artery occlusion pressure or pulmonary artery wedge pressure waveform (Fig. 71-1).
• Understanding of a, c, and v waves is necessary. The a wave reflects left atrial contraction. The c wave reflects closure of the mitral valve. The v wave reflects passive filling of the left atrium during left ventricular systole.
• The LAP is measured with a polyvinyl catheter placed in the left atrium during cardiac surgery. The left atrial catheter can be inserted via a needle puncture of the right superior pulmonary vein, with subsequent threading into the left atrium, or it can be inserted via direct cannulation of the left atrium through a needle puncture at the intraatrial groove.20
• LAP monitoring may be used in the following situations:
 For patients with prosthetic tricuspid or pulmonic valves, in whom pulmonary artery catheters are contraindicated
For patients with prosthetic tricuspid or pulmonic valves, in whom pulmonary artery catheters are contraindicated
 For patients with abnormal heart anatomy (e.g., those with a single ventricle or tricuspid atresia)
For patients with abnormal heart anatomy (e.g., those with a single ventricle or tricuspid atresia)
 For patients with high pulmonary artery pressures, which may interfere with the correlation of pulmonary artery diastolic pressure (PADP) with pulmonary artery occlusion pressure (PAOP)
For patients with high pulmonary artery pressures, which may interfere with the correlation of pulmonary artery diastolic pressure (PADP) with pulmonary artery occlusion pressure (PAOP)
 For accurate information when vasoconstriction medications are infused in conjunction with pulmonary vasodilator medications
For accurate information when vasoconstriction medications are infused in conjunction with pulmonary vasodilator medications
• The normal LAP is 4 to 12 mm Hg.
• One danger with use of this catheter is the potential for air or a blood clot embolus to enter the left atrium and be carried to the brain or other body organs. Close attention to the hemodynamic monitoring system and assessment of the waveform are imperative.
EQUIPMENT
• Left atrial catheter (inserted in the operating room)
Additional equipment to have available, if needed, includes the following:
PATIENT AND FAMILY EDUCATION
• Assess the patient and family understanding of LAP monitoring.  Rationale: Assessment provides information about patient and family knowledge.
Rationale: Assessment provides information about patient and family knowledge.
• Discuss the purpose of the catheter.  Rationale: This discussion informs the patient and family about the catheter and may also decrease anxiety.
Rationale: This discussion informs the patient and family about the catheter and may also decrease anxiety.
• Discuss with the patient and family the location of the catheter and the importance of not touching the catheter or putting tension on the catheter tubing.  Rationale: This discussion may prevent LA catheter contamination and inadvertent LA catheter removal.
Rationale: This discussion may prevent LA catheter contamination and inadvertent LA catheter removal.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess the patient’s hemodynamic, cardiovascular, peripheral vascular, and neurovascular status.  Rationale: The assessment provides baseline data that can be used to compare with the LAP.
Rationale: The assessment provides baseline data that can be used to compare with the LAP.
• Assess the patient’s current laboratory test results, including coagulation studies.  Rationale: Assessment identifies laboratory value abnormalities. Baseline coagulation studies are helpful in determining the risk for bleeding.
Rationale: Assessment identifies laboratory value abnormalities. Baseline coagulation studies are helpful in determining the risk for bleeding.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of previously taught information is evaluated and reinforced.
Rationale: Understanding of previously taught information is evaluated and reinforced.
• Consider administration of sedation as prescribed.  Rationale: An agitated or restless patient could accidentally pull out the LA catheter.
Rationale: An agitated or restless patient could accidentally pull out the LA catheter.
References
![]() 1. Akl, BF, Pett, SB, Jr., Wernly, JA, et al. Unusual complication of direct left atrial pressure monitoring line. J Thorac Cardiovasc Surg. 1984; 88:1033–1035.
1. Akl, BF, Pett, SB, Jr., Wernly, JA, et al. Unusual complication of direct left atrial pressure monitoring line. J Thorac Cardiovasc Surg. 1984; 88:1033–1035.
![]() 2. Bojar, RM, Manual of perioperative care in cardiac and thoracic surgery,. ed 4. Blackwell Sciences, Malden, MA, 2005:229–230.
2. Bojar, RM, Manual of perioperative care in cardiac and thoracic surgery,. ed 4. Blackwell Sciences, Malden, MA, 2005:229–230.
![]() 3. Bridges, EJ, Woods, SL, Pulmonary artery pressure measurement. state of the art. Heart Lung 1993; 22:99–111.
3. Bridges, EJ, Woods, SL, Pulmonary artery pressure measurement. state of the art. Heart Lung 1993; 22:99–111.
![]() 4. Cason, CL, et al. Effects of backrest elevation and position on pulmonary artery pressures. Cardiovasc Nurs. 1990; 26:1–5.
4. Cason, CL, et al. Effects of backrest elevation and position on pulmonary artery pressures. Cardiovasc Nurs. 1990; 26:1–5.
![]() 5. Chulay, M, Miller, T. The effect of backrest elevation on pulmonary artery and pulmonary capillary wedge pressures in patients after cardiac surgery. Heart Lung. 1984; 13:40–138.
5. Chulay, M, Miller, T. The effect of backrest elevation on pulmonary artery and pulmonary capillary wedge pressures in patients after cardiac surgery. Heart Lung. 1984; 13:40–138.
![]() 6. Clochesy, J, Hinshaw, AD, Otto, CW. Effects of change of position on pulmonary artery and pulmonary capillary wedge pressure in mechanically ventilated patients. NITA. 1984; 7:223–225.
6. Clochesy, J, Hinshaw, AD, Otto, CW. Effects of change of position on pulmonary artery and pulmonary capillary wedge pressure in mechanically ventilated patients. NITA. 1984; 7:223–225.
![]() 7. Dobbin, K, et al, Pulmonary artery pressure measurement in patients with elevated pressures. effect of backrest elevation and method of measurement. Am J Crit Care 1992; 1:61–69.
7. Dobbin, K, et al, Pulmonary artery pressure measurement in patients with elevated pressures. effect of backrest elevation and method of measurement. Am J Crit Care 1992; 1:61–69.
![]() 8. Ducharme, FM, et al, Incidence of infection related to arterial catheterization in children. a prospective study. Crit Care Med 1988; 16:272–276.
8. Ducharme, FM, et al, Incidence of infection related to arterial catheterization in children. a prospective study. Crit Care Med 1988; 16:272–276.
![]() 9. Fullerton, DA, St Cyr JA, Albert, JD, et al. Hemodynamic advantage of left atrial epinephrine administration after cardiac operations. Ann Thorac Surg. 1986; 56:1263–1266.
9. Fullerton, DA, St Cyr JA, Albert, JD, et al. Hemodynamic advantage of left atrial epinephrine administration after cardiac operations. Ann Thorac Surg. 1986; 56:1263–1266.
![]() 10. Haider, W, Zwolfer, W, Hiesmayr, M, et al. Improved cardiac performance and reduced pulmonary vascular constriction by epinephrine administration via a left atrial catheter in cardiac surgical patients. J Cardiothorac Vasc Anesth. 1993; 7:684–687.
10. Haider, W, Zwolfer, W, Hiesmayr, M, et al. Improved cardiac performance and reduced pulmonary vascular constriction by epinephrine administration via a left atrial catheter in cardiac surgical patients. J Cardiothorac Vasc Anesth. 1993; 7:684–687.
![]() 11. Hochberg, MS, Gielschinsky, I, Parsonnet, V, et al. Pulmonary inactivation of vasopressors following cardiac operations. Ann Thorac Surg. 1986; 41:200–203.
11. Hochberg, MS, Gielschinsky, I, Parsonnet, V, et al. Pulmonary inactivation of vasopressors following cardiac operations. Ann Thorac Surg. 1986; 41:200–203.
![]() 12. Keating, D, et al. Effect of sidelying positions on pulmonary artery pressures. Heart Lung. 1986; 15:605–610.
12. Keating, D, et al. Effect of sidelying positions on pulmonary artery pressures. Heart Lung. 1986; 15:605–610.
![]() 13. Kelleher, RM, Rose, AA, Ordway, L, Prostaglandins for control of pulmonary hypertension in the postoperative cardiac surgery patient. nursing implications. Crit Care Nurs Clin North Am 1991; 3:741–748.
13. Kelleher, RM, Rose, AA, Ordway, L, Prostaglandins for control of pulmonary hypertension in the postoperative cardiac surgery patient. nursing implications. Crit Care Nurs Clin North Am 1991; 3:741–748.
![]() 14. Lambert, CW, Cason, CL, Backrest elevation and pulmonary artery pressures. research analysis. Dimens Crit Care Nurs 1990; 9:327–335.
14. Lambert, CW, Cason, CL, Backrest elevation and pulmonary artery pressures. research analysis. Dimens Crit Care Nurs 1990; 9:327–335.
![]() 15. Laulive, JL. Pulmonary artery pressures and position changes in the critically ill adult. Dimens Crit Care Nurs. 1982; 1:28–34.
15. Laulive, JL. Pulmonary artery pressures and position changes in the critically ill adult. Dimens Crit Care Nurs. 1982; 1:28–34.
![]() 16. Luskin, RL, et al, Extended use of disposable pressure transducers. a bacteriologic evaluation. JAMA 1986; 255 :916–920.
16. Luskin, RL, et al, Extended use of disposable pressure transducers. a bacteriologic evaluation. JAMA 1986; 255 :916–920.
![]() 17. Mark, JB, Atlas of cardiovascular monitoring. Churchill Livingstone, New York, 1998:18–24.
17. Mark, JB, Atlas of cardiovascular monitoring. Churchill Livingstone, New York, 1998:18–24.
![]() 18. O’Grady, NP, et al, Am J Infect Control. Guidelines for the prevention of intravascular catheter-related infections, 30, 2002:476–489.
18. O’Grady, NP, et al, Am J Infect Control. Guidelines for the prevention of intravascular catheter-related infections, 30, 2002:476–489.
![]() 19. O’Mailley, MK, et al. Value of routine pressure monitoring system changes after 72 hours of use. Crit Care Med. 1994; 22:1424–1430.
19. O’Mailley, MK, et al. Value of routine pressure monitoring system changes after 72 hours of use. Crit Care Med. 1994; 22:1424–1430.
![]() 20. Recker, DH. Procedure for left atrial catheter insertion. Crit Care Nurse. 1985; 5:36–41.
20. Recker, DH. Procedure for left atrial catheter insertion. Crit Care Nurse. 1985; 5:36–41.
![]() 21. Retailliau, MA, McGregor, LM, Woods, SL. The effect of the backrest position on the measurement of left atrial pressure in patients after cardiac surgery. Heart Lung. 1985; 14:477–483.
21. Retailliau, MA, McGregor, LM, Woods, SL. The effect of the backrest position on the measurement of left atrial pressure in patients after cardiac surgery. Heart Lung. 1985; 14:477–483.
![]() 22. Taylor, T. Monitoring left atrial pressures in the open-heart surgical patient. Crit Care Nurse. 1986; 6:62–68.
22. Taylor, T. Monitoring left atrial pressures in the open-heart surgical patient. Crit Care Nurse. 1986; 6:62–68.
![]() 23. Wilson, AE, et al. Effect of backrest position on hemodynamic and right ventricular measurements in critically ill adults. Am J Crit Care. 1996; 5:264–270.
23. Wilson, AE, et al. Effect of backrest position on hemodynamic and right ventricular measurements in critically ill adults. Am J Crit Care. 1996; 5:264–270.
![]() 24. Woods, SL, Mansfield, LW. Effect of body position upon pulmonary artery and pulmonary capillary wedge pressures in noncritically ill patients. Heart Lung. 1976; 5:83–90.
24. Woods, SL, Mansfield, LW. Effect of body position upon pulmonary artery and pulmonary capillary wedge pressures in noncritically ill patients. Heart Lung. 1976; 5:83–90.
![]() Ahrens, TS, Taylor, LA. Hemodynamic waveform analysis. Philadelphia: Saunders; 1992.
Ahrens, TS, Taylor, LA. Hemodynamic waveform analysis. Philadelphia: Saunders; 1992.
![]() Gawlinski, A. Facts and fallacies of patient positioning and hemodynamic management. J Cardiovasc Nurs. 1997; 12:1–15.
Gawlinski, A. Facts and fallacies of patient positioning and hemodynamic management. J Cardiovasc Nurs. 1997; 12:1–15.
![]() Leitman, BS, et al, The left atrial catheter. its uses and complications. Radiology 1992; 185:611–612.
Leitman, BS, et al, The left atrial catheter. its uses and complications. Radiology 1992; 185:611–612.
![]() Rao, PS, Sathyanarayana, PV, Transseptal insertion of left atrial line. a simple and safe technique. Ann Thorac Surg 1993; 55:785–786.
Rao, PS, Sathyanarayana, PV, Transseptal insertion of left atrial line. a simple and safe technique. Ann Thorac Surg 1993; 55:785–786.
![]() Santini, F, et al, Routine left atrial catheterization for the post-operative management of cardiac surgical patients. is the risk justified. Eur J Cardiothoracic Surg 1999; 16:218–221.
Santini, F, et al, Routine left atrial catheterization for the post-operative management of cardiac surgical patients. is the risk justified. Eur J Cardiothoracic Surg 1999; 16:218–221.
![]() Yeo, TC, et al, Retained left atrial catheter. an unusual cardiac source of embolism identified by transesophageal echocardiography. J Am Soc Echocardiogr 1998; 11:66–70.
Yeo, TC, et al, Retained left atrial catheter. an unusual cardiac source of embolism identified by transesophageal echocardiography. J Am Soc Echocardiogr 1998; 11:66–70.