Central Venous/Right Atrial Pressure Monitoring
PREREQUISITE NURSING KNOWLEDGE
• Knowledge of the normal anatomy and physiology of the cardiovascular system is needed.
• Knowledge of the principles of aseptic technique and infection control is necessary.
• Knowledge is needed of the principles of hemodynamic monitoring.
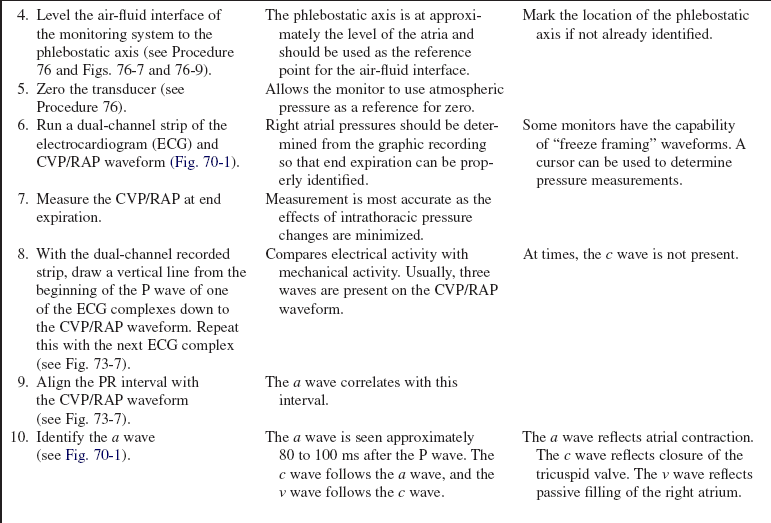
• The central venous pressure (CVP)/right atrial pressure (RAP) represents right-sided heart preload or the volume of blood found in the right ventricle at the end of diastole.
• CVP/RAP influences and is influenced by venous return and cardiac function. Although the CVP/RAP is used as a measure of changes in the right ventricle, the relationship is not linear. Because the right ventricle has the ability to expand and alter its compliance, changes in volume can occur with little change in pressure.
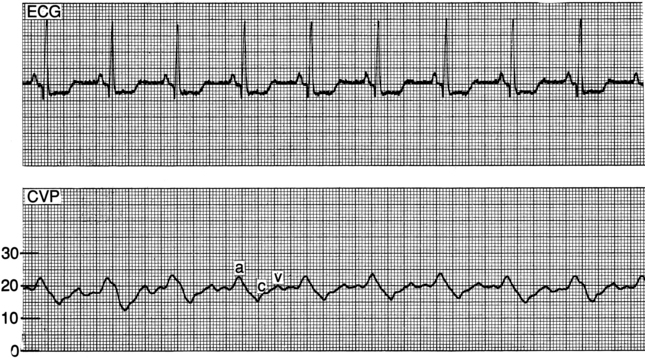
• The CVP/RAP normally ranges from 2 to 8 mm Hg in the adult.
• The central venous catheter is inserted in a central vein with the tip of the catheter placed in the proximal superior vena cava.
• Knowledge is needed of the setup, leveling, and zeroing of the hemodynamic monitoring system (see Procedure 76).
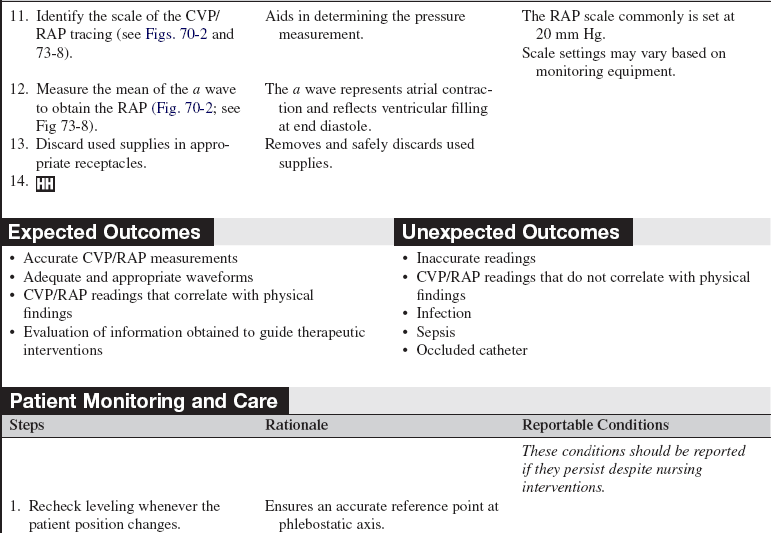
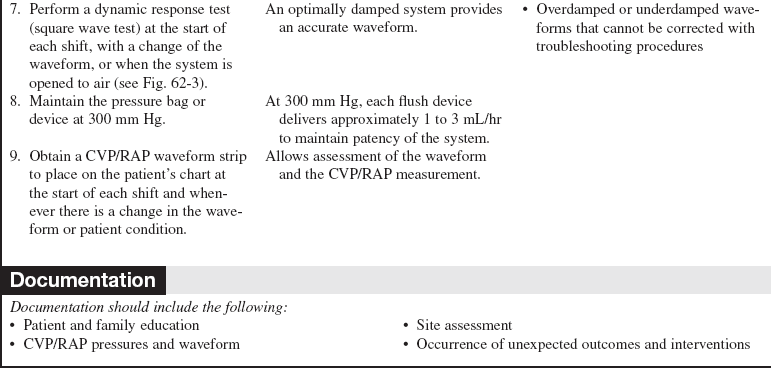
• Understanding of a, c, and v waves is necessary. The a wave reflects right atrial contraction. The c wave reflects closure of the tricuspid valve. The v wave reflects the right atrial filling during ventricular systole. The CVP/RAP measurement is the mean of the a wave.
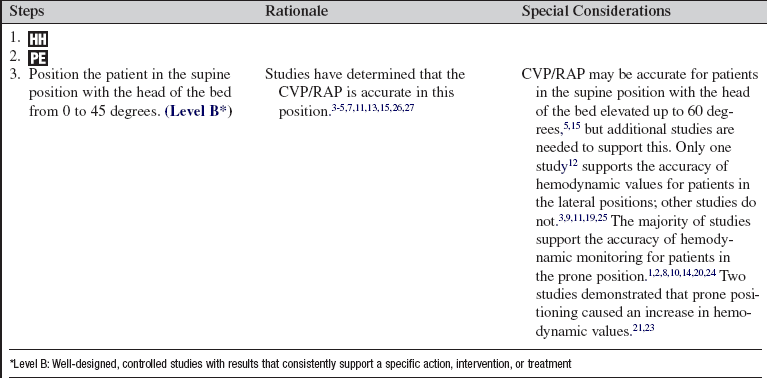
• CVP/RAP values are useful in evaluation of volume status, effect of medication therapy (especially medication that decreases preload), and cardiac function (Table 70-1).
Table 70-1
Conditions Causing Increased CVP
Elevated intravascular volume
Depressed right-sided cardiac function (RV infarct, RV failure)
Cardiac tamponade
Constrictive pericarditis
Pulmonary hypertension
Chronic left ventricular failure
Conditions Causing Decreased CVP
Reduced intravascular volume*
Decreased mean arterial pressure (MAP)
Venodilation
*Although the measured CVP is low, cardiac function may be depressed, normal, or hyperdynamic when there is reduced vascular volume.
• Monitoring parameters from the femoral catheter is not recommended. The catheter is too distant from the right atrium to produce reliable data.
EQUIPMENT
• Pressure transducer system, including flush solution recommended according to institution standard, a pressure bag or device, pressure tubing with transducer, and flush device (see Procedure 76)
• Pressure module and cable for interface with the monitor
Additional equipment to have available as needed includes the following:
PATIENT AND FAMILY EDUCATION
• Discuss the purpose of the central venous catheter and monitoring with both the patient and family.  Rationale: This discussion reduces anxiety and includes the patient and family in the plan of care.
Rationale: This discussion reduces anxiety and includes the patient and family in the plan of care.
• Explain the patient’s expected participation during the procedure.  Rationale: The explanation encourages patient assistance.
Rationale: The explanation encourages patient assistance.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Determine hemodynamic, cardiovascular, and peripheral vascular status.  Rationale: This assessment provides baseline data.
Rationale: This assessment provides baseline data.
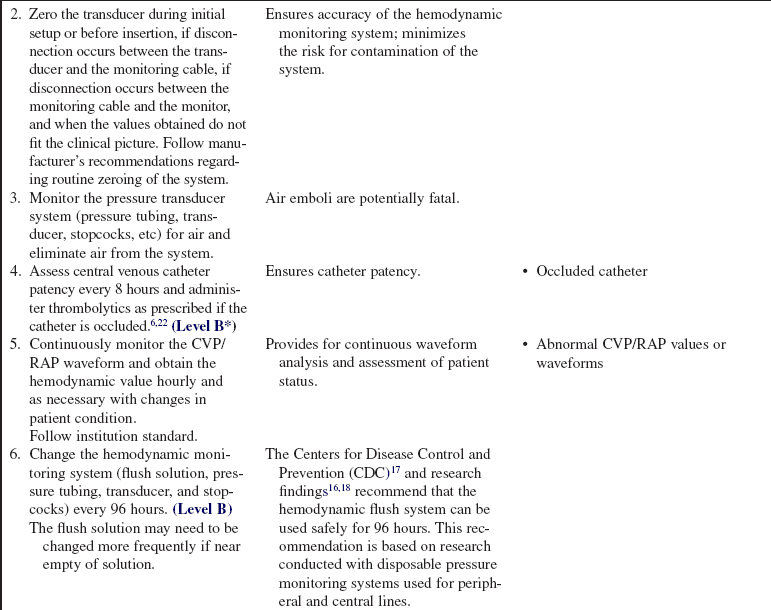
• Determine the patient’s baseline pulmonary status. If the patient is mechanically ventilated, note the type of support, ventilator mode, and presence or absence of positive end-expiratory pressure (PEEP) or continuous positive airway pressure (CPAP).  Rationale: The presence of mechanical ventilation alters hemodynamic waveforms and pressures.
Rationale: The presence of mechanical ventilation alters hemodynamic waveforms and pressures.
• Assess for signs and symptoms of fluid volume deficit. Signs and symptoms may include thirst, oliguria, tachycardia, and dry mucous membranes.  Rationale: Assessment data should correlate with a decreased CVP/RAP value.
Rationale: Assessment data should correlate with a decreased CVP/RAP value.
• Assess for signs and symptoms of fluid volume excess. Signs and symptoms may include dyspnea, abnormal breath sounds (i.e., crackles), S3 heart sound, peripheral edema, tachycardia, and jugular vein distention.  Rationale: Assessment data should correlate with an increased CVP/RAP value.
Rationale: Assessment data should correlate with an increased CVP/RAP value.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of previously taught information is evaluated and reinforced.
Rationale: Understanding of previously taught information is evaluated and reinforced.
• Place the patient in the supine position with the head of the bed flat or elevated up to 45 degrees.  Rationale: This positioning prepares the patient for hemodynamic monitoring.
Rationale: This positioning prepares the patient for hemodynamic monitoring.
References
![]() 1. Blanch, L, et al. Short-term effect of prone position in critically ill patients with acute respiratory distress syndrome. Intensive Care Med. 1997; 23:1003–1039.
1. Blanch, L, et al. Short-term effect of prone position in critically ill patients with acute respiratory distress syndrome. Intensive Care Med. 1997; 23:1003–1039.
![]() 2. Brussel, T, et al. Mechanical ventilation in the prone position for acute respiratory failure after cardiac surgery. J Cardiothorac Vasc Anesth. 1993; 7:541–546.
2. Brussel, T, et al. Mechanical ventilation in the prone position for acute respiratory failure after cardiac surgery. J Cardiothorac Vasc Anesth. 1993; 7:541–546.
![]() 3. Cason, CL, et al. Effects of backrest elevation and position on pulmonary artery pressures. Cardiovasc Nurs. 1990; 26:1–5.
3. Cason, CL, et al. Effects of backrest elevation and position on pulmonary artery pressures. Cardiovasc Nurs. 1990; 26:1–5.
![]() 4. Chulay, M, Miller, T. The effect of backrest elevation on pulmonary artery and pulmonary capillary wedge pressures in patients after cardiac surgery. Heart Lung. 1984; 13:138–140.
4. Chulay, M, Miller, T. The effect of backrest elevation on pulmonary artery and pulmonary capillary wedge pressures in patients after cardiac surgery. Heart Lung. 1984; 13:138–140.
![]() 5. Clochesy, J, Hinshaw, AD, Otto, CW. Effects of change of position on pulmonary artery and pulmonary capillary wedge pressure in mechanically ventilated patients. NITA. 1984; 7:223–225.
5. Clochesy, J, Hinshaw, AD, Otto, CW. Effects of change of position on pulmonary artery and pulmonary capillary wedge pressure in mechanically ventilated patients. NITA. 1984; 7:223–225.
![]() 6. Deitcher, SR, et al, Safety and efficacy of alteplase for restoring function in occluded central venous catheters . results of the cardiovascular thrombolytic to open occluded lines trial. J Clin Oncol 2002; 20:317–324.
6. Deitcher, SR, et al, Safety and efficacy of alteplase for restoring function in occluded central venous catheters . results of the cardiovascular thrombolytic to open occluded lines trial. J Clin Oncol 2002; 20:317–324.
![]() 7. Dobbin, K, et al, Pulmonary artery pressure measurement in patients with elevated pressures. effect of backrest elevation and method of measurement. Am J Crit Care 1992; 1:61–69.
7. Dobbin, K, et al, Pulmonary artery pressure measurement in patients with elevated pressures. effect of backrest elevation and method of measurement. Am J Crit Care 1992; 1:61–69.
![]() 8. Fridrich, P, et al. The effects of long-term prone positioning in patients with trauma-induced adult respiratory distress syndrome. Anesth Analg. 1996; 83:1206–1211.
8. Fridrich, P, et al. The effects of long-term prone positioning in patients with trauma-induced adult respiratory distress syndrome. Anesth Analg. 1996; 83:1206–1211.
![]() 9. Groom, L, Frisch, SR, Elliot, M. Reproducibility and accuracy of pulmonary artery pressure measurement in supine and lateral positions. Heart Lung. 1990; 19:147–151.
9. Groom, L, Frisch, SR, Elliot, M. Reproducibility and accuracy of pulmonary artery pressure measurement in supine and lateral positions. Heart Lung. 1990; 19:147–151.
![]() 10. Jolliet, P, Bulpa, P, Chevrolet, JC. Effects of prone position on gas exchange and hemodynamics in severe acute respiratory distress syndrome. Crit Care Med. 1998; 26:1977–1985.
10. Jolliet, P, Bulpa, P, Chevrolet, JC. Effects of prone position on gas exchange and hemodynamics in severe acute respiratory distress syndrome. Crit Care Med. 1998; 26:1977–1985.
![]() 11. Keating, D, et al. Effect of sidelying positions on pulmonary artery pressures. Heart Lung. 1986; 15:605–610.
11. Keating, D, et al. Effect of sidelying positions on pulmonary artery pressures. Heart Lung. 1986; 15:605–610.
![]() 12. Kennedy, GT, Bryant, A, Crawford, MH. The effects of lateral body positioning on measurements of pulmonary artery and pulmonary wedge pressures. Heart Lung. 1984; 13:155–158.
12. Kennedy, GT, Bryant, A, Crawford, MH. The effects of lateral body positioning on measurements of pulmonary artery and pulmonary wedge pressures. Heart Lung. 1984; 13:155–158.
![]() 13. Lambert, CW, Cason, CL, Backrest elevation and pulmonary artery pressures. research analysis. Dimens Crit Care Nurs 1990; 9:327–335.
13. Lambert, CW, Cason, CL, Backrest elevation and pulmonary artery pressures. research analysis. Dimens Crit Care Nurs 1990; 9:327–335.
![]() 14. Langer, M, et al. The prone position in ARDS patients. Chest. 1982; 94:103–107.
14. Langer, M, et al. The prone position in ARDS patients. Chest. 1982; 94:103–107.
![]() 15. Laulive, JL. Pulmonary artery pressures and position changes in the critically ill adult. Dimens Crit Care Nurs. 1982; 1:28–34.
15. Laulive, JL. Pulmonary artery pressures and position changes in the critically ill adult. Dimens Crit Care Nurs. 1982; 1:28–34.
![]() 16. Luskin, RL, et al, Extended use of disposable pressure transducers. a bacteriologic evaluation. JAMA 1986; 255:916–920.
16. Luskin, RL, et al, Extended use of disposable pressure transducers. a bacteriologic evaluation. JAMA 1986; 255:916–920.
![]() 17. O’Grady, NP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.
17. O’Grady, NP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.
![]() 18. O’Malley, MK, et al. Value of routine pressure monitoring system changes after 72 hours of use. Crit Care Med. 1994; 22:1424–1430.
18. O’Malley, MK, et al. Value of routine pressure monitoring system changes after 72 hours of use. Crit Care Med. 1994; 22:1424–1430.
![]() 19. Osida, C, Measurement of pulmonary artery pressures . supine verses side-lying head elevated positions. Heart Lung 1989; 18:298–299.
19. Osida, C, Measurement of pulmonary artery pressures . supine verses side-lying head elevated positions. Heart Lung 1989; 18:298–299.
![]() 20. Pappert, D, et al. Influence of positioning on ventilation-perfusion relationships in severe adult respiratory distress syndrome. Chest. 1994; 106:1511–1516.
20. Pappert, D, et al. Influence of positioning on ventilation-perfusion relationships in severe adult respiratory distress syndrome. Chest. 1994; 106:1511–1516.
![]() 21. Pelosi, P, et al. Effects of the prone position on respiratory mechanics and gas exchange during acute lung injury. Am J Respir Crit Care Med. 1998; 157:387–393.
21. Pelosi, P, et al. Effects of the prone position on respiratory mechanics and gas exchange during acute lung injury. Am J Respir Crit Care Med. 1998; 157:387–393.
![]() 22. Ponec, D, et al, Recombinant tissue plasminogen activator (Alteplase) for restoration of flow in occluded central venous access devices. a double-blind placebo-controlled trialthe cardiovascular thrombolytic to open occluded lines (COOL) efficacy trial. J Vasc Interv Radiol 2001; 12:951–955.
22. Ponec, D, et al, Recombinant tissue plasminogen activator (Alteplase) for restoration of flow in occluded central venous access devices. a double-blind placebo-controlled trialthe cardiovascular thrombolytic to open occluded lines (COOL) efficacy trial. J Vasc Interv Radiol 2001; 12:951–955.
![]() 23. Voggenreiter, G, et al. Intermittent prone positioning in the treatment of severe and moderate posttraumatic lung injury. Crit Care Med. 1999; 27:2375–2382.
23. Voggenreiter, G, et al. Intermittent prone positioning in the treatment of severe and moderate posttraumatic lung injury. Crit Care Med. 1999; 27:2375–2382.
![]() 24. Vollman, KM, Bander, JJ. Improved oxygenation utilizing a prone positioner in patients with acute respiratory distress syndrome. Intensive Care Med. 1996; 22:1105–1111.
24. Vollman, KM, Bander, JJ. Improved oxygenation utilizing a prone positioner in patients with acute respiratory distress syndrome. Intensive Care Med. 1996; 22:1105–1111.
![]() 25. Wild, L. Effect of lateral recumbent positions on measurement of pulmonary artery and pulmonary artery wedge pressures in critically ill adults. Heart Lung. 1984; 13:305.
25. Wild, L. Effect of lateral recumbent positions on measurement of pulmonary artery and pulmonary artery wedge pressures in critically ill adults. Heart Lung. 1984; 13:305.
![]() 26. Wilson, AE, et al. Effect of backrest position on hemodynamic and right ventricular measurements in critically ill adults. Am J Crit Care. 1996; 5:264–270.
26. Wilson, AE, et al. Effect of backrest position on hemodynamic and right ventricular measurements in critically ill adults. Am J Crit Care. 1996; 5:264–270.
![]() 27. Woods, SL, Mansfield, LW. Effect of body position upon pulmonary artery and pulmonary capillary wedge pressures in noncritically ill patients. Heart Lung. 1976; 5:83–90.
27. Woods, SL, Mansfield, LW. Effect of body position upon pulmonary artery and pulmonary capillary wedge pressures in noncritically ill patients. Heart Lung. 1976; 5:83–90.
Bridges, EJ, Pulmonary artery pressure monitoring. when, how, and what else to use. AACN Adv Crit Care 2006; 17:286–305.
Darovic, GO, Hemodynamic monitoring. invasive and noninvasive clinical application. ed 3. Saunders, Philadelphia, 2002.
Keckeisen, M, Protocols for practice. hemodynamic monitoring seriespulmonary artery pressure monitoring. American Association of Critical-Care Nurses, Aliso Viejo, CA, 1997.
Magder, S, Invasive intravascular hemodynamic monitoring. technical issues. Crit Care Clin 2007; 23:401–414.