Laryngeal Mask Airway
Laryngeal Mask Airway
A laryngeal mask airway may be used to provide an emergency airway during resuscitation of a profoundly unconscious patient who needs artificial ventilation when endotracheal intubation is not readily available or has failed in establishing an airway.1
PREREQUISITE NURSING KNOWLEDGE
• The requirement for rapid airway management in an unconscious patient should be understood.
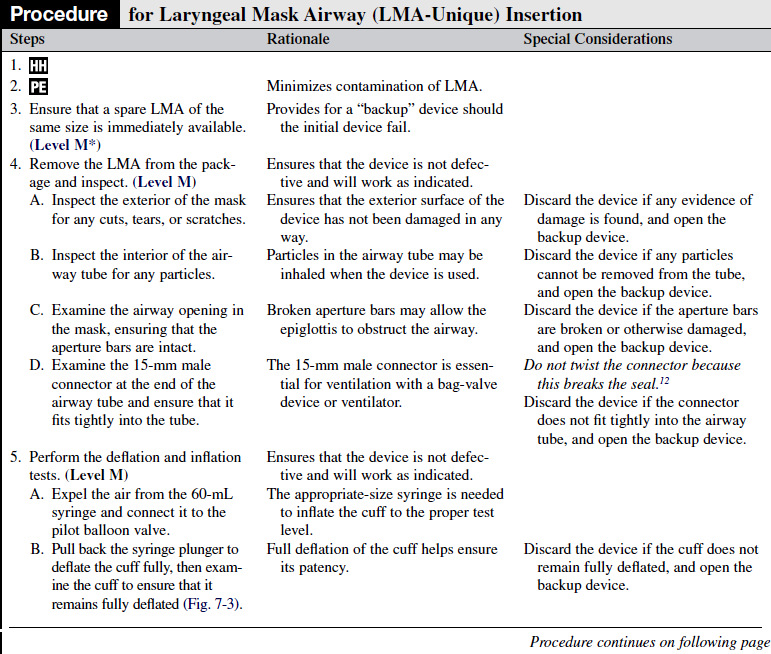
• The anatomy and physiology of the upper airway should be understood.
• The design of the laryngeal mask airway (LMA) available to the practitioner should be understood (Fig. 7-1):
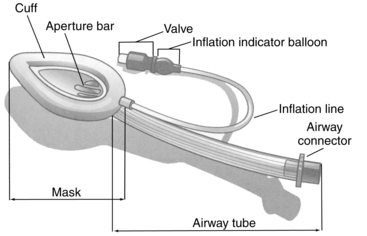
Figure 7-1 Components of the laryngeal mask airway. (From The Laryngeal Mask Company Limited: Instruction manual: LMA-Classic, San Diego, 2005, LMA.)
 An airway tube connects the mask and the 15-mm male adapter.
An airway tube connects the mask and the 15-mm male adapter.
 The mask’s cuff, when inflated, conforms to the contours of the hypopharynx, with the opening of the air tube positioned directly over the laryngeal opening. Two aperture bars cross the opening where the tube exits into the mask.
The mask’s cuff, when inflated, conforms to the contours of the hypopharynx, with the opening of the air tube positioned directly over the laryngeal opening. Two aperture bars cross the opening where the tube exits into the mask.
 An inflation line is fitted with a valve and a pilot balloon that leads to the mask’s cuff.
An inflation line is fitted with a valve and a pilot balloon that leads to the mask’s cuff.
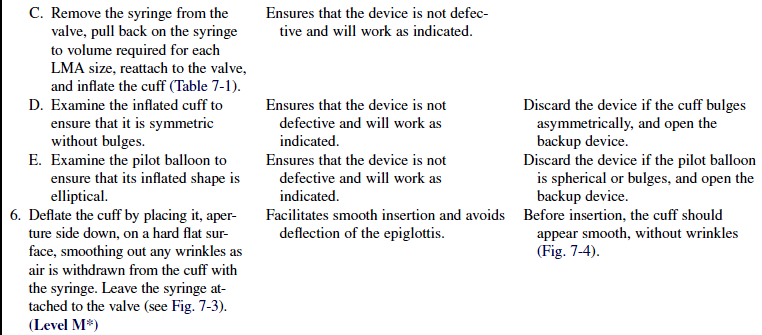
• The final placement of an LMA in the airway should be understood (Fig. 7-2).
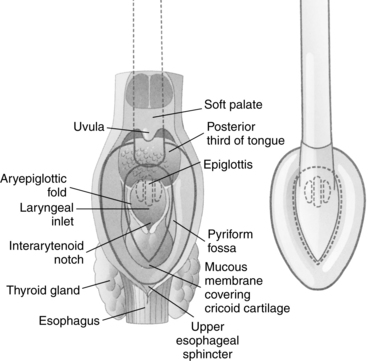
Figure 7-2 Dorsal view of the laryngeal mask airway showing position in relation to pharyngeal anatomy. (From The Laryngeal Mask Company Limited: Instruction manual: LMA-Classic, San Diego, 2005, LMA.)
• The ability to ventilate an unconscious patient adequately with a mouth-to-mask or bag-valve-mask device is necessary.
• An understanding of the limitations of the LMA is needed. Limitations are as follows:
 The LMA does not protect the airway from aspiration of stomach contents, and the risks of insertion and aspiration must be weighed against the need to establish an airway.12
The LMA does not protect the airway from aspiration of stomach contents, and the risks of insertion and aspiration must be weighed against the need to establish an airway.12
v The presence of a nasogastric tube may make regurgitation more likely because of its effect on the esophageal sphincter tone and may also prevent the LMA from properly sealing the hypopharynx.12,13
 The LMA should not be used on patients who need high ventilator pressures (e.g., patients with pulmonary fibrosis, significant obesity) because the LMA provides a low-pressure seal.12
The LMA should not be used on patients who need high ventilator pressures (e.g., patients with pulmonary fibrosis, significant obesity) because the LMA provides a low-pressure seal.12
 The LMA should not be used in an emergency situation in which the patient is not profoundly unconscious and may resist insertion of the device.12
The LMA should not be used in an emergency situation in which the patient is not profoundly unconscious and may resist insertion of the device.12
 The LMA should be used with caution in patients with oropharyngeal trauma, only when all other means of establishing an airway fail1 and when the risks of insertion are weighed against the need to establish an airway.
The LMA should be used with caution in patients with oropharyngeal trauma, only when all other means of establishing an airway fail1 and when the risks of insertion are weighed against the need to establish an airway.
 The LMA can cause local irritation that leads to coughing and pressure lesions, which may cause 12th cranial nerve palsy.2
The LMA can cause local irritation that leads to coughing and pressure lesions, which may cause 12th cranial nerve palsy.2
• There are no absolute contraindications to the LMA if the alternative is loss of the airway with its associated complications.6
• The LMA may provide a more viable means of ventilation than a self-inflating manual resuscitation bag-valve-mask device in patients with a beard or without teeth.11
• Initial and ongoing training is necessary to maximize insertion success and minimize complications.8,11
• This procedure refers specifically to the LMA-Unique, a disposable model of the nondisposable LMA-Classic. Other types of LMA devices are available and provide additional features, such as endotracheal intubation through the LMA or gastric suctioning.
EQUIPMENT
• Two LMA-Unique devices of the appropriate size for patient weight3
 Weight ranges listed for LMA-Unique sizes are only approximations; the size used may need to be adjusted for individual body habitus variations (i.e., patients who are short and obese may need a smaller size). Emerging clinical data suggest that use of a larger size provides an effective seal without associated higher pharyngeal pressures.3,7
Weight ranges listed for LMA-Unique sizes are only approximations; the size used may need to be adjusted for individual body habitus variations (i.e., patients who are short and obese may need a smaller size). Emerging clinical data suggest that use of a larger size provides an effective seal without associated higher pharyngeal pressures.3,7
• Gloves, mask, and eye protection
• Suction equipment (suction canister with control head, tracheal suction catheters, Yankauer suction tip)
• Mouth-to-mask or self-inflating manual resuscitation bag-valve-mask device, with peak pressure manometer, attached to a high-flow oxygen source
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Assess level of consciousness and responsiveness.  Rationale: In an emergency situation, the LMA should be inserted only into a patient who is profoundly unconscious and unresponsive.12 Laryngospasm and inability to ventilate may occur if an LMA is introduced into a conscious or semiconscious patient.
Rationale: In an emergency situation, the LMA should be inserted only into a patient who is profoundly unconscious and unresponsive.12 Laryngospasm and inability to ventilate may occur if an LMA is introduced into a conscious or semiconscious patient.
• Assess history and patient information for possibility of delayed gastric emptying (e.g., hiatal hernia, recent food ingestion, poorly controlled diabetes).  Rationale: In a patient with delayed gastric emptying, the benefits of LMA insertion must be weighed against the possibility of regurgitation.12
Rationale: In a patient with delayed gastric emptying, the benefits of LMA insertion must be weighed against the possibility of regurgitation.12
• Assess history and patient information for possibility of decreased pulmonary compliance (i.e., pulmonary fibrosis, obesity).  Rationale: The high pressures needed to ventilate a patient with decreased pulmonary compliance may override the occlusive pressure of the LMA.12
Rationale: The high pressures needed to ventilate a patient with decreased pulmonary compliance may override the occlusive pressure of the LMA.12
Patient Preparation
• Perform a pre-procedure verification and time out, if non-emergent.  Rationale: Ensures patient safety.
Rationale: Ensures patient safety.
• Ensure adequate ventilation and oxygenation with either a mouth-to-mask or bag-valve-mask device.  Rationale: The patient is nonresponsive and apneic without assisted ventilation before the LMA insertion.
Rationale: The patient is nonresponsive and apneic without assisted ventilation before the LMA insertion.
• Ensure that the suction equipment is assembled and in working order.  Rationale: The patient may regurgitate during the insertion or while the LMA is in place and need oropharyngeal or tracheal suctioning.
Rationale: The patient may regurgitate during the insertion or while the LMA is in place and need oropharyngeal or tracheal suctioning.
• Anything that is not permanently affixed in the patient’s mouth (e.g., dentures, partials, jewelry) should be removed.  Rationale: Inadvertent dislodgment and aspiration might occur with the placement of the LMA.
Rationale: Inadvertent dislodgment and aspiration might occur with the placement of the LMA.
Table 7-1
| Laryngeal Mask Airway Size | Air Volume for Testing Only |
| 3 | 30 mL |
| 4 | 45 mL |
| 5 | 60 mL |
| 6 | 75 mL |
(From The Laryngeal Mask Company Limited: Instruction manual: LMA-Classic, San Diego, 2005, LMA.)
Table 7-2
Maximal Cuff Inflation Volumes
| Laryngeal Mask Airway Size | Cuff Inflation Volume |
| 3 | 20 mL |
| 4 | 30 mL |
| 5 | 40 mL |
| 6 | 50 mL |
(From The Laryngeal Mask Company Limited:Instruction manual: LMA-Classic, San Diego, 2005, LMA.)
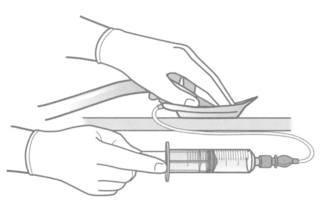
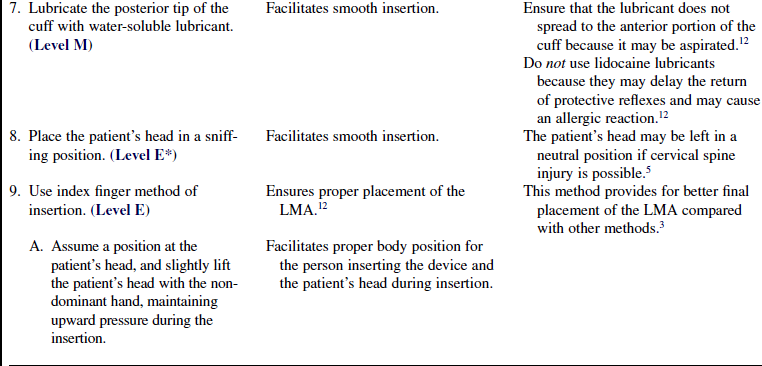
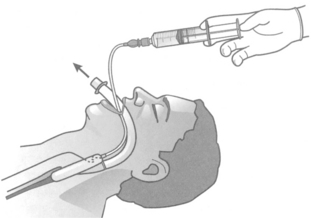
Figure 7-3 Method for deflating the laryngeal mask airway cuff. (From The Laryngeal Mask Company Limited: Instruction manual: LMA-Classic, San Diego, 2005, LMA.)
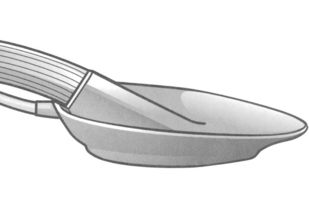
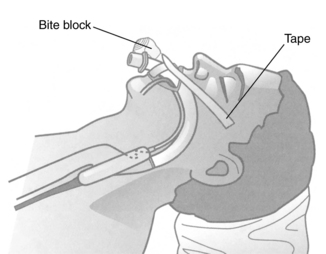
Figure 7-4 Laryngeal mask airway cuff properly deflated for insertion. (From The Laryngeal Mask Company Limited: Instruction manual: LMA-Classic, San Diego, 2005, LMA.)
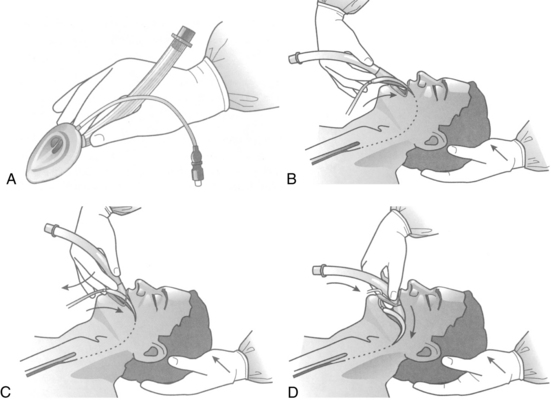
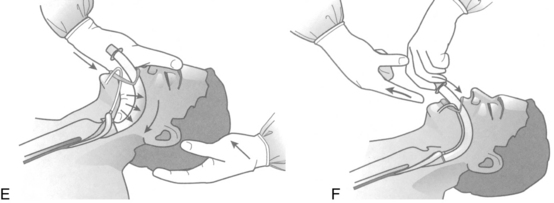
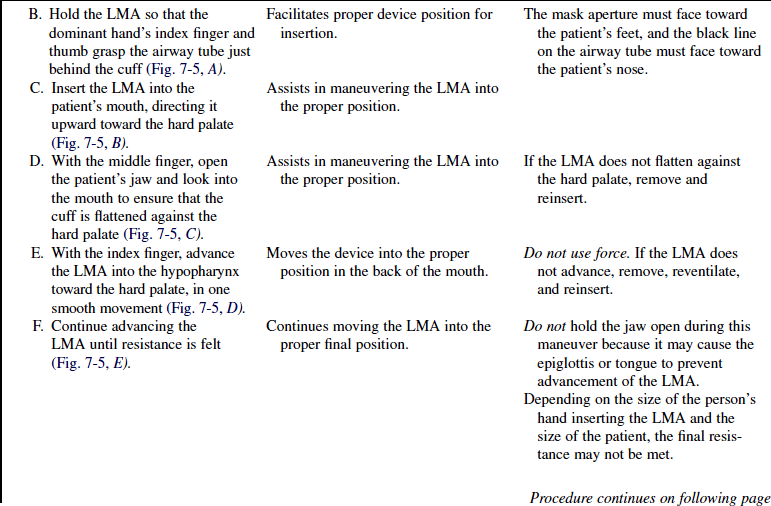
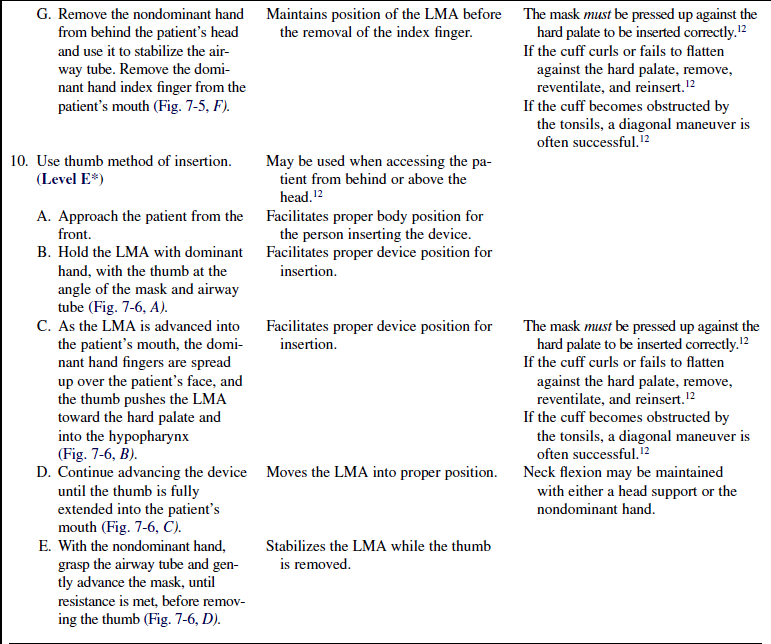
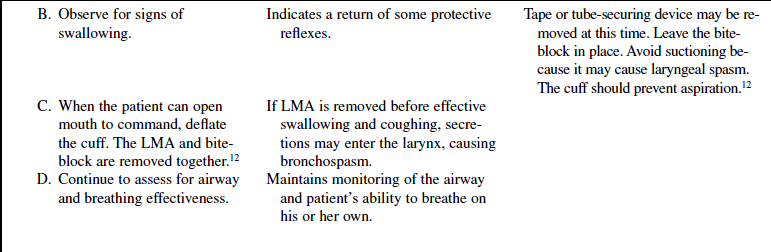
Figure 7-5 A, Method for holding the LMA for insertion. B, With the head extended and the neck flexed, the caregiver carefully flattens the LMA tip against the hard palate. C, To facilitate LMA introduction into the oral cavity, the caregiver gently presses the middle finger down on the jaw. D, The index finger pushes the LMA in the cranial direction following the contours of the hard and soft palates. E, Maintaining pressure with the finger in the tube in the cranial direction, the caregiver advances the LMA until definite resistance is felt at the base of the hypopharynx. Note the flexion of the wrist. F, The caregiver gently maintains cranial pressure with the nondominant hand while removing the index finger. (From The Laryngeal Mask Company Limited: Instruction manual: LMA-Classic, San Diego, 2005, LMA.)
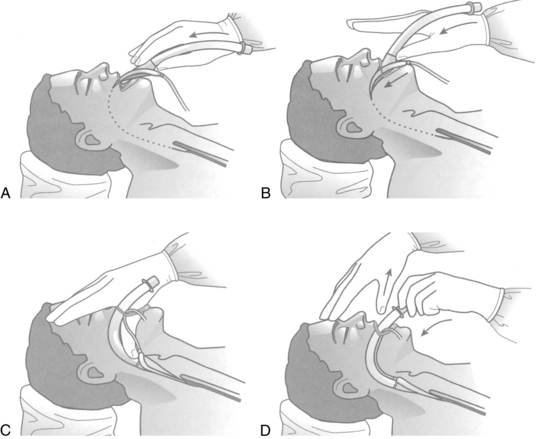
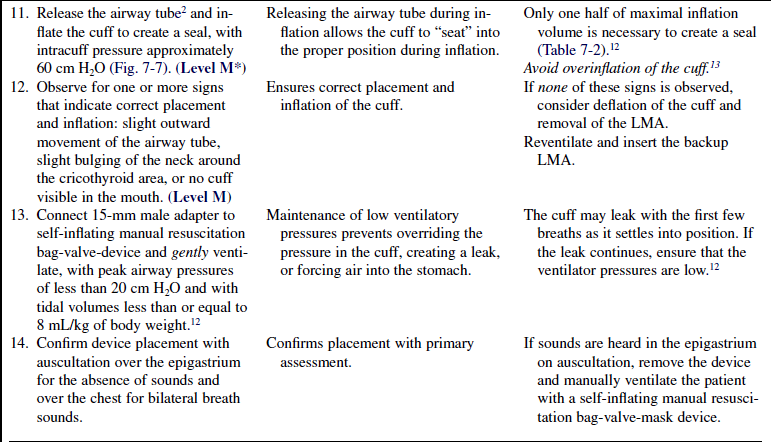
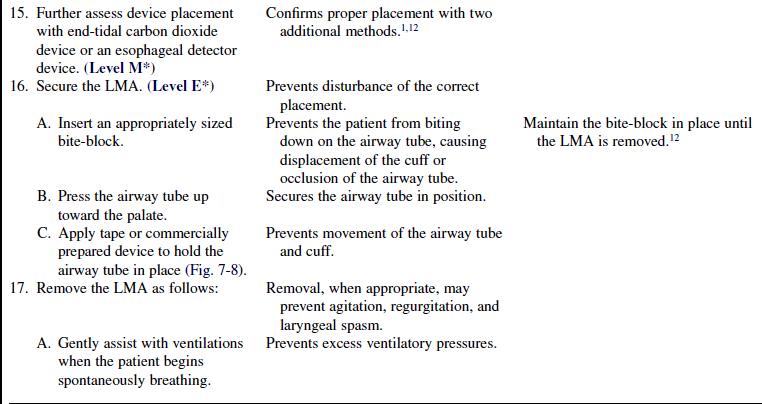
Figure 7-6 A, Method for holding the LMA for thumb insertion. B, With the fingers extended, press the thumb along the posterior pharynx. C, Advance the thumb to its fullest extent. D, Press LMA gently into place with the nondominant hand while removing the thumb. (From The Laryngeal Mask Company Limited: Instruction manual: LMA-Classic, San Diego, 2005, LMA.)
References
1. American Heart Association. Advanced cardiac life support (ACLS). Dallas: AHA; 2006.
![]() 2. Birnbaumer, D, Pollack, C, Jr. Troubleshooting and managing the difficult airway. Semin Respir Crit Care Med. 2002; 23(1):3–9.
2. Birnbaumer, D, Pollack, C, Jr. Troubleshooting and managing the difficult airway. Semin Respir Crit Care Med. 2002; 23(1):3–9.
![]() 3. Brimacombe, J, Berry, A, Insertion of the laryngeal mask airway. a prospective study of four techniques. Anaesth Intensive Care 1993; 21:89–92.
3. Brimacombe, J, Berry, A, Insertion of the laryngeal mask airway. a prospective study of four techniques. Anaesth Intensive Care 1993; 21:89–92.
4. Duk-Kyung, K, et al. A heated humidifier does not reduce laryngo-pharyngeal complaints after brief laryngeal mask anesthesia. Can J Anesthesia. 2007; 54:134–140.
![]() 5. Hand, H, Cardiopulmonary resuscitation. the laryngeal mask airway. Emerg Nurse 2002; 10:31–37.
5. Hand, H, Cardiopulmonary resuscitation. the laryngeal mask airway. Emerg Nurse 2002; 10:31–37.
![]() 6. Idris, AH, Gabrielli, A. Advances in airway management. Emerg Med Clin North Am. 2002; 20:843–857.
6. Idris, AH, Gabrielli, A. Advances in airway management. Emerg Med Clin North Am. 2002; 20:843–857.
7. LMA, Inc. LMA. www.lmana.com/faqs.php#faq06, 2008. [retrieved February 25, 2009. from].
8. Lopez, AM, et al. A clinical evaluation of four disposable laryngeal masks in adult patients. J Clin Anesth. 2008; 20(7):508–513.
![]() 9. Ocker, H. A comparison of the laryngeal tube with the laryngeal mask airway during routine surgical procedures. Anesth Analg. 2002; 95(4):1094–1097.
9. Ocker, H. A comparison of the laryngeal tube with the laryngeal mask airway during routine surgical procedures. Anesth Analg. 2002; 95(4):1094–1097.
10. Radu, AD, et al, Pharyngo-laryngeal discomfort after breast surgery. comparison between orotracheal intubation and laryngeal mask. Breast. 2008; 17(4):407–411.
![]() 11. Shuster, M, Nolan, J, Barnes, TA. Airway and ventilation management. Emerg Cardiovasc Care. 2002; 20:23–35.
11. Shuster, M, Nolan, J, Barnes, TA. Airway and ventilation management. Emerg Cardiovasc Care. 2002; 20:23–35.
12. The Laryngeal Mask Company Limited. LMA instruction manual. San Diego: LMA; 2005.
13. Ulrich-Pur H, et al. Comparison of mucosal pressures induced by cuffs of different airway devices. Anesthesiology. 2006; 104(5):933–938.
Bogetz, MS. Using the laryngeal mask airway to manage the difficult airway. Anesthesiol Clin North Am. 2002; 20:863–870.
Burns, SM. Safely caring for patients with a laryngeal mask airway. Crit Care Nurse. 2001; 21:72–74.
Gabrielli, A, et al. Alternative ventilation strategies in cardiopulmonary resuscitation. Curr Opin Crit Care. 2002; 8:199–211.
Maltby, JR, Loken, RG, Watson, NC, The laryngeal mask -airway. clinical appraisal in 250 patients. Can J Anesth 1990; 37:509–513.
Nolan, JD, Prehospital and resuscitative airway care. should the gold standard be reassessed. Curr Opin Crit Care 2001; 7:413–421.





 Rationale: This information assists the family in understanding why the procedure is necessary and decreases family anxiety.
Rationale: This information assists the family in understanding why the procedure is necessary and decreases family anxiety.