History
The patient is a 66-year-old woman who first came to medical attention for her heart disease 3 years ago. She had been on a cruise when she initially noticed some functional limitation. She began to have difficulty climbing the stairs and found it necessary to use the elevator. By the end of the cruise she had pedal edema to the midcalf and had to sleep semirecumbant because of shortness of breath while lying flat.
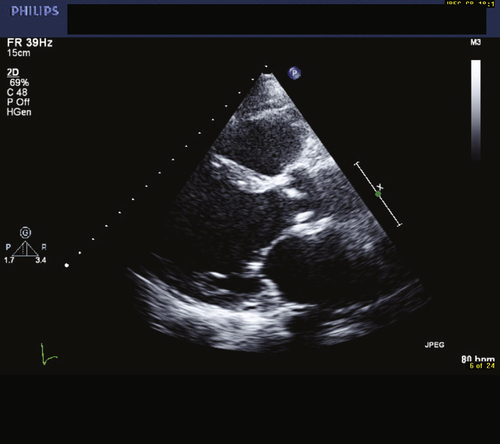
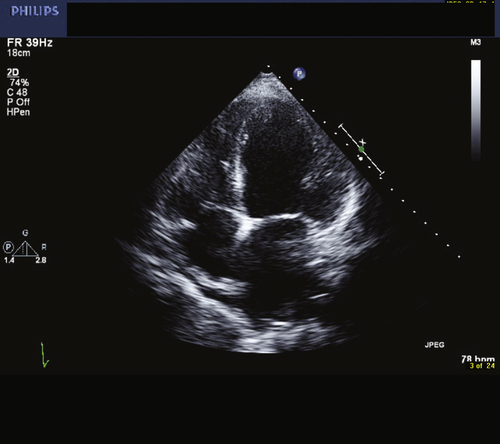
On her return home, she went to see her family doctor, who ordered an echocardiogram. This showed an ejection fraction of 20%. There was trivial mitral regurgitation. The left ventricular mass index was 153 g/m
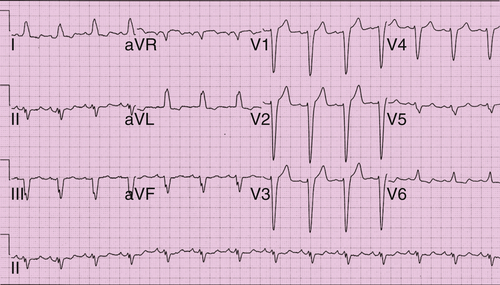
2. The left ventricular end-systolic and end-diastolic dimensions were 44 and 66 mm, respectively. An electrocardiogram (ECG) demonstrated normal sinus rhythm at 77 bpm with left bundle branch block (LBBB) and left axis deviation.
She was initially treated with a diuretic (furosemide [Lasix]) and an angiotensin-converting enzyme inhibitor (ramipril). When she became euvolemic a beta blocker was added (carvedilol) and titrated up to target doses.
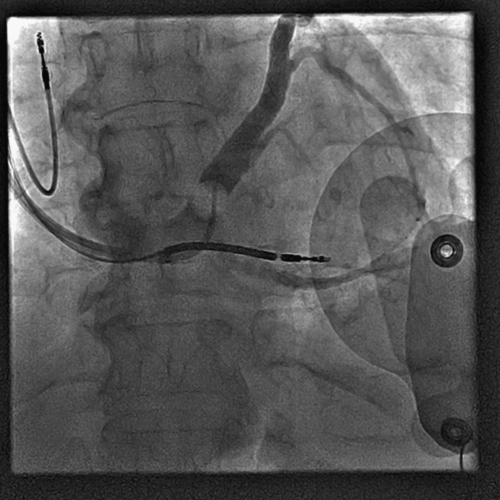
She underwent a coronary angiogram, which showed no evidence of flow-limiting coronary artery disease.
Her past medical history included smoking (she stopped smoking 3 years ago, after smoking one pack per day for 20 years). She had a history of breast cancer for which she was treated with chemotherapy (including doxorubicin) and radiation. She drinks 1 to 2 glasses of wine on weekend evenings. She has no family history of cardiomyopathy.
The workup for her heart failure revealed no evidence of human immunodeficiency virus, thyroid disease, hemochromatosis, or amyloidosis. She had no recent history of viral infection.
After 9 months of therapy a repeat echocardiogram was performed and showed an ejection fraction of 30%. Her symptoms had improved such that she denied any functional limitation. An exercise stress test was performed to assess her functional ability objectively. She performed a bicycle stress test and was able to perform 3.8 metabolic equivalents. This was deemed to be below expected for her age and gender.
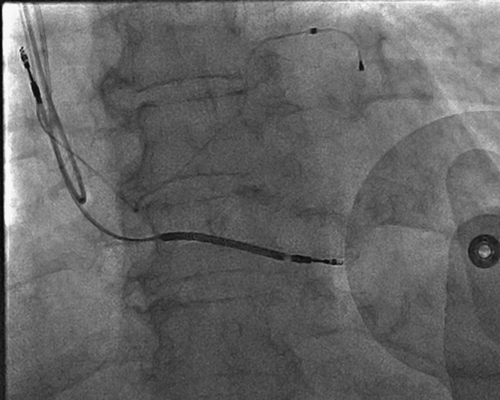
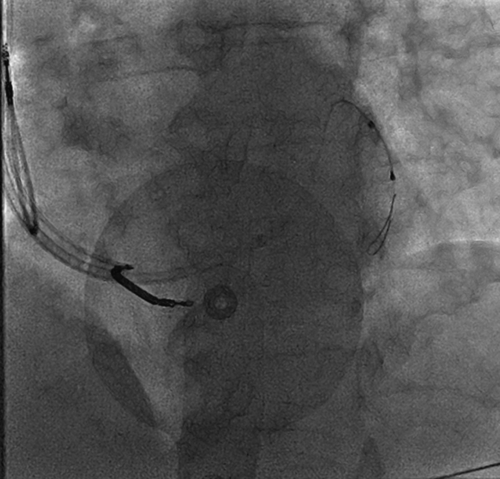
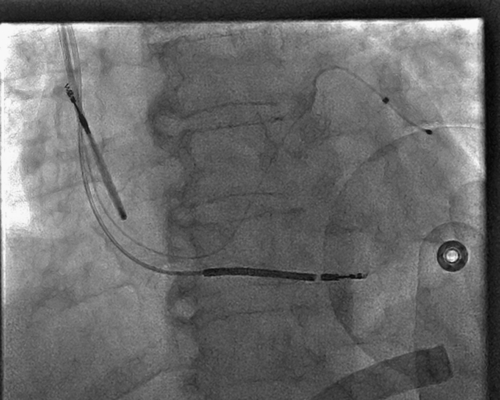
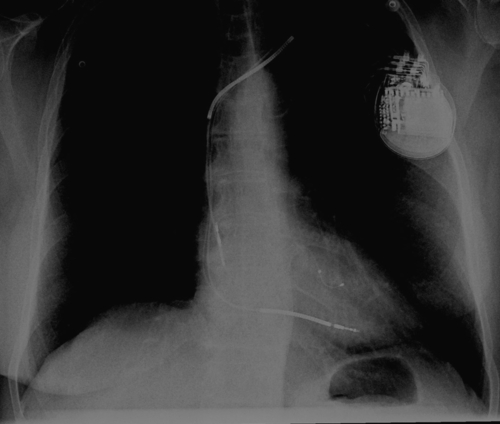
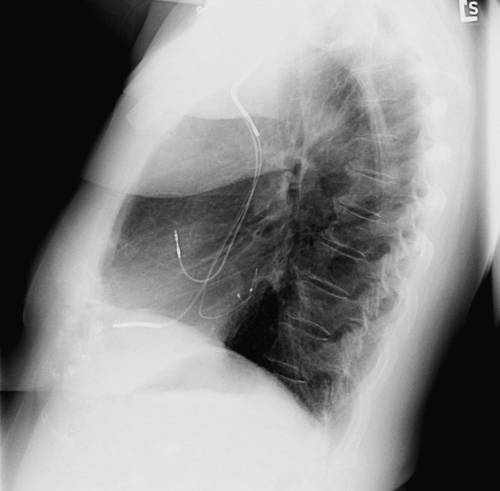
She was referred for a biventricular implantable cardioverter-defibrillator (ICD), but she initially refused because she felt well. During the subsequent 2 years she had one hospitalization for heart failure. At that time her weight was 5 kg over her usual dry weight. She was admitted for a total of 3 days and after intravenous diuretics was back to her baseline weight and functional status.
At a recent visit to the cardiac function clinic it was recommended again that she consider a cardiac resynchronization therapy defibrillator (CRT-D). She wished to discuss it further and was referred to a cardiac electrophysiologist.
Comments
This woman is a 66-year-old woman with nonischemic (presumably chemotherapy induced) cardiomyopathy. Although she denies functional limitation, her exercise stress test demonstrates mild functional limitation (New York Heart Association class II [NYHA]).
Current Medications
The patient takes ramipril 10 mg, carvedilol 25 mg, and spironolactone 12.5 mg in the morning and carvedilol 25 mg in the evening.
Comments
The patient appears to be on optimal medical therapy.
Current Symptoms
The patient currently denies orthopnea and paroxysmal nocturnal dyspnea. She is now able to walk eight blocks on the flat surfaces. However, she no longer rides her bike or does aerobics and she takes the elevator instead of the stairs when at the mall.
Comments
This patient has NYHA II heart failure symptoms despite medical therapy. Often, patients will habituate to their functional limitation and feel well. They may not realize that they have changed their lifestyle to accommodate the change in their functional decline.