Central Venous Catheter Removal
PREREQUISITE NURSING KNOWLEDGE
• Knowledge of the normal anatomy and physiology of the vasculature and cardiovascular system is necessary.
• Knowledge of normal coagulation values is needed.
• Principles of aseptic technique should be known.
• Advanced cardiac life support knowledge and skills are necessary.
• Clinical and technical competence in central venous catheter (CVC) removal is necessary.
• Knowledge of the state nurse practice act is important because some states do not allow this intervention to be performed by a registered nurse.
• Knowledge of potential complications associated with the removal of the CVC is needed.
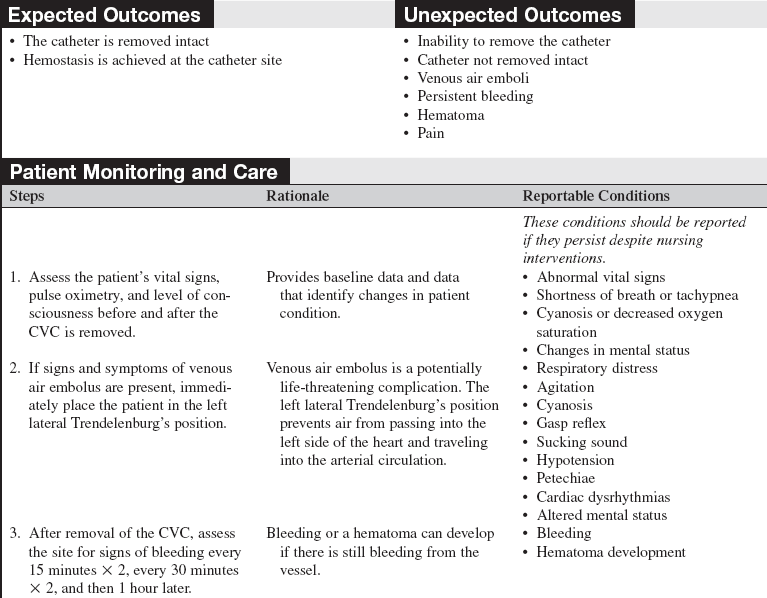
• An air embolism can occur during or after the removal of the catheter as a result of air drawn in along the subcutaneous tract and into the vein. During inspiration, negative intrathoracic pressure is transmitted to the central veins. Any opening external to the body to one of these veins may result in aspiration of air into the central venous system. The pathologic effects depend on the volume and rate of air aspirated. Signs and symptoms include: respiratory distress, agitation, cyanosis, gasp reflex, sucking sound, hypotension, petechiae, cardiac dysrhythmias, and altered mental status.
EQUIPMENT
• Face mask, sterile glows, nonsterile gloves
• Antiseptic solution (e.g., 2% chlorhexidine-based preparation)
Additional equipment to have as needed includes the following:
PATIENT AND FAMILY EDUCATION
• Explain the procedure to the patient and family and the reason for catheter removal.  Rationale: This explanation provides information and decreases anxiety.
Rationale: This explanation provides information and decreases anxiety.
• Explain the importance of the patient lying still during the catheter removal.  Rationale: This explanation ensures patient cooperation and facilitates safe removal of the catheter.
Rationale: This explanation ensures patient cooperation and facilitates safe removal of the catheter.
• Instruct the patient and family to report any signs and symptoms of shortness of breath, bleeding, or discomfort at the site of catheter removal.  Rationale: Identifies patient discomfort and early recognition of complications.
Rationale: Identifies patient discomfort and early recognition of complications.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess vital signs and the neurovascular status of the extremity distal to the catheter insertion site.  Rationale: This assessment provides baseline data.
Rationale: This assessment provides baseline data.
• Assess the patient’s current coagulation values.  Rationale: If the patient has abnormal coagulation study results, hemostasis may be difficult to obtain.
Rationale: If the patient has abnormal coagulation study results, hemostasis may be difficult to obtain.
• Assess the catheter site for redness, warmth, tenderness, or presence of drainage.  Rationale: Determines if signs or symptoms of infection are present.
Rationale: Determines if signs or symptoms of infection are present.
Patient Preparation
• In collaboration with the physician, determine when the CVC should be removed.  Rationale: The invasive catheter is removed when it is no longer indicated.
Rationale: The invasive catheter is removed when it is no longer indicated.
• In collaboration with the physician, determine whether the tip of the catheter will be cultured.  Rationale: This discussion determines additional supplies that may be needed.
Rationale: This discussion determines additional supplies that may be needed.
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand preprocedural teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of previously taught information is evaluated and reinforced.
Rationale: Understanding of previously taught information is evaluated and reinforced.
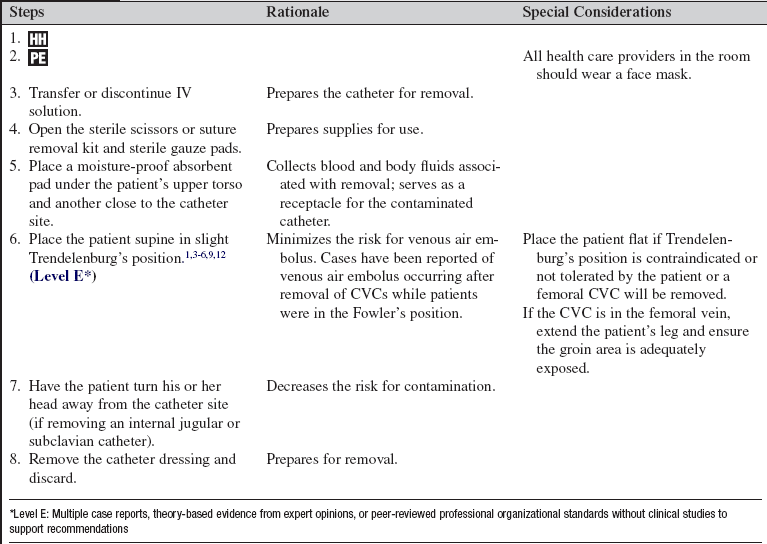
• Place the patient in a supine position with the head of the bed in a slight Trendelenburg’s position (or flat if Trendelenburg’s position is contraindicated or not tolerated by the patient).  Rationale: A normal pressure gradient exists between atmospheric air and the central venous compartment that promotes air entry if the compartment is open. Placing the patient in a head-down position decreases the risk of air being drawn into the venous circulation.
Rationale: A normal pressure gradient exists between atmospheric air and the central venous compartment that promotes air entry if the compartment is open. Placing the patient in a head-down position decreases the risk of air being drawn into the venous circulation.
• Start a new peripheral intravenous (IV) line or ensure that an existing peripheral IV line is patent.  Rationale: IV access is established for fluids or medications.
Rationale: IV access is established for fluids or medications.
References
![]() 1. Ely, EW, et al, Venous air embolism from central venous catheterization. a need for increased physician awareness. Crit Care Med 1999; 27:2113–2117.
1. Ely, EW, et al, Venous air embolism from central venous catheterization. a need for increased physician awareness. Crit Care Med 1999; 27:2113–2117.
![]() 2. Eyer, S, et al, Catheter-related sepsis. prospective, randomized study of three methods of long-term catheter maintainence. Crit Care Med 1990; 18:1073–1079.
2. Eyer, S, et al, Catheter-related sepsis. prospective, randomized study of three methods of long-term catheter maintainence. Crit Care Med 1990; 18:1073–1079.
![]() 3. Hsiung, GR, Swanson, PD. Cerebral air embolism after central venous catheter removal. Neurolgy. 2000; 55:1063–1064.
3. Hsiung, GR, Swanson, PD. Cerebral air embolism after central venous catheter removal. Neurolgy. 2000; 55:1063–1064.
![]() 4. Kim, DK, et al, The CVC removal distress syndrome. an unappreciated complication of central venous catheter removal. Am Surgeon 1998; 64:344–347.
4. Kim, DK, et al, The CVC removal distress syndrome. an unappreciated complication of central venous catheter removal. Am Surgeon 1998; 64:344–347.
![]() 5. McCarthy, PM, et al. Air embolism in single-lung transplant patients after central venous catheter removal. Chest. 1995; 107:1178–1179.
5. McCarthy, PM, et al. Air embolism in single-lung transplant patients after central venous catheter removal. Chest. 1995; 107:1178–1179.
![]() 6. Mennim, P, Cormac, FC, Taylor, JD. Venous air embolism associated with removal of central venous catheter. BMJ. 1992; 305:171–172.
6. Mennim, P, Cormac, FC, Taylor, JD. Venous air embolism associated with removal of central venous catheter. BMJ. 1992; 305:171–172.
![]() 7. O’Grady, NP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.
7. O’Grady, NP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.
8. Oztekin, DS, et al. Comparison of complications and procedural activities of pulmonary artery catheter removal by critical care nurses versus medical doctors. Nurs Crit Care. 2008; 13:105–115.
![]() 9. Pronovost, PJ, Wu, AW, Sexton, JB, Acute decompensation after removing a central line. practical approaches to increasing safety in the intensive care unit. Ann Intern Med 2004; 140:1025–1033.
9. Pronovost, PJ, Wu, AW, Sexton, JB, Acute decompensation after removing a central line. practical approaches to increasing safety in the intensive care unit. Ann Intern Med 2004; 140:1025–1033.
![]() 10. Rountree, WD, Removal of pulmonary artery catheters by registered nurses. a study in safety and complications. Focus Crit Care 1991; 18:313–318.
10. Rountree, WD, Removal of pulmonary artery catheters by registered nurses. a study in safety and complications. Focus Crit Care 1991; 18:313–318.
![]() 11. Safdar, N, Klugar, DM, Maki, DG, A review of risk factors for catheter-related bloodstream infection caused by percutaneously inserted, noncuffed central venous catheters. implications for preventive strategies . Medicine 2002; 81:466–472.
11. Safdar, N, Klugar, DM, Maki, DG, A review of risk factors for catheter-related bloodstream infection caused by percutaneously inserted, noncuffed central venous catheters. implications for preventive strategies . Medicine 2002; 81:466–472.
![]() 12. Turnage, WS, Harper, JV. Venous air embolism occurring after removal of a central venous catheter. Anesth Analg. 1991; 72:559–560.
12. Turnage, WS, Harper, JV. Venous air embolism occurring after removal of a central venous catheter. Anesth Analg. 1991; 72:559–560.
![]() 13. Wadas, TM. Pulmonary artery catheter removal. Crit Care Nurse. 1994; 14:62–72.
13. Wadas, TM. Pulmonary artery catheter removal. Crit Care Nurse. 1994; 14:62–72.