Blood Sampling from an Arterial Catheter
PREREQUISITE NURSING KNOWLEDGE
• Knowledge of aseptic and sterile technique is necessary.
• Knowledge of the vascular anatomy and physiology is needed.
• Understanding of gas exchange and acid-base balance is necessary.
• Technique for specimen collection and labeling should be understood.
• Principles of hemodynamic monitoring are necessary.
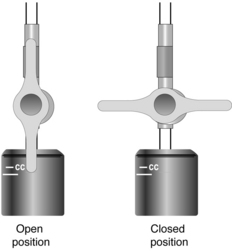
• Knowledge about the care of patients with arterial catheters (see Procedure 62) and stopcock manipulation (see Procedure 76) is needed.
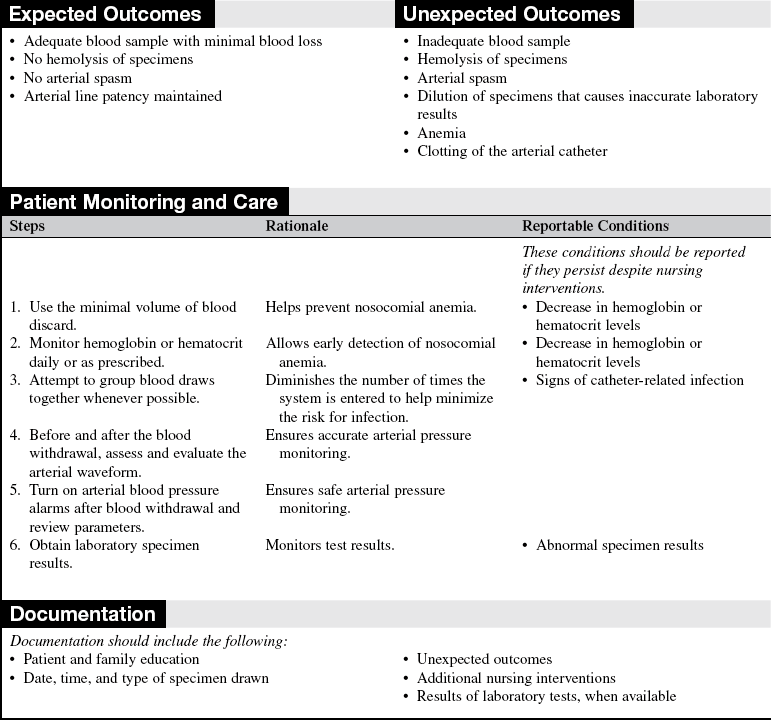
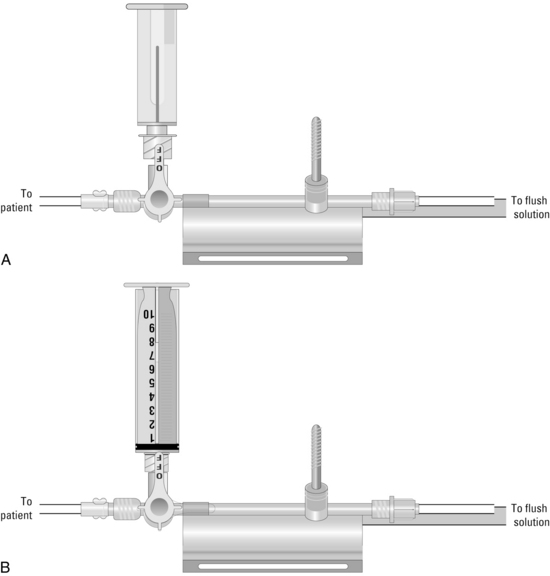
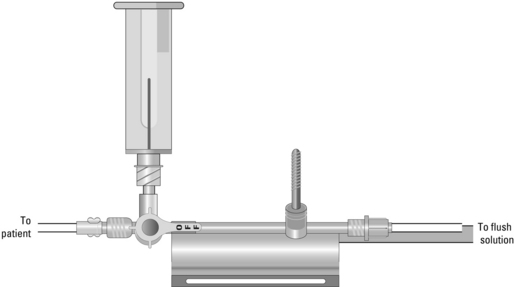
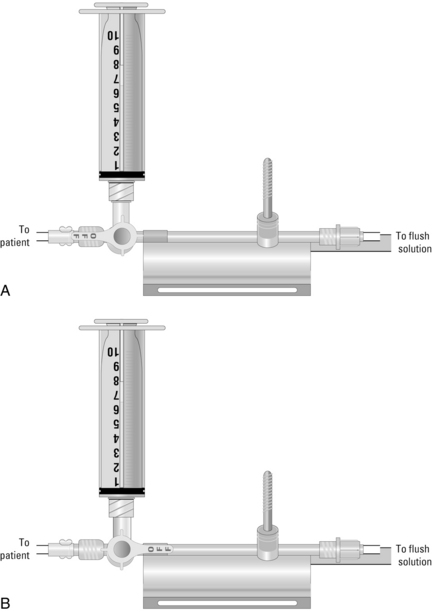
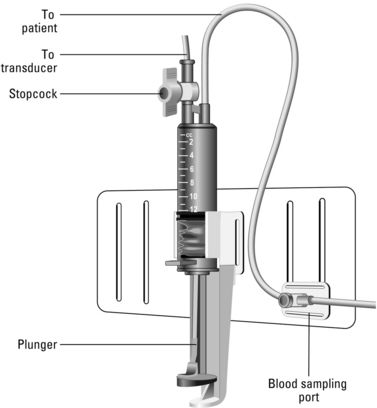
• Understanding of the closed arterial line blood sampling system is necessary.
• Closed blood sampling systems provide the opportunity to reinfuse the blood to the patient after the laboratory sample is obtained to help reduce the risk of nosocomial anemia.3,7,10,14,15
EQUIPMENT
• Appropriate blood specimen tubes (or arterial blood gas [ABG] kit)
• Labels with the patient’s name and appropriate identifying data
• Laboratory form and specimen labels
• Goggles or fluid shield face mask
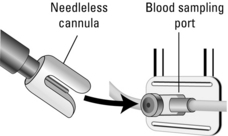
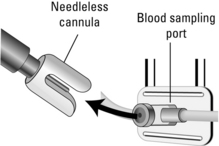
• Needleless blood sampling access device
• Extra blood specimen tube (for discard)
PATIENT ASSESSMENT AND PREPARATION
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand preprocedural teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of previously taught information is evaluated and reinforced.
Rationale: Understanding of previously taught information is evaluated and reinforced.
• Expose the stopcock to be used for blood sampling, and position the patient’s extremity so that the site can easily be accessed.  Rationale: This prepares the site for blood withdrawal.
Rationale: This prepares the site for blood withdrawal.
References
![]() 1. Casey, AL, et al. A randomized, prospective clinical trial to assess the potential infection risk associated with the PosiFlow needleless connector. J Hosp Infection. 2003; 54:288–293.
1. Casey, AL, et al. A randomized, prospective clinical trial to assess the potential infection risk associated with the PosiFlow needleless connector. J Hosp Infection. 2003; 54:288–293.
![]() 2. Darovic, GO, Arterial pressure monitoringInHemodynamic monitoring. invasive and noninvasive clinical -application. ed 3. Saunders, Philadelphia, 2002.
2. Darovic, GO, Arterial pressure monitoringInHemodynamic monitoring. invasive and noninvasive clinical -application. ed 3. Saunders, Philadelphia, 2002.
![]() 3. Gleason, E, Grossman, S, Campbell, C. Minimizing diagnostic blood loss in critically ill patients. Am J Crit Care. 1992; 1:85–90.
3. Gleason, E, Grossman, S, Campbell, C. Minimizing diagnostic blood loss in critically ill patients. Am J Crit Care. 1992; 1:85–90.
![]() 4. Gregersen, RA, et al. Accurate coagulation studies from heparinized radial artery catheters. Heart Lung. 1987; 16(6):686–692.
4. Gregersen, RA, et al. Accurate coagulation studies from heparinized radial artery catheters. Heart Lung. 1987; 16(6):686–692.
![]() 5. Harper, J. Use of intraarterial lines to obtain coagulation samples. Focus Crit Care. 1988; 15:51–55.
5. Harper, J. Use of intraarterial lines to obtain coagulation samples. Focus Crit Care. 1988; 15:51–55.
![]() 6. Laxson, CJ, Titler, MG, Drawing coagulation studies from arterial lines. an integrative literature review. Am J Crit Care 1994; 3:16–24.
6. Laxson, CJ, Titler, MG, Drawing coagulation studies from arterial lines. an integrative literature review. Am J Crit Care 1994; 3:16–24.
![]() 7. MacIsaac, CM, et al. The influence of a blood conserving device on anaemia in intensive care patients. Anaesth Intensive Care. 2003; 31:653–657.
7. MacIsaac, CM, et al. The influence of a blood conserving device on anaemia in intensive care patients. Anaesth Intensive Care. 2003; 31:653–657.
![]() 8. Molyneaux, RD, Papciak, B, Rorem, DA. Coagulation studies and the indwelling heparinized catheter. Heart Lung. 1987; 16:20–23.
8. Molyneaux, RD, Papciak, B, Rorem, DA. Coagulation studies and the indwelling heparinized catheter. Heart Lung. 1987; 16:20–23.
![]() 9. O’Grady, NP, et al, Guidelines for the prevention of intravascular catheter-related infections. Centers for Disease Control and Prevention. MMWR Rec Rep. 2002; 51(RR-10):1–29.
9. O’Grady, NP, et al, Guidelines for the prevention of intravascular catheter-related infections. Centers for Disease Control and Prevention. MMWR Rec Rep. 2002; 51(RR-10):1–29.
![]() 10. Peruzzi, WT, et al. A clinical evaluation of a blood conservation device in medical intensive care unit patients. Crit Care Med. 1993; 21:501–506.
10. Peruzzi, WT, et al. A clinical evaluation of a blood conservation device in medical intensive care unit patients. Crit Care Med. 1993; 21:501–506.
![]() 11. Preusser, BA, et al. Quantifying the minimum discard sample required for accurate arterial blood gases. Nurs Res. 1989; 38:276–279.
11. Preusser, BA, et al. Quantifying the minimum discard sample required for accurate arterial blood gases. Nurs Res. 1989; 38:276–279.
![]() 12. Rickard, CM, et al, A discard volume of twice the deadspace ensures clinically accurate arterial blood gases and electrolytes and prevents unnecessary blood loss. Care Med. Crit . 2003; 31:1654–1658.
12. Rickard, CM, et al, A discard volume of twice the deadspace ensures clinically accurate arterial blood gases and electrolytes and prevents unnecessary blood loss. Care Med. Crit . 2003; 31:1654–1658.
![]() 13. Rudisill, PT, Moore, LA. Relationship between arterial and venous activated partial thromboplastin time values in patients after percutaneous transluminal coronary angioplasty. Heart Lung. 1989; 18:514–519.
13. Rudisill, PT, Moore, LA. Relationship between arterial and venous activated partial thromboplastin time values in patients after percutaneous transluminal coronary angioplasty. Heart Lung. 1989; 18:514–519.
![]() 14. Silver, MJ, et al. Evaluation of a new blood-conserving arterial line system for patients in intensive care units. Crit Care Med. 1993; 21:507–511.
14. Silver, MJ, et al. Evaluation of a new blood-conserving arterial line system for patients in intensive care units. Crit Care Med. 1993; 21:507–511.
![]() 15. Silver, MJ, et al. Reduction of blood loss from diagnostic sampling in critically ill patients using a blood-conserving arterial line system. Chest. 1993; 104:1711–1715.
15. Silver, MJ, et al. Reduction of blood loss from diagnostic sampling in critically ill patients using a blood-conserving arterial line system. Chest. 1993; 104:1711–1715.
Alzetani, A, Vohra, HA, Patel, RL. Can we rely on arterial line sampling in performing activated plasma thromboplastin time after cardiac surgery. Eur J Anaesthesiol. 2004; 21:384–388.
Andrews, T, Waterman, H, Hillier, V, Blood gas analysis. a study of blood loss in intensive care. J Adv Nurs 1999; 30:851–857.
Cannon, K, Mitchell, KA, Fabian, TC. Prospective randomized evaluation of two methods of drawing coagulation studies from heparinized arterial lines. Heart Lung. 1985; 14:392–395.
Dirks, JL, Innovations in technology. continuous intra-arterial blood gas monitoring. Crit Care Nurs 1995; 15:19–29.
Heap, MJ, et al. Are coagulation studies on blood sampled from arterial lines valid. Anaesthesia. 1997; 52:640–645.
Hoste, EAJ, et al. Significant increase of activated partial thromboplastin time by heparinization of the radial artery catheter flush solution with a closed arterial system. Crit Care Med. 2002; 30:1030–1034.
Imperial-Perez F, McRae, M, Protocols for practice. hemodynamic monitoring seriesarterial pressure monitoring. American Association of Critical-Care Nurses, Aliso Viejo, CA, 1998.
Kaplow, R, Comparison of two techniques for obtaining samples for coagulation studies. venipuncture and intraarterial. Heart Lung 1988; 17:651–653.
Kajs, M. Comparison of coagulation values obtained by traditional venipuncture and intra-arterial line methods. Heart Lung. 1986; 15:622–627.
Martinez, JA, et al. Clinical utility of blood cultures drawn from central venous or arterial catheters in critically ill surgical patients. Crit Care Med. 2002; 30:7–13.
Reinhardt, AC, et al. Minimum discard volume from arterial catheters to obtain coagulation studies free from heparin effect. Heart Lung. 1987; 16:699–705.
Richiuso, N. Accuracy of aPTT values drawn from heparinized arterial lines in children. DCCN. 1998; 17:14–19.
Templin, K, Shively, M, Riley, J. Accuracy of drawing coagulation samples from heparinized arterial lines. Am J Crit Care. 1993; 2:88–95.

 Rationale: Teaching provides information and may reduce anxiety and fear.
Rationale: Teaching provides information and may reduce anxiety and fear. Rationale: This explanation encourages patient cooperation during blood withdrawal.
Rationale: This explanation encourages patient cooperation during blood withdrawal. Rationale: This ensures a functional arterial catheter.
Rationale: This ensures a functional arterial catheter. Rationale: This assessment provides data for comparison.
Rationale: This assessment provides data for comparison.