Arterial Catheter Insertion (Assist), Care, and Removal
PREREQUISITE NURSING KNOWLEDGE
• Knowledge of the anatomy and physiology of the vasculature and adjacent structures is needed.
• Knowledge of the principles of hemodynamic monitoring is necessary.
• Understanding of the principles of aseptic technique is needed.
• Conditions that warrant the use of arterial pressure monitoring include patients with:
 Hemodynamic instability (e.g., acute hypotension, hypertensive crisis)
Hemodynamic instability (e.g., acute hypotension, hypertensive crisis)
 Shock from any cause (e.g., hemorrhagic, septic)
Shock from any cause (e.g., hemorrhagic, septic)
 Continuous infusion of vasoactive medications
Continuous infusion of vasoactive medications
 Frequent arterial blood gas measurements (e.g., patients who need ventilatory support, patients with acute critical illnesses)
Frequent arterial blood gas measurements (e.g., patients who need ventilatory support, patients with acute critical illnesses)
 Nonpulsatile blood flow (e.g., those patients with ventricular assist device therapy or extracorporeal membrane oxygenation therapy)
Nonpulsatile blood flow (e.g., those patients with ventricular assist device therapy or extracorporeal membrane oxygenation therapy)
 Intraaortic balloon pump therapy
Intraaortic balloon pump therapy
 Coronary interventional procedures
Coronary interventional procedures
 Major surgical procedures (e.g., neurologic, abdominal, cardiac, thoracic, vascular, trauma)
Major surgical procedures (e.g., neurologic, abdominal, cardiac, thoracic, vascular, trauma)
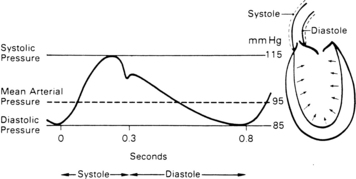
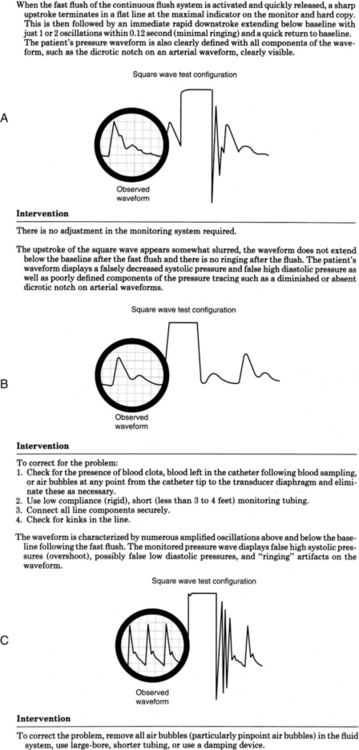
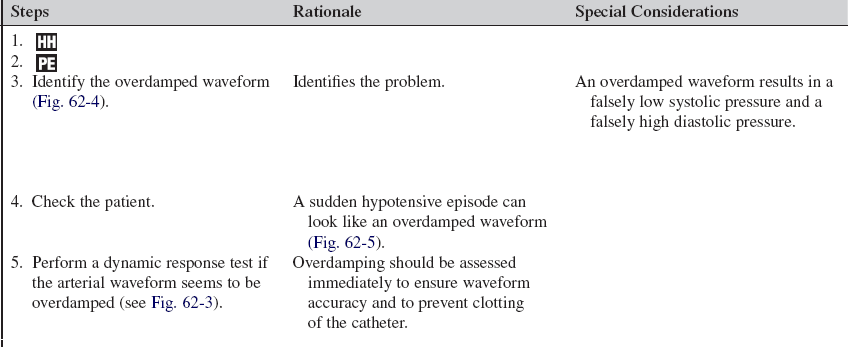
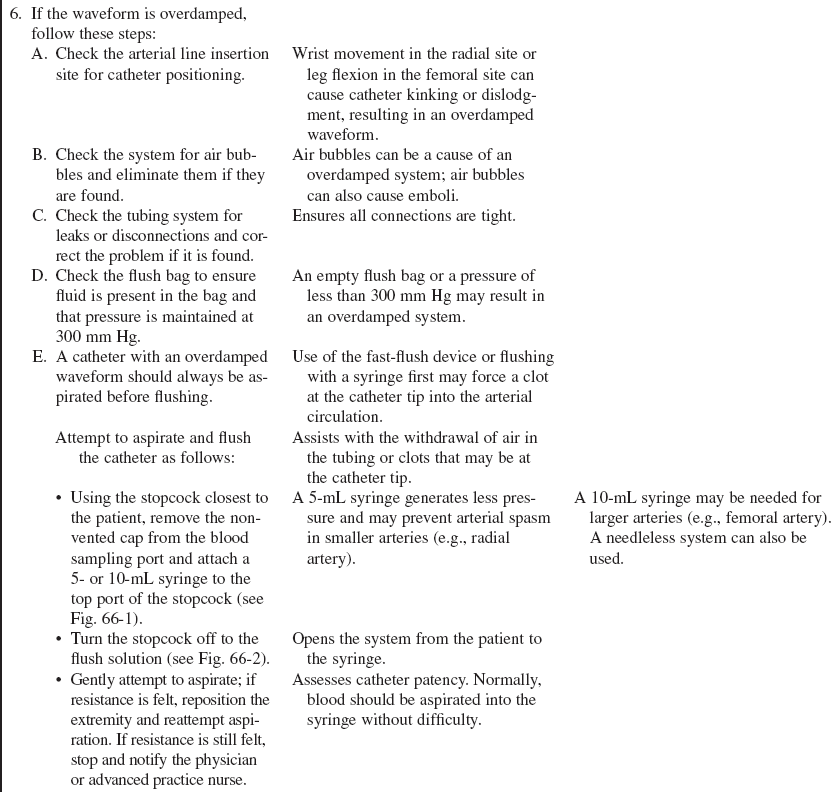
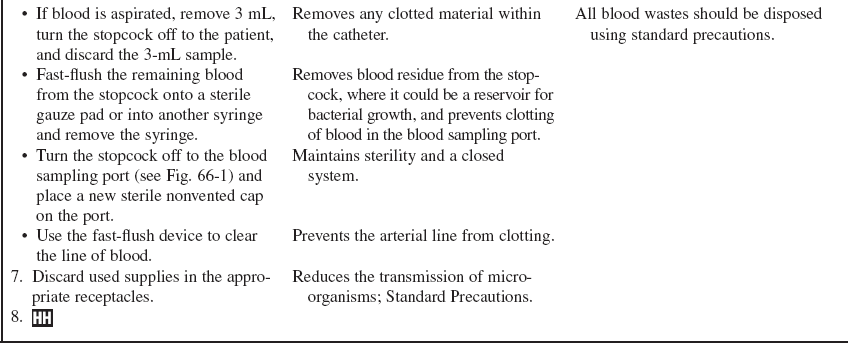
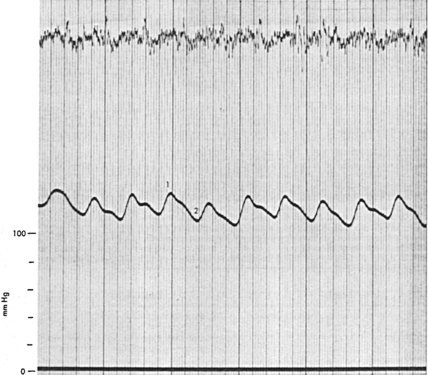
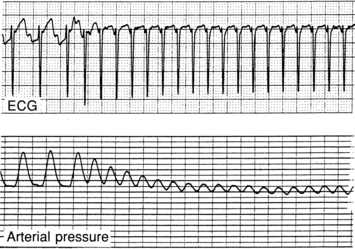
• Arterial pressure represents the forcible ejection of blood from the left ventricle into the aorta and out into the arterial system. During ventricular systole, blood is ejected into the aorta, generating a pressure wave. Because of the intermittent pumping action of the heart, this arterial pressure wave is generated in a pulsatile manner (Fig. 62-1). The ascending limb of the aortic pressure wave (anacrotic limb) represents an increase in pressure because of left ventricular ejection. The peak of this ejection is the peak systolic pressure, which should be less than 120 mm Hg in adults.18 After reaching this peak, the ventricular pressure declines to a level below aortic pressure and the aortic valve closes, marking the end of ventricular systole. The closure of the aortic valve produces a small rebound wave that creates a notch known as the dicrotic notch. The descending limb of the curve (diastolic downslope) represents diastole and is characterized by a long declining pressure wave, during which the aortic wall recoils and propels blood into the arterial network. The diastolic pressure is measured as the lowest point of the diastolic downslope, which should be less than 80 mm Hg in adults.18
• The difference between the systolic and diastolic pressures is the pulse pressure, with a normal value of about 40 mm Hg.
• Arterial pressure is determined by the relationship between blood flow through the vessels (cardiac output) and the resistance of the vessel walls (systemic vascular resistance). The arterial pressure is therefore affected by any factors that change either cardiac output or systemic vascular resistance.
• The average arterial pressure during a cardiac cycle is called the mean arterial pressure (MAP). MAP is not the average of the systolic plus the diastolic pressures because during the cardiac cycle, the pressure remains closer to diastole than to systole for a longer period (at normal heart rates). The MAP is calculated automatically by most patient monitoring systems; however, it can be calculated with the following formula:
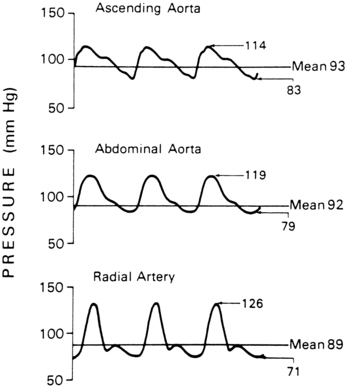
• MAP represents the driving force (perfusion pressure) for blood flow through the cardiovascular system. MAP is at its highest point in the aorta. As blood travels through the circulatory system, systolic pressure increases and diastolic pressure decreases, with an overall decline in the MAP (Fig. 62-2).
• The location of arterial catheter placement depends on the condition of the arterial vessels and the presence of other catheters (i.e., the presence of a dialysis shunt is a contraindication for placement of an arterial catheter in the same extremity). Once inserted, the arterial catheter causes little or no discomfort to the patient and allows continuous blood pressure assessment and intermittent blood sampling. If intraaortic balloon pump therapy is necessary, arterial pressure may be directly monitored from the tip of the balloon in the aorta.
• The radial artery is the most common site for arterial pressure monitoring. When arterial pulse waveforms are recorded from a peripheral site (instead of a central site), the waveform morphology changes. The anacrotic limb becomes more peaked and narrowed, with increased amplitude; therefore, the systolic pressure in peripheral sites is higher than the systolic pressure recorded from a more central site (see Fig. 62-2). In addition, the diastolic pressure decreases, the diastolic downslope may show a secondary wave, and the dicrotic notch becomes less prominent from distal sites.
• Vasodilators and vasoconstrictors may change the appearance of the waveforms from distal sites. Vasodilators may cause the waveform to take on a more central appearance. Vasoconstrictors may cause the systolic pressure to become more exaggerated because of enhanced resistance in the peripheral arteries.
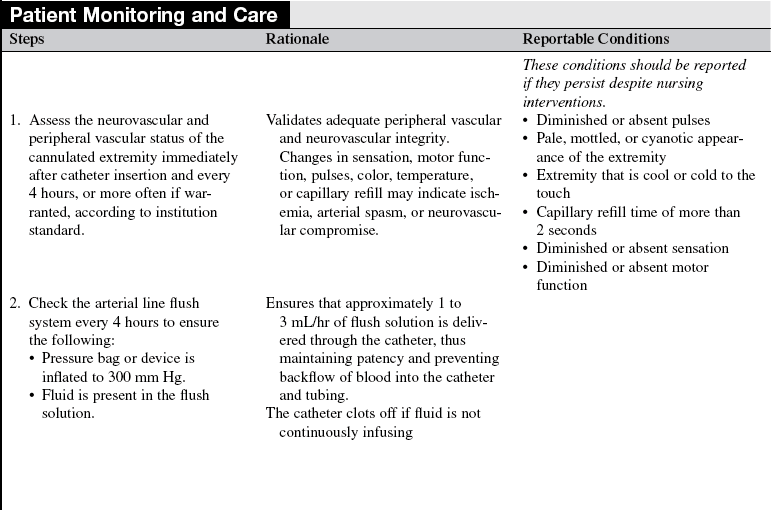
• Several potential complications are associated with arterial pressure monitoring. Infection at the insertion site can develop and cause sepsis. Clot formation in the catheter can lead to arterial embolization. The catheter can cause vessel perforation with extravasation of blood and flush solution into the surrounding tissue. Finally, the distal extremity can develop circulatory or neurovascular impairment.
EQUIPMENT
• 1- to 2-inch (2.5- to 5-cm) over-the-needle catheter (14-gauge to 20-gauge for adults) or prepackaged kit with catheter, introducer, and guidewire
• Single-pressure transducer system (see Procedure 76)
• Monitoring equipment consisting of a connecting cable, monitor, oscilloscope display screen, and recorder
• Nonsterile gloves, head coverings, goggles
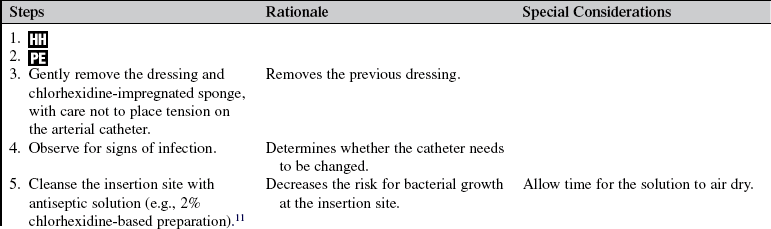
• Antiseptic solution (e.g., 2% chlorhexidine-based preparation)
• 1% lidocaine without epinephrine, 1 to 2 mL
Additional equipment to have available as needed includes the following:
PATIENT AND FAMILY EDUCATION
• Explain the procedure and the purpose of the arterial catheter.  Rationale: This explanation decreases patient and family anxiety.
Rationale: This explanation decreases patient and family anxiety.
• Explain the standard of care to the patient and family, including insertion procedure, alarms, dressings, and length of time the catheter is expected to be in place.  Rationale: This explanation encourages the patient and family to ask questions and voice concerns about the procedure and decreases patient and family anxiety.
Rationale: This explanation encourages the patient and family to ask questions and voice concerns about the procedure and decreases patient and family anxiety.
• Explain the patient’s expected participation during the procedure.  Rationale: Patient cooperation during insertion is encouraged.
Rationale: Patient cooperation during insertion is encouraged.
• Explain the importance of keeping the affected extremity immobile.  Rationale: This explanation encourages patient cooperation to prevent catheter dislodgment and ensures a more accurate waveform.
Rationale: This explanation encourages patient cooperation to prevent catheter dislodgment and ensures a more accurate waveform.
• Instruct the patient to report any warmth, redness, pain, or wet feeling at the insertion site at any time, including after catheter removal.  Rationale: These symptoms may indicate infection, bleeding, or disconnection of the tubing or catheter.
Rationale: These symptoms may indicate infection, bleeding, or disconnection of the tubing or catheter.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Obtain the patient’s medical history, including a history of diabetes and hypertension.  Rationale: Patients with diabetes mellitus or hypertension are at higher risk for arterial or venous insufficiency.
Rationale: Patients with diabetes mellitus or hypertension are at higher risk for arterial or venous insufficiency.
• Obtain the patient’s medical history for peripheral arterial disease, vascular grafts, arteriovenous (AV) fistulas or shunts, arterial vasospasm, thrombosis, or embolism. In addition, obtain the patient’s history of coronary artery bypass graft surgery in which radial arteries were removed for use as conduits.  Rationale: Extremities with any of these problems should be avoided as sites for cannulation because of the potential for complications.
Rationale: Extremities with any of these problems should be avoided as sites for cannulation because of the potential for complications.
• Assess the patient’s current anticoagulation therapy, history of blood dyscrasias, and pertinent laboratory values (prothrombin time [PT], international normalized ratio [INR], partial thromboplastin time [PTT], and platelets) before the procedure.  Rationale: Anticoagulation therapy, blood dyscrasias, or alterations in coagulation studies could increase the risk of hematoma formation or hemorrhage.
Rationale: Anticoagulation therapy, blood dyscrasias, or alterations in coagulation studies could increase the risk of hematoma formation or hemorrhage.
• Assess the patient’s allergy history (e.g., allergy to heparin, lidocaine, antiseptic solutions, or adhesive tape).  Rationale: This assessment decreases the risk for allergic reactions. Patients with heparin-induced thrombocytopenia should not receive heparin in the flush solution.
Rationale: This assessment decreases the risk for allergic reactions. Patients with heparin-induced thrombocytopenia should not receive heparin in the flush solution.
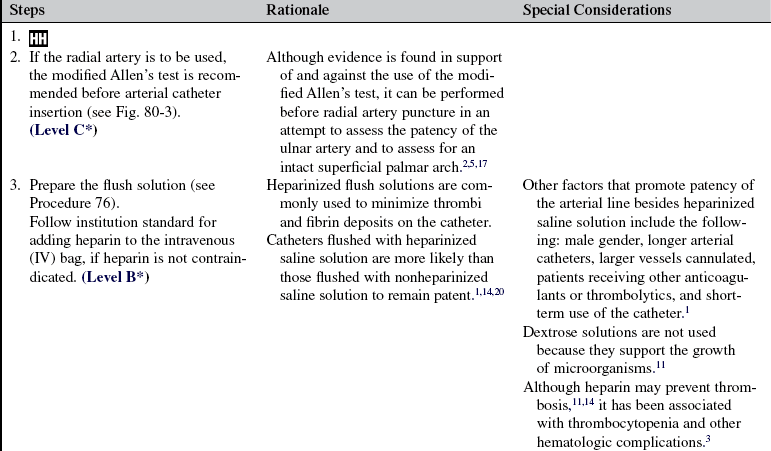
• Assess the neurovascular and peripheral vascular status of the extremity to be used for the arterial cannulation, including color, temperature, presence and fullness of pulses, capillary refill, presence of bruit (in larger arteries such as the femoral artery), and motor and sensory function (as compared with the opposite extremity). Note: A modified Allen’s test should be performed before cannulation of the radial artery (see Fig. 80-3).  Rationale: This assessment may help identify any neurovascular or circulatory impairment before cannulation to avoid potential complications.
Rationale: This assessment may help identify any neurovascular or circulatory impairment before cannulation to avoid potential complications.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand preprocedural teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of previously taught information is evaluated and reinforced.
Rationale: Understanding of previously taught information is evaluated and reinforced.
• Ensure that informed consent is obtained.  Rationale: Informed consent protects the rights of the patient and allows a competent decision to be made by the patient; however, in emergency circumstances, time may not allow the form to be signed.
Rationale: Informed consent protects the rights of the patient and allows a competent decision to be made by the patient; however, in emergency circumstances, time may not allow the form to be signed.
• Perform a pre-procedure verification and time out, if non-emergent.  Rationale: Ensures patient safety.
Rationale: Ensures patient safety.
• Place the patient’s extremity in the appropriate position with adequate lighting of the insertion site.  Rationale: This placement prepares the site for cannulation and facilitates an accurate insertion.
Rationale: This placement prepares the site for cannulation and facilitates an accurate insertion.
References
![]() 1. American Association of Critical-Care Nurses, Evaluation of the effects of heparinized and nonheparinized flush solutions on the patency of arterial pressure monitoring lines. the AACN Thunder Project. Am J Crit Care 1993; 2:3–15.
1. American Association of Critical-Care Nurses, Evaluation of the effects of heparinized and nonheparinized flush solutions on the patency of arterial pressure monitoring lines. the AACN Thunder Project. Am J Crit Care 1993; 2:3–15.
2. Barone, J, Madlinger, RV. Should an Allen test be performed before radial artery cannulation. J Trauma. 2006; 6:468–470.
![]() 3. Chong, BH. Heparin-induced thrombocytopenia. Br J -Haematol. 1995; 89:431–439.
3. Chong, BH. Heparin-induced thrombocytopenia. Br J -Haematol. 1995; 89:431–439.
![]() 4. Gleason, E, Grossman, S, Campbell, C. Minimizing diagnostic blood loss in critically ill patients. Am J Crit Care. 1992; 1:85–90.
4. Gleason, E, Grossman, S, Campbell, C. Minimizing diagnostic blood loss in critically ill patients. Am J Crit Care. 1992; 1:85–90.
![]() 5. Greenwood, MJ, et al, Vascular communications of the hand in patients being considered for transradial coronary angiography. is the Allen’s test accurate. J Am Coll -Cardiol 2005; 46:2013–2017.
5. Greenwood, MJ, et al, Vascular communications of the hand in patients being considered for transradial coronary angiography. is the Allen’s test accurate. J Am Coll -Cardiol 2005; 46:2013–2017.
6. Infusion Nurses Society. Infusion nursing standards of practice. J Infusion Nurs. 2006; 29:S1–S92.
![]() 7. Luskin, RL, et al, Extended use of disposable pressure transducers. a bacteriologic evaluation. JAMA 1986; 255 :916–920.
7. Luskin, RL, et al, Extended use of disposable pressure transducers. a bacteriologic evaluation. JAMA 1986; 255 :916–920.
![]() 8. MacIsaac, CM, et al. The influence of a blood conserving device on anaemia in intensive care patients. Anaesth Intensive Care. 2003; 31:653–657.
8. MacIsaac, CM, et al. The influence of a blood conserving device on anaemia in intensive care patients. Anaesth Intensive Care. 2003; 31:653–657.
![]() 9. Maki, DG, Narans, LL, Knasinski, V, et al. Prospective, randomized, investigator-masked trial of novel chlohexidine-impregnated disk (Biopatch) on central venous and arterial catheters [abstract]. Infect Control Hosp Epidemiol. 2000; 21:96.
9. Maki, DG, Narans, LL, Knasinski, V, et al. Prospective, randomized, investigator-masked trial of novel chlohexidine-impregnated disk (Biopatch) on central venous and arterial catheters [abstract]. Infect Control Hosp Epidemiol. 2000; 21:96.
![]() 10. McGhee, BH, Bridges, MEJ, Monitoring arterial blood pressure. what you may not know. Crit Care Nurse 2002; 60–79.
10. McGhee, BH, Bridges, MEJ, Monitoring arterial blood pressure. what you may not know. Crit Care Nurse 2002; 60–79.
![]() 11. O’Grady, NP, et al. Guidelines for the prevention of intravascular catheter-related infections, Centers for Disease Control and Prevention. MMWR. 2002; 51(RR-10):1–36.
11. O’Grady, NP, et al. Guidelines for the prevention of intravascular catheter-related infections, Centers for Disease Control and Prevention. MMWR. 2002; 51(RR-10):1–36.
![]() 12. O’Malley, MK, et al. Value of routine pressure monitoring system changes after 72 hours of continuous use. Crit Care Med. 1994; 22:1424–1430.
12. O’Malley, MK, et al. Value of routine pressure monitoring system changes after 72 hours of continuous use. Crit Care Med. 1994; 22:1424–1430.
![]() 13. Peruzzi, WT, et al. A clinical evaluation of a blood conservation device in medical intensive care unit patients. Crit Care Med. 1993; 21:501–506.
13. Peruzzi, WT, et al. A clinical evaluation of a blood conservation device in medical intensive care unit patients. Crit Care Med. 1993; 21:501–506.
![]() 14. Randolph, AG, et al, Benefit of heparin in peripheral venous and arterial catheters. systematic review and meta-analysis of randomised controlled trials. BMJ 1998; 316:969–975.
14. Randolph, AG, et al, Benefit of heparin in peripheral venous and arterial catheters. systematic review and meta-analysis of randomised controlled trials. BMJ 1998; 316:969–975.
![]() 15. Silver, MJ, et al. Evaluation of a new blood-conserving arterial line system for patients in intensive care units. Crit Care Med. 1993; 21:507–511.
15. Silver, MJ, et al. Evaluation of a new blood-conserving arterial line system for patients in intensive care units. Crit Care Med. 1993; 21:507–511.
![]() 16. Silver, MJ, et al. Reduction of blood loss from diagnostic sampling in critically ill patients using a blood-conserving arterial line system. Chest. 1993; 104:1711–1715.
16. Silver, MJ, et al. Reduction of blood loss from diagnostic sampling in critically ill patients using a blood-conserving arterial line system. Chest. 1993; 104:1711–1715.
![]() 17. Slogoff, S, Keats, AS, Arlund, C. On the safety of radial artery cannulation. Anesthesiology. 1983; 59:42–47.
17. Slogoff, S, Keats, AS, Arlund, C. On the safety of radial artery cannulation. Anesthesiology. 1983; 59:42–47.
![]() 18. US Department of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute, National High Blood Pressure Education Program. The seventh report of the joint national committee on prevention, detection, evaluation and treatment of high blood pressure retrieved July 27, 2009. www.nhlbi.nih.gov/guidelines/hypertension/jnc7full.pdf, 2004 [Publication No. 04 – 5230].
18. US Department of Health and Human Services, National Institutes of Health, National Heart, Lung, and Blood Institute, National High Blood Pressure Education Program. The seventh report of the joint national committee on prevention, detection, evaluation and treatment of high blood pressure retrieved July 27, 2009. www.nhlbi.nih.gov/guidelines/hypertension/jnc7full.pdf, 2004 [Publication No. 04 – 5230].
19. Timsit, J, et al, Chlorhexidine-impregnated sponges and less frequent dressing changes for prevention of catheter-related infections in critically ill adults. JAMA 2009; 310 :1231–1241.
![]() 20. Zevola, DR, Dioso, J, Moggio, R. Comparison of heparinized solutions for maintaining patency of arterial and pulmonary artery catheters. Am J Crit Care. 1997; 6:52–55.
20. Zevola, DR, Dioso, J, Moggio, R. Comparison of heparinized solutions for maintaining patency of arterial and pulmonary artery catheters. Am J Crit Care. 1997; 6:52–55.
Barbeito, A, Mark, JB. Arterial and central venous pressure monitoring. Anesthesiol Clin. 2006; 24:717–735.
Bridges, EJ, et al. Ask the experts. Crit Care Nurse. 1997; 17:96–102.
Chulay, M, Holland, S, Ask the experts. where should the transducer be leveled for radial or femoral arterial pressure monitoring. Crit Care Nurse 1996; 16:103–107.
Darovic, GO, Arterial pressure monitoring. In: Hemodynamic monitoring: invasive and noninvasive clinical application. ed 3. Saunders, Philadelphia, 2002.
Foster, B. Continuing discussion on transducer placement. ask the experts column of the December issue 1996. zero referencing arterial lines. Crit Care Nurse. 1997; 17:18.
Gorny, DA. Arterial blood pressure measurement technique. AACN Clin Issues. 1993; 4:66–80.
Halm, MS, Flushing hemodynamic catheters. what does the science tell us. Am J Crit Care 2008; 17:73–76.
Imperial-Perez, F, McRae, M, Protocols for practice. applying research at the bedsidearterial pressure monitoring. Crit Care Nurse 2002; 22:70–72.
Imperial-Perez, F, McRae, M, Protocols for practice. hemodynamic monitoring seriesarterial pressure monitoring. American Association of Critical-Care Nurses, Aliso Viejo, CA, 1998.
Lapum, JL, Patency of arterial catheters with heparinized solutions versus non-heparinized solutions. a review of the literature. Can J Cardiovasc Nurs 2006; 16:64–67.
Leeper, B, Ask the experts. what is the standard regarding isotonic sodium chloride solution versus heparin in pressure monitoring systems. Crit Care Nurse 2006; 26:137–138.
O’Grady, NP, et al, Patient safety and the science of prevention. the time for implementing the guidelines for the prevention of intravascular catheter-related infections is now. Crit Care Med 2003; 31:291–292.
Shaffer, C. Diagnostic blood loss in mechanically ventilated patients. Heart Lung. 2007; 36:217–222.
Tuncali, BE, et al. A comparison of the efficacy of heparinized and nonheparinized solutions for maintenance of perioperative radial arterial catheter patency and subsequent occlusion. Anesth Analg. 2005; 100:1117–1121.