Twelve-Lead Electrocardiogram
A 12-lead electrocardiogram provides information about the electrical system of the heart from 12 different views or leads. The electrocardiogram is the most commonly conducted cardiovascular diagnostic procedure.3 Common uses of a 12-lead electrocardiogram include diagnosis of acute coronary syndromes, identification of dysrhythmias and conduction disturbances, and determination of the effects of medications or electrolytes on the electrical system of the heart.
PREREQUISITE NURSING KNOWLEDGE
• Understanding of the anatomy and physiology of the cardiovascular system, principles of cardiac conduction, the cardiac cycle, properties of cardiac tissue (automaticity, excitability, conductivity, and refractoriness), principles of electrophysiology, electrocardiographic (ECG) lead placement, basic dysrhythmia interpretation, and electrical safety is necessary.
• Advanced cardiac life support knowledge and skills are needed.
• Clinical and technical competence in the use of the 12-lead ECG machine and recorder is necessary.
• A 12-lead ECG provides different views or leads of the electrical activity of the heart. The leads are standard limb leads (I, II, III), augmented limb leads (Augmented Vector Right or aVR, Augmented Vector Foot or aVF, and Augmented vector Left or aVL), and six chest leads (V1 to V6).
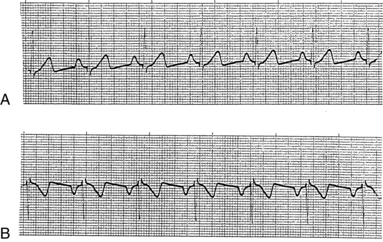
• The standard and augmented leads view the heart from the vertical or frontal plane (Fig. 60-1), and the chest leads view the heart from the horizontal plane (Fig. 60-2).

Figure 60-1 Vertical plane leads: I, II, III, aVR, aVL, aVF.

Figure 60-2 Horizontal plane leads: V1 to V6.
• The graphic display consists of the P, Q, R, S, and T waves, which represent electrical activity within the heart.
• Serial 12-lead ECGs (more than two ECGs recorded at different times) may be obtained. The accuracy of interpretation relies on consistent electrode placement. Indelible markers can be used to identify the electrode locations to ensure that the same lead placement is used when serial ECGs are recorded.
• Advances in technology have allowed for online or wireless transmission, networking capabilities, and computerized interpretation of the 12-lead ECG (Fig. 60-3). The 12-lead ECG cable is attached to a processing device that digitizes the 12-lead ECG recording and transfers the information to the wireless device, which transmits the information to the medical record. This increases access to the 12-lead ECG for review and can assist with rapid interpretation and treatment of the patient.
EQUIPMENT
• 12-lead ECG machine and recorder
• Gauze pads or terrycloth washcloth
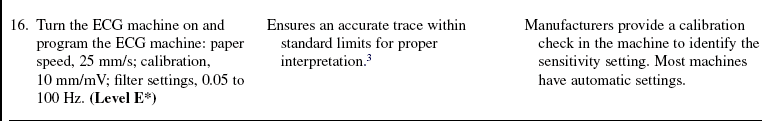
• Cleansing pads or nonemollient soap and water
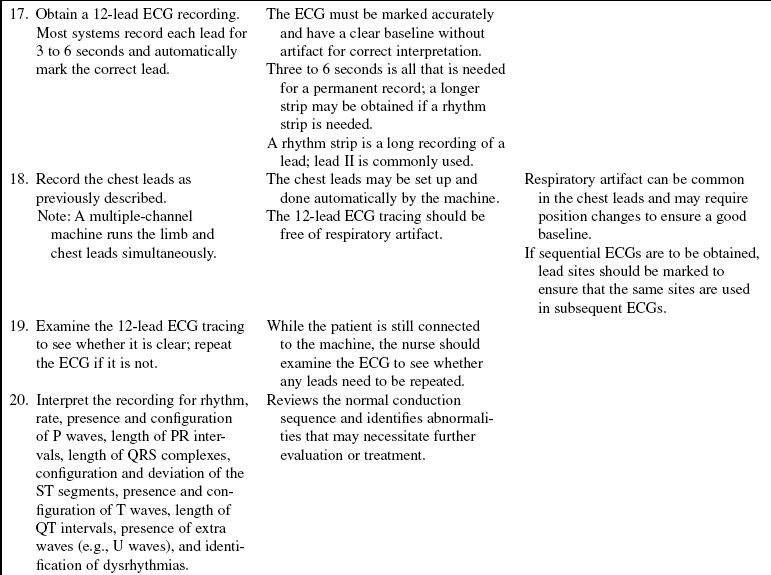
Additional equipment to have available as needed includes the following:
PATIENT AND FAMILY EDUCATION
• Assess the readiness of the patient and family to learn.  Rationale: Anxiety and concerns of the patient and family may inhibit the ability to learn.
Rationale: Anxiety and concerns of the patient and family may inhibit the ability to learn.
• Provide explanations of the equipment and procedure to the patient and family.  Rationale: Information may decrease anxiety.
Rationale: Information may decrease anxiety.
• Emphasize that the patient should not talk but should relax, lie still, and breathe normally.  Rationale: Chest movement can distort the ECG picture.
Rationale: Chest movement can distort the ECG picture.
• Reassure the patient and family that the 12-lead ECG will be reviewed and that any alterations or problems will be addressed.  Rationale: Patients and families need to be reassured that immediate care is available if it is needed.
Rationale: Patients and families need to be reassured that immediate care is available if it is needed.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess the patient’s peripheral pulses, vital signs, heart sounds, level of consciousness, lung sounds, neck vein distention, presence of chest pain or palpitations, and peripheral circulatory disorders (e.g., clubbing, cyanosis, and dependent edema).  Rationale: Physical signs and symptoms may result from alterations in performance of the cardiovascular system.
Rationale: Physical signs and symptoms may result from alterations in performance of the cardiovascular system.
• Assess the patient’s history of cardiac dysrhythmias or cardiac problems.  Rationale: This assessment provides baseline data.
Rationale: This assessment provides baseline data.
• Assess patient medications.  Rationale: This assessment provides baseline data.
Rationale: This assessment provides baseline data.
• Assess previous 12-lead ECGs.  Rationale: Previous ECGs provide baseline data.
Rationale: Previous ECGs provide baseline data.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand preprocedural teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: This information evaluates and reinforces understanding of previously taught information.
Rationale: This information evaluates and reinforces understanding of previously taught information.
• Assist the patient to a supine position.  Rationale: This position allows easy access to the chest for electrode placement; changes in body position may affect the accuracy of the ECG recording.
Rationale: This position allows easy access to the chest for electrode placement; changes in body position may affect the accuracy of the ECG recording.
• Assist the patient in removing clothing that covers the chest while providing for the patient’s privacy.  Rationale: Removal of clothing provides a clear view of the chest and allows for identification of landmarks and proper placement of leads while maintaining the patient’s privacy.
Rationale: Removal of clothing provides a clear view of the chest and allows for identification of landmarks and proper placement of leads while maintaining the patient’s privacy.
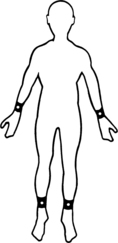
Figure 60-4 Limb lead placement in 12-lead ECG.
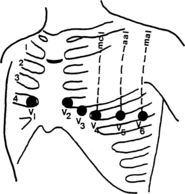
Figure 60-5 Precordial or chest lead placement.
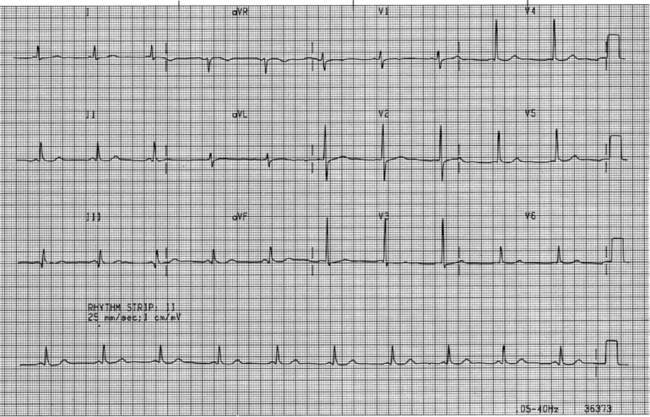
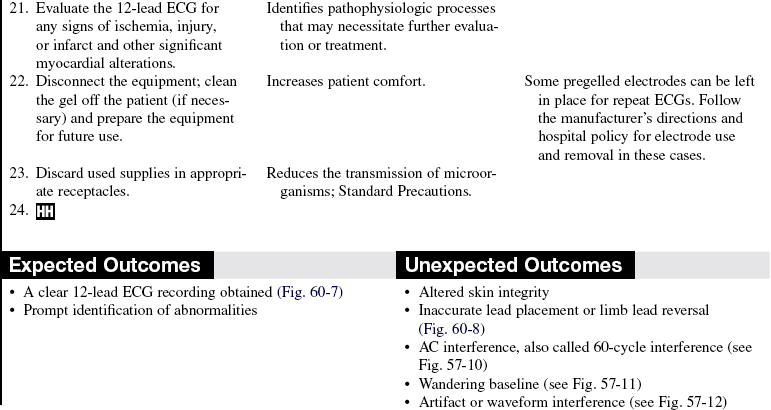
Figure 60-7 Clear 12-lead ECG recording.
References
1. Drew, BJ. Pitfalls and artifacts in electrocardiography. Cardiol Clin. 2006; 24:309–315.
![]() 2. Drew, BJ, et al, Practice standards for electrocardiographic monitoring in hospital settings. an American Heart Association Scientific Statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young. Circulation 2004; 110:2721–2746.
2. Drew, BJ, et al, Practice standards for electrocardiographic monitoring in hospital settings. an American Heart Association Scientific Statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young. Circulation 2004; 110:2721–2746.
3. Kligfield, P, et al, Recommendations for the standardization and interpretation of the electrocardiogram . part 1: the electrocardiogram and its technology: a scientific statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology: The American College of Cardiology Foundation; and the Heart Rhythm Society. Circulation 2007; 115:1306–1324.
Adams-Hamoda MG, et al. Factors to consider when analyzing 12-lead electrocardiograms for evidence of acute myocardial ischemia. Am J Crit Care. 2003; 12:9–16.
Adams-Hamoda MG, Pelter, M. Interpreting a postoperative 12-lead ECG waveform. Am J Crit Care. 2003; 12:267–268.
Alspach, J. Core curriculum for critical care nursing. Philadelphia: Saunders; 2006.
Donnely, MP, et al, Lead selection. old and new methods for locating the most electrocardiogram information. J Electrocardiol 2008; 41:257–263.
Drew, BJ, Kligfield, P, Standardizing electrocardiographic leads. introduction to a symposium. J Electrocardiol 2008; 41:187–189.
Drew, BJ, Putting it all together. case studies on ECG monitoring. AACN Adv Crit Care 2007; 18:305–317.
Drew, BJ, et al. An American Heart Association scientific statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young. Circulation. 2004; 110:2721–2746.
Gregg, RE, et al. What is inside the electrocardiograph. J Electrocardiol. 2008; 41:8–14.
Jefferies, P, Woolf, S, Linde, B, Technology-based vs. traditional instruction. a comparison of two methods for teaching the skill of performing a 12-lead ECG . Nurs Educ Perspect . 2003; 24:70–74.