Continuous ST-Segment Monitoring
Bedside ST-segment monitoring provides ongoing surveillance for detection of transient myocardial ischemia. This technology should be applied to patients who are being evaluated or are diagnosed with acute coronary syndrome, including acute myocardial infarction and unstable angina.2,3,8,13,16 For these patients, continuous ST-segment monitoring is valuable in determining the success of thrombolytic therapy and percutaneous coronary intervention and detecting recurrent or transient ischemia. The goal of continuous ST-segment monitoring is to detect new or recurrent myocardial ischemia.
PREREQUISITE NURSING KNOWLEDGE
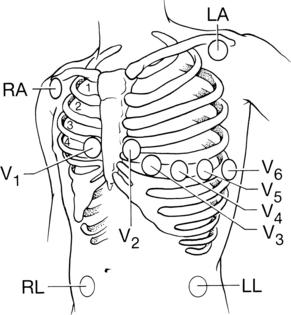
• Understanding of the anatomy and physiology of the cardiovascular system, principles of cardiac conduction, electrocardiogram (ECG) lead placement, basic dysrhythmia interpretation, and electrical safety is needed.
• Advanced cardiac life support knowledge and skills are necessary.
• Continuous monitoring of the ECG for ischemic ST-segment changes is more reliable than patient symptoms because more than three quarters of ECG-detected ischemic events are clinically silent.2,8,13,16 Patients who have transient ischemia detected with continuous ST-segment monitoring are more likely to have unfavorable outcomes, including myocardial infarction (MI) and death, compared with patients without such events.2,3,8,10,11,13,16
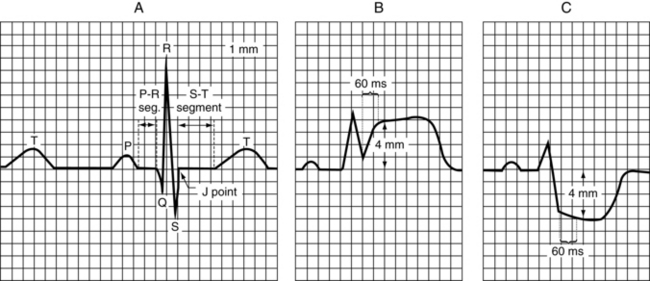
• Because of the dynamic, unpredictable, and silent nature of myocardial ischemia, continuous monitoring of patients for ischemia is essential. Clinicians should monitor the trend of the ST segments over time and evaluate any ST-segment changes (elevation or depression) for possible myocardial ischemia (Fig. 59-1).
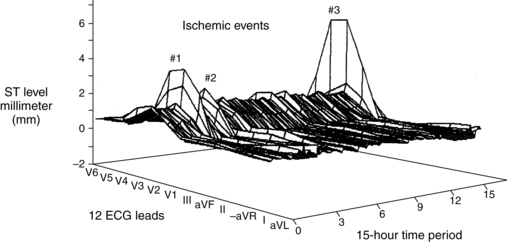
Figure 59-1 The importance of assessing the trend of the ST segments over time. The three-dimensional image illustrates ST-segment deviation in millimeters (Y-axis) in all 12 ECG leads (X-axis) over a 15-hour period (Z-axis). Illustrated are three separate ischemic events, characterized by ST-segment elevation, in leads V3 to V5. (Adapted from Pelter MM, Adams MG, Drew BJ: Transient myocardial ischemia is an independent predictor of adverse in-hospital outcomes in patients with acute coronary syndromes treated in the telemetry unit, Heart Lung 32:71-78, 2003.)
• Other nonischemic causes for a change in the ST-segment trend are movement of the skin electrodes, dysrhythmias, intermittent bundle-branch block pattern, body position changes, and ventricular paced rhythms.8,12
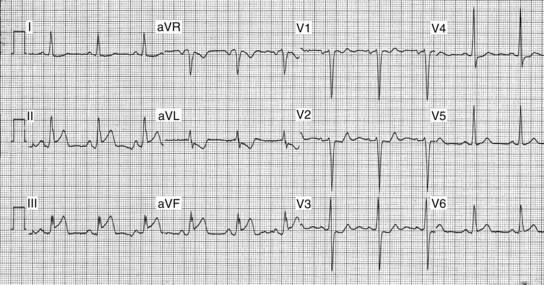
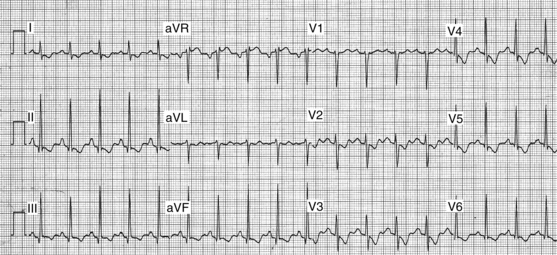
• The first type of ischemia seen in patients with acute coronary syndrome (ACS) is supply-related ischemia from coronary occlusion. Coronary occlusion is brought on by disruption of an atherosclerotic plaque followed by cycles of plaque rupture, platelet stimulation, coronary vasospasm, and thrombus formation.5,6,14,19 Because this type of ischemia threatens the entire thickness of the myocardium, immediate treatment to reestablish blood flow to the heart is essential. The typical ECG manifestation of total coronary occlusion is ST-segment elevation visible in the ECG leads that lie directly over the ischemic myocardial zone. Occlusion of the right coronary artery (RCA) typically produces ST-segment elevation in leads II, III, and augmented vector foot or aVF (Fig. 59-2). Occlusion of the left anterior descending (LAD) coronary artery typically produces ST-segment elevation in leads V2, V3, and V4 (Fig. 59-3). Diagnosis of total coronary occlusion of the left circumflex coronary artery (LCX) is more complex because placement of the standard ECG electrodes is on the anterior chest, opposite the wall that this coronary artery supplies. Occlusion of the LCX may produce ST-segment depression in leads V1, V2, or V3, which reflects the reciprocal, or mirror image, ST-segment elevation occurring in the posterior wall of the myocardium.
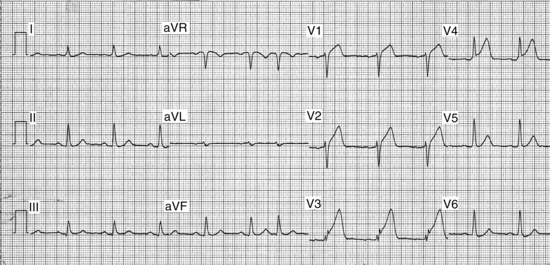
Figure 59-3 The typical ST-segment pattern of supply-related ischemia in the anterior wall. The LAD artery is likely occluded, resulting in ST-segment elevation in leads V2 to V4.
• A second type of ischemia for which patients with ACS or stable angina are at risk is demand-related ischemia. This type of ischemia may occur when the demand for oxygen (i.e., exercise, tachycardia, or stress) exceeds the flow capabilities of a coronary artery with a stable atherosclerotic plaque. The ST-segment pattern of demand-related ischemia is depression, often appearing in several ECG leads (Fig. 59-4).
• Diagnosis of myocardial ischemia necessitates continuous monitoring of all 12 ECG leads because the mechanism of ischemia may vary (i.e., occlusion versus demand-related ischemia), resulting in distinctly different ST-segment patterns (e.g., elevation or depression). If only two ECG leads are available, however, the best two are leads III and V3.8 Patient-specific monitoring also may be done if a prior 12-lead ECG was obtained during acute ischemia (i.e., ST-segment elevation MI, percutaneous coronary intervention [PCI], or treadmill test). In this scenario, the ECG lead or leads showing maximal ST-segment deviation should be selected for continuous monitoring to detect recurrent ischemia.
• According to current consensus statements,8,9 multilead ST-segment monitoring is indicated in most patients with the following diagnoses:
 Early phase of acute MI (ST elevation, non-ST elevation, “rule-out”)
Early phase of acute MI (ST elevation, non-ST elevation, “rule-out”)
 Chest pain (or anginal equivalent) that prompts a visit to the emergency department
Chest pain (or anginal equivalent) that prompts a visit to the emergency department
• According to these same guidelines,8,9 ST-segment monitoring may be of benefit for the following cases:
• ST-segment monitoring may not be appropriate for certain patient groups because current software cannot reliably interpret ST-segment changes resulting from myocardial ischemia.8,9 Specifically, it may not be suitable to monitor patients with:
• A variety of bedside and telemetry cardiac monitors are currently available for use in clinical practice. Not all monitoring systems are equipped with ST-segment monitoring software, however. Clinicians must determine whether their cardiac monitoring system has ST-segment monitoring capabilities.
EQUIPMENT
• Electrodes, pregelled and disposable
• Cardiac monitor with ST-segment monitoring capability and patient cable
• Gauze pads or terrycloth washcloth
Additional equipment to have available as needed includes the following:
PATIENT AND FAMILY EDUCATION
• Explain the purpose of ST-segment monitoring.  Rationale: This explanation decreases patient and family anxiety.
Rationale: This explanation decreases patient and family anxiety.
• Encourage the patient to report any symptoms of chest pain or anginal equivalent (e.g., arm pain, jaw pain, shortness of breath, or nausea).  Rationale: This education heightens the patient’s awareness of cardiac sensations and encourages communication of anginal symptoms.
Rationale: This education heightens the patient’s awareness of cardiac sensations and encourages communication of anginal symptoms.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Identify patients at risk for ischemia.8  Rationale: Patients at risk for myocardial ischemia need to be identified.
Rationale: Patients at risk for myocardial ischemia need to be identified.
• Assess the patient’s cardiac rhythm.  Rationale: This assessment provides baseline data and ensures the patient has a cardiac rhythm suitable for ST-segment monitoring.
Rationale: This assessment provides baseline data and ensures the patient has a cardiac rhythm suitable for ST-segment monitoring.
• Identify the patient’s baseline ST-segment levels before initiating ST-segment monitoring.  Rationale: The patient’s baseline ST-segment level is identified for comparison with subsequent changes.
Rationale: The patient’s baseline ST-segment level is identified for comparison with subsequent changes.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand preprocedural teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: This communication evaluates and reinforces understanding of previously taught information.
Rationale: This communication evaluates and reinforces understanding of previously taught information.
• Place the patient in a resting supine position in bed, and expose the patient’s torso while maintaining modesty.  Rationale: This preparation provides access to the patient’s chest for electrode placement and ensures that an artifact-free ECG is obtained.
Rationale: This preparation provides access to the patient’s chest for electrode placement and ensures that an artifact-free ECG is obtained.
References
![]() 1. Adams, MG, Drew, BJ, Body position effects on the ECG. implication for ischemia monitoring. J Electrocardiol. 1997; 30(4):285–291.
1. Adams, MG, Drew, BJ, Body position effects on the ECG. implication for ischemia monitoring. J Electrocardiol. 1997; 30(4):285–291.
![]() 2. Adams, MG, Pelter, MM, Wung, SF, et al, Frequency of silent myocardial ischemia with 12-lead ST segment monitoring in the coronary care unit. are there sex-related differences. Heart Lung. 1999; 28(2):81–86.
2. Adams, MG, Pelter, MM, Wung, SF, et al, Frequency of silent myocardial ischemia with 12-lead ST segment monitoring in the coronary care unit. are there sex-related differences. Heart Lung. 1999; 28(2):81–86.
![]() 3. Akkerhuis, KM, Klootwijk, PA, Lindeboom, W, et al. Recurrent ischaemia during continuous multilead ST-segment monitoring identifies patients with acute coronary syndromes at high risk of adverse cardiac events; meta-analysis of three studies involving 995 patients. Eur Heart J. 2001; 22(21):1997–2006.
3. Akkerhuis, KM, Klootwijk, PA, Lindeboom, W, et al. Recurrent ischaemia during continuous multilead ST-segment monitoring identifies patients with acute coronary syndromes at high risk of adverse cardiac events; meta-analysis of three studies involving 995 patients. Eur Heart J. 2001; 22(21):1997–2006.
![]() 4. Clochesy, JM, Cifani, L, Howe, K, Electrode site preparation techniques. a follow-up study. Heart Lung. 1991; 20(1):27–30.
4. Clochesy, JM, Cifani, L, Howe, K, Electrode site preparation techniques. a follow-up study. Heart Lung. 1991; 20(1):27–30.
5. Cura, FA, Escudero, AG, Berrocal, D0, et al. Protection of distal embolization in high-risk patients with acute ST-segment elevation myocardial infarction (PREMIAR). Am J Cardiol. 2007; 99(3):357–363.
![]() 6. DeWood, MA, Spores, J, Notske, R, et al. Prevalence of -total coronary occlusion during the early hours of transmural myocardial infarction. N Engl J Med. 1980; 303(16):897–902.
6. DeWood, MA, Spores, J, Notske, R, et al. Prevalence of -total coronary occlusion during the early hours of transmural myocardial infarction. N Engl J Med. 1980; 303(16):897–902.
![]() 7. Drew, BJ, Adams, MG, Clinical consequences of ST-segment changes caused by body position mimicking transient myocardial ischemia. hazards of ST-segment monitoring. J Electrocardiol. 2001; 34(3):261–264.
7. Drew, BJ, Adams, MG, Clinical consequences of ST-segment changes caused by body position mimicking transient myocardial ischemia. hazards of ST-segment monitoring. J Electrocardiol. 2001; 34(3):261–264.
![]() 8. Drew, BJ, Califf, RM, Funk, M, et al, AHA scientifi c statement: practice standards for electrocardiographic monitoring in hospital settings. an American Heart Association Scientifi c Statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young: endorsed by the International Society of Computerized electrocardiology and the American Association of Critical-Care Nurses. J Cardiovasc Nurs. 2005; 20(2):76–106.
8. Drew, BJ, Califf, RM, Funk, M, et al, AHA scientifi c statement: practice standards for electrocardiographic monitoring in hospital settings. an American Heart Association Scientifi c Statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young: endorsed by the International Society of Computerized electrocardiology and the American Association of Critical-Care Nurses. J Cardiovasc Nurs. 2005; 20(2):76–106.
![]() 9. Drew, BJ, Krucoff, MW, Multilead ST-segment monitoring in patients with acute coronary syndromes. a consensus statement for healthcare professionals ST-Segment Monitoring Practice Guideline International Working Group,. Am J Crit Care. 1999; 8(6):372–388.
9. Drew, BJ, Krucoff, MW, Multilead ST-segment monitoring in patients with acute coronary syndromes. a consensus statement for healthcare professionals ST-Segment Monitoring Practice Guideline International Working Group,. Am J Crit Care. 1999; 8(6):372–388.
![]() 10. Drew, BJ, Pelter, MM, Adams, MG. Frequency, characteristics, and clinical significance of transient ST segment elevation in patients with acute coronary syndromes. Eur Heart J. 2002; 23(12):941–947.
10. Drew, BJ, Pelter, MM, Adams, MG. Frequency, characteristics, and clinical significance of transient ST segment elevation in patients with acute coronary syndromes. Eur Heart J. 2002; 23(12):941–947.
![]() 11. Drew, BJ, Pelter, MM, Lee, E, et al, Designing prehospital ECG systems for acute coronary syndromes. lessons learned from clinical trials involving 12-lead ST-segment monitoring. J Electrocardiol. 2005; 38(4 Suppl):180–185.
11. Drew, BJ, Pelter, MM, Lee, E, et al, Designing prehospital ECG systems for acute coronary syndromes. lessons learned from clinical trials involving 12-lead ST-segment monitoring. J Electrocardiol. 2005; 38(4 Suppl):180–185.
![]() 12. Drew, BJ, Wung, SF, Adams, MG, et al, Bedside diagnosis of myocardial ischemia with ST-segment monitoring technology. measurement issues for real-time clinical decision making and trial designs . J Electrocardiol . 1998; 30:157–165. [(Suppl)].
12. Drew, BJ, Wung, SF, Adams, MG, et al, Bedside diagnosis of myocardial ischemia with ST-segment monitoring technology. measurement issues for real-time clinical decision making and trial designs . J Electrocardiol . 1998; 30:157–165. [(Suppl)].
![]() 13. Gottlieb, SO, Weisfeldt, ML, Ouyang, P, et al. Silent ischemia as a marker for early unfavorable outcomes in patients with unstable angina. N Engl J Med. 1986; 314(19):1214–1219.
13. Gottlieb, SO, Weisfeldt, ML, Ouyang, P, et al. Silent ischemia as a marker for early unfavorable outcomes in patients with unstable angina. N Engl J Med. 1986; 314(19):1214–1219.
![]() 14. Krucoff, MW, Croll, MA, Pope, JE, et al. Continuously updated 12-lead ST-segment recovery analysis for myocardial infarct artery patency assessment and its correlation with multiple simultaneous early angiographic observations. Am J Cardiol. 1993; 71(2):145–151.
14. Krucoff, MW, Croll, MA, Pope, JE, et al. Continuously updated 12-lead ST-segment recovery analysis for myocardial infarct artery patency assessment and its correlation with multiple simultaneous early angiographic observations. Am J Cardiol. 1993; 71(2):145–151.
![]() 15. Medina, V, Clochesy, JM, Omery, A. Comparison of electrode site preparation techniques. Heart Lung. 1989; 18(5):456–460.
15. Medina, V, Clochesy, JM, Omery, A. Comparison of electrode site preparation techniques. Heart Lung. 1989; 18(5):456–460.
![]() 16. Pelter, MM, Adams, MG, Drew, BJ. Transient myocardial ischemia is an independent predictor of adverse in-hospital outcomes in patients with acute coronary syndromes treated in the telemetry unit. Heart Lung. 2003; 32(2):71–78.
16. Pelter, MM, Adams, MG, Drew, BJ. Transient myocardial ischemia is an independent predictor of adverse in-hospital outcomes in patients with acute coronary syndromes treated in the telemetry unit. Heart Lung. 2003; 32(2):71–78.
17. Shusterman, V, Goldberg, A, Schindler, DM, et al. Dynamic tracking of ischemia in the surface electrocardiogram. J Electrocardiol. 2007; 40(6 Suppl):S179–S186.
18. Stephens, KE, Anderson, H, Carey, MG, et al, Interpreting 12-lead electrocardiograms for acute ST-elevation myocardial infarction. what nurses know. J Cardiovasc Nurs. 2007; 22(3):186–193.
![]() 19. Stone, GW, Webb, J, Cox, DA, et al, Distal microcirculatory protection during percutaneous coronary intervention in acute ST-segment elevation myocardial infarction. a randomized controlled trial. JAMA. 2005; 293(9):1063–1072.
19. Stone, GW, Webb, J, Cox, DA, et al, Distal microcirculatory protection during percutaneous coronary intervention in acute ST-segment elevation myocardial infarction. a randomized controlled trial. JAMA. 2005; 293(9):1063–1072.
![]() Adams, MG, Pelter, MM, hospital cardiac monitoring Conover M, ed.. Understanding electrocardiography. ed 8. Mosby, St Louis, 2003:431–443.
Adams, MG, Pelter, MM, hospital cardiac monitoring Conover M, ed.. Understanding electrocardiography. ed 8. Mosby, St Louis, 2003:431–443.
![]() Adams-Hamoda MG, et al, Factors to consider when analyzing 12-lead electrocardiograms for evidence of acute myocardial ischemia . Am J Crit Care 2003; 12:9–18.
Adams-Hamoda MG, et al, Factors to consider when analyzing 12-lead electrocardiograms for evidence of acute myocardial ischemia . Am J Crit Care 2003; 12:9–18.
Wagner, GS, Marriott’s practical electrocardiology . ed 11 . 2008 . Lippincott Williams & Wilkins: Philadelphia.