Extra Electrocardiographic Leads: Right Precordial and Left Posterior Leads
PREREQUISITE NURSING KNOWLEDGE
• Understanding of the anatomy and physiology of the cardiovascular system, basic rhythm interpretation, and electrical safety is necessary.
• Advanced cardiac life support knowledge and skills are needed.
• Familiarity with principles of electrophysiology is needed.
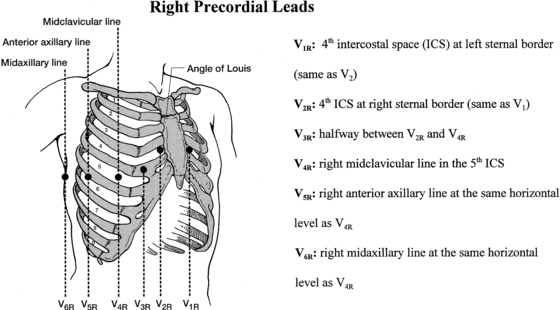
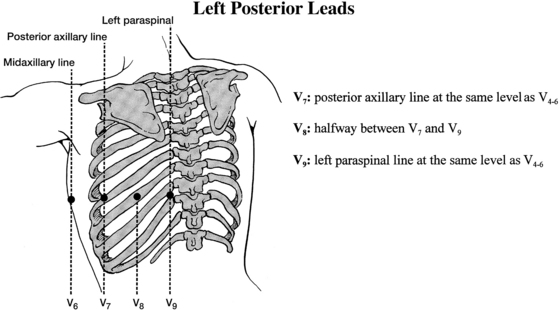
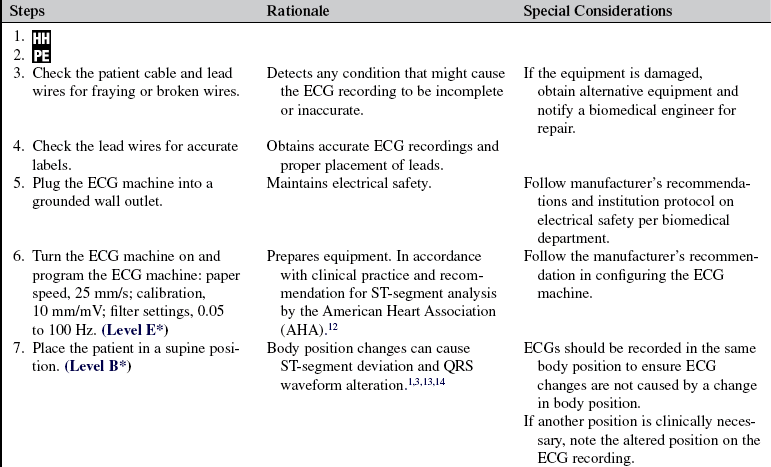
• The right ventricular (RV) leads V1R through V6R and left posterior leads V7 through V9 are unipolar leads in which the chest electrode serves as the “exploring” electrode or positive pole of the lead. These precordial leads view the heart from the vantage point of their electrode positions on the chest, similar to the standard precordial leads V1 through V6.
• For recordings of RV or left posterior leads, the three limb electrodes (right arm [RA], left arm [LA], left leg [LL]) also are required to create a central terminal (negative pole); one limb electrode (right leg [RL]) serves as the ground lead and is used to stabilize the electrocardiographic (ECG) recording.
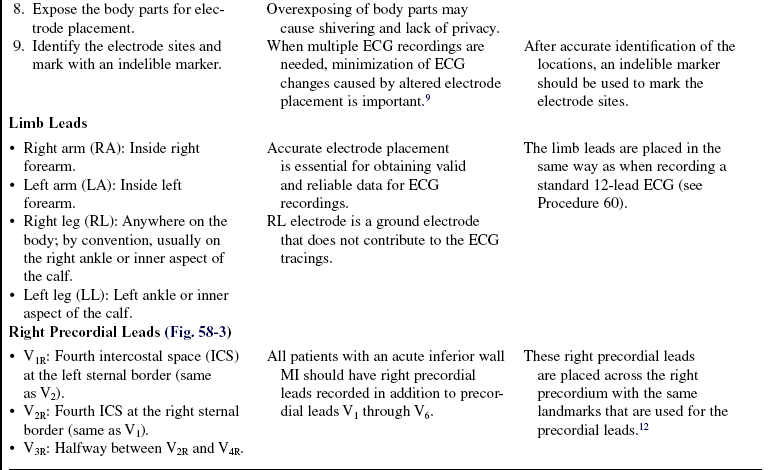
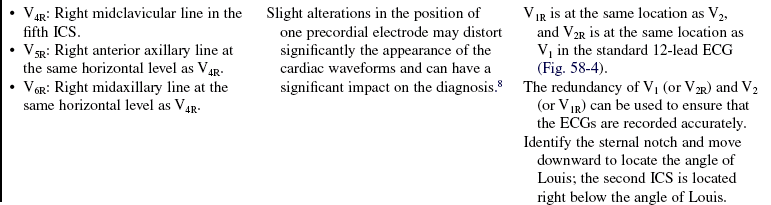
• Accuracy in identification of anatomic landmarks for location of electrode sites and knowledge of the importance of accurate electrode placement are needed. Nurses must locate accurately the electrode positions for the standard 12-lead ECG because the same anatomic landmarks are used to locate the RV and left posterior leads. Accurate ECG interpretation is possible only when the recording electrodes are placed in the proper positions. Slight alterations of the electrode positions may distort significantly the appearance of the ECG waveforms and can lead to misdiagnosis.9 Reliable comparison of serial (more than two ECGs recorded at different times) ECG recordings relies on accurate and consistent electrode placement. An indelible marker is recommended for use with clear identification of the electrode locations to ensure that the same electrode locations are selected when serial ECGs are recorded.
• Nurses should be aware of body positional changes that can alter ECG recordings. Serial ECGs should be recorded with the patient in a supine position to ensure that all recordings are done in a consistent manner. Side-lying positions and elevation of the torso may change the position of the heart within the chest and can change the waveforms on the ECG recording.2,3 If a position other than supine is clinically necessary, notation of the altered position should be made on the tracing.
• Right precordial leads are useful in diagnosis of a RV myocardial infarction (MI).
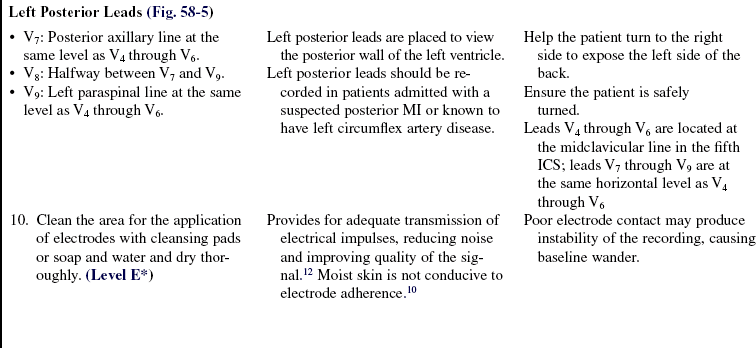
v. These RV leads are important because they enable clinicians to identify patients with an acute MI who are at high risk of atrioventricular (AV) conduction disturbances,4 to predict the site of coronary artery occlusion, and to guide appropriate hemodynamic monitoring and interventions. Left posterior leads are used to aid in the detection of posterior wall MI and to facilitate timely reperfusion treatment. Recording of left posterior leads also can help in the differential diagnosis of tall R waves in lead V1 and V2.6
• Nurses should be able to operate the 12-lead ECG machine. Calibration of 1 mV equals 10 mm and paper speed of 25 mm/s are standards used in clinical practice. For ST-segment analysis, filter settings of 0.05 to 100 Hz are recommended by the American Heart Association.12 Any variation used for particular clinical purposes should be noted on the tracing. Specific information regarding configuring the ECG machine, troubleshooting, and safety features is available from the manufacturer and should be read before use of the equipment.
• Nurses should be able to interpret recorded ECGs for the presence or absence of myocardial ischemia, MI, and dysrhythmias so that patients can be treated appropriately. Patients with an acute inferior MI and RV involvement, determined by ST-segment elevation in the right precordial leads, are at high risk for high-degree AV block. Nurses should monitor patients closely for conduction disturbances and anticipate the need for temporary pacing. Patients with RV infarction are prone to hypotension and shock that responds to treatment with fluid resuscitation.
• Indications for recording a right precordial ECG are as follows:
v. Evaluation and treatment of suspected acute MI, especially patients with inferior wall MI (ST-segment elevation in leads II, III, and augmented vector foot or aVF)
v. Evaluation of the risk for AV node conduction disturbances and anticipation of treatment plans
v. Prediction of the site of coronary artery occlusion (RV infarction occurs with proximal right coronary artery [RCA] occlusion)
v. Determination of the risk of “volume-responsive” shock, in which case fluid resuscitation is warranted and vasodilators (e.g., nitroglycerin) are contraindicated
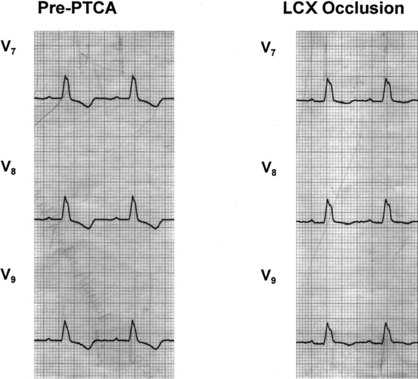
• Indications for recording a left posterior ECG are as follows:
v. Evaluation and treatment of acute or suspected MI, especially patients with isolated ST-segment depression in the precordial leads V1 through V3 and patients with a nondiagnostic ECG
v. Presence of chest pain or anginal-equivalent symptoms (e.g., jaw, left shoulder or arm discomfort, or shortness of breath) or ST-segment depression in the left precordial leads V1 through V3 after percutaneous coronary interventions of the left circumflex artery
v. Any of these ECG characteristics indicative of posterior MI in lead V1: R waves greater than or equal to 6 mm in height, R wave greater than or equal to 40 ms in duration, R/S ratio (R wave amplitude in mm over S wave amplitude in mm) greater than or equal to 1, or S wave less than or equal to 3 mm. In lead V2: R wave greater than or equal to 15 mm in height, R wave greater than or equal to 50 ms in duration, R/S ratio greater than or equal to 1.5, or S wave less than or equal to 4 mm.11
v. Differentiation of true posterior MI from other conditions that can cause tall R waves in lead V1, such as RV hypertrophy, right bundle-branch block, Wolff-Parkinson-White syndrome, and ventricular septal hypertrophy
• In patients with RV infarction who exhibit shock, volume expansion is used to provide adequate RV and left ventricular filling pressures and to restore arterial pressure and peripheral blood flow. Positive inotropic agents also may be indicated to augment the residual contractile force of the damaged RV. Use of vasodilators (e.g., nitroglycerin) should generally be avoided because they cause venous dilation and reduced preload. Use of diuretics (e.g., furosemide). Diuretics should be avoided because they reduce preload and left ventricular filling.7
EQUIPMENT
• Dry gauze pads or terrycloth washcloth
• Cleansing pads or nonemollient soap and water
• 12-lead ECG machine with attached patient cable and lead wires
Additional equipment to have available as needed includes the following:
PATIENT AND FAMILY EDUCATION
• Describe the procedure and reasons for obtaining extra ECG leads. Reassure the patient that the procedure is painless.  Rationale: This communication clarifies information, reduces anxiety, and gains cooperation from the patient.
Rationale: This communication clarifies information, reduces anxiety, and gains cooperation from the patient.
• Explain the patient’s role in assisting with the ECG recording and emphasize actions that improve the quality of the ECG tracing, such as relaxing, avoiding conversation and body movement, and breathing normally.  Rationale: This explanation ensures the patient’s cooperation to improve the quality of the tracing and avoids unnecessary repeating of ECGs because of muscle artifact.
Rationale: This explanation ensures the patient’s cooperation to improve the quality of the tracing and avoids unnecessary repeating of ECGs because of muscle artifact.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Interpret previously recorded ECGs.  Rationale: Each patient has an individual baseline ECG. Previous ECG recordings can help clinicians determine whether a change is acute or chronic.
Rationale: Each patient has an individual baseline ECG. Previous ECG recordings can help clinicians determine whether a change is acute or chronic.
• Assess for the presence of anginal symptoms, such as chest pain, pressure, tightness, heaviness, fullness, or squeezing sensation; radiated pain; shortness of breath, nausea, and extreme fatigue.  Rationale: This evaluation correlates ECG changes with patient symptoms.
Rationale: This evaluation correlates ECG changes with patient symptoms.
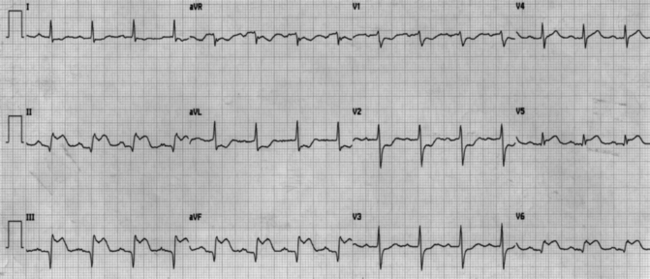
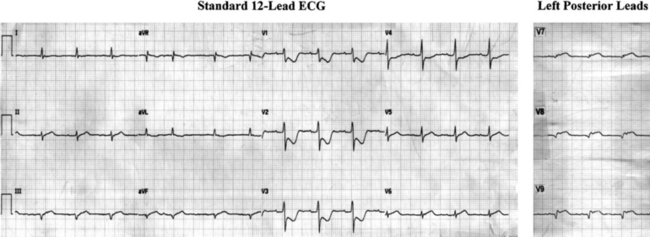
• Assess the patient’s medical history of cardiac diseases, such as MI and medications.  Rationale: Knowledge about the patient’s cardiac history and medications can help in interpretation of ECG recordings (Fig. 58-1). For example, digitalis therapy causes chronic ST-segment depression that does not indicate ischemia. A normal-looking isoelectric ST segment in a patient on digitalis therapy may indicate acute ischemia. Patients with a prior posterior MI might have abnormal Q waves in the left posterior leads.
Rationale: Knowledge about the patient’s cardiac history and medications can help in interpretation of ECG recordings (Fig. 58-1). For example, digitalis therapy causes chronic ST-segment depression that does not indicate ischemia. A normal-looking isoelectric ST segment in a patient on digitalis therapy may indicate acute ischemia. Patients with a prior posterior MI might have abnormal Q waves in the left posterior leads.
• Interpret the patient’s standard 12-lead ECG for any signs of myocardial ischemia or MI and dysrhythmias.  Rationale: Nurses should be able to evaluate the standard 12-lead ECG for the location of ischemia or infarction and assess the possibility of RV and posterior involvement (Fig. 58-2).
Rationale: Nurses should be able to evaluate the standard 12-lead ECG for the location of ischemia or infarction and assess the possibility of RV and posterior involvement (Fig. 58-2).
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand preprocedural teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: This communication evaluates and reinforces the understanding of previously taught information.
Rationale: This communication evaluates and reinforces the understanding of previously taught information.
• Assist the patient to the supine position and expose the patient’s torso while maintaining the patient’s modesty.  Rationale: This position enables the recording of a standard 12-lead ECG and allows comparison of serial ECGs and comparison with standard waveforms. Body positional changes, such as elevation and rotation, can change recorded amplitudes and axes.
Rationale: This position enables the recording of a standard 12-lead ECG and allows comparison of serial ECGs and comparison with standard waveforms. Body positional changes, such as elevation and rotation, can change recorded amplitudes and axes.
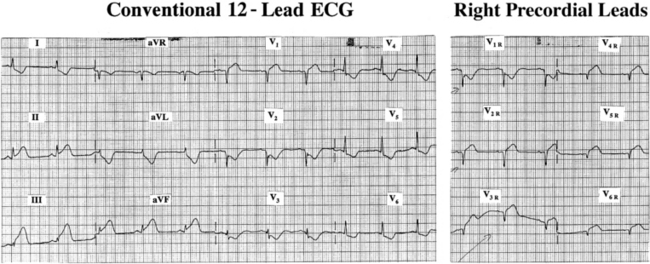
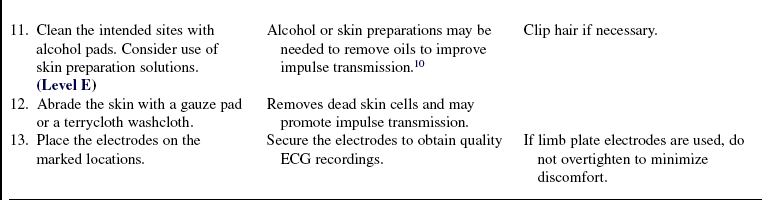
Figure 58-4 ST-segment elevation in leads II, III, and aVF indicates acute inferior wall MI. These characteristics on the standard 12-lead ECG (left panel) suggest RV infarction: diagnosis of an inferior MI; ST-segment elevation in lead III exceeding that of lead II; ST-segment elevation confined to V1 without elevation in the remaining precordial leads; and ST depression in lead aVL.15 Definitive diagnosis of RV infarction is made by observing ST-segment elevation greater than or equal to 1 mm in one or more of the right precordial leads. In the right panel, ST-segment elevation is seen in V2R (V1) through V6R. (From Drew BJ, Ide B: Right ventricular infarction, Prog Cardiovasc Nurs10:46, 1995.)
References
![]() 1. Adams, MG, Drew, BJ, Body position effects on the ECG. implication for ischemia monitoring. J Electrocardiol 1997; 30:285–291.
1. Adams, MG, Drew, BJ, Body position effects on the ECG. implication for ischemia monitoring. J Electrocardiol 1997; 30:285–291.
![]() 2. Adams-Hamoda MG, Caldwell, MA, Stotts, NA, et al. Factors to consider when analyzing 12-lead electrocardiograms for evidence of acute myocardial ischemia. Am J Crit Care. 2003; 12:9–18.
2. Adams-Hamoda MG, Caldwell, MA, Stotts, NA, et al. Factors to consider when analyzing 12-lead electrocardiograms for evidence of acute myocardial ischemia. Am J Crit Care. 2003; 12:9–18.
3. Baevsky, RH, Haber, MD, Blank, FS, et al, Supine vs semirecumbent and upright 12-lead electrocardiogram. does change in body position alter the electrocardiographic -interpretation for ischemia. Am J Emerg Med . 2007; 25:753–756.
![]() 4. Braat, SH, Brugada, P, den Dulk K, et al. Value of lead V4R for recognition of the infarct coronary artery in -acute inferior myocardial infarction. Am J Cardiol. 1984; 53:1538–1541.
4. Braat, SH, Brugada, P, den Dulk K, et al. Value of lead V4R for recognition of the infarct coronary artery in -acute inferior myocardial infarction. Am J Cardiol. 1984; 53:1538–1541.
![]() 5. Braat, SH, Gorgels, AP, Bar, FW, et al. Value of the ST-T segment in lead V4R in inferior wall acute myocardial -infarction to predict the site of coronary arterial occlusion. Am J Cardiol. 1988; 62:140–142.
5. Braat, SH, Gorgels, AP, Bar, FW, et al. Value of the ST-T segment in lead V4R in inferior wall acute myocardial -infarction to predict the site of coronary arterial occlusion. Am J Cardiol. 1988; 62:140–142.
![]() 6. Casas, RE, Marriott, HJ, Glancy, DL. Value of leads -V7-V9 in diagnosing posterior wall acute myocardial -infarction and other causes of tall R waves in V1-V2. Am J Cardiol. 1997; 80:508–509.
6. Casas, RE, Marriott, HJ, Glancy, DL. Value of leads -V7-V9 in diagnosing posterior wall acute myocardial -infarction and other causes of tall R waves in V1-V2. Am J Cardiol. 1997; 80:508–509.
![]() 7. Cohn, JN, Guiha, NH, Broder, MI, et al, Right ventricular infarction. clinical and hemodynamic features. Am J Cardiol 1974; 33:209–214.
7. Cohn, JN, Guiha, NH, Broder, MI, et al, Right ventricular infarction. clinical and hemodynamic features. Am J Cardiol 1974; 33:209–214.
8. Drew, BJ. Pitfalls and artifacts in electrocardiography. Cardiol Clin. 2006; 24:309–315. [vii].
9. Drew, BJ. Pseudo myocardial injury patterns because -of nonstandard electrocardiogram electrode placement. J Electrocardiol. 2008; 41:202–204.
![]() 10. Drew, BJ, et al, Practice standards for electrocardiographic monitoring in hospital settings. an American Heart Association Scientific Statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young. Circulation 2004; 110:2721–2746.
10. Drew, BJ, et al, Practice standards for electrocardiographic monitoring in hospital settings. an American Heart Association Scientific Statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young. Circulation 2004; 110:2721–2746.
![]() 11. Haisty, WK, Jr., Pahlm, O, Wagner, NB, et al. Performance of the automated complete Selvester QRS scoring system in normal subjects and patients with single and multiple myocardial infarctions. J Am Coll Cardiol. 1992; 19:341–346.
11. Haisty, WK, Jr., Pahlm, O, Wagner, NB, et al. Performance of the automated complete Selvester QRS scoring system in normal subjects and patients with single and multiple myocardial infarctions. J Am Coll Cardiol. 1992; 19:341–346.
12. Kligfield, P, Gettes, LS, Bailey, JJ, et al, Recommendations for the standardization and interpretation of the electrocardiogram: part I. the electrocardiogram and its technology: a scientifi c statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology; the American College of Cardiology Foundation; and the Heart Rhythm Society: endorsed by the International Society for Computerized Electrocardiology. Circulation 2007; 115:1306–1324.
![]() 13. Nelwan, SP, Meij, SH, van Dam TB, et al. Correction of ECG variations caused by body position changes and electrode placement during ST-T monitoring. J Electrocardiol. 2001; 34:213–216. [(Suppl)].
13. Nelwan, SP, Meij, SH, van Dam TB, et al. Correction of ECG variations caused by body position changes and electrode placement during ST-T monitoring. J Electrocardiol. 2001; 34:213–216. [(Suppl)].
![]() 14. Pharand, C, Nasmith, JB, Rajaonah, JC, et al, Distinction between myocardial ischemia and postural changes in continuous ECG monitoring based on ST-segment amplitude and vector orientation. preliminary results. Can J Cardiol 2003; 19:1023–1029.
14. Pharand, C, Nasmith, JB, Rajaonah, JC, et al, Distinction between myocardial ischemia and postural changes in continuous ECG monitoring based on ST-segment amplitude and vector orientation. preliminary results. Can J Cardiol 2003; 19:1023–1029.
15. Wung, SF. Discriminating between right coronary artery and circumflex artery occlusion by using a noninvasive 18-lead electrocardiogram. Am J Crit Care. 2007; 16:63–71.