Electrocardiographic Leads and Cardiac Monitoring
PREREQUISITE NURSING KNOWLEDGE
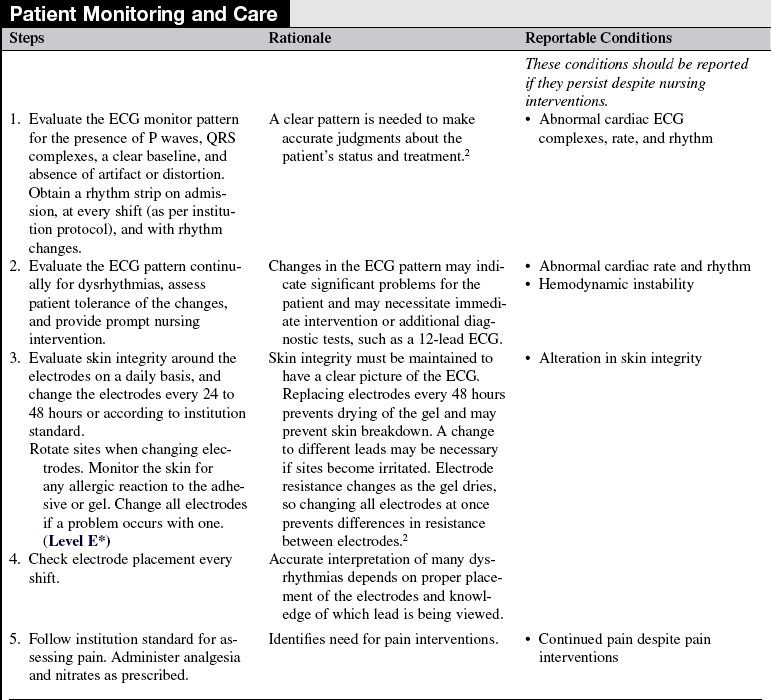
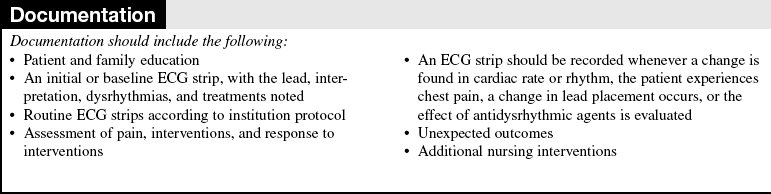
• Knowledge of the anatomy and physiology of the cardiovascular system, principles of cardiac conduction, principles of electrophysiology, electrocardiogram (ECG) lead placement, basic dysrhythmia interpretation, and electrical safety is necessary.
• Advanced cardiac life support knowledge and skills are needed.
• Electrophysiologic monitoring with hardwire and telemetry is indicated for all patients in critical care units and for patients in selected acute care settings, postanesthesia areas, operating rooms, and emergency departments.
• Electrophysiologic monitoring is designed to give a graphic display of the electrical activity in the heart generated by depolarization and repolarization of cardiac tissue.
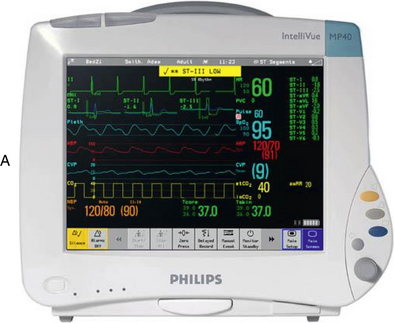
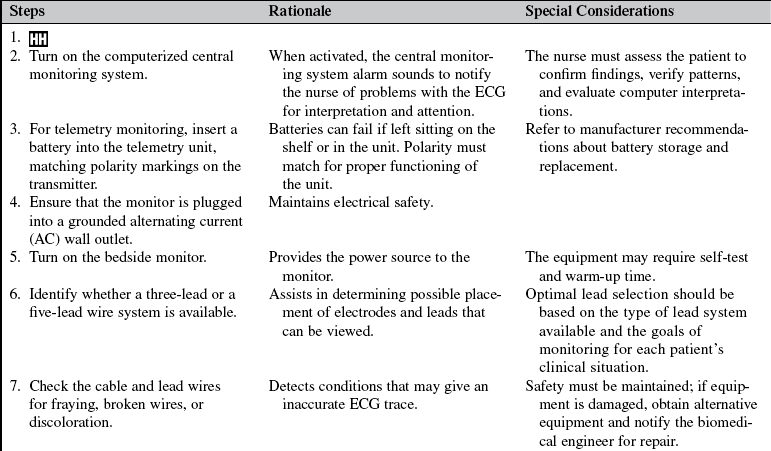
• Hardwire ECG monitors have electrodes and lead wires that are attached directly to the patient. Impulses are transmitted directly from the patient to the monitor (Fig. 57-1).
• Telemetry systems have electrodes and lead wires that are attached from the patient to a battery pack and transmit impulses to the monitor via radio wave transmission (Fig. 57-2).
• Telemetry is useful in progressive ambulation and evaluation of activity tolerance. A disadvantage to telemetry is that ambulation and activity can increase distortion of the ECG pattern.
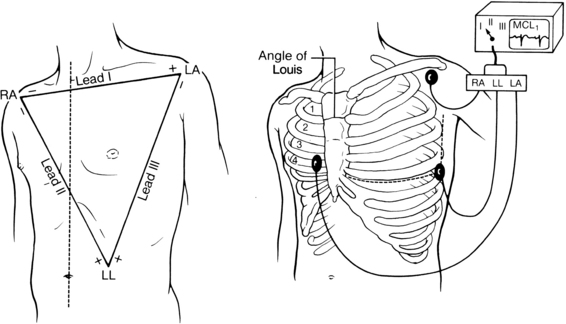
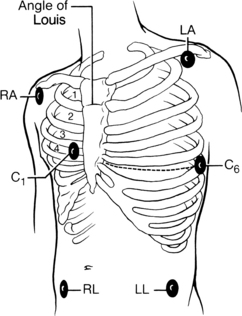
• Specific areas of the chest are used for electrode placement to obtain a view of the electrical activity in a particular area of the heart (commonly called a lead).
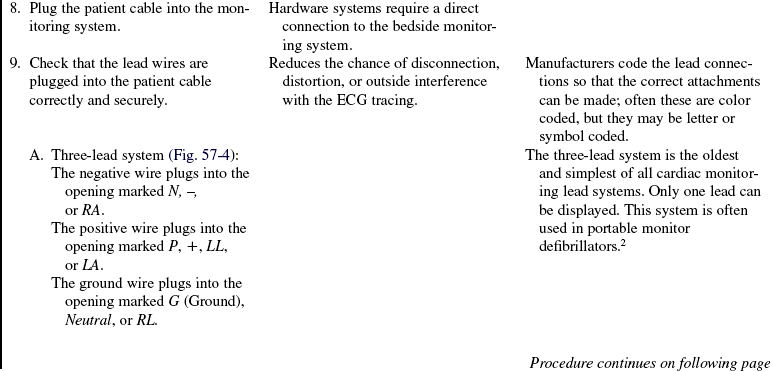
• ECG monitors use a three-lead or five-lead wire system to provide different views (leads) of the heart’s electrical activity. Most acute and critical care units use a five-lead system for continuous bedside monitoring or telemetry.
• Standardized placement of leads is important so that information obtained is assessed within a common frame of reference and so that appropriate judgments can be made on the patient’s cardiac status. Alterations of electrode position may distort the appearance of the waveform significantly and can lead to misdiagnosis or mistreatment.
• The two major factors that determine the views of the ECG deflection on the monitor are the location of the electrodes on the body and the direction of the cardiac impulse in relation to the position of the electrode.
• A basic rule of electrocardiography is the rule of electrical flow. This rule notes that if electricity flows toward the positive electrode, an upright pattern is produced on the monitor or graph paper. If the electricity flows away from the positive electrode (or toward the negative electrode), a downward pattern or deflection is produced on the monitor or graph paper. Lead wires attached to the patient are coded (+, P [positive]; or –, N [negative]; RA [right arm]; RL [right leg]; LA [left arm]; LL [left leg]; V or C [V or precordial vector and C or chest lead] in some way for ease in correct placement. Placement of the leads gives different views of the electrical conduction through the heart.
• Information from the bedside via hardwire or telemetry can be transferred to a central monitor, where it can be printed, stored, and analyzed (Fig. 57-3).
• Five-lead bedside monitoring systems provide a continuous readout of two or more leads simultaneously. This readout provides more information and a comparison of the ECG patterns. Optimal lead selection is based on the goals of monitoring for each patient’s clinical situation.
• Bedside electrophysiologic monitoring may also provide continuous derived 12-lead ECG acquisition via a torso-positioned reduced lead system (e.g., the EASI lead system; Philips Monitoring, Andover, MA). In this application, the reduced lead configuration varies according to the manufacturer and the device but provides the availability of a continuous 12-lead ECG, which can be accessed for information over a predetermined time (commonly 24 to 48 hours). This application greatly expands the information available from bedside monitors and requires accurate and consistent lead placement based on the manufacturer’s requirements. Derived ECGs are not equivalent to standard 12-lead ECGs and are not recommended as a substitute.1
EQUIPMENT
• ECG monitor (central and bedside monitor) or battery pack (telemetry monitoring only)
• Electrodes, pregelled and disposable
• Dry gauze pads or terrycloth washcloth
• Cleansing pads or nonemollient soap and water
• Lead wires (no longer than 18 inches)
• Patient cable (should be compatible with the monitor and the lead wires)
• ECG calipers (may be available electronically via the central monitor)
Additional equipment to have available as needed includes the following:
PATIENT AND FAMILY EDUCATION
• Assess the readiness of the patient and family to learn.  Rationale: Anxiety and concerns of the patient and family may inhibit the ability to learn.
Rationale: Anxiety and concerns of the patient and family may inhibit the ability to learn.
• Provide explanations of the equipment and alarms to the patient and family.  Rationale: These explanations assist in making the patient and family feel more comfortable with monitoring and may reduce anxiety.
Rationale: These explanations assist in making the patient and family feel more comfortable with monitoring and may reduce anxiety.
• Reassure the patient and family that monitoring is continuous and that the patient’s heart rate and rhythm will be monitored and treated as indicated.  Rationale: The patient and family are reassured that immediate care is available.
Rationale: The patient and family are reassured that immediate care is available.
• Emphasize that the patient should feel free to move about in bed.  Rationale: This emphasis encourages movement on the part of the patient and allays fears about disruption of the monitoring system.
Rationale: This emphasis encourages movement on the part of the patient and allays fears about disruption of the monitoring system.
• Explain the importance of reporting any symptoms, such as pain, dizziness, palpitations, or chest discomfort.  Rationale: Reporting of symptoms ensures appropriate and timely assessment and intervention.
Rationale: Reporting of symptoms ensures appropriate and timely assessment and intervention.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess the patient’s peripheral pulses, vital signs, heart sounds, level of consciousness, lung sounds, neck vein distention, presence of chest pain or palpitations, and any peripheral circulatory disorders (i.e., decreased pulses, clubbing, cyanosis, and dependent edema).  Rationale: This assessment provides baseline assessment data.
Rationale: This assessment provides baseline assessment data.
• Assess whether the patient has a history of cardiac dysrhythmias or cardiac problems.  Rationale: The history provides baseline data and may guide selection of monitoring leads.
Rationale: The history provides baseline data and may guide selection of monitoring leads.
• Assess landmarks for identification of correct placement of electrodes.  Rationale: This assessment ensures accurate placement of leads for accurate interpretation.
Rationale: This assessment ensures accurate placement of leads for accurate interpretation.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand preprocedural teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: This communication evaluates and reinforces the understanding of previously taught information.
Rationale: This communication evaluates and reinforces the understanding of previously taught information.
• Assist the patient to the supine position.  Rationale: This position enables easy access to the chest for electrode placement.
Rationale: This position enables easy access to the chest for electrode placement.
• Assist the patient in removing clothing that covers the chest while providing for the patient’s privacy.  Rationale: Clothing removal provides a clear view of the chest and allows for identification of landmarks and proper placement of leads while the patient’s privacy is maintained.
Rationale: Clothing removal provides a clear view of the chest and allows for identification of landmarks and proper placement of leads while the patient’s privacy is maintained.
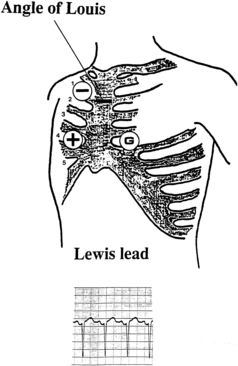
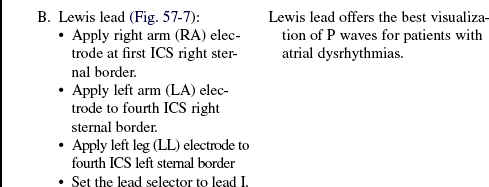
Figure 57-7 Three-lead system with Lewis lead.
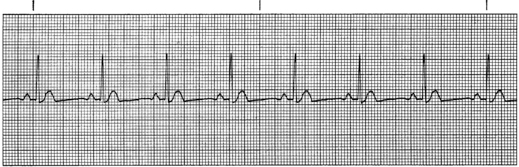
Figure 57-9 Monitor strip of clear ECG pattern.

Figure 57-10 Monitor strip with 60-cycle interference.
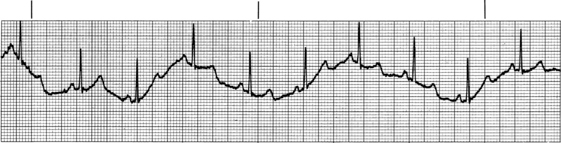
Figure 57-11 Monitor strip with erratic baseline.

Figure 57-12 Monitor strip with interference.
References
1. AACN, AACN practice alert, dysrhythmia monitoring. 2008 . American Association of Critical Care: Aliso Viejo, CA.
![]() 2. Drew, BJ, et al, Practice standards for electrocardiographic monitoring in hospital settings. an American Heart Association scientific statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young. Circulation 2004; 110:2721–2746.
2. Drew, BJ, et al, Practice standards for electrocardiographic monitoring in hospital settings. an American Heart Association scientific statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Young. Circulation 2004; 110:2721–2746.
3. Kligfield, P, et al, Recommendations for the standardization and interpretation of the electrocardiogram: . part 1: the electrocardiogram and its technology: a scientifi c statement from the American Heart Association Electrocardiography and Arrhythmias Committee, Council on Clinical Cardiology: The American College of Cardiology Foundation; and the Heart Rhythm -Society. Circulation 2007; 115:1306–1324.
Leeper, B. Continuous ST-segment monitoring. AACN Clin Issues. 2003; 14:145–154.
Alspach, J. Core curriculum for critical care nursing. Philadelphia: Saunders; 2006.
Donnely, MP, et al, Lead selection. old and new methods -for locating the most electrocardiogram information. J Electrocardiol 2008; 41:257–263.
Drew, BJ, Kingfield, P, Standardizing electrocardiograpic leads. introduction to a symposium. J Electrocardiol 2008; 41:187–189.
Drew, BJ, Putting it all together. case studies on ECG -monitoring. AACN Adv Crit Care 2007; 18:305–317.
Drew, BJ. Pitfalls and artifacts in electrocardiography. Cardiol Clin. 2006; 24:309–315.
Drew, BJ, et al, Practice standards for ECG monitoring in hosptial settings. executive summary and guide for implementation. Crit Care Nurs Clin North Am 2006; 18:157–168.
![]() Jahrsdoerfer, M, et al. Clinical usefulness of the EASI -12-continuous electrographic monitoring system. Crit Care Nurse. 2005; 25:28–38.
Jahrsdoerfer, M, et al. Clinical usefulness of the EASI -12-continuous electrographic monitoring system. Crit Care Nurse. 2005; 25:28–38.
![]() Sole, M, Klein, D, Moseley, M. Introduction to critical care nursing, ed 4. Philadelphia: Saunders; 2004.
Sole, M, Klein, D, Moseley, M. Introduction to critical care nursing, ed 4. Philadelphia: Saunders; 2004.