Intraaortic Balloon Pump Management
PREREQUISITE NURSING KNOWLEDGE
• Knowledge of the anatomy and physiology of the cardiovascular system is needed.
• Understanding of the principles of hemodynamic monitoring, electrophysiology, dysrhythmias, and coagulation is necessary.
• Clinical and technical competence related to the use of the intra-aortic balloon pump (IABP) is needed.
• Advanced cardiac life support knowledge and skills are necessary.
• Indications for IABP therapy are as follows:
 Acute myocardial infarction (MI) complicated by left ventricular failure3,12,26,28
Acute myocardial infarction (MI) complicated by left ventricular failure3,12,26,28
 Recurrent ventricular dysrhythmias as a result of ischemia16
Recurrent ventricular dysrhythmias as a result of ischemia16
 Support before, during, and after coronary artery bypass graft surgery2,29
Support before, during, and after coronary artery bypass graft surgery2,29
 Support before, during, and after coronary artery angioplasty or additional interventional cardiology procedures for patients at high risk4,11
Support before, during, and after coronary artery angioplasty or additional interventional cardiology procedures for patients at high risk4,11
 Mechanical complications of acute MI, including aortic stenosis, mitral stenosis, mitral valvuloplasty, mitral insufficiency, ventricular septal defect, and left ventricular aneurysm
Mechanical complications of acute MI, including aortic stenosis, mitral stenosis, mitral valvuloplasty, mitral insufficiency, ventricular septal defect, and left ventricular aneurysm
 Intractable ventricular dysrhythmias13,18
Intractable ventricular dysrhythmias13,18
 Bridge to cardiac transplantation, ventricular assist devices, or total artificial hearts
Bridge to cardiac transplantation, ventricular assist devices, or total artificial hearts
 Cardiac injury, including contusion and coronary artery tears
Cardiac injury, including contusion and coronary artery tears
• Contraindications to IABP therapy are as follows:
• The relative value of IABP therapy in the presence of severe aortoiliac disease, major coagulopathies, and terminal disease should be evaluated individually.
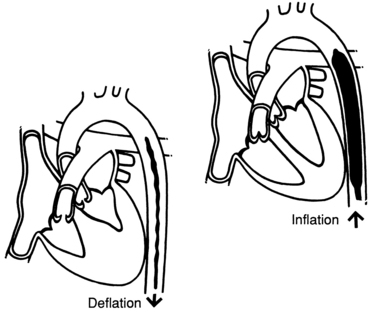
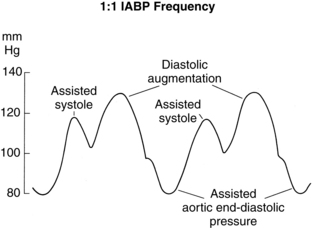
• IABP therapy is an acute short-term therapy for patients with reversible left ventricular failure or an adjunct to other therapies for irreversible heart failure. Cardiac assistance with the IABP is performed to improve myocardial oxygen supply and reduce cardiac workload. Intra-aortic balloon (IAB) pumping is based on the principles of counterpulsation (Fig. 55-1).
• The events of the cardiac cycle provide the stimulus for balloon function, and the movement of helium gas between the balloon and the control console gas source produces inflation and deflation of the balloon.
• Recognition of the R wave or the QRS complex on the electrocardiogram (ECG) is the most commonly used trigger source.
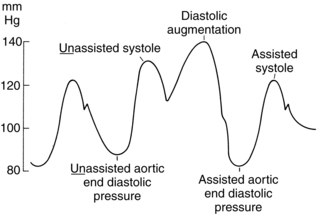
• Inflation occurs during ventricular diastole and causes an increase in aortic pressure. This increased pressure displaces blood proximally to the coronary arteries and distally to the rest of the body. The result is an increase in myocardial oxygen supply and subsequent improvement in cardiac output.
• Deflation occurs just before ventricular systole or ejection, which decreases the pressure within the aortic root, reducing afterload and cardiac workload.
• Insertion and placement verification:
 The IAB catheter is commonly placed in the femoral artery via percutaneous puncture or arteriotomy.
The IAB catheter is commonly placed in the femoral artery via percutaneous puncture or arteriotomy.
 The IAB catheter can also be placed via a transthoracic approach.15
The IAB catheter can also be placed via a transthoracic approach.15
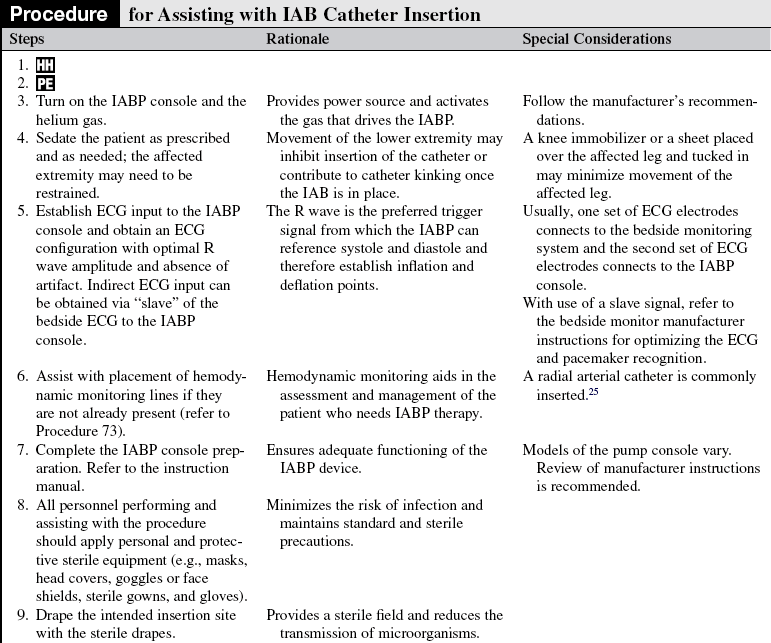
 The IAB catheter lies approximately 2 cm inferior to the left subclavian artery and superior to the renal arteries. This position allows for maximum balloon effect without occlusion of other arterial supplies (Fig. 55-2).
The IAB catheter lies approximately 2 cm inferior to the left subclavian artery and superior to the renal arteries. This position allows for maximum balloon effect without occlusion of other arterial supplies (Fig. 55-2).
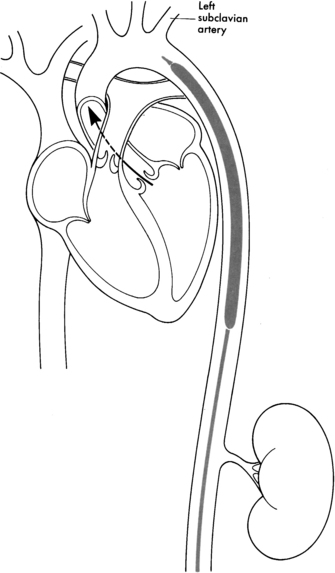
Figure 55-2 Intra-aortic balloon positioned in the descending thoracic aorta, just below the left subclavian artery but above the renal artery. (From Quaal SJ: Comprehensive intraaortic balloon counterpulsation, ed 2, St Louis, 1993, Mosby.)
 The IAB should not fully occlude the aorta during inflation. It should be 85% to 90% occlusive.
The IAB should not fully occlude the aorta during inflation. It should be 85% to 90% occlusive.
 Fluoroscopy may be used to aid in IAB catheter positioning, especially for patients with a tortuous aorta.
Fluoroscopy may be used to aid in IAB catheter positioning, especially for patients with a tortuous aorta.
 Correct catheter position is verified via radiography if fluoroscopy is not used during catheter insertion. The visibility of the IAB catheter tip may be enhanced when the IABP is temporarily placed on standby (follow manufacturer’s guidelines).
Correct catheter position is verified via radiography if fluoroscopy is not used during catheter insertion. The visibility of the IAB catheter tip may be enhanced when the IABP is temporarily placed on standby (follow manufacturer’s guidelines).
 The central lumen of many IAB catheters provides a means for monitoring aortic pressure.
The central lumen of many IAB catheters provides a means for monitoring aortic pressure.
 Some IAB catheters use fiberoptic technology. These catheters have a fiberoptic sensor located at the tip of the IAB catheter. The sensor transmits the pressure signal to the IAB console.
Some IAB catheters use fiberoptic technology. These catheters have a fiberoptic sensor located at the tip of the IAB catheter. The sensor transmits the pressure signal to the IAB console.
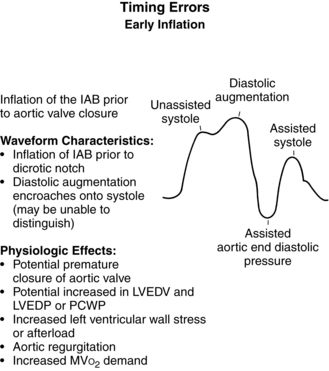
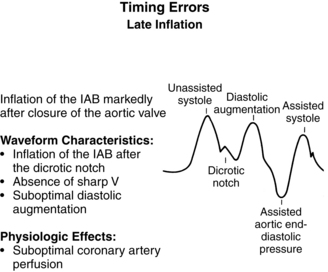
• Timing methods of IABP therapy vary slightly from manufacturer to manufacturer. With the traditional or conventional method, the IAB deflates at the QRS complex, before isovolumetric contraction. The IAB also deflates at the QRS complex with the real-time method. An important principle of real timing is the duration of the balloon deflation during cardiac systole. During real timing, the IAB is timed to deflate at the onset of each QRS complex and to remain deflated throughout systole. A constant diastolic interval is not necessary for real timing.5,6,19,22
• The mechanics of the IABP control console vary from manufacturer to manufacturer.
• Specific information concerning controls, alarms, troubleshooting, and safety features is available from each manufacturer and should be read thoroughly by the nurse before use of the equipment.
EQUIPMENT
• ECG and arterial pressure monitoring supplies
• IAB catheter (size range, 7 Fr to 10 Fr for adults; balloon catheters vary in balloon volumes, 25 to 50 mL)
• Antiseptic solution (e.g., 2% chlorhexidine-based preparation)
• Caps, goggles or face shields, masks, sterile gowns, gloves, and drapes
• O-silk suture on a cutting needle or a sutureless securement device
• No. 11 scalpel, used for skin entry
• 1% Lidocaine without epinephrine, one 30-mL vial
• Stopcocks, one two-way and one three-way
• 500 mL of normal saline flush solution (refer to institution standards or physician prescription regarding use of a heparin flush solution)
Additional equipment to have available depending on patient status includes the following:
PATIENT AND FAMILY EDUCATION
• Assess patient and family understanding of IABP therapy and the reason for its use.  Rationale: Clarification or reinforcement of information is an expressed family need during times of stress and anxiety.
Rationale: Clarification or reinforcement of information is an expressed family need during times of stress and anxiety.
• Explain the standard care to the patient and family, including the insertion procedure, IABP sounds, frequency of assessment, alarms, dressings, need for immobility of the affected extremity, expected length of therapy, and parameters for discontinuation of therapy.  Rationale: This explanation encourages the patient and family to ask questions and prepares the patient and family for what to expect.
Rationale: This explanation encourages the patient and family to ask questions and prepares the patient and family for what to expect.
• After catheter removal, instruct the patient to report any warm or wet feeling on the leg and any dizziness or lightheadedness.  Rationale: These feelings may be indicative of bleeding at the insertion site.
Rationale: These feelings may be indicative of bleeding at the insertion site.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess the patient’s medical history, specifically related to competency of the aortic valve, aortic disease, or peripheral vascular disease.  Rationale: This assessment provides baseline data regarding cardiac functioning and identifies contraindications to IABP therapy.
Rationale: This assessment provides baseline data regarding cardiac functioning and identifies contraindications to IABP therapy.
• Assess the patient’s cardiovascular, hemodynamic, peripheral vascular, and neurovascular status.  Rationale: This assessment provides baseline data.
Rationale: This assessment provides baseline data.
• Assess the extremity for the intended IAB catheter placement for the quality and strength of the femoral, popliteal, dorsalis pedal, and posterior tibial pulses.7,27
• Assess the ankle/arm index as follows:
 Record the brachial systolic pressure with a Doppler scan signal.
Record the brachial systolic pressure with a Doppler scan signal.
 Locate the posterior tibial or dorsalis pedalis pulse with a Doppler scan signal.
Locate the posterior tibial or dorsalis pedalis pulse with a Doppler scan signal.
 Apply the blood pressure cuff around the ankle, above the malleolus.
Apply the blood pressure cuff around the ankle, above the malleolus.
 Inflate the cuff to 20 mm Hg above the brachial systolic pressure.
Inflate the cuff to 20 mm Hg above the brachial systolic pressure.
 Note the reappearance of the Doppler scan signal as the cuff deflates.
Note the reappearance of the Doppler scan signal as the cuff deflates.
 Divide the ankle systolic pressure by the brachial systolic pressure to determine the ankle/arm index (normal range, 0.8 to 1.2).
Divide the ankle systolic pressure by the brachial systolic pressure to determine the ankle/arm index (normal range, 0.8 to 1.2).
 Rationale: The IAB catheter is inserted into the vasculature of the extremity that exhibits the best perfusion. Also, this assessment provides baseline data related to peripheral blood flow, which may be compromised by the IAB.
Rationale: The IAB catheter is inserted into the vasculature of the extremity that exhibits the best perfusion. Also, this assessment provides baseline data related to peripheral blood flow, which may be compromised by the IAB.
• Assess the patient’s current laboratory profile, including complete blood count (CBC), platelet count, prothrombin time (PT), partial thromboplastin time (PTT), bleeding time, and international normalized ratio (INR).  Rationale: Provides baseline data. Baseline coagulation studies are helpful in determining the risk for bleeding. Platelet function may be affected by the mechanical trauma from balloon inflation and deflation.
Rationale: Provides baseline data. Baseline coagulation studies are helpful in determining the risk for bleeding. Platelet function may be affected by the mechanical trauma from balloon inflation and deflation.
• Assess for signs and symptoms of cardiac failure that necessitate IABP therapy, including the following:
 Heart rate greater than 110 beats/min
Heart rate greater than 110 beats/min
 Systolic blood pressure less than 90 mm Hg
Systolic blood pressure less than 90 mm Hg
 Mean arterial pressure (MAP) less than 70 mm Hg with vasopressor support
Mean arterial pressure (MAP) less than 70 mm Hg with vasopressor support
 Pulmonary artery occlusion pressure (pulmonary artery wedge pressure) greater than 18 mm Hg
Pulmonary artery occlusion pressure (pulmonary artery wedge pressure) greater than 18 mm Hg
 Decreased mixed venous oxygen saturation (SVO2)
Decreased mixed venous oxygen saturation (SVO2)
 Rationale: Physical signs and symptoms result from the heart’s inability to adequately contract and from inadequate coronary or systemic perfusion.
Rationale: Physical signs and symptoms result from the heart’s inability to adequately contract and from inadequate coronary or systemic perfusion.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand preprocedural teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of previously taught information is evaluated and reinforced.
Rationale: Understanding of previously taught information is evaluated and reinforced.
• Validate that the informed consent form has been signed.  Rationale: Informed consent protects the rights of the patient and makes a competent decision possible for the patient; however, in emergency circumstances, time may not allow the form to be signed.
Rationale: Informed consent protects the rights of the patient and makes a competent decision possible for the patient; however, in emergency circumstances, time may not allow the form to be signed.
• Perform a pre-procedure verification and time out, if non-emergent.  Rationale: Ensures patient safety.
Rationale: Ensures patient safety.
• Validate the patency of central and peripheral intravenous access.  Rationale: Central access is needed for vasopressor administration; peripheral access is needed for fluid administration.
Rationale: Central access is needed for vasopressor administration; peripheral access is needed for fluid administration.
• Place the patient in a supine position and prepare the intended insertion site with an antiseptic solution.  Rationale: Prepares the intended access site and positions the patient for IAB insertion.
Rationale: Prepares the intended access site and positions the patient for IAB insertion.
References
![]() 1. Arafa, OE, et al. Intra-aortic balloon pumping for predominantly right ventricular failure after heart transplantation. Ann Thoracic Surg. 2000; 70:1587–1593.
1. Arafa, OE, et al. Intra-aortic balloon pumping for predominantly right ventricular failure after heart transplantation. Ann Thoracic Surg. 2000; 70:1587–1593.
![]() 2. Arafa, OE, et al, Vascular complications of the intra-aortic balloon pump in patients undergoing open heart operations. 15-year experience. Ann Thoracic Surg 1999; 67:645–651.
2. Arafa, OE, et al, Vascular complications of the intra-aortic balloon pump in patients undergoing open heart operations. 15-year experience. Ann Thoracic Surg 1999; 67:645–651.
![]() 3. Barron, HV, Every, NR, Parson, LS, et al, The use of intraaortic balloon counterpulsation in patients with cardiogenic shock complicating acute myocardial infarction. data from national registry of myocardial infarction. Am Heart J 2001; 141:933–939.
3. Barron, HV, Every, NR, Parson, LS, et al, The use of intraaortic balloon counterpulsation in patients with cardiogenic shock complicating acute myocardial infarction. data from national registry of myocardial infarction. Am Heart J 2001; 141:933–939.
![]() 4. Brodie, BR, et al. Intra-aortic balloon counterpulsation before primary percutaneous transluminal coronary angioplasty reduces catheterization laboratory events in high-risk patients with acute myocardial infarction. Am J Cardiol. 1999; 84:18–23.
4. Brodie, BR, et al. Intra-aortic balloon counterpulsation before primary percutaneous transluminal coronary angioplasty reduces catheterization laboratory events in high-risk patients with acute myocardial infarction. Am J Cardiol. 1999; 84:18–23.
![]() 5. Cadwell, CA, Tyson, G. Real timing. In Quaal S, ed. : Comprehensive intraaortic balloon counterpulsation, ed 2, St Louis: Mosby, 1993.
5. Cadwell, CA, Tyson, G. Real timing. In Quaal S, ed. : Comprehensive intraaortic balloon counterpulsation, ed 2, St Louis: Mosby, 1993.
![]() 6. Cadwell, CA, Hobson, KS, Petis, S. Clinical observations with real timing. Crit Care Nurs Clin North Am. 1996; 8:357–370.
6. Cadwell, CA, Hobson, KS, Petis, S. Clinical observations with real timing. Crit Care Nurs Clin North Am. 1996; 8:357–370.
7. Christenson, JT, Sierra, J, Romand, JA, et al. Long intraaortic balloon treatment time leads to more vascular complications. Asian Cardiovasc Thoracic Ann. 2007; 15(5):408–412.
![]() 8. Cook, L, et al, Intra-aortic balloon pump complications. a five-year retrospective study of 283 patients. Heart Lung 1999; 28:195–202.
8. Cook, L, et al, Intra-aortic balloon pump complications. a five-year retrospective study of 283 patients. Heart Lung 1999; 28:195–202.
![]() 9. Diver, D. Sheathless balloon insertion. In: Quaal SJ, ed. Comprehensive intra-aortic balloon counterpulsation. St Louis: Mosby, 1993.
9. Diver, D. Sheathless balloon insertion. In: Quaal SJ, ed. Comprehensive intra-aortic balloon counterpulsation. St Louis: Mosby, 1993.
10. Erdogan, HB, Goksedef, D, Erentug, V, et al, In which patients should sheathless IABP be used? An analysis of vascular complications in 1211 cases. J Cardiac Surg. 2006:342–346 [July (4)].
![]() 11. Ferguson, JJ, Cohen, M, Freedman, RJ, Jr., et al, The current practice of intraaortic balloon counterpulsation. results from the benchmark registry. J Am Coll Cardiol 2001; 38:1456–1462.
11. Ferguson, JJ, Cohen, M, Freedman, RJ, Jr., et al, The current practice of intraaortic balloon counterpulsation. results from the benchmark registry. J Am Coll Cardiol 2001; 38:1456–1462.
![]() 12. Hochman, JS, et al, Cardiogenic shock complicating acute myocardial infarction-etiologies. management and outcome: a report from the SHOCK trial registry: should we emergently revascularize occluded coronaries for cardiogenic shock. J Am Coll Cardiol. 2000; 36(3A):1610–1663.
12. Hochman, JS, et al, Cardiogenic shock complicating acute myocardial infarction-etiologies. management and outcome: a report from the SHOCK trial registry: should we emergently revascularize occluded coronaries for cardiogenic shock. J Am Coll Cardiol. 2000; 36(3A):1610–1663.
![]() 13. Kang, N, Edwards, M, Larbalestier, R. Preoperative intra-aortic balloon pumps in high risk patients undergoing open heart surgery. Ann Thoracic Surg. 2001; 72:54–57.
13. Kang, N, Edwards, M, Larbalestier, R. Preoperative intra-aortic balloon pumps in high risk patients undergoing open heart surgery. Ann Thoracic Surg. 2001; 72:54–57.
14. Klein, AJ, Messenger, JC, Casserly, IP. Endovascular treatment of intraaortic balloon pump-induced acute limb ischemia. Catheter Cardiovasc Interv. 2007; 70(1):138–142.
15. Marcu, CB, Donohue, TJ, Ferneini, A, et al, Intraaortic balloon pump insertion through the subclavian artery . subclavain artery insertion of IABP. Heart Lung Circ. 2006; 15(2):148–150.
![]() 16. Nordhaug, D, Steensrud, T, Muller, S, et al. Intraaortic balloon pumping improves hemodynamic and right ventricular efficiency in acute ischemic right ventricular failure. Ann Thoracic Surg. 2004; 78(4):1426–1432.
16. Nordhaug, D, Steensrud, T, Muller, S, et al. Intraaortic balloon pumping improves hemodynamic and right ventricular efficiency in acute ischemic right ventricular failure. Ann Thoracic Surg. 2004; 78(4):1426–1432.
![]() 17. O’Grady, NP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.
17. O’Grady, NP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.
![]() 18. Prunler, F, et al, Intra-aortic balloon counterpulsation (IABP) in high-risk acute myocardial infarction [abstract]. presented at First World Conference on Intra-Aortic Balloon Counterpulsation, Athens, 2000.
18. Prunler, F, et al, Intra-aortic balloon counterpulsation (IABP) in high-risk acute myocardial infarction [abstract]. presented at First World Conference on Intra-Aortic Balloon Counterpulsation, Athens, 2000.
![]() 19. Quaal, SJ. Conventional timing using the arterial pressure waveform. In Quaal SJ, ed. : Comprehensive intra-aortic balloon counterpulsation, ed 2, St Louis: Mosby, 2000.
19. Quaal, SJ. Conventional timing using the arterial pressure waveform. In Quaal SJ, ed. : Comprehensive intra-aortic balloon counterpulsation, ed 2, St Louis: Mosby, 2000.
![]() 20. Quaal, SJ, Caring for the intra-aortic balloon pump patient. most frequently asked questions. Crit Care Nurs Clin North Am 1996; 8:471–476.
20. Quaal, SJ, Caring for the intra-aortic balloon pump patient. most frequently asked questions. Crit Care Nurs Clin North Am 1996; 8:471–476.
![]() 21. Quaal, SJ. Interactive hemodynamics of IABC. In: Quaal SJ, ed. Comprehensive intra-aortic balloon counterpulsation. St Louis: Mosby, 1993.
21. Quaal, SJ. Interactive hemodynamics of IABC. In: Quaal SJ, ed. Comprehensive intra-aortic balloon counterpulsation. St Louis: Mosby, 1993.
![]() 22. Quaal, SJ, Intra-aortic balloon pumping timing. an overview. Crit Care Int 1997; 12–14. [Jan-Feb].
22. Quaal, SJ, Intra-aortic balloon pumping timing. an overview. Crit Care Int 1997; 12–14. [Jan-Feb].
![]() 23. Quaal, SJ. Nursing care of the intra-aortic balloon catheter’s inner lumen. Prog Cardiovasc Nurs. 1999; 14:11–13.
23. Quaal, SJ. Nursing care of the intra-aortic balloon catheter’s inner lumen. Prog Cardiovasc Nurs. 1999; 14:11–13.
![]() 24. Quaal, SJ. Interpreting the arterial pressure waveform in the intra-aortic balloon pumped patient. Prog Cardiovasc Nurs. 2001; 15:116–118.
24. Quaal, SJ. Interpreting the arterial pressure waveform in the intra-aortic balloon pumped patient. Prog Cardiovasc Nurs. 2001; 15:116–118.
![]() 25. Quaal, SJ. Physiological and clinical analysis of the arterial pressure waveform in the IABP patient. Can Perfusion Canadienne. 2000; 10:6–13.
25. Quaal, SJ. Physiological and clinical analysis of the arterial pressure waveform in the IABP patient. Can Perfusion Canadienne. 2000; 10:6–13.
![]() 26. Sanborn, T, Sleeper, LA, Bates, ER, et al, Impact of thrombolysis, intraaortic balloon pump counterpulsation and their combination in cardiogenic shock complicating acute myocardial infarction. a report from the SHOCK Trial registry. J Am Coll Cardiol. 2000; 36(3):1123–1129.
26. Sanborn, T, Sleeper, LA, Bates, ER, et al, Impact of thrombolysis, intraaortic balloon pump counterpulsation and their combination in cardiogenic shock complicating acute myocardial infarction. a report from the SHOCK Trial registry. J Am Coll Cardiol. 2000; 36(3):1123–1129.
27. Sice, A. Intraaortic balloon counterpulsation complicated by limb ischemia, a reflective commentary. Nurs Crit Care. 2006; 11(6):297–304.
![]() 28. Sleeper, LA, Ramanathan, K, Picard, MH, et al. Functional status and quality of life after emergency revascularization for cardiogenic shock complicating acute myocardial infarction. J Am Coll Cardiol. 2005; 46(2):266–273.
28. Sleeper, LA, Ramanathan, K, Picard, MH, et al. Functional status and quality of life after emergency revascularization for cardiogenic shock complicating acute myocardial infarction. J Am Coll Cardiol. 2005; 46(2):266–273.
![]() 29. Torchiana, DF, et al. Intra-aortic balloon pumping for cardiac support; trends in practice and outcome. J Thoracic Cardiovasc Surg. 1997; 114:758–764.
29. Torchiana, DF, et al. Intra-aortic balloon pumping for cardiac support; trends in practice and outcome. J Thoracic Cardiovasc Surg. 1997; 114:758–764.
![]() 30. Vanderheide, RH, Thadhani, R, Kufer, DJ. Association of thrombocytopenia with the use of intra-aortic balloon pumps. Am J Med. 1998; 105:27–32.
30. Vanderheide, RH, Thadhani, R, Kufer, DJ. Association of thrombocytopenia with the use of intra-aortic balloon pumps. Am J Med. 1998; 105:27–32.
![]() Bates, ER, et al. The use of intra-aortic balloon counterpulsation as an adjunct to reperfusion therapy in cardiogenic shock. J Cardiol. 1998; 65(Suppl 1):S37–S42.
Bates, ER, et al. The use of intra-aortic balloon counterpulsation as an adjunct to reperfusion therapy in cardiogenic shock. J Cardiol. 1998; 65(Suppl 1):S37–S42.
![]() Berger, PB, et al, Impact of an aggressive invasive catheterization and revascularization strategy on mortality in patients with cardiogenic shock in the Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries (GUSTO-I) trial. an observational study. Circulation 1997; 96:122–127.
Berger, PB, et al, Impact of an aggressive invasive catheterization and revascularization strategy on mortality in patients with cardiogenic shock in the Global Utilization of Streptokinase and Tissue Plasminogen Activator for Occluded Coronary Arteries (GUSTO-I) trial. an observational study. Circulation 1997; 96:122–127.
![]() Blusch, T, et al, Vascular complications related to intra-aortic balloon counterpulsation. an analysis of ten years experience. Thorac Cardiovasc Surg 1997; 45:55–59.
Blusch, T, et al, Vascular complications related to intra-aortic balloon counterpulsation. an analysis of ten years experience. Thorac Cardiovasc Surg 1997; 45:55–59.
Bream-Rouwenhorst HR, Hobbs, RA, Horwitz, PA. Thrombocytopenia in patients treated with heparin, combination -antiplatelet therapy, and intra-aortic balloon pump counterpulsation. J Interv Cardiol. 2008; 21(4):350–356.
![]() Christenson, JT, et al. Evaluation of preoperative intra-aortic balloon pump support in high risk coronary patients. Eur J Cardiothoracic Surg. 1997; 11:1097–1103.
Christenson, JT, et al. Evaluation of preoperative intra-aortic balloon pump support in high risk coronary patients. Eur J Cardiothoracic Surg. 1997; 11:1097–1103.
![]() Christenson, JT, Schmuziber, M, Simonet, F. Effective surgical management of high-risk coronary patients using preoperative intra-aortic balloon counterpulsation therapy. Cardiovasc Surg. 2001; 9:383–390.
Christenson, JT, Schmuziber, M, Simonet, F. Effective surgical management of high-risk coronary patients using preoperative intra-aortic balloon counterpulsation therapy. Cardiovasc Surg. 2001; 9:383–390.
Field, ML, Rengarajan, A, Khan, O, et al, Preoperative intra aortic balloon pumps in patients undergoing coronary artery bypass grafting . Cochrane Database Syst Rev 2007; 1
![]() Garrett, K, Grady, KL, Intra-aortic balloon pumping through the common iliac artery. management of the ambulatory intra-aortic balloon pump patient. Prog Cardiovasc Nurs 2000; 15:14–20.
Garrett, K, Grady, KL, Intra-aortic balloon pumping through the common iliac artery. management of the ambulatory intra-aortic balloon pump patient. Prog Cardiovasc Nurs 2000; 15:14–20.
![]() Kovak, PJ, et al. Thrombolysis plus aortic counterpulsation -improved survival of patients who present to the community hospital with cardiogenic shock. J Am Coll Cardiol. 1997; 29:454–458.
Kovak, PJ, et al. Thrombolysis plus aortic counterpulsation -improved survival of patients who present to the community hospital with cardiogenic shock. J Am Coll Cardiol. 1997; 29:454–458.
![]() Low, R, Intra-aortic balloon counterpulsation in acute myocardial infarction. too few or too many. JACC 2003; 41:1946–1947.
Low, R, Intra-aortic balloon counterpulsation in acute myocardial infarction. too few or too many. JACC 2003; 41:1946–1947.
![]() Mertlich, GB, et al, Effect of increased intra-aortic balloon pressure on catheter volume. relationship to changing -attitude. Crit Care Med 1992; 20:297–303.
Mertlich, GB, et al, Effect of increased intra-aortic balloon pressure on catheter volume. relationship to changing -attitude. Crit Care Med 1992; 20:297–303.
Mishra, S, et al. Role of prophylactic intra-aortic balloon pump in high-risk patients undergoing percutaneous intervention. Am J Cardiol. 2006; 98(5):608–612.
![]() Ohman, E, Hochman, J, Aortic counterpulsion in acute myocardial infarction. physiologically important, but does the -patient benefit. Am Heart J 2001; 141:889–892.
Ohman, E, Hochman, J, Aortic counterpulsion in acute myocardial infarction. physiologically important, but does the -patient benefit. Am Heart J 2001; 141:889–892.
Osentowski, MK, Holt, DW. Evaluating the efficacy of intra-aortic balloon pump timing using the auto-timing mode of operation with the Datascope CS100. J Extracorp Technol. 2007; 39(2):87–90.
Reid, MB, Cottrell, D. Nursing care of patients receiving intra-aortic balloon counterpulsation. Crit Care Nurse. 2005; 25(5):40–49.
Santa-Cruz RA, Cohen, RA, Ohman, EM, Aortic counterpulsation. a review of the hemodynamic effects and indications for use. Catheter Cardiovasc Interv. 2006; 67(1):68–77.
![]() Stone, GW, Ohman, E, Miller, M. Contemporary utilization and outcomes of intra-aortic balloon counterpulsation in acute myocardial infarction. JACC. 2003; 41:1940–1947.
Stone, GW, Ohman, E, Miller, M. Contemporary utilization and outcomes of intra-aortic balloon counterpulsation in acute myocardial infarction. JACC. 2003; 41:1940–1947.
![]() Talley, JD, Ohman, EM, Mark, OB, Economic implications of the prophylactic use of intra-aortic balloon counterpulsation in the setting of acute myocardial infarction. the Randomized IABP Study Group. Am J Cardiol 1997; 79:S90–S94.
Talley, JD, Ohman, EM, Mark, OB, Economic implications of the prophylactic use of intra-aortic balloon counterpulsation in the setting of acute myocardial infarction. the Randomized IABP Study Group. Am J Cardiol 1997; 79:S90–S94.