Temporary Transvenous and Epicardial Pacing
PREREQUISITE NURSING KNOWLEDGE
• Knowledge of the normal anatomy and physiology of the cardiovascular system, principles of cardiac conduction, and basic dysrhythmia interpretation is necessary.
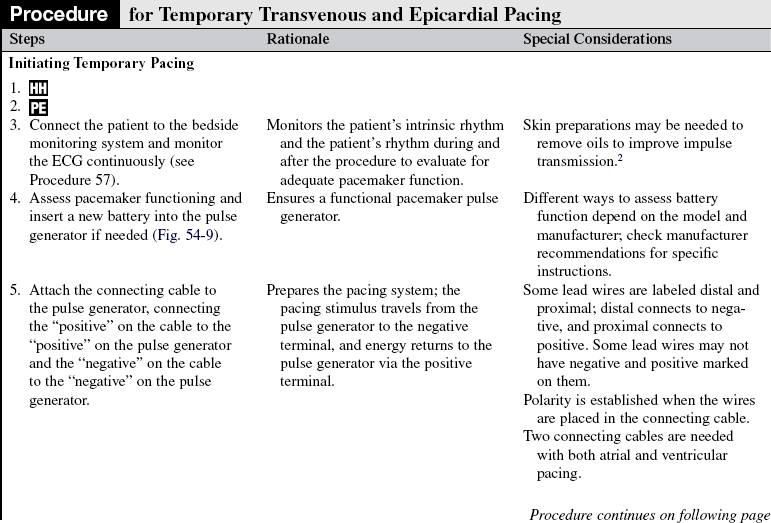
• Understanding of temporary pacemakers is needed to evaluate pacemaker function and the patient’s response to pacemaker therapy.
• Clinical and technical competence related to use of temporary pacemakers is needed.
• Advanced cardiac life support knowledge and skills are necessary.
• Basic principles of hemodynamic monitoring are essential in assessment of the efficacy of temporary pacing therapy.
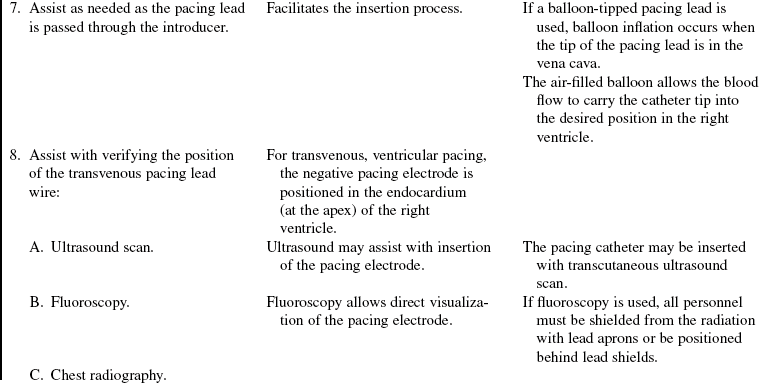
• Knowledge of the pulmonary artery (PA) catheter function and its use relative to hemodynamic monitoring is a necessity with use of a PA catheter with pacing function (see Procedure 73).
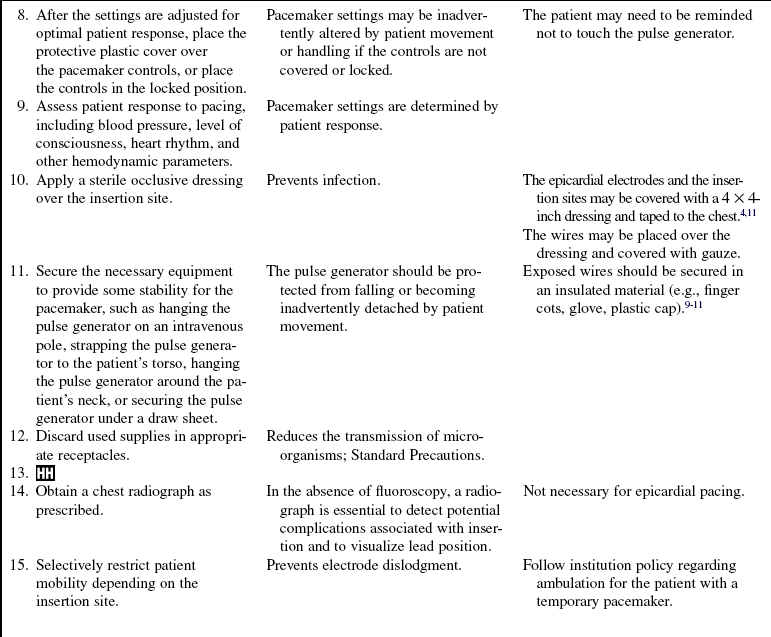
• Knowledge of the care of the patient with central venous catheters (see Procedure 70) is needed.
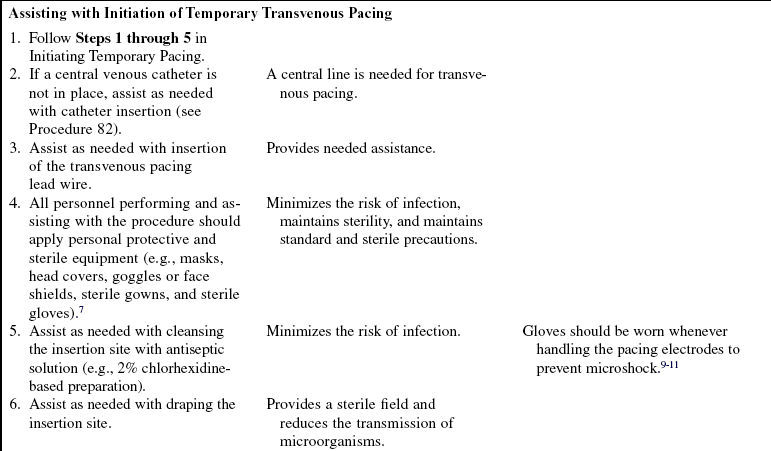
• Principles of general electrical safety apply with use of temporary invasive pacing methods. Gloves always should be worn when handling electrodes to prevent microshock. In addition, the exposed proximal ends of the pacing wires should be insulated when not in use to prevent microshock.9–11
• The insertion of a temporary pacemaker is performed in emergent and elective clinical situations.
• Temporary pacing may be used to stimulate the myocardium to contract in the absence of an intrinsic rhythm, establish an adequate cardiac output and blood pressure to ensure tissue perfusion to vital organs, reduce the possibility of ventricular dysrhythmias in the presence of bradycardia, supplement an inadequate rhythm with transient decreases in heart rate (e.g., chronotropic incompetence in shock), or allow the administration of medications (e.g., beta blockers) to treat ischemia or tachydysrhythmias in the presence of conduction system dysfunction or bradycardia.
• Temporary invasive pacing is indicated for the following4,6,8:
 Symptomatic third-degree atrioventricular (AV) block
Symptomatic third-degree atrioventricular (AV) block
 Symptomatic second-degree heart block
Symptomatic second-degree heart block
 Dysrhythmias that complicate acute myocardial infarction
Dysrhythmias that complicate acute myocardial infarction
 Symptomatic bradycardia or bradydysrhythmias
Symptomatic bradycardia or bradydysrhythmias
 New bundle-branch block with transient complete heart block
New bundle-branch block with transient complete heart block
 Alternating bundle-branch block
Alternating bundle-branch block
 Symptomatic sinus node dysfunction
Symptomatic sinus node dysfunction
 Treatment of bradycardia-tachycardia syndrome (sick sinus syndrome)
Treatment of bradycardia-tachycardia syndrome (sick sinus syndrome)
 Ventricular standstill or cardiac arrest
Ventricular standstill or cardiac arrest
 Long QT syndrome with ventricular dysrhythmias
Long QT syndrome with ventricular dysrhythmias
 Medication toxicity or adverse effects of a medication
Medication toxicity or adverse effects of a medication
 Prophylaxis with cardiac diagnostic or interventional procedures
Prophylaxis with cardiac diagnostic or interventional procedures
 Chronotropic incompetence in the setting of cardiogenic shock
Chronotropic incompetence in the setting of cardiogenic shock
• The three primary methods of invasive temporary pacing are: transvenous endocardial pacing, pacing via a PA catheter, and epicardial pacing.
 In temporary transvenous pacing, the pulse generator is externally attached to a pacing lead that is inserted through a vein into the right atrium or ventricle.
In temporary transvenous pacing, the pulse generator is externally attached to a pacing lead that is inserted through a vein into the right atrium or ventricle.
 Veins used for insertion of the pacing lead are the subclavian, femoral, brachial, internal jugular, or external jugular veins.
Veins used for insertion of the pacing lead are the subclavian, femoral, brachial, internal jugular, or external jugular veins.
 Single-chamber ventricular pacing is the most common method used in an emergency because the goal is to establish a heart rate as quickly as possible.
Single-chamber ventricular pacing is the most common method used in an emergency because the goal is to establish a heart rate as quickly as possible.
 Temporary atrial or dual-chamber pacing can be initiated if the patient needs atrial contraction for improvement in hemodynamics.
Temporary atrial or dual-chamber pacing can be initiated if the patient needs atrial contraction for improvement in hemodynamics.
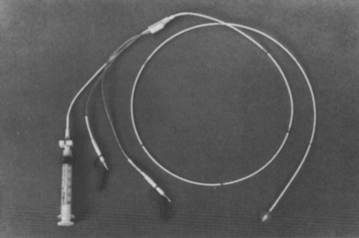
 The pacing lead is an insulated wire with one or two electrodes at the tip of the wire (Fig. 54-1).
The pacing lead is an insulated wire with one or two electrodes at the tip of the wire (Fig. 54-1).
 The pacing lead can be a hard-tipped or balloon-tipped pacing catheter that is placed in direct contact with the endocardium. Most temporary leads are bipolar, with the distal tip electrode separated from the proximal ring by 1 to 2 cm (see Fig. 53-1).
The pacing lead can be a hard-tipped or balloon-tipped pacing catheter that is placed in direct contact with the endocardium. Most temporary leads are bipolar, with the distal tip electrode separated from the proximal ring by 1 to 2 cm (see Fig. 53-1).
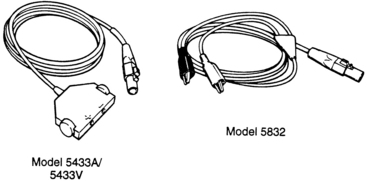
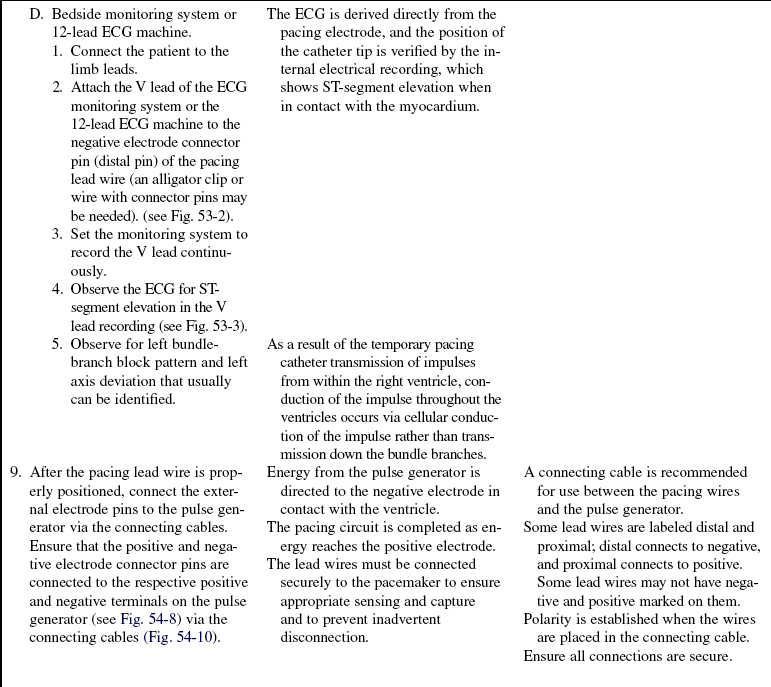
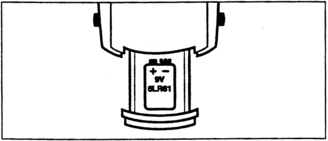
 An external temporary pulse generator is connected to the transvenous pacing wire via a bridging or connecting cable.
An external temporary pulse generator is connected to the transvenous pacing wire via a bridging or connecting cable.
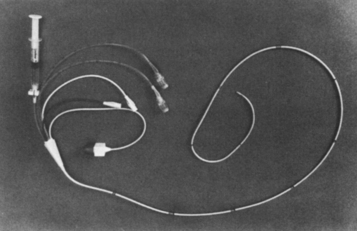
 Temporary atrial or ventricular pacing via a thermodilution PA catheter can be done with combination catheters that are specifically designed for temporary pacing.
Temporary atrial or ventricular pacing via a thermodilution PA catheter can be done with combination catheters that are specifically designed for temporary pacing.
 PA pacing catheters feature atrial and ventricular ports for the introduction of the pacing lead wires (Fig. 54-2).
PA pacing catheters feature atrial and ventricular ports for the introduction of the pacing lead wires (Fig. 54-2).
 Use of a PA catheter combines the capabilities of PA pressure monitoring, thermodilution cardiac output measurement, fluid infusion, mixed venous oxygen sampling, and temporary pacing.
Use of a PA catheter combines the capabilities of PA pressure monitoring, thermodilution cardiac output measurement, fluid infusion, mixed venous oxygen sampling, and temporary pacing.
 One limitation of these multifunction catheters is that the simultaneous measurement of pulmonary artery occlusion pressure (PAOP) and pacing is usually not possible. Balloon inflation can cause repositioning of the pacing electrode with catheter movement; measurement of the PAOP may cause pacing to become intermittent.8
One limitation of these multifunction catheters is that the simultaneous measurement of pulmonary artery occlusion pressure (PAOP) and pacing is usually not possible. Balloon inflation can cause repositioning of the pacing electrode with catheter movement; measurement of the PAOP may cause pacing to become intermittent.8
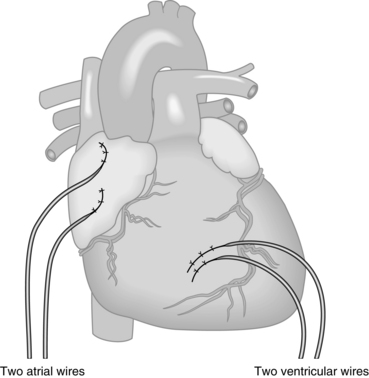
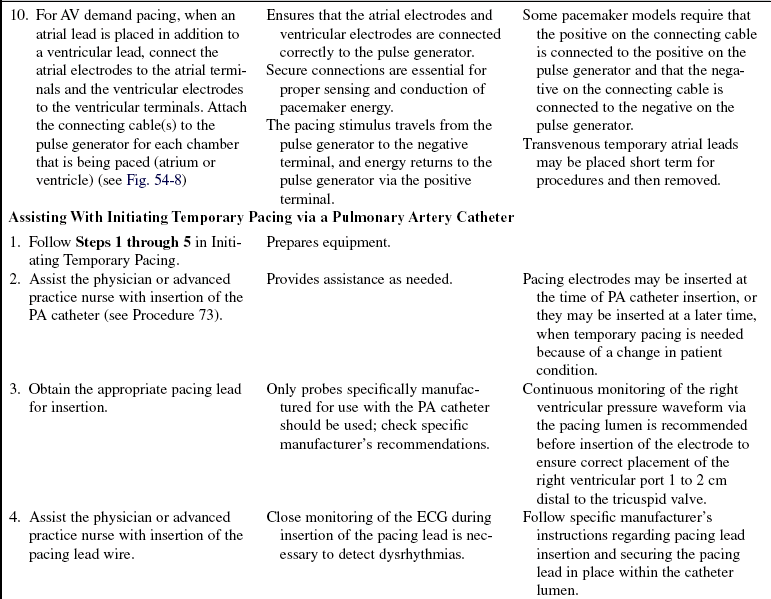
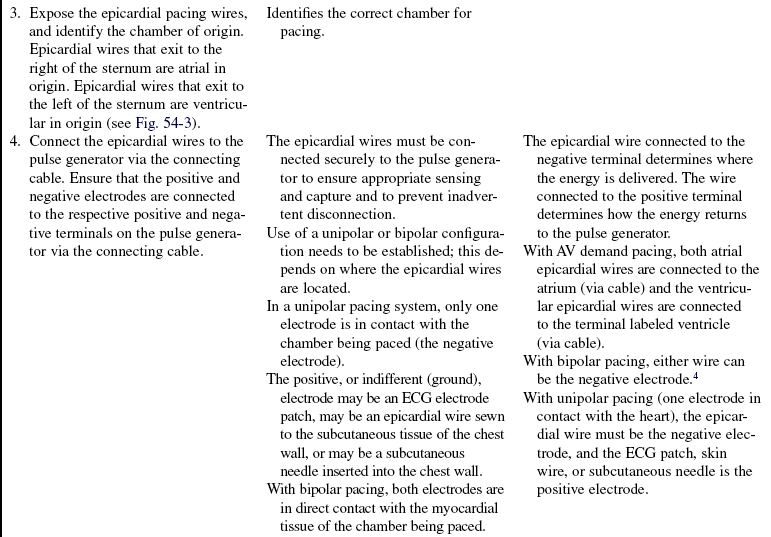
 Temporary epicardial pacing is a method of stimulating the myocardium through the use of polytetrafluoroethylene (PTFE)-coated, unipolar or bipolar stainless steel wires that are sutured loosely to the epicardium after cardiac surgery (Fig. 54-3).
Temporary epicardial pacing is a method of stimulating the myocardium through the use of polytetrafluoroethylene (PTFE)-coated, unipolar or bipolar stainless steel wires that are sutured loosely to the epicardium after cardiac surgery (Fig. 54-3).
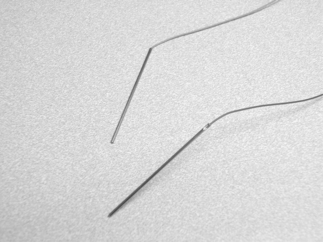
Figure 54-3 Epicardial wires.
 The epicardial wires may be attached to the right atrium for atrial pacing, the right ventricle for ventricular pacing, or both for AV pacing.
The epicardial wires may be attached to the right atrium for atrial pacing, the right ventricle for ventricular pacing, or both for AV pacing.
 Each pacing wire is brought through the chest wall before the chest is closed.
Each pacing wire is brought through the chest wall before the chest is closed.
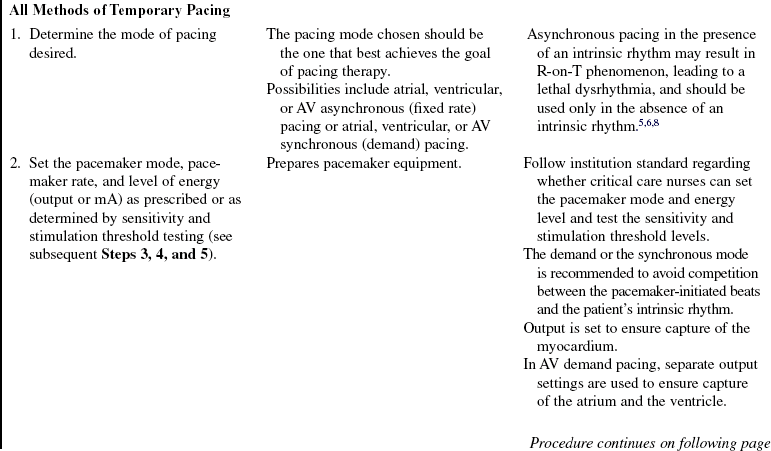
 Typically, the atrial wires are located on the right of the sternum, and the ventricular wires exit to the left of the sternum (Fig. 54-4)
Typically, the atrial wires are located on the right of the sternum, and the ventricular wires exit to the left of the sternum (Fig. 54-4)
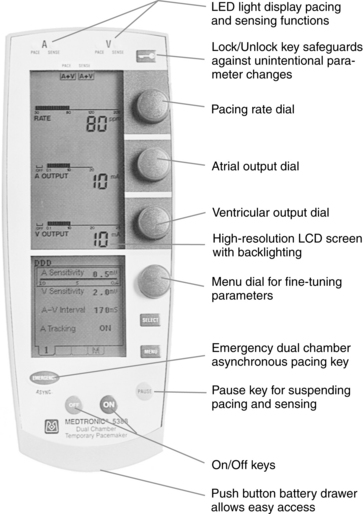
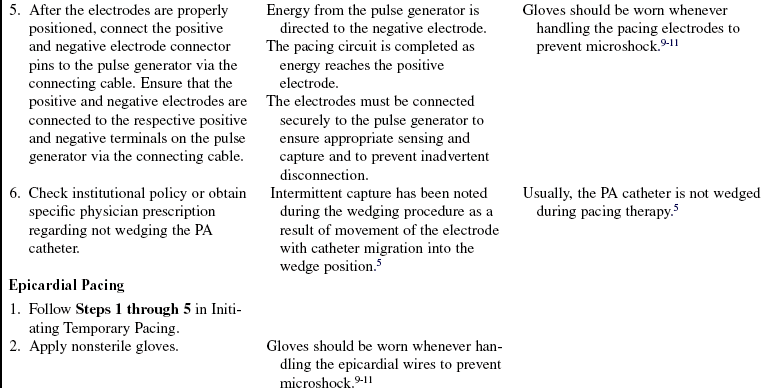
 An external temporary pulse generator (Figs. 54-5 and 54-6) is connected to the epicardial pacing wires via a bridging or connecting cable (Figs. 54-7).
An external temporary pulse generator (Figs. 54-5 and 54-6) is connected to the epicardial pacing wires via a bridging or connecting cable (Figs. 54-7).
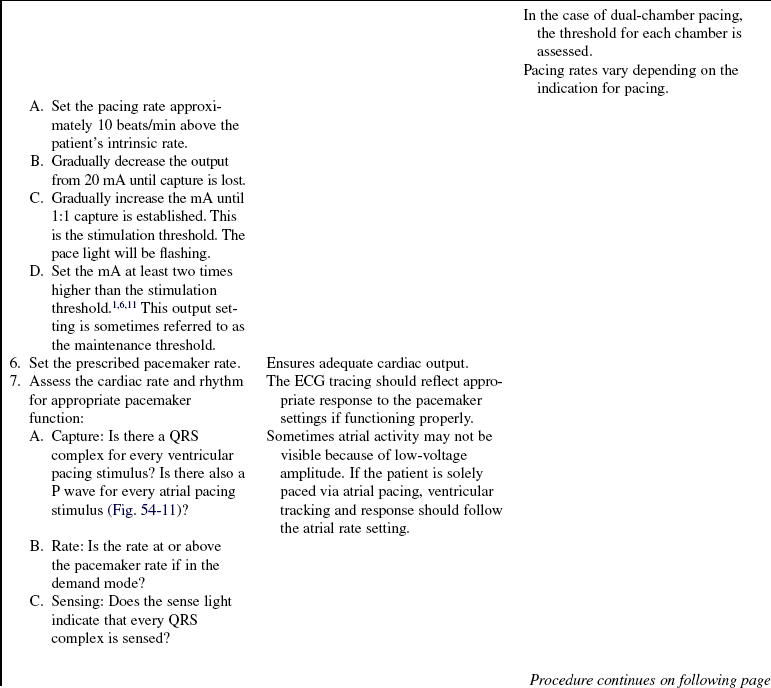
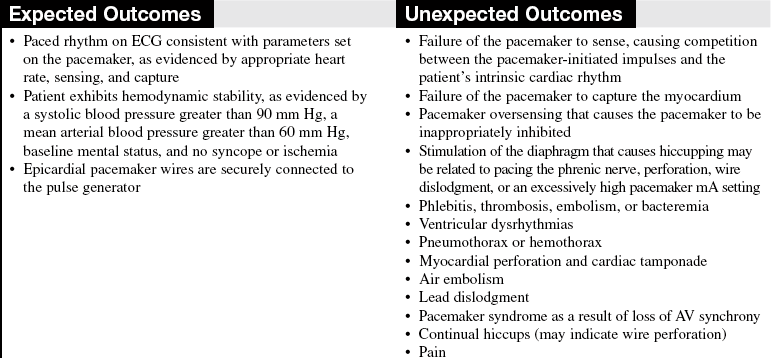
• Basic principles of cardiac pacing include sensing, pacing, and capture.
• Sensing refers to the ability of the pacemaker device to detect intrinsic myocardial electrical activity. Sensing occurs if the pulse generator is in the synchronous or demand mode. The pacemaker either is inhibited from delivering a stimulus or initiates an electrical impulse.
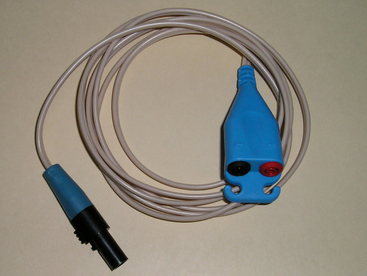
• Pacing occurs when the temporary pulse generator is activated and the requisite level of energy travels from the pulse generator through the temporary wires to the myocardium, which is known as pacemaker firing and is represented as a line or spike on the electrocardiogram (ECG) recording.
• Capture refers to the successful stimulation of the myocardium by the pacemaker, resulting in depolarization. Capture is evidenced on the ECG as an atrial or ventricular complex following the pacemaker spike, depending on the chamber being paced.
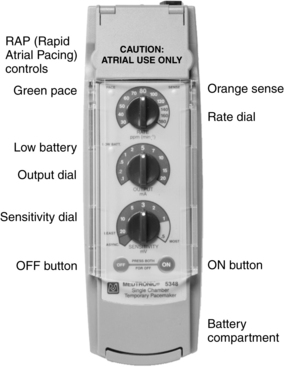
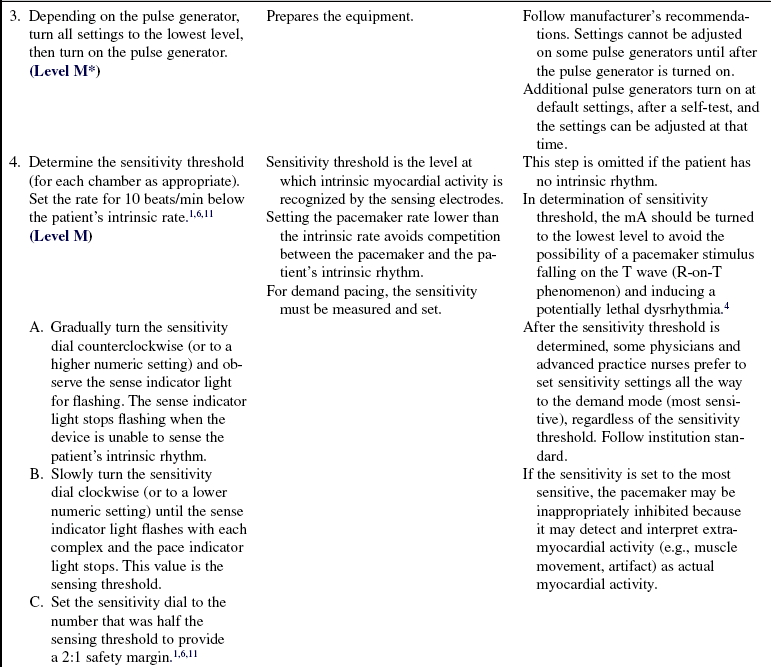
 The temporary pulse generator houses the controls and energy source for pacing.
The temporary pulse generator houses the controls and energy source for pacing.
 Some pulse generators can be used for single-chamber pacing and have one set of terminals at the top of the pulse generator into which the pacing wires are inserted (via connecting cable; see Fig. 54-5).
Some pulse generators can be used for single-chamber pacing and have one set of terminals at the top of the pulse generator into which the pacing wires are inserted (via connecting cable; see Fig. 54-5).
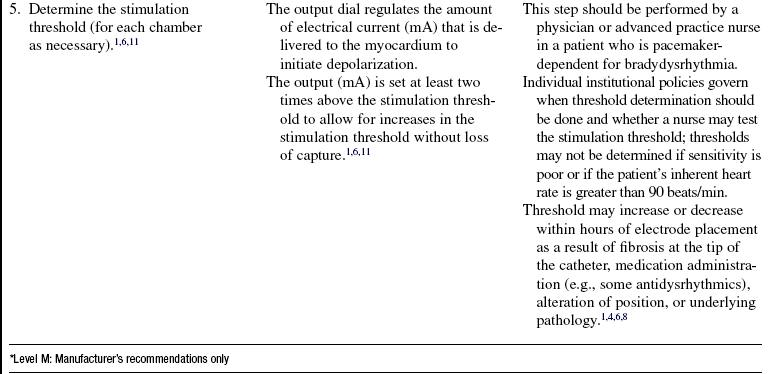
• A dual-chamber pacemaker requires two sets of terminals for the atrial and ventricular wires (see Figs. 54-6 and 54-8).
• Different models of pacemakers use either dials or touch pads to change the settings.
 The pacing rate is determined by the rate dial or touch pad.
The pacing rate is determined by the rate dial or touch pad.
 The AV interval dial or pad on a dual-chamber pacemaker controls the amount of time between atrial and ventricular stimulation (electronic PR interval).
The AV interval dial or pad on a dual-chamber pacemaker controls the amount of time between atrial and ventricular stimulation (electronic PR interval).
 The energy delivered to the myocardium is determined by setting the output (milliampere [mA]) dial or pad on the pulse generator.
The energy delivered to the myocardium is determined by setting the output (milliampere [mA]) dial or pad on the pulse generator.
 Dual-chamber pacing requires that mA be set for the atria and the ventricle.
Dual-chamber pacing requires that mA be set for the atria and the ventricle.
• The ability of the pacemaker to detect the patient’s intrinsic rhythm is determined by the pacing mode and sensitivity setting. In the asynchronous mode, the pacemaker functions as a fixed-rate pacemaker and is not able to sense any of the patient’s inherent cardiac activity. In the synchronous mode, the pacemaker is able to sense the patient’s inherent cardiac activity.
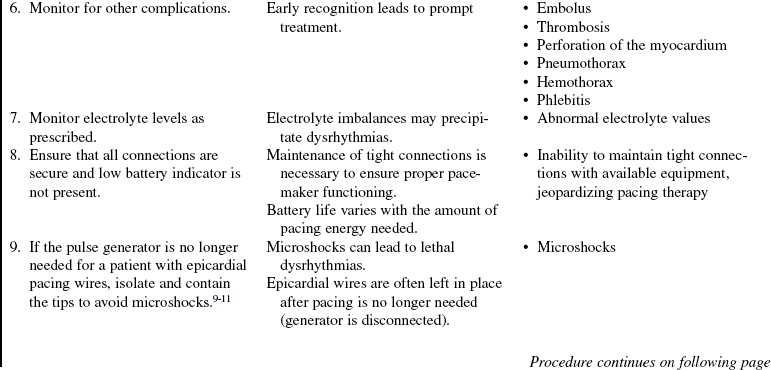
• The ability of the pacemaker to depolarize the myocardium depends on many variables: the position of the electrodes and degree of contact with viable myocardial tissue; the level of energy delivered through the pacing wire; the presence of hypoxia, acidosis, or electrolyte imbalances; fibrosis around the tip of the catheter; and concomitant medication therapy.8,10
• Atrial and ventricular thresholds for epicardial wires increase by the fourth postoperative day.3
EQUIPMENT
PATIENT AND FAMILY EDUCATION
• Assess learning needs, readiness to learn, and factors that influence learning.  Rationale: This assessment enables teaching to be individualized in a manner that is meaningful to the patient and family.
Rationale: This assessment enables teaching to be individualized in a manner that is meaningful to the patient and family.
• Discuss basic information about the normal conduction system, such as structure and function of the conduction system, normal and abnormal heart rhythms, and symptoms or significance of abnormal heart rhythms.  Rationale: The patient and family should understand the conduction system and why the procedure is necessary.
Rationale: The patient and family should understand the conduction system and why the procedure is necessary.
• Provide a basic description of the temporary pacemaker insertion procedure.  Rationale: The patient and family should be informed of the invasive nature of the procedure and any risks associated with it. An understanding of the procedure may reduce anxiety.
Rationale: The patient and family should be informed of the invasive nature of the procedure and any risks associated with it. An understanding of the procedure may reduce anxiety.
• Describe the precautions and restrictions required while the temporary pacemaker is in place, such as limitation of movement, avoidance of handling the pacemaker or touching exposed portions of the electrodes, and when to notify the nurse (e.g., if the dressing becomes wet, if the patient experiences dizziness).  Rationale: Understanding limitations may improve patient cooperation with restrictions and precautions. The patient and family also will alert nurses to potential problems.
Rationale: Understanding limitations may improve patient cooperation with restrictions and precautions. The patient and family also will alert nurses to potential problems.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess the patient’s baseline cardiac rhythm for the presence of the dysrhythmia that necessitates temporary cardiac pacing.  Rationale: This assessment determines the need for invasive cardiac pacing.
Rationale: This assessment determines the need for invasive cardiac pacing.
• Assess the patient’s hemodynamic response to the dysrhythmia. Rhythm disturbances may reduce cardiac output significantly with detrimental effects on perfusion to vital organs.  Rationale: This assessment determines the urgency of the procedure. It may indicate the need for temporizing measures, such as vasopressors or transcutaneous pacing.
Rationale: This assessment determines the urgency of the procedure. It may indicate the need for temporizing measures, such as vasopressors or transcutaneous pacing.
• Review the patient’s current medications.  Rationale: Medications may be a cause of the dysrhythmia that led to the need for pacemaker therapy, or medications may need to be held because of concomitant effect. Other medications, such as antidysrhythmics, may alter the pacing threshold.
Rationale: Medications may be a cause of the dysrhythmia that led to the need for pacemaker therapy, or medications may need to be held because of concomitant effect. Other medications, such as antidysrhythmics, may alter the pacing threshold.
• Review the patient’s current laboratory study results, including chemistry or electrolyte profile, arterial blood gases, or cardioactive medication levels.  Rationale: This review assists in determining whether the need for pacing was precipitated by metabolic disturbances or medication toxicity and establishes the pacing milieu.
Rationale: This review assists in determining whether the need for pacing was precipitated by metabolic disturbances or medication toxicity and establishes the pacing milieu.
Patient Preparation
• Verify correct patient using two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand preprocedural teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: This communication evaluates and reinforces understanding of previously taught information.
Rationale: This communication evaluates and reinforces understanding of previously taught information.
• Confirm that informed consent has been obtained.  Rationale: Informed consent protects the rights of the patient and makes a competent decision possible for the patient; however, in emergency circumstances, time may not allow the consent form to be signed.
Rationale: Informed consent protects the rights of the patient and makes a competent decision possible for the patient; however, in emergency circumstances, time may not allow the consent form to be signed.
• Perform a pre-procedure verification and time out, if non-emergent.  Rationale: Ensures patient safety.
Rationale: Ensures patient safety.
References
1. Abate, E, Kusumoto, FM, Goldschlager, NF. Techniques for temporary pacing. In Kusumoto FM, Goldschlager NF, eds. : Cardiac pacing for the clinician,, ed 2, New York: Springer-Verlag, 2007.
![]() 2. Drew, B, Practice standards for electrocardiographic monitoring in hospital settings. an American Heart Association scientific statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Youngendorsed by the International Society of Computerized Electrocardiology and the American -Association of Critical-Care Nurses. Circulation 2004; 110:2721–2746.
2. Drew, B, Practice standards for electrocardiographic monitoring in hospital settings. an American Heart Association scientific statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular Disease in the Youngendorsed by the International Society of Computerized Electrocardiology and the American -Association of Critical-Care Nurses. Circulation 2004; 110:2721–2746.
![]() 3. Elmi, F, Tullo, NG, Khalighi, K. Natural history and predictors of temporary epicardial pacemaker wire function in patients after open heart surgery. Cardiology. 2002; 98:175–180.
3. Elmi, F, Tullo, NG, Khalighi, K. Natural history and predictors of temporary epicardial pacemaker wire function in patients after open heart surgery. Cardiology. 2002; 98:175–180.
![]() 4. Finkelmeier, BA. Temporary pacing and defibrillation in cardiothoracic surgical nursing,. Philadelphia: Lippincott; 2000.
4. Finkelmeier, BA. Temporary pacing and defibrillation in cardiothoracic surgical nursing,. Philadelphia: Lippincott; 2000.
![]() 5. Gammage, MD. Temporary cardiac pacing. Heart. 2000; 83:715–720.
5. Gammage, MD. Temporary cardiac pacing. Heart. 2000; 83:715–720.
6. Medtronic Corp. Model 5388 dual chamber temporary pacemaker technical manual. Minneapolis: Medtronic; 2007.
![]() 7. O’Grady, NP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.
7. O’Grady, NP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.
8. Overbay, D, Criddle, L. Mastering temporary invasive cardiac pacing. Crit Care Nurse. 2004; 24(3):25–32.
![]() 9. Reade, MC, Temporary epicardial pacing after cardiac surgery. a practical review: part 1: general considerations in the management of epicardial pacing. Anaesthesia 2007; 62:264–271.
9. Reade, MC, Temporary epicardial pacing after cardiac surgery. a practical review: part 1: general considerations in the management of epicardial pacing. Anaesthesia 2007; 62:264–271.
![]() 10. Timothy, PR, Rodeman, BJ, Temporary pacemakers in critically ill patients. assessment and management strategies. AACN Clin Issues 2004; 15:305–325.
10. Timothy, PR, Rodeman, BJ, Temporary pacemakers in critically ill patients. assessment and management strategies. AACN Clin Issues 2004; 15:305–325.
![]() 11. Woods SL, Froelicher ES, Adams S, et al, eds.. Pacemakers and implantable defibrillators. Cardiac nursing. ed 5. Lippincott Williams and Wilkins, Philadelphia, 2005.
11. Woods SL, Froelicher ES, Adams S, et al, eds.. Pacemakers and implantable defibrillators. Cardiac nursing. ed 5. Lippincott Williams and Wilkins, Philadelphia, 2005.
Batra, AS, Balaji, S, Post operative temporary epicardial pacing. when, how and why. Ann Pediatr Card. 2008; 1(2):120–125.
![]() Conover, M. Electrical stimulation therapies in understanding electrocardiography, ed 8. St Louis: Mosby; 2003. [Chapter 33].
Conover, M. Electrical stimulation therapies in understanding electrocardiography, ed 8. St Louis: Mosby; 2003. [Chapter 33].
![]() Conover, M. Pacemaker therapies for bradyarrhythmias in understanding electrocardiography, ed 8. St Louis: Mosby; 2003. [Chapter 34].
Conover, M. Pacemaker therapies for bradyarrhythmias in understanding electrocardiography, ed 8. St Louis: Mosby; 2003. [Chapter 34].
Hongo, RH, Goldschlager, NF. Cardiac pacing in the critical care setting. In Kusumoto FM, Goldschlager NF, eds. : Cardiac pacing for the clinician, ed 2, New York: Springer-Verlag, 2007.