Temporary Transvenous Pacemaker Insertion (Perform)
Temporary Transvenous Pacemaker Insertion (Perform)
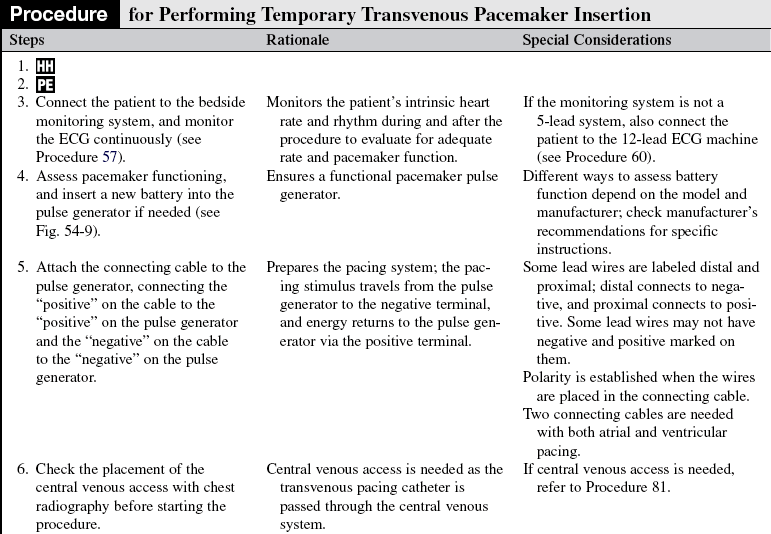
PREREQUISITE NURSING KNOWLEDGE
• Knowledge of the normal anatomy and physiology of the cardiovascular system, principles of cardiac conduction, and basic and advanced dysrhythmia interpretation is needed.
• Knowledge of temporary pacemaker function and expected patient responses to pacemaker therapy is necessary.
• Clinical and technical competence in central line insertion, temporary transvenous pacemaker insertion, and suturing is needed.
• Clinical and technical competence related to use of temporary pacemakers is necessary.
• Competence in chest radiograph interpretation is needed.
• Advanced cardiac life support knowledge and skills are needed.
• Principles of general electrical safety apply with use of temporary invasive pacing methods. Gloves always should be worn when handling electrodes to prevent microshock.
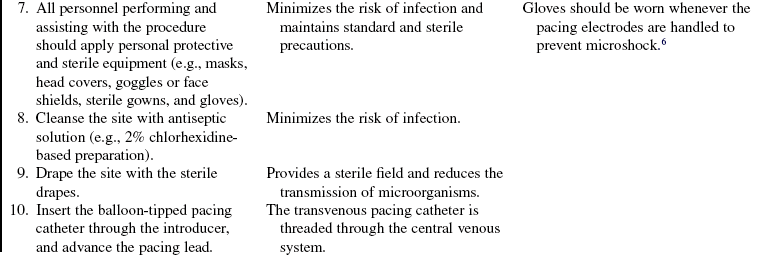
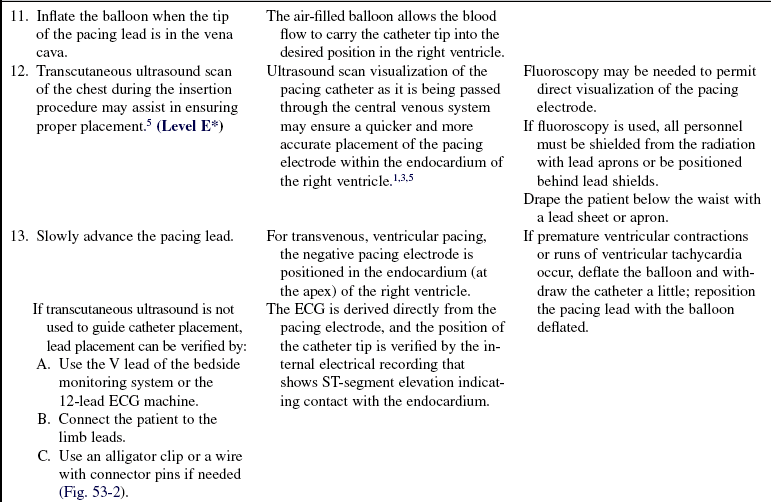
• The insertion of a temporary transvenous pacemaker is performed in emergency and elective clinical situations. Temporary transvenous pacing may be used to:
 Stimulate the myocardium to contract in the absence of an intrinsic rhythm
Stimulate the myocardium to contract in the absence of an intrinsic rhythm
 Establish adequate cardiac output and blood pressure
Establish adequate cardiac output and blood pressure
 Ensure tissue perfusion to vital organs
Ensure tissue perfusion to vital organs
 Reduce the possibility of ventricular dysrhythmias in the presence of bradycardia
Reduce the possibility of ventricular dysrhythmias in the presence of bradycardia
 Supplement an inadequate rhythm, such as when transient decreases in heart rate occur (e.g., chronotropic incompetence in shock)
Supplement an inadequate rhythm, such as when transient decreases in heart rate occur (e.g., chronotropic incompetence in shock)
 Allow the administration of medications that may cause a rhythm or conduction abnormality (e.g., beta blockers) in the symptomatic bradycardia, complete heart block, new bundle-branch block with transient complete heart block, alternating bundle-branch block)
Allow the administration of medications that may cause a rhythm or conduction abnormality (e.g., beta blockers) in the symptomatic bradycardia, complete heart block, new bundle-branch block with transient complete heart block, alternating bundle-branch block)
• Temporary transvenous pacing is indicated for the following:
 Third-degree atrioventricular (AV) block
Third-degree atrioventricular (AV) block
 Dysrhythmias that are complicating acute myocardial infarction (e.g., symptomatic bradycardia, complete heart block, new bundle-branch block with transient complete heart block, alternating bundle-branch block)
Dysrhythmias that are complicating acute myocardial infarction (e.g., symptomatic bradycardia, complete heart block, new bundle-branch block with transient complete heart block, alternating bundle-branch block)
 Sinus node dysfunction (e.g., symptomatic bradydysrhythmias, treatment of bradycardia-tachycardia syndromes, sick sinus syndrome)
Sinus node dysfunction (e.g., symptomatic bradydysrhythmias, treatment of bradycardia-tachycardia syndromes, sick sinus syndrome)
 Ventricular standstill or cardiac arrest
Ventricular standstill or cardiac arrest
 Long QT syndrome with ventricular dysrhythmias
Long QT syndrome with ventricular dysrhythmias
 Prophylaxis with cardiac diagnostic or interventional procedures
Prophylaxis with cardiac diagnostic or interventional procedures
 Chronotropic incompetence in the setting of cardiogenic shock
Chronotropic incompetence in the setting of cardiogenic shock
• When temporary transvenous pacing is used, the pulse generator is attached externally to a pacing lead wire that is inserted through a vein into the right atrium or right ventricle.
• Veins used for the insertion of a transvenous pacing lead wire are the subclavian, femoral, brachial, internal jugular, or external jugular.
• Single-chamber ventricular pacing is the most appropriate method in an emergency because the goal is to establish a heart rate as quickly as possible.
• The transvenous pacing lead is an insulated wire with one or two electrodes at the tip of the wire (Fig. 53-1).
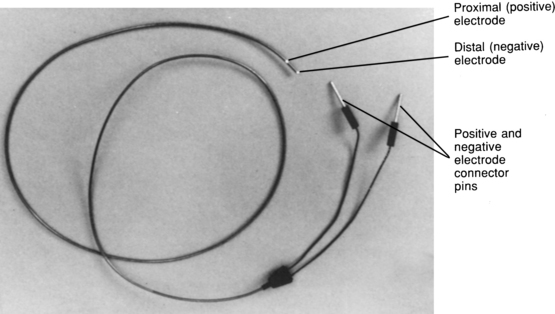
FIGURE 53-1 Bipolar lead wire.
• The pacing lead can be a hard-tipped or a balloon-tipped pacing catheter that is placed in direct contact with the endocardium. Most temporary leads are bipolar with the distal tip electrode (seen as a metal ring) separated from the proximal electrode by 1 to 2 cm of pacing catheter (also seen as a metal ring; see Fig. 53-1).
• Basic principles of cardiac pacing include sensing, pacing, and capture.
• Sensing refers to the ability of the pacemaker device to detect intrinsic myocardial electrical activity. Sensing occurs if the pulse generator is in the synchronous or demand mode. The pacemaker either is inhibited from delivering a stimulus or initiates an electrical impulse.
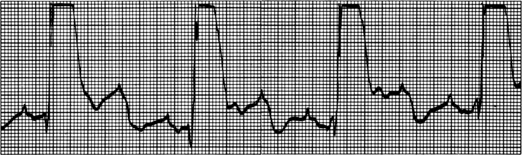
• Pacing occurs when the temporary pulse generator is activated and the programmed level of energy travels from the pulse generator through the temporary pacing lead wire to the endocardium, which is known as pacemaker firing and is represented as a vertical line or spike on the electrocardiogram (ECG) recording.
• Capture refers to the successful conduction of the pacemaker impulse through the myocardium, resulting in depolarization. Capture is evidenced on the ECG by a pacemaker spike followed by either an atrial or a ventricular complex, depending on the chamber being paced. The healthcare provider can assess whether the electrical depolarization resulted in mechanical activity by observing the right atrial pressure, left atrial pressure, or pulmonary artery or arterial pressure waveforms or whether the ventricle is paced by palpating a pulse.
• Temporary pulse generator features include the following:
 The temporary pulse generator houses the controls and the energy source for pacing.
The temporary pulse generator houses the controls and the energy source for pacing.
 Pulse generators can be used for single-chamber pacing with one set of terminals at the top of the pulse generator, into which the pacing wires are inserted (via connecting cable).
Pulse generators can be used for single-chamber pacing with one set of terminals at the top of the pulse generator, into which the pacing wires are inserted (via connecting cable).
 A dual-chamber pacemaker requires two sets of terminals, one each for the atrial and ventricular wires.
A dual-chamber pacemaker requires two sets of terminals, one each for the atrial and ventricular wires.
 Different models of pacemakers use either dials or touch pads for changing the settings.
Different models of pacemakers use either dials or touch pads for changing the settings.
 The pacing rate is determined by the rate set by the dial or rate pad.
The pacing rate is determined by the rate set by the dial or rate pad.
 The AV interval dial or pad on a dual-chamber pacemaker controls the amount of time between atrial and ventricular stimulation (electronic PR interval).
The AV interval dial or pad on a dual-chamber pacemaker controls the amount of time between atrial and ventricular stimulation (electronic PR interval).
 The energy delivered to the endocardium is determined by setting the output (milliamperage [mA]) dial or pad on the pulse generator.
The energy delivered to the endocardium is determined by setting the output (milliamperage [mA]) dial or pad on the pulse generator.
 Dual-chamber pacing requires that mA are set for the atria and the ventricle.
Dual-chamber pacing requires that mA are set for the atria and the ventricle.
• The ability of the pacemaker to detect the patient’s intrinsic rhythm is determined by the pacing mode. In the asynchronous mode, the pacemaker functions as a fixed-rate pacemaker and is not able to sense any of the patient’s inherent cardiac electrical activity. In the synchronous mode, the pacemaker is able to sense the patient’s inherent cardiac electrical activity.
• The ability of the pacemaker to depolarize the myocardium depends on many variables: position of the electrode and degree of contact with viable endocardial tissue; level of energy delivered through the pacing wire; presence of hypoxia, acidosis, or electrolyte imbalances; fibrosis around the tip of the catheter; and concomitant medication therapy.2,4
• All electrical equipment in the patient’s room must be properly grounded to prevent interference from occurring.
EQUIPMENT
• Antiseptic skin preparation solution (e.g., 2% chlorhexidine-based solution)
• Sterile drapes, towels, masks, head cover, goggles or face shields, gowns, gloves, and dressings
• Balloon-tipped pacing catheter and insertion tray
• Pacing lead wire (if balloon-tipped catheter is unavailable)
• 9-V battery for pulse generator
PATIENT AND FAMILY EDUCATION
• Assess learning needs, readiness to learn, and factors that influence learning.  Rationale: This assessment enables teaching to be individualized in a manner that is meaningful to the patient and the family.
Rationale: This assessment enables teaching to be individualized in a manner that is meaningful to the patient and the family.
• Discuss basic facts about the normal conduction system, such as structure and function of the conduction system, normal and abnormal heart rhythms, and symptoms and significance of abnormal heart rhythms.  Rationale: The patient and family should understand the conduction system, why the procedure is necessary, and what potential risks and benefits are associated with this invasive procedure.
Rationale: The patient and family should understand the conduction system, why the procedure is necessary, and what potential risks and benefits are associated with this invasive procedure.
• Provide a basic description of the temporary transvenous pacemaker insertion procedure.  Rationale: The patient and family should be informed of the invasive nature of the procedure and any risks associated with the procedure. An understanding of the procedure may reduce anxiety associated with the procedure.
Rationale: The patient and family should be informed of the invasive nature of the procedure and any risks associated with the procedure. An understanding of the procedure may reduce anxiety associated with the procedure.
• Describe the precautions and restrictions required while the temporary pacemaker is in place, such as limitation of movement, avoiding handling the pacemaker or touching exposed portions of the electrodes, and situations in which the nurse should be notified (e.g., if the dressing becomes damp, if the patient experiences dizziness).  Rationale: Understanding potential limitations may improve the patient’s cooperation with restrictions and precautions.
Rationale: Understanding potential limitations may improve the patient’s cooperation with restrictions and precautions.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess the patient’s cardiac rhythm for the presence of the dysrhythmia that necessitates the initiation of temporary cardiac pacing.  Rationale: This assessment determines the need for invasive cardiac pacing.
Rationale: This assessment determines the need for invasive cardiac pacing.
• Assess the patient’s hemodynamic response to the dysrhythmia. Rhythm disturbances may reduce cardiac output significantly, with detrimental effects on perfusion of vital organs.  Rationale: This assessment determines the urgency of the procedure. It may indicate the need for temporizing measures (e.g., vasopressors or transcutaneous pacing).
Rationale: This assessment determines the urgency of the procedure. It may indicate the need for temporizing measures (e.g., vasopressors or transcutaneous pacing).
• Review current medications.  Rationale: Medications may be implicated as a cause of the dysrhythmia that led to the need for pacemaker therapy, or medications may need to be held as a result of concomitant effect. Other medications, such as antidysrhythmics, may alter the pacing threshold.
Rationale: Medications may be implicated as a cause of the dysrhythmia that led to the need for pacemaker therapy, or medications may need to be held as a result of concomitant effect. Other medications, such as antidysrhythmics, may alter the pacing threshold.
• Review the patient’s current laboratory study results, including chemistry, electrolyte profile, arterial blood gases, coagulation profile, platelet count, and cardioactive medication levels.  Rationale: This review assists in determining whether inserting the pacemaker was precipitated by metabolic disturbances or medication toxicity and establishes the pacing milieu. The review provides the healthcare provider with information regarding the risk for abnormal bleeding during or after the procedure is performed.
Rationale: This review assists in determining whether inserting the pacemaker was precipitated by metabolic disturbances or medication toxicity and establishes the pacing milieu. The review provides the healthcare provider with information regarding the risk for abnormal bleeding during or after the procedure is performed.
• Assess the presence and position of the central venous access.  Rationale: The temporary transvenous pacing catheter is advanced through the central venous circulation. If access already is established, proper placement must be ensured before the pacing catheter can be advanced through the circulatory system.
Rationale: The temporary transvenous pacing catheter is advanced through the central venous circulation. If access already is established, proper placement must be ensured before the pacing catheter can be advanced through the circulatory system.
Patient Preparation
• Verify correct patient using two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand preprocedural teaching. Answer questions as they arise and reinforce information as needed.  Rationale: Evaluates and reinforces understanding of previously taught information.
Rationale: Evaluates and reinforces understanding of previously taught information.
• Obtain informed consent.  Rationale: Informed consent protects the rights of the patient and makes a competent decision possible for the patient; however, in emergency circumstances, time may not allow a consent form to be signed.
Rationale: Informed consent protects the rights of the patient and makes a competent decision possible for the patient; however, in emergency circumstances, time may not allow a consent form to be signed.
• Perform a pre-procedure verification and time out, if non-emergent.  Rationale: Ensures patient safety.
Rationale: Ensures patient safety.
• Connect the patient to a 5-lead monitoring system or to a 12-lead ECG machine.  Rationale: This monitoring facilitates the placement of the balloon-tipped catheter by indicating the position of the catheter during its placement. Also, it allows for monitoring of the patient’s cardiac rhythm during the procedure.
Rationale: This monitoring facilitates the placement of the balloon-tipped catheter by indicating the position of the catheter during its placement. Also, it allows for monitoring of the patient’s cardiac rhythm during the procedure.
• Prescribe and ensure that pain medication and/or sedation is administered.  Rationale: Medication may be indicated depending on the patient’s level of anxiety and pain. Sedation or pain medication may not be possible if the patient’s condition is hemodynamically unstable.
Rationale: Medication may be indicated depending on the patient’s level of anxiety and pain. Sedation or pain medication may not be possible if the patient’s condition is hemodynamically unstable.
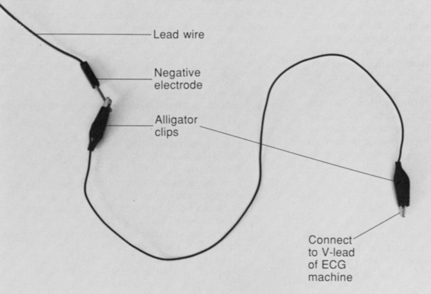
FIGURE 53-2 Alligator clips. ECG, electrocardiogram.
References
1. Dahlberg, ST. Temporary cardiac pacing. In Irwin RS, et al, eds. : Procedures and techniques in intensive care medicine,, ed 6, Philadelphia: Lippincott Williams & Wilkins, 2008.
![]() 2. Espiritu, JD, Keller, CA. Pneumomediastinum and subcutaneous emphysema from pacemaker placement. Pacing Clin Electrophysiol. 2001; 24:1041–1042.
2. Espiritu, JD, Keller, CA. Pneumomediastinum and subcutaneous emphysema from pacemaker placement. Pacing Clin Electrophysiol. 2001; 24:1041–1042.
3. Harrigan, RA, Chan, TC, Moonblatt, S, et al. Temporary transvenous pacemaker placement in the emergency -department. J Emerg Med. 2007; 32:105–111.
4. Huysmans, W, Budts, W. Late free atrial wall rupture after percutaneous atrial septal defect closure and transvenous pacemaker implantation. Catheter Cardiovasc Interv. 2008; 72:286–288.
![]() 5. Macedo, W, Jr., et al, Ultrasonographic guidance of -transvenous pacemaker insertion in the emergency -department. a report of three cases. J Emerg Med 1999; 17:491–496.
5. Macedo, W, Jr., et al, Ultrasonographic guidance of -transvenous pacemaker insertion in the emergency -department. a report of three cases. J Emerg Med 1999; 17:491–496.
![]() 6. Norman, EM, Critical care extra. critical questions-avoiding electrical hazards, temporary pacing wires. Am J Nurs 1998; 98:16GG-HH.
6. Norman, EM, Critical care extra. critical questions-avoiding electrical hazards, temporary pacing wires. Am J Nurs 1998; 98:16GG-HH.
![]() 7. O’Grady, NP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.
7. O’Grady, NP, et al. Guidelines for the prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.