Temporary Transcutaneous (External) Pacing
PREREQUISITE NURSING KNOWLEDGE
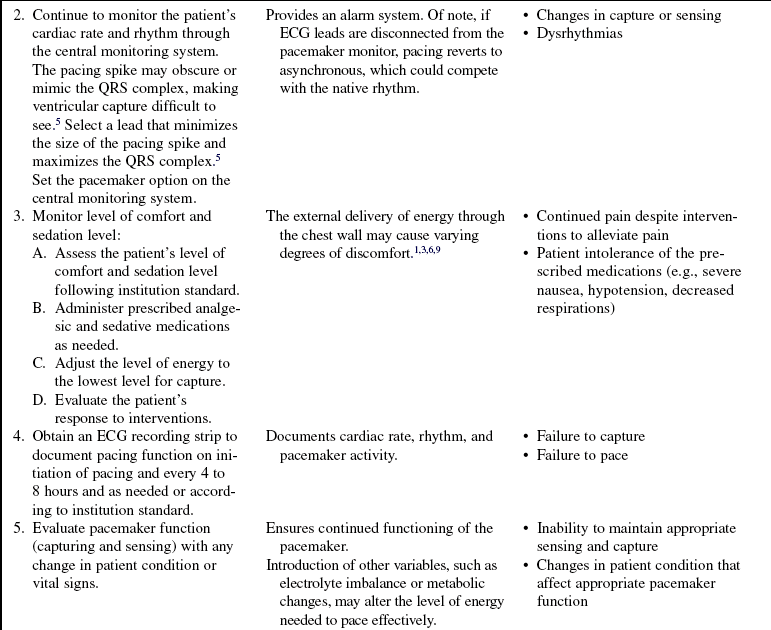
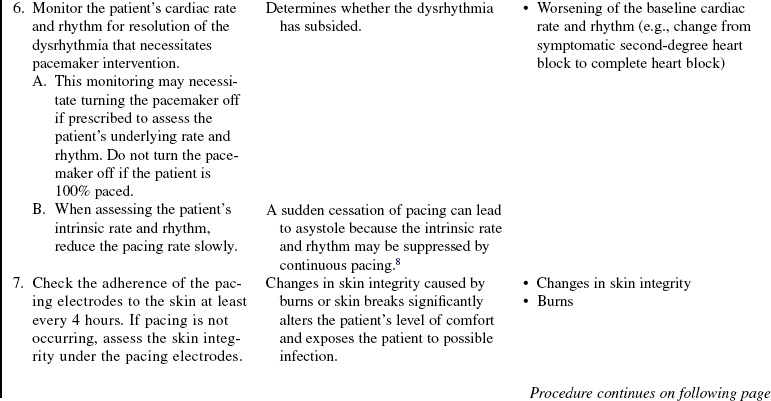
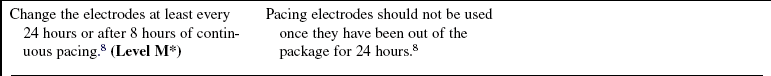
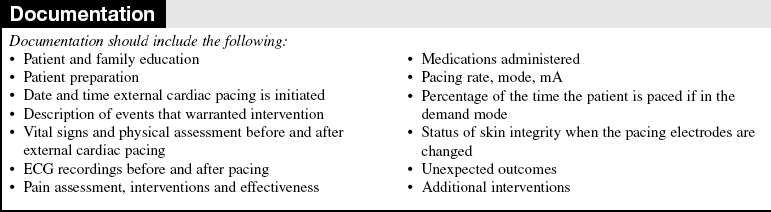
• Knowledge of cardiac anatomy and physiology is needed.
• Knowledge of cardiac monitoring (see Procedure 57) is necessary.
• The ability to interpret basic dysrhythmias is needed.
• Knowledge of temporary pacemaker function and expected patient responses to pacemaker therapy is needed.
• Clinical and technical competence in the use of the external pacing equipment is necessary.
• Indications for transcutaneous pacing are as follows1,6:
 Symptomatic bradycardia unresponsive to medications
Symptomatic bradycardia unresponsive to medications
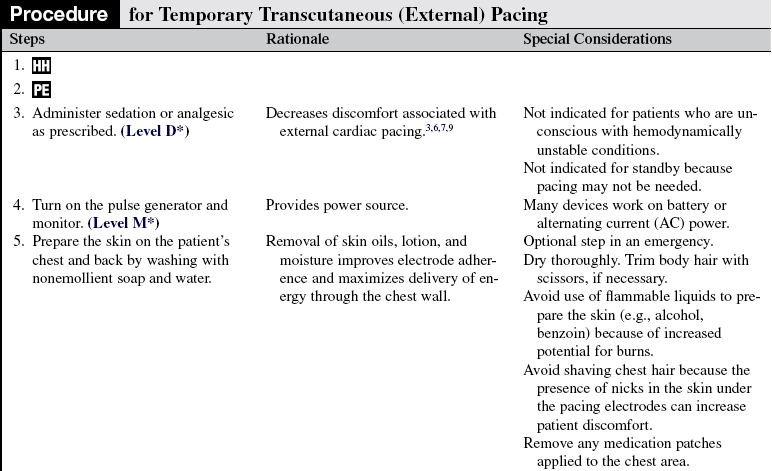
 In standby mode for the following rhythms in acute myocardial infarction setting4:
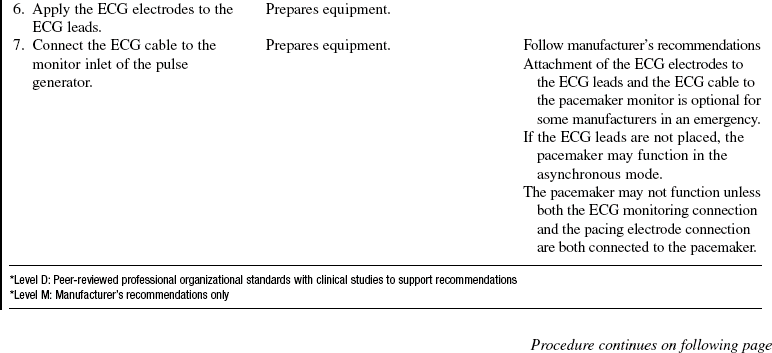
In standby mode for the following rhythms in acute myocardial infarction setting4:
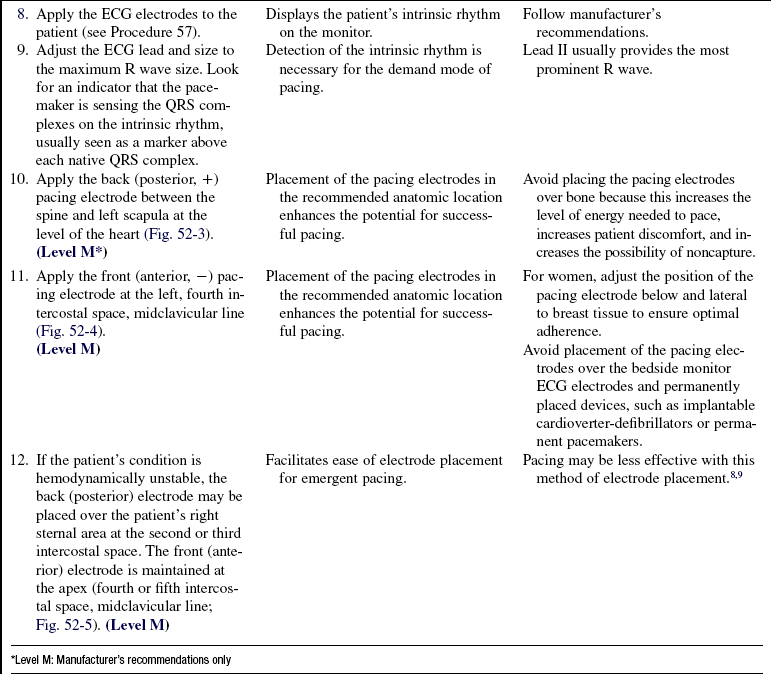
• Temporary transvenous pacing is indicated when prolonged pacing is needed.
• Contraindications for transcutaneous pacing are as follows2,6:
• Pacing is contraindicated in severe hypothermia because cold ventricles are more prone to ventricular fibrillation and are more resistant to defibrillation.6 Transcutaneous pacing for an asystolic arrest is no longer recommended in the 2005 Advanced cardiac life support (ACLS) guidelines because of a lack of evidence that it improves survival rates.2
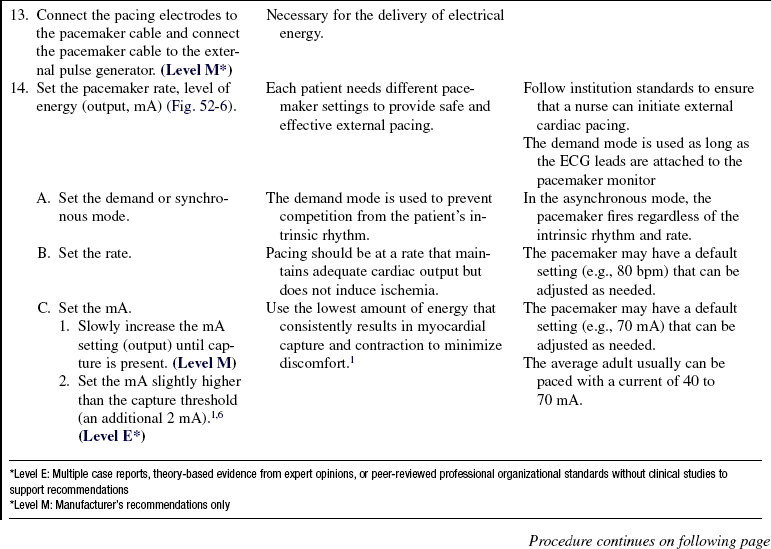
• External cardiac pacing is a temporary method of stimulating ventricular myocardial depolarization through the chest wall via two large pacing electrodes (patches). The electrodes are placed on the anterior and posterior chest wall and are attached by a cable to an external pulse generator (Fig. 52-1). The external pulse generator delivers energy (milliamps) to the myocardium based on the set pacing rate, output, and sensitivity. Some models of external pulse generators are combined with an external defibrillator, and the electrodes of these models may be used for pacing and defibrillation.
• Sensitivity refers to the ability of the pacemaker to detect intrinsic myocardial activity.
• In the nondemand or asynchronous mode, pacing occurs at the set rate regardless of the patient’s intrinsic rate. In the demand or synchronous mode, the pacemaker senses intrinsic myocardial activity and paces when the intrinsic cardiac rate is lower than the set rate on the external pulse generator.
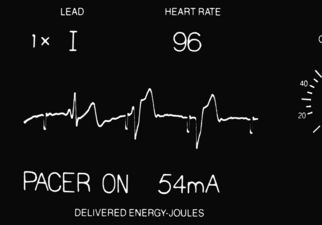
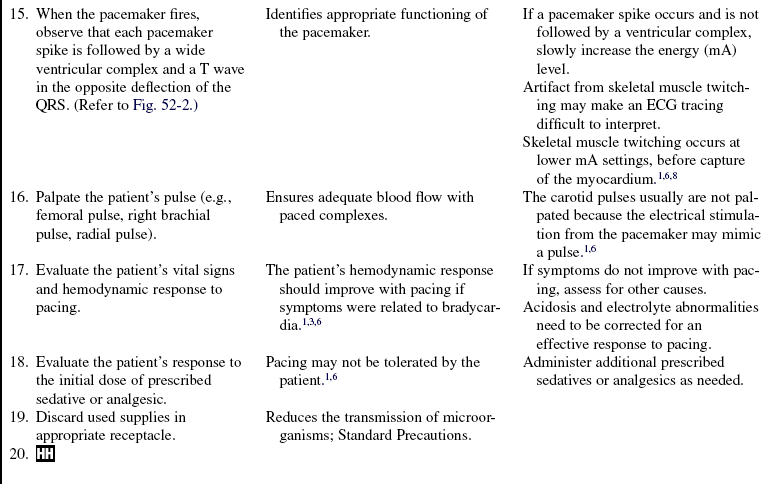
• Pacing occurs when the external pulse generator delivers enough energy through the pacing electrodes to the myocardium, which is known as pacemaker firing and is represented as a spike on the electrocardiographic (ECG) tracing (Fig. 52-2).
• Electrical capture occurs when the pacemaker delivers enough energy to the myocardium so that depolarization occurs. Capture is seen on the ECG with a pacemaker spike followed by a ventricular complex. The ventricular complex occurs after the pacemaker spike, and the QRS is wide, with the initial and terminal deflections in opposite directions. In Fig. 52-2, complexes 2 and 3 begin with a downward (negative) deflection and end with an upward (positive) direction. Mechanical capture occurs when a paced QRS complex results in a palpable pulse.
• Standby pacing is when the pacing electrodes are applied in anticipation of possible use but pacing is not needed at the time.
EQUIPMENT
Additional equipment to have available as needed includes the following:
PATIENT AND FAMILY EDUCATION
• Assess learning needs, readiness to learn, and factors that influence learning.  Rationale: This assessment reveals the patient’s and family’s knowledge so that teaching can be individualized to be meaningful to the patient and family.
Rationale: This assessment reveals the patient’s and family’s knowledge so that teaching can be individualized to be meaningful to the patient and family.
• Discuss basic facts about the normal conduction system, the reason external cardiac pacing is indicated, and what happens to the patient when pacing occurs.  Rationale: This discussion assists the patient and family in recognizing the need for external pacing and what to expect when pacing occurs.
Rationale: This discussion assists the patient and family in recognizing the need for external pacing and what to expect when pacing occurs.
• Discuss interventions to alleviate discomfort.  Rationale: This discussion provides the patient with an opportunity to validate perceptions. It gives the patient and family knowledge that interventions are used to minimize the level of discomfort.
Rationale: This discussion provides the patient with an opportunity to validate perceptions. It gives the patient and family knowledge that interventions are used to minimize the level of discomfort.
• If indicated, inform the patient and family of the possibility of the need for transvenous or permanent pacing support.  Rationale: This information prepares the patient and family for the possibility of additional therapy. If permanent pacing is necessary, the patient and family need further instruction about possible lifestyle modifications and follow-up visits and information about the pacemaker to be implanted.
Rationale: This information prepares the patient and family for the possibility of additional therapy. If permanent pacing is necessary, the patient and family need further instruction about possible lifestyle modifications and follow-up visits and information about the pacemaker to be implanted.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess the patient’s cardiac rate and rhythm for the presence of dysrhythmias that indicate the need for external cardiac pacing.  Rationale: Recognition of a dysrhythmia is the first step in determining the need for external cardiac pacing or placing the external pacemaker on standby.
Rationale: Recognition of a dysrhythmia is the first step in determining the need for external cardiac pacing or placing the external pacemaker on standby.
• Determine the patient’s hemodynamic response to the dysrhythmia, such as the presence or absence of a pulse; presence of hypotension, altered level of consciousness; dizziness; shortness of breath; nausea and vomiting; cool, clammy, diaphoretic skin; or the development of chest pain.  Rationale: The decision to initiate pacing depends on the effect of the dysrhythmia on the patient’s cardiac output.
Rationale: The decision to initiate pacing depends on the effect of the dysrhythmia on the patient’s cardiac output.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand pre-procedural teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: This communication evaluates and reinforces understanding of previously taught information.
Rationale: This communication evaluates and reinforces understanding of previously taught information.
• Maintain bedside ECG monitoring.  Rationale: External pacing units do not provide central monitoring or dysrhythmia detection.
Rationale: External pacing units do not provide central monitoring or dysrhythmia detection.
• Administer sedative or analgesic medication as prescribed to a conscious patient before initiation of pacing.  Rationale: External cardiac pacing is uncomfortable.
Rationale: External cardiac pacing is uncomfortable.
• Assist the patient to the supine position and expose the patient’s torso while maintaining modesty.  Rationale: This positioning prepares for electrode (patch) placement.
Rationale: This positioning prepares for electrode (patch) placement.

Figure 52-3 Location of the posterior (back) pacing electrode. (Aehlert B: ACLS study guide, ed 3, St Louis, 2007, Mosby, 229.)
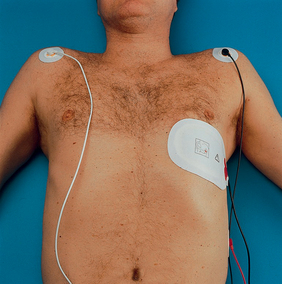
Figure 52-4 Location of the anterior (front) pacing electrode. (Aehlert B: ACLS study guide, ed 3, St Louis, 2007, Mosby, 229.)
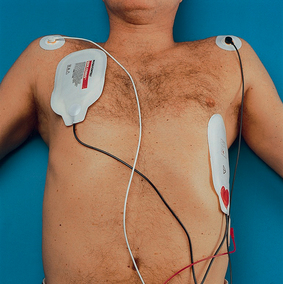
Figure 52-5 Location of anterior-lateral pacing electrodes. (Aehlert B: ACLS study guide, ed 3, St Louis, 2007, Mosby, 229.)

Figure 52-6 Controls for external pacemaker settings.
References
1. Aehlert, B. ACLS study guide,, ed 3. St Louis: Mosby; 2007.
![]() 2. American Heart Association, Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care: g. part5: electrical therapies: automated external defi brillators,defi brillation, cardioversion, and pacin. Circulation. 2005; 112(Suppl IV):IV-35–IV-45.
2. American Heart Association, Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care: g. part5: electrical therapies: automated external defi brillators,defi brillation, cardioversion, and pacin. Circulation. 2005; 112(Suppl IV):IV-35–IV-45.
![]() 3. American Heart Association, Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. part 7. 3management of symptomatic bradycardia and tachycardia. Circulation. 2005; 112(Suppl IV):IV-67–IV-77.
3. American Heart Association, Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care. part 7. 3management of symptomatic bradycardia and tachycardia. Circulation. 2005; 112(Suppl IV):IV-67–IV-77.
![]() 4. Antman, EM, et al, ACC/AHA guidelines for management of patients with ST-elevation myocardial infarction. a -report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2004; 100:e82–e293.
4. Antman, EM, et al, ACC/AHA guidelines for management of patients with ST-elevation myocardial infarction. a -report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 2004; 100:e82–e293.
![]() 5. Drew, B, et al, Practice standards for electrocardiographic monitoring in hospital settings. an American Heart -Association scientific statement from the Councils on -Cardiovascular Nursing, Clinical Cardiology, and -Cardiovascular Disease in the Youngendorsed by the -International Society of Computerized Electrocardiology and the American Association of Critical-Care Nurses. Circulation 2004; 110:2721–2746.
5. Drew, B, et al, Practice standards for electrocardiographic monitoring in hospital settings. an American Heart -Association scientific statement from the Councils on -Cardiovascular Nursing, Clinical Cardiology, and -Cardiovascular Disease in the Youngendorsed by the -International Society of Computerized Electrocardiology and the American Association of Critical-Care Nurses. Circulation 2004; 110:2721–2746.
6. Field J, ed.. Part 4. ACLS core cases, bradycardia case in advanced cardiac life support provider manual. American Heart Association: Dallas, 2006.
7. Gibson, T. A practical guide to external cardiac pacing. Nursing Standard. 2008; 22:20–48.
8. Medtronic Physio-Control Corp. LIFEPAK 20 defibrillator/monitor operating instructions. Inc. Redmond, WA: Physio-Control; 2008.
![]() 9. Zoll, P. Noninvasive temporary cardiac pacing. J Electrophys. 1987; 1:2–161.
9. Zoll, P. Noninvasive temporary cardiac pacing. J Electrophys. 1987; 1:2–161.
Doukky, R, et al, Using transcutaneous cardiac pacing to best advantage. how to ensure successful capture and avoid complications. J Crit Illness 2003; 5:25–219.
Jacobson, C, Marzlin, K, Webner, C, Electrical management of arrhythmias in cardiovascular nursing practice Chapter 17. Cardiovascular Nursing Education Associates, Burien, WA, 2007.