Epicardial Pacing Wire Removal
Epicardial Pacing Wire Removal
PREREQUISITE NURSING KNOWLEDGE
• Knowledge of the cardiovascular anatomy and physiology is necessary.
• Knowledge of principles of aseptic technique is needed.1,4,6,7
• Knowledge of placement and function of epicardial pacing wires is necessary.
• Advanced cardiac life support knowledge and skills are needed.
• Principles of general electrical safety need to be applied with use of temporary epicardial pacemaker wires.
• Gloves always should be worn when handling epicardial pacemaker electrodes to prevent microshock because even small amounts of electrical current can cause serious dysrhythmias if they are transmitted to the heart.
• Knowledge of cardiac dysrhythmias and treatment of life-threatening dysrhythmias is necessary.
• Relative contraindications to epicardial pacing wire removal include bleeding, abnormal coagulation study results, presence of dysrhythmias that necessitate pacing assistance, and compromised hemodynamic status.
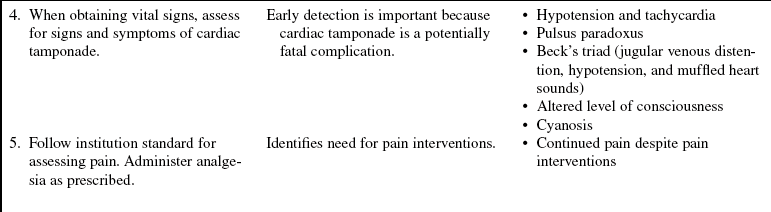
• Knowledge of signs and symptoms of cardiac tamponade is needed (e.g., hemodynamic instability, dyspnea, muffled heart sounds, diaphoresis, equalizing pulmonary artery pressures, jugular venous distention, pulsus paradoxus, altered level of consciousness).
EQUIPMENT
• Gown, goggles or face shield with mask, nonsterile gloves
• Antiseptic solution (e.g., 2% chlorhexidine-based solution)
Additional equipment that may be needed includes the following:
PATIENT AND FAMILY EDUCATION
• Assess patient and family readiness to learn, and identify factors that affect learning.  Rationale: This assessment allows the nurse to individualize teaching.
Rationale: This assessment allows the nurse to individualize teaching.
• Provide information about the epicardial pacing wires, the reason for their removal, and an explanation of the procedure.  Rationale: This information helps the patient and family to understand the procedure and why it is needed and may decrease anxiety.
Rationale: This information helps the patient and family to understand the procedure and why it is needed and may decrease anxiety.
• Explain the patient’s expected participation during and after the procedure.  Rationale: Encourages patient participation in the treatment plan and may decrease anxiety.
Rationale: Encourages patient participation in the treatment plan and may decrease anxiety.
• Explain that the patient may feel mild pain and a burning or pulling sensation during the procedure.2,5  Rationale: This explanation prepares the patient for the procedure.
Rationale: This explanation prepares the patient for the procedure.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess the patient’s baseline cardiovascular, hemodynamic, and peripheral vascular status.  Rationale: This assessment provides data that can be used for comparison with posremoval assessment data and hemodynamic values.
Rationale: This assessment provides data that can be used for comparison with posremoval assessment data and hemodynamic values.
• Assess the patient’s current laboratory data, including electrolyte and coagulation study results.  Rationale: This assessment identifies laboratory abnormalities. Baseline coagulation studies are helpful in determining the patient’s risk for bleeding. Electrolyte abnormalities may increase cardiac irritability.
Rationale: This assessment identifies laboratory abnormalities. Baseline coagulation studies are helpful in determining the patient’s risk for bleeding. Electrolyte abnormalities may increase cardiac irritability.
• Ensure that the patient is not receiving anticoagulation therapy.  Rationale: Epicardial pacing wires are not usually discontinued while the patient is receiving anticoagulation therapy; follow physician prescription.
Rationale: Epicardial pacing wires are not usually discontinued while the patient is receiving anticoagulation therapy; follow physician prescription.
Patient Preparation
• Verify correct patient with two patient identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand preprocedural teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: Evaluates and reinforces understanding of previously taught information.
Rationale: Evaluates and reinforces understanding of previously taught information.
• Remove epicardial pacing wires at least the day before discharge (approximately 24 hours or longer).3,6,9  Rationale: Removal at this time provides time for observation for potential complications.
Rationale: Removal at this time provides time for observation for potential complications.
• Administer prescribed analgesic medication before removing the epicardial pacing wires.8  Rationale: Analgesics may minimize discomfort during epicardial pacing wire removal.
Rationale: Analgesics may minimize discomfort during epicardial pacing wire removal.
• Determine the patency of an intravenous (IV) catheter.  Rationale: A patent IV is necessary should emergency fluids or medications be needed.
Rationale: A patent IV is necessary should emergency fluids or medications be needed.
• Ensure that patient has electrocardiographic (ECG) monitoring.  Rationale: ECG monitoring provides assessment for the presence of potential dysrhythmias during epicardial wire removal.
Rationale: ECG monitoring provides assessment for the presence of potential dysrhythmias during epicardial wire removal.
References
1. AORN, Association of periOperative Registered NursesPerioperative standards and recommended practices,. Denver: AORN, 2008.
![]() 2. Carroll, KC, Reeves, LM, Andersen, G, et al. Risks associated with removal of ventricular epicardial pacing wires after cardiac surgery. Am J Crit Care. 1998; 7(6):444–449.
2. Carroll, KC, Reeves, LM, Andersen, G, et al. Risks associated with removal of ventricular epicardial pacing wires after cardiac surgery. Am J Crit Care. 1998; 7(6):444–449.
3. Clark, L, Bedside nurses removing epicardial pacer wires. from concept to practice. Can J Cardiovascr Nurs. 2007; 17(1):27–30.
4. Conte, JV, et al. The Johns Hopkins manual of cardiac -surgical care, ed 2. Philadelphia: Mosby; 2008.
5. Mullin, MH, Roschkov, S, Jensen, L, et al. Sensations -during removal of epidural pacing wires after coronary -artery bypass graft surgery. Heart Lung. 2009; 38(5):337–381.
6. Pennsylvania Patient Safety Authority. Minimizing complications from temporary epicardial pacing wires after cardiac surgery. PA-PSRS Patient Safe Advis. 2006; 3(1):1–6.
7. Phillips, N. Berry & Kohn’s operating room technique,, ed 11. St Louis: Mosby; 2007.
8. Roschkov, S, Jensen, L. Coronary artery bypass graft -patients’ pain perception during epicardial pacing wire -removal. Can J Cardiovasc Nurs. 14, 2004.
![]() 9. Wollan, DL, Removal of epicardial pacing wires. an -expanded role for nurses. Prog Cardiovasc Nurs. 1995; 10(4):21–26.
9. Wollan, DL, Removal of epicardial pacing wires. an -expanded role for nurses. Prog Cardiovasc Nurs. 1995; 10(4):21–26.
![]() Gentry, WH, Hassan, AA, Complications of retained epicardial pacing wires. an unusual bronchial foreign body. Ann Thorac Surg. 1993; 56(6):1391–1393.
Gentry, WH, Hassan, AA, Complications of retained epicardial pacing wires. an unusual bronchial foreign body. Ann Thorac Surg. 1993; 56(6):1391–1393.
Hornig, GS, Ashley, E, Balsam, L, et al, Progressive dyspnea after CABG. complication of retained epicardial pacing wires. Ann Thorac Surg 2008; 86:1352–1354.
![]() Matwiyoff, GN, McKinlay, JR. Transepidermal migration of external cardiac pacing wire presenting as a cutaneous nodule. J Am Acad Dermatol. 42(5), 2000.
Matwiyoff, GN, McKinlay, JR. Transepidermal migration of external cardiac pacing wire presenting as a cutaneous nodule. J Am Acad Dermatol. 42(5), 2000.
![]() Meier, DJ, Tamirisa, KP, Eitzman, DT. Ventricular tachycardia associated with transmyocardial migration of an epicardial pacing wire. Ann Thorac Surg. 2004; 77:1077–1079.
Meier, DJ, Tamirisa, KP, Eitzman, DT. Ventricular tachycardia associated with transmyocardial migration of an epicardial pacing wire. Ann Thorac Surg. 2004; 77:1077–1079.
Rothrock, JC. Alexander’s care of the patient in surgery,, ed 13. St Louis: Mosby; 2007.