Atrial Overdrive Pacing (Perform)
Atrial Overdrive Pacing (Perform)
PREREQUISITE NURSING KNOWLEDGE
• Knowledge of the anatomy and physiology of the cardiovascular system, principles of cardiac conduction, and basic and advanced dysrhythmia interpretation is necessary.
• Knowledge of pacemaker function and patient response to pacemaker therapy is needed.
• Principles of general electrical safety need to be applied with use of temporary invasive pacing.
• Gloves always should be worn when handling pacemaker electrodes to prevent microshock because even small amounts of electrical current can cause serious dysrhythmias if they are transmitted to the heart.
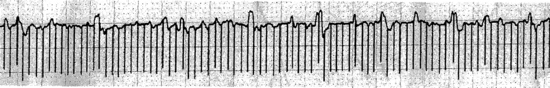
• Clinical and technical competence related to the use of a temporary atrial pacemaker pulse generator and the rapid atrial pacing feature is needed (Fig. 48-1).
• Advanced cardiac life support knowledge and skills are necessary.
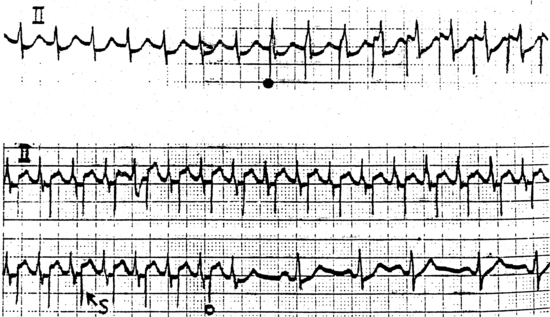
• Supraventricular dysrhythmias (e.g., atrial flutter, reentrant atrial tachycardia, atrioventricular [AV] nodal reentry tachycardia, reentrant tachycardias that use an accessory pathway, such as Wolff-Parkinson-White [WPW] syndrome) sometimes can be terminated by overdrive atrial pacing.
• Atrial fibrillation occasionally terminates with overdrive atrial pacing, but this is not a reliable therapy for atrial fibrillation.
• Overdrive atrial pacing is performed most commonly with epicardial atrial pacing wires placed during cardiac surgery. A transvenous atrial pacing lead with an active fixation tip to help keep the lead in the atrium also can be used.
• Overdrive atrial pacing involves the delivery of short bursts of rapid pacing stimuli through an epicardial atrial pacing wire or a transvenous lead in the atrium. The physician or advanced practice nurse determines the duration and rate of the burst.
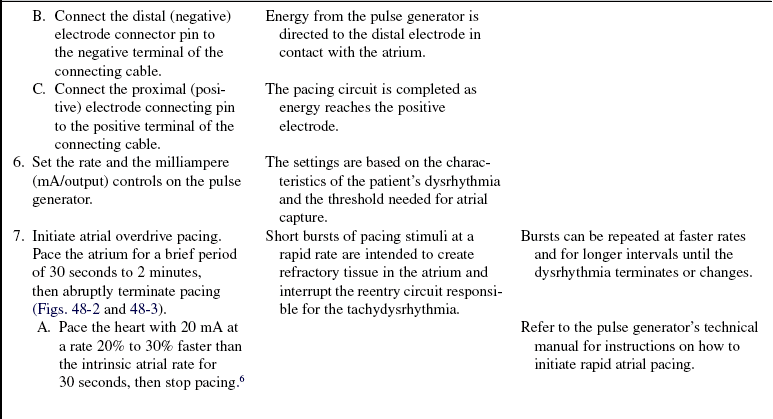
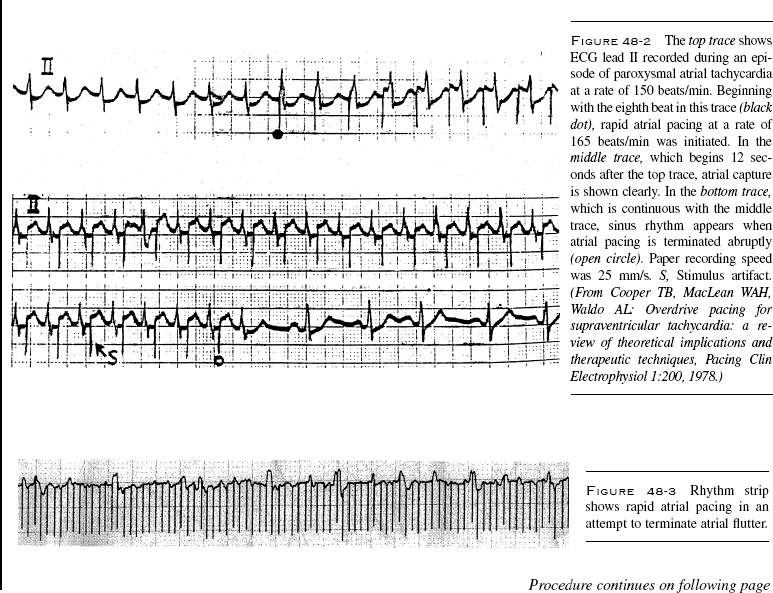
 One approach to overdrive pacing is to atrial pace the heart with 20 milliampere (mA) at a rate 20% to 30% faster than the intrinsic atrial rate for 30 seconds, then stop pacing. An alternate approach is to initiate atrial pacing at a rate 20 beats/min faster than the intrinsic atrial rate; if 1:1 capture does not occur after 30 seconds, the paced rate can be increased by 20 beats/min; repeat every 30 seconds until 1:1 capture is achieved. Continue pacing until the heart rate decreases from AV block (e.g., 2:1, 3:1) or 1 to 2 minutes of 1:1 pacing have occurred, then stop pacing.6
One approach to overdrive pacing is to atrial pace the heart with 20 milliampere (mA) at a rate 20% to 30% faster than the intrinsic atrial rate for 30 seconds, then stop pacing. An alternate approach is to initiate atrial pacing at a rate 20 beats/min faster than the intrinsic atrial rate; if 1:1 capture does not occur after 30 seconds, the paced rate can be increased by 20 beats/min; repeat every 30 seconds until 1:1 capture is achieved. Continue pacing until the heart rate decreases from AV block (e.g., 2:1, 3:1) or 1 to 2 minutes of 1:1 pacing have occurred, then stop pacing.6
 Successive bursts usually are performed at gradually increasing rates (maximal capability of the pulse generator for overdrive atrial pacing is 800 pulses/min) and may be delivered for up to 2 minutes.7
Successive bursts usually are performed at gradually increasing rates (maximal capability of the pulse generator for overdrive atrial pacing is 800 pulses/min) and may be delivered for up to 2 minutes.7
• The atrial pacing wire or atrial pacing lead needs to be accurately identified with initiation of overdrive pacing because pacing the ventricle at rapid rates may result in ventricular tachycardia or ventricular fibrillation.
• Rapid atrial pacing may result in degeneration of the atrial rhythm to atrial fibrillation with a rapid ventricular response. This pacemaker-induced atrial fibrillation usually does not sustain itself for more than a few minutes before it converts to normal sinus rhythm.6
• If an accessory pathway is present, rapid atrial pacing can result in conduction to the ventricles over the accessory pathway, leading to ventricular fibrillation.
• Overdrive suppression of the sinus node may result in periods of bradycardia, asystole, junctional or ventricular escape rhythms, or polymorphic ventricular tachycardia on termination of the atrial overdrive pacing and the atrial tachydysrhythmia.
• Conversion of an atrial tachydysrhythmia can result in dislodgment of atrial thrombus and embolization of clots to the pulmonary or systemic circulation.
EQUIPMENT
• External pulse generator capable of rapid atrial pacing
• Connecting cable (between the pulse generator and the patient’s pacemaker leads)
• Cardiac monitor and recorder
• Electrocardiogram (ECG) electrodes
• Double alligator clip or wire with connector pins (if needed to create a ground wire)
• Materials for epicardial pacing wire site care:
• Insulating material for epicardial pacing wires or transvenous pacing electrode connector pins (e.g., finger cots, glove, needle caps)
Additional equipment to have available as needed includes the following:
PATIENT AND FAMILY EDUCATION
• Explain the procedure and its purpose to the patient and family.  Rationale: This explanation decreases patient and family anxiety and promotes cooperation with the procedure.
Rationale: This explanation decreases patient and family anxiety and promotes cooperation with the procedure.
• Reassure the patient that atrial pacing usually cannot be felt and that any sensation most likely will be a “fluttering” feeling in the chest.  Rationale: This reassurance prepares the patient and may decrease the patient’s anxiety.
Rationale: This reassurance prepares the patient and may decrease the patient’s anxiety.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess the patient’s ECG rhythm and intervals, noting atrial and ventricular rates.  Rationale: This assessment determines baseline cardiac conduction.
Rationale: This assessment determines baseline cardiac conduction.
• Assess the patient’s vital signs and hemodynamic parameters.  Rationale: This assessment determines baseline cardiovascular function.
Rationale: This assessment determines baseline cardiovascular function.
• Assess for signs and symptoms that might be caused by the dysrhythmia (e.g., shortness of breath, dizziness, nausea, chest pain, signs of poor peripheral perfusion).  Rationale: The patient’s response to the dysrhythmia is determined.
Rationale: The patient’s response to the dysrhythmia is determined.
• Assess the patency of the intravenous access.  Rationale: Intravenous access is needed for possible administration of fluids and medications.
Rationale: Intravenous access is needed for possible administration of fluids and medications.
• Note any medications that might have an effect on the patient’s cardiac rhythm or hemodynamic parameters (e.g., beta blockers, calcium channel blockers, antidysrhythmics, digoxin).  Rationale: Knowledge of medication therapy can alert the healthcare providers to potential cardiac rhythms (e.g., bradycardia or atrioventricular block) after termination of the atrial dysrhythmia.
Rationale: Knowledge of medication therapy can alert the healthcare providers to potential cardiac rhythms (e.g., bradycardia or atrioventricular block) after termination of the atrial dysrhythmia.
• Review the patient’s coagulation study results.  Rationale: Therapeutic coagulation levels may decrease the risk of embolization.2,4,6,7
Rationale: Therapeutic coagulation levels may decrease the risk of embolization.2,4,6,7
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Obtain informed consent (may not be possible in an emergency).  Rationale: Informed consent protects the rights of the patient and makes a competent decision possible for the patient.
Rationale: Informed consent protects the rights of the patient and makes a competent decision possible for the patient.
• Ensure that the patient and family understand pre-procedural teaching. Answer questions as they arise and reinforce information as needed.  Rationale: This communication evaluates and reinforces understanding of previously taught information.
Rationale: This communication evaluates and reinforces understanding of previously taught information.
• Perform a pre-procedure verification and time out, if non-emergent.  Rationale: Ensures patient safety.
Rationale: Ensures patient safety.
• Initiate continuous bedside cardiac monitoring (if not already in place).  Rationale: The patient’s cardiac rate and rhythm must be visible at the bedside during the procedure to determine atrial capture during pacing and to evaluate the response of the patient’s cardiac rate and rhythm after pacing.
Rationale: The patient’s cardiac rate and rhythm must be visible at the bedside during the procedure to determine atrial capture during pacing and to evaluate the response of the patient’s cardiac rate and rhythm after pacing.
• Obtain a 12-lead ECG as needed.  Rationale: The ECG may aid in determining the patient’s baseline cardiac rhythm.
Rationale: The ECG may aid in determining the patient’s baseline cardiac rhythm.
• Assist the patient to a supine position.  Rationale: This position facilitates access to the epicardial pacemaker wires or the transvenous atrial pacing lead wire.
Rationale: This position facilitates access to the epicardial pacemaker wires or the transvenous atrial pacing lead wire.
• Place a blood pressure cuff on the patient’s arm and obtain the patient’s blood pressure or obtain the patient’s blood pressure from the arterial catheter.  Rationale: This aids in assessment of the patient’s hemodynamic response to rapid atrial pacing.
Rationale: This aids in assessment of the patient’s hemodynamic response to rapid atrial pacing.
References
1. Batra, AS, Balaji, S, Post operative temporary epicardial pacing. when, how and why. Ann Pediatr Cardiol. 2008; 1(2):120–125.
2. Blomström-Lundqvist C, et, al, ACC/AHA/ESC guidelines for the management of patients with supraventricular -arrhythmias. executive summarya report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines (Writing Committee to Develop Guidelines for the Management of Patients With Supraventricular Arrhythmias). J Am Coll Cardiol 2008; 42:1493–1531.
![]() 3. O’Grady, NP, et al. Guidelines for the prevention of -intravascular catheter-related infections. Am J Infect -Control. 2002; 30:476–489.
3. O’Grady, NP, et al. Guidelines for the prevention of -intravascular catheter-related infections. Am J Infect -Control. 2002; 30:476–489.
4. Oligin, JE, Zipes, DP, et al, Specific arrhythmias. diagnosis and treatmentLibby P, ed. Braunwald’s heart disease: a textbook of cardiovascular medicine, ed 8, Philadelphia: Saunders/Elsevier, 2008.
![]() 5. Overbay, D, Criddle, L. Mastering temporary invasive -cardiac pacing. Crit Care Nurs. 2004; 24(3):25–32.
5. Overbay, D, Criddle, L. Mastering temporary invasive -cardiac pacing. Crit Care Nurs. 2004; 24(3):25–32.
6. Palazzo, MO. Atrial fibrillation and postoperative -cardiac surgery patient. Crit Care Nurs Clin North Am. 2007; 19:395–402.
7. Smith, W, Hood, M. Arrhythmias. In: Sidebotham D, et al, eds. Cardiothoracic critical care. Philadelphia: Butterworth-Heinemann, 2007.