Atrial Electrogram
PREREQUISITE NURSING KNOWLEDGE
• Understanding of the anatomy and physiology of the cardiovascular system, principles of cardiac conduction, and basic dysrhythmia interpretation is necessary.
• Principles of general electrical safety apply with use of temporary invasive pacing. Gloves should always be worn when handling pacing electrodes to prevent microshock because even small amounts of electrical current can cause serious dysrhythmias if transmitted to the heart.
• Advanced cardiac life support knowledge and skills are needed.
• Atrial electrograms (AEGs) offer a more definitive means for assessing and interpreting rhythm abnormalities.4
• The American Heart Association Practice Standards for Electrocardiographic Monitoring in Hospital Settings recommend recording an AEG whenever tachycardia of unknown origin develops in a patient after cardiac surgery.2,4
• Indications for AEG are as follows:
 When atrial activity is not clearly detected on electrocardiographic (ECG) monitoring
When atrial activity is not clearly detected on electrocardiographic (ECG) monitoring
 For determination of the relationship between atrial and ventricular activity
For determination of the relationship between atrial and ventricular activity
 For differentiation of wide-complex rhythms (i.e., ventricular tachycardia and supraventricular tachycardia with aberrant ventricular conduction)
For differentiation of wide-complex rhythms (i.e., ventricular tachycardia and supraventricular tachycardia with aberrant ventricular conduction)
 For differentiation of narrow-complex supraventricular tachycardias (i.e., sinus tachycardia, atrial tachycardia, paroxysmal supraventricular tachycardia, atrial flutter, atrial fibrillation with relatively regular RR intervals, or junctional tachycardia)
For differentiation of narrow-complex supraventricular tachycardias (i.e., sinus tachycardia, atrial tachycardia, paroxysmal supraventricular tachycardia, atrial flutter, atrial fibrillation with relatively regular RR intervals, or junctional tachycardia)
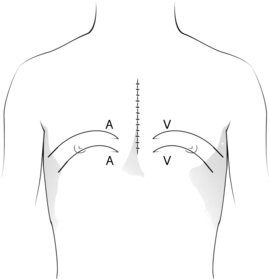
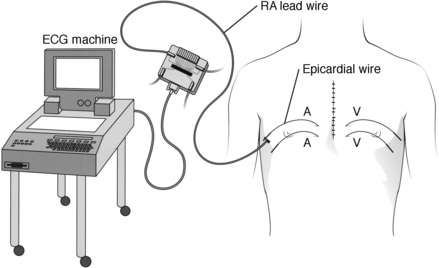
• AEGs can be performed with multichannel telemetry or a bedside ECG monitor that allows for simultaneous display of the AEG along with the surface ECG. A 12-lead ECG machine also can be used to obtain an AEG.
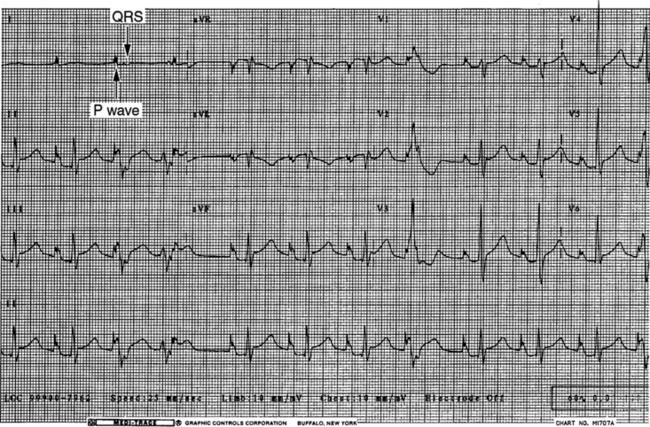
• AEG is a method of recording electrical activity that originates from the atria with use of temporary atrial epicardial wires placed during cardiac surgery. Standard ECG monitoring records electrical events from the heart with electrodes located on the surface of the patient’s body, which is a considerable distance from the myocardium. One limitation of ECG monitoring may be its inability to detect P waves effectively.
• AEGs detect electrical events directly from the atria, which provides a greatly enhanced tracing of atrial activity. This enhanced tracing allows for comparison of atrial events with ventricular events and determination of the relationship between the two.
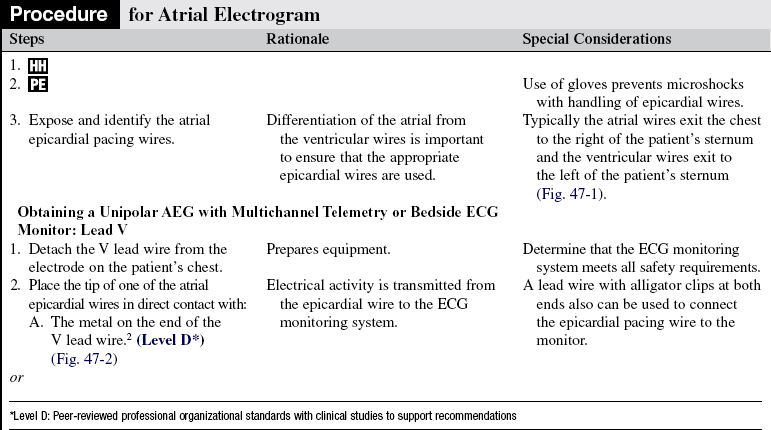
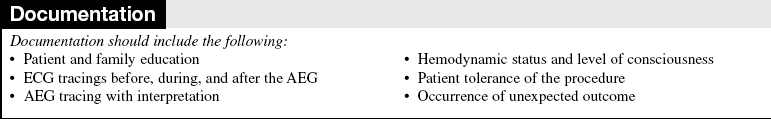
• Accurate identification of the epicardial atrial pacing wire or wires is important.
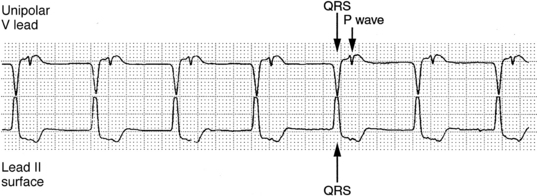
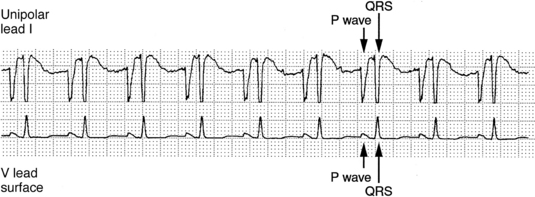
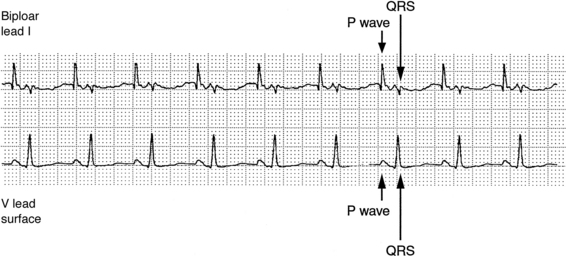
• The two types of AEGs that can be obtained from epicardial pacing wires are unipolar and bipolar.
 A unipolar electrogram measures electrical activity between one atrial epicardial wire and a surface ECG electrode. The unipolar AEG detects atrial and ventricular activity.
A unipolar electrogram measures electrical activity between one atrial epicardial wire and a surface ECG electrode. The unipolar AEG detects atrial and ventricular activity.
 A bipolar electrogram detects electrical activity between the two atrial epicardial wires. The bipolar AEG predominantly detects atrial activity because both electrodes are attached to the atria.
A bipolar electrogram detects electrical activity between the two atrial epicardial wires. The bipolar AEG predominantly detects atrial activity because both electrodes are attached to the atria.
EQUIPMENT
PATIENT AND FAMILY EDUCATION
• Provide information about the normal conduction system, normal and abnormal heart rhythms, and symptoms of abnormal heart rhythms.  Rationale: This information helps the patient and family to understand the patient’s condition and encourages the patient and family to ask questions.
Rationale: This information helps the patient and family to understand the patient’s condition and encourages the patient and family to ask questions.
• Provide information about the AEG and the reason for the AEG and explanation of the equipment.  Rationale: This communication decreases patient anxiety and helps the patient and family to understand the procedure, why it is needed, and how it will help the patient.
Rationale: This communication decreases patient anxiety and helps the patient and family to understand the procedure, why it is needed, and how it will help the patient.
• Explain the patient’s expected participation during the procedure.  Rationale: This explanation encourages patient assistance.
Rationale: This explanation encourages patient assistance.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess the patient’s cardiac rhythm for the presence of atrial activity in more than one lead from the multichannel ECG monitor or 12-lead ECG.  Rationale: This assessment determines the presence or absence of P waves and the potential need for an AEG.
Rationale: This assessment determines the presence or absence of P waves and the potential need for an AEG.
• Assess the patient’s cardiac rhythm for the relationship between atrial and ventricular activity.  Rationale: This assessment determines the relationship between P waves and QRS complexes and the potential need for an AEG.
Rationale: This assessment determines the relationship between P waves and QRS complexes and the potential need for an AEG.
• Assess for dysrhythmias.  Rationale: This assessment determines the patient’s baseline cardiac rhythm.
Rationale: This assessment determines the patient’s baseline cardiac rhythm.
• Assess the patient’s hemodynamic status (e.g., systolic, diastolic and mean arterial pressure, level of consciousness, dizziness, shortness of breath, nausea, vomiting, cool or clammy skin, and chest pain).  Rationale: Hemodynamic status and need for immediate intervention are determined.
Rationale: Hemodynamic status and need for immediate intervention are determined.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient understands pre-procedure teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: This communication evaluates and reinforces understanding of previously taught information.
Rationale: This communication evaluates and reinforces understanding of previously taught information.
• Expose the patient’s chest and identify the epicardial pacing wires.  Rationale: This action provides access to the atrial pacing wires.
Rationale: This action provides access to the atrial pacing wires.
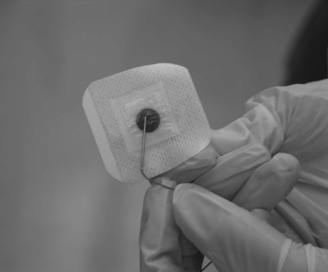
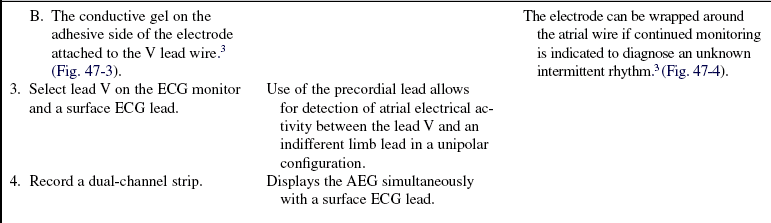
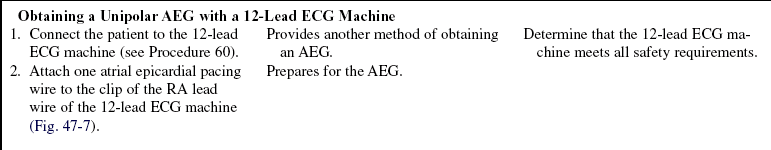
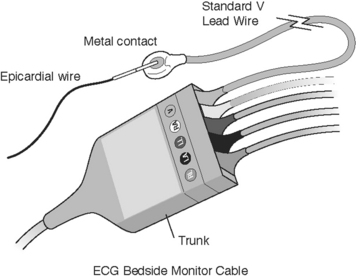
Figure 47-3 The tip of the atrial epicardial wire in direct contact with the conductive gel on the adhesive side of the electrode. (Kern LS , McRae ME, Funk M: ECG monitoring after cardiac surgery: post-opeative atrial fibrillation and the atrial electrogram, AACN Adv Crit Care 18[3]:298, 2007.)
References
1. Batra, AS, Balaji, S, Postoperative temporary epicardial pacing. when, how and why. Ann Ped Cardiol. 2008; 1(2):120–125.
![]() 2. Drew, BJ, et al, Practice standards for electrocardiographic monitoring in hospital settings. an American Heart Association Scientific Statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular -Disease in the Young. Circulation 2004; 110:2721–2746.
2. Drew, BJ, et al, Practice standards for electrocardiographic monitoring in hospital settings. an American Heart Association Scientific Statement from the Councils on Cardiovascular Nursing, Clinical Cardiology, and Cardiovascular -Disease in the Young. Circulation 2004; 110:2721–2746.
3. Kern, LS, McRae, ME, Funk, M, ECG monitoring after cardiac surgery. postopeative atrial fibrillation and the atrial electrogram. AACN Adv Crit Care 2007; 18:294–304.
4. Miller, JN, Drew, BJ, Atrial electrogrms after cardiac -surgery. survey of clinical practice. Am J Crit Care 2007; 16:350–359.
5. Overbay, D, Criddle, L. Mastering temporary invasive cardiac pacing. Crit Care Nurs. 2004; 24(3):25–32.
6. O’Grady, NP, et al. Guidelines for prevention of intravascular catheter-related infections. Am J Infect Control. 2002; 30:476–489.
![]() Waldo, AL, Henthorn, RW, Plumb, VJ, Temporary epicardial wire electrodes in the diagnosis and treatment of arrhythmias after open heart surgery. Am J Surg . 1984; 148:275–283.
Waldo, AL, Henthorn, RW, Plumb, VJ, Temporary epicardial wire electrodes in the diagnosis and treatment of arrhythmias after open heart surgery. Am J Surg . 1984; 148:275–283.
![]() Waldo, AL, et al, Use of temporarily placed epicardial atrial wire electrodes for the diagnosis and treatment of cardiac arrhythmias following open-heart surgery. J Thorac Cardiovasc Surg . 1978; 76:500–506.
Waldo, AL, et al, Use of temporarily placed epicardial atrial wire electrodes for the diagnosis and treatment of cardiac arrhythmias following open-heart surgery. J Thorac Cardiovasc Surg . 1978; 76:500–506.