Pericardiocentesis (Perform)
Pericardiocentesis (Perform)
PREREQUISITE NURSING KNOWLEDGE
• Advanced cardiac life support knowledge and skills are needed.
• Knowledge of sterile technique is required.
• Clinical and technical competence in the performance of pericardiocentesis is necessary.
• Knowledge of cardiovascular anatomy and physiology is needed.
• Pericardial effusion is the abnormal accumulation of greater than 50 mL of serosanguineous fluid within the pericardial sac.
• A pericardial effusion can be noncompressive or compressive. With a compressive effusion, increased pressure is found within the pericardial sac, which may result in cardiac tamponade and resistance to cardiac filling.
• The presentation of acute and chronic fluid accumulation varies. A rapid collection of fluid (over minutes to hours) may result in hemodynamic compromise with volumes of less than 250 mL. Chronically developing effusions (over days to weeks) allow for hypertrophy and distention of the fibrous parietal membrane.2 Patients with chronic effusions may accumulate greater than or equal to 2000 mL of fluid before exhibiting symptoms of hemodynamic compromise.1–4
• Symptoms of cardiac tamponade are not specific. Patients may have signs and symptoms of an associated disease. With a decrease in cardiac output, the patient often has development of tachycardia, tachypnea, pallor, cyanosis, impaired cerebral and renal function, diaphoresis, hypotension, neck vein distention, distant or faint heart sounds, and pulsus paradoxus.1–3
• The amount of fluid in the pericardium is evaluated through chest radiograph, two-dimensional echocardiogram, and clinical findings.
• When cardiac tamponade or a large enough effusion to warrant drainage is verified, a pericardiocentesis is performed to remove fluid from the pericardial sac. An acute tamponade resulting in hemodynamic instability necessitates an emergency procedure. Blind pericardiocentesis should be performed only in extreme emergency situations.4
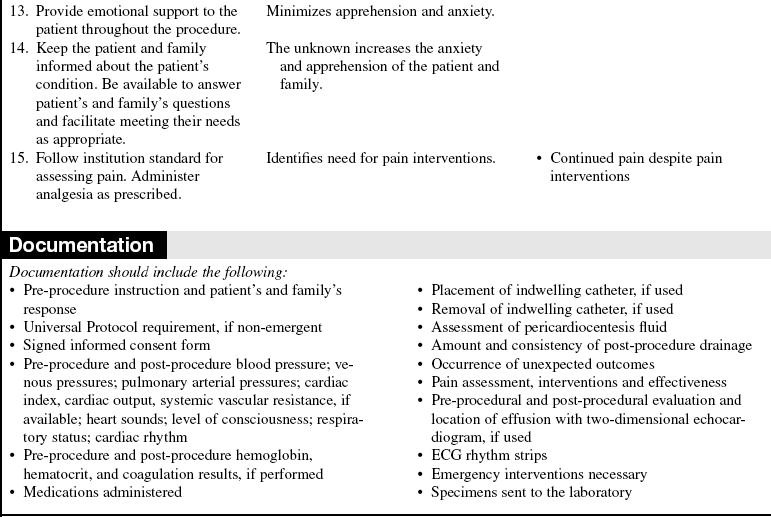
• Pericardiocentesis commonly is performed via a subxiphoid approach.
• Two-dimensional echocardiography is recommended to assist in guiding the needle during the pericardiocentesis.8
• This procedure may be performed in the cardiac catheterization laboratory with fluoroscopy.
• Inability to obtain pericardial drainage, reaccumulation of pericardial fluid, or cardiac injury may progress into cardiac tamponade, which necessitates urgent or emergent chest exploration.
EQUIPMENT
• Pericardiocentesis tray (or thoracentesis tray)
• 16-gauge or 18-gauge, 3-inch cardiac needle or catheter over the needle
• Antiseptic solution (e.g., 2% chlorhexidine-based preparation)
• Two packs of 4 × 4 gauze sponges
• No. 11 knife blade with handle (scalpel)
• Sterile 50-mL to 60-mL, 10-mL, 5-mL, and 3-mL syringes
• Masks, goggles or face shields, surgical head covers, sterile gowns, and gloves
PATIENT AND FAMILY EDUCATION
• Instruct the patient and family regarding the reason the pericardiocentesis is needed; describe the procedure; and explain expected outcomes, alternatives, and possible complications.  Rationale: This communication helps the patient and family to understand the procedure. Information about the procedure reduces anxiety and apprehension.
Rationale: This communication helps the patient and family to understand the procedure. Information about the procedure reduces anxiety and apprehension.
• Instruct the patient and family about potential signs and symptoms of recurrent pericardial effusion (e.g., dyspnea, dull ache or pressure within the chest, dysphagia, cough, tachypnea, hoarseness, hiccups, or nausea).2,3  Rationale: Early detection of pericardial effusion may prevent complications from cardiac compression.
Rationale: Early detection of pericardial effusion may prevent complications from cardiac compression.
• Instruct the patient and family about the patient’s risk for recurrent pericardial effusion.  Rationale: Prediction of pericardial effusion may allow early detection of a potentially life-threatening problem.
Rationale: Prediction of pericardial effusion may allow early detection of a potentially life-threatening problem.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Determine the history of the present illness and mechanism of injury (if applicable), medical history, and current medical therapies.  Rationale: The history is needed to determine the patient’s present health, to identify potential risk factors, and to provide an opportunity for the nurse to establish a relationship with the patient.
Rationale: The history is needed to determine the patient’s present health, to identify potential risk factors, and to provide an opportunity for the nurse to establish a relationship with the patient.
• Assess the patient’s heart rate, cardiac rhythm, heart sounds (S1, S2, rubs), venous pressure (noninvasive or invasive), blood pressure, pulse pressure, oxygen saturation via pulse oximetry (SpO2), respiratory status, and neurologic status.  Rationale: These data are needed to compare baseline data to assess for changes during or after the procedure.
Rationale: These data are needed to compare baseline data to assess for changes during or after the procedure.
• Assess current laboratory values, including the complete blood cell count, electrolytes, and coagulation profile.  Rationale: These data are needed to identify the potential for cardiac dysrhythmias or abnormal bleeding. If the international normalized ratio or partial thromboplastin time or both are elevated, consider reversing the level of anticoagulation therapy before performing the procedure or defer the procedure until the levels indicate a reduced possibility of bleeding.
Rationale: These data are needed to identify the potential for cardiac dysrhythmias or abnormal bleeding. If the international normalized ratio or partial thromboplastin time or both are elevated, consider reversing the level of anticoagulation therapy before performing the procedure or defer the procedure until the levels indicate a reduced possibility of bleeding.
Patient Preparation
• Ensure that the patient and family understand pre-procedural teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: This communication evaluates and reinforces understanding of previously taught information.
Rationale: This communication evaluates and reinforces understanding of previously taught information.
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Obtain informed consent (may not be possible if the procedure is an emergency).  Rationale: Informed consent protects the rights of the patient and ensures a competent decision for the patient and the family.
Rationale: Informed consent protects the rights of the patient and ensures a competent decision for the patient and the family.
• Perform a pre-procedure verification and time out, if non-emergent.  Rationale: Ensures patient safety.
Rationale: Ensures patient safety.
• Coordinate the procedure with the echocardiogram technician to assist with the two-dimensional echocardiogram if this approach is being taken.  Rationale: Echocardiogram-directed pericardiocentesis allows for more precise localization of the effusion and may help to prevent complications.1,2,7
Rationale: Echocardiogram-directed pericardiocentesis allows for more precise localization of the effusion and may help to prevent complications.1,2,7
• If tolerated, position the patient comfortably in the supine position with the head of the bed elevated 30 to 60 degrees.  Rationale: This position facilitates the aspiration of pericardial fluids and the ease of breathing.
Rationale: This position facilitates the aspiration of pericardial fluids and the ease of breathing.
• Prescribe and ensure that an analgesic or sedative is administered.  Rationale: Analgesia and sedation reduce anxiety and promote comfort.
Rationale: Analgesia and sedation reduce anxiety and promote comfort.
• Apply the limb leads and connect the leads to the cardiac bedside monitoring system or to the 12-lead ECG machine.  Rationale: The ECG is analyzed during and after the procedure to monitor the patient for changes that may indicate cardiac injury.
Rationale: The ECG is analyzed during and after the procedure to monitor the patient for changes that may indicate cardiac injury.
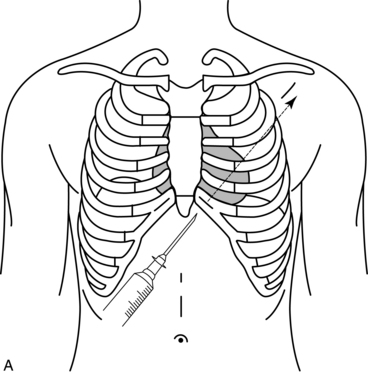
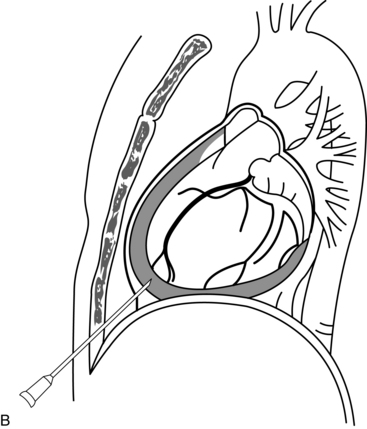
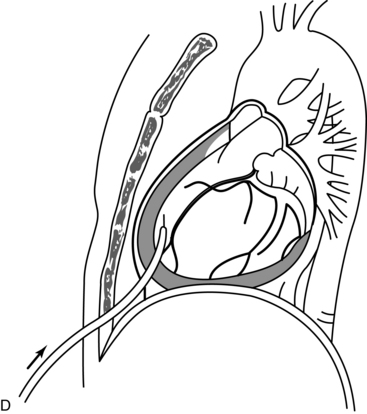
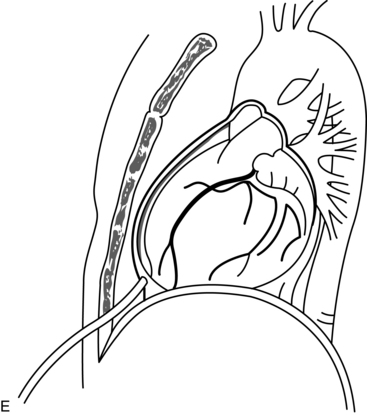
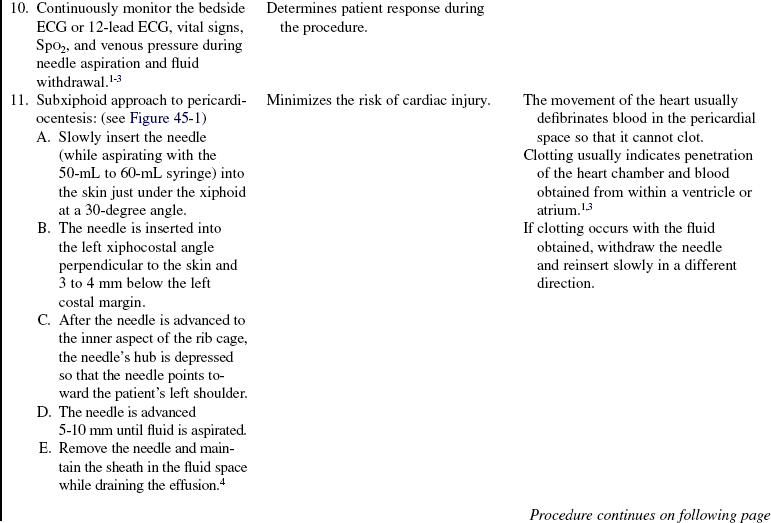
Figure 45-1 Subxiphoid approach to catheter placement into pericordial space. A, A short needle (16-gauge or 18-gauge) is inserted into the left xiphocostal angle perpendicular to the skin and 3 to 4 mm below the left costal margin. B, After the needle is advanced to the inner aspect of the rib cage, the needle’s hub is depressed so that the needle points toward the patient’s left shoulder. The needle is then cautiously advanced about 5 to 10 mm until fluid is reached. The fingers may sense a distinct “give” when the needle penetrates the parietal pericardium. Successful removal of fluid confirms the needle’s position. C, The syringe is then disconnected from the needle, and the flexible tip of the guidewire is advanced into the pericardial space. The needle is withdrawn and replaced with a soft multihole pigtail catheter (no. 6F to 8F) with use of the Seldinger technique. D, After dilation of the needle tract, the catheter is advanced over the guidewire into the pericardial space. E, Once the catheter is properly positioned, aspiration of fluid should result in rapid improvement in blood pressure and cardiac output, a decrease in atrial and pericardial pressures, and a decrease in the degree of any paradoxical pulse. Electrical alternans, if present, also decreases or disappears. (From Spodick DH: The technique of pericardiocentesis, J Crit Ill 2:91, 1987.)
References
1. Becker, RC. Pericardiocentesis. In Irwin RS, et al, eds. : Procedures and techniques in intensive care medicine,, ed 6, Philadelphia: Lippincott Williams & Wilkins, 2008.
![]() 2. Belenkie, I. Pericardial disease. In Hall JB, et al, eds. : Principles of critical care, ed 3, Quebec, 2005.
2. Belenkie, I. Pericardial disease. In Hall JB, et al, eds. : Principles of critical care, ed 3, Quebec, 2005.
![]() 3. Harper, RJ. Pericardiocentesis. In Roberts JR, et al, eds. : Clinical procedures in emergency medicine,, ed 4, Philadelphia: Elsevier, 2004.
3. Harper, RJ. Pericardiocentesis. In Roberts JR, et al, eds. : Clinical procedures in emergency medicine,, ed 4, Philadelphia: Elsevier, 2004.
![]() 4. Hoit, BD. Circulation. Management of effusive and constrictive pericardial heart disease. 2002; 105:2939–2942.
4. Hoit, BD. Circulation. Management of effusive and constrictive pericardial heart disease. 2002; 105:2939–2942.
5. LeWinter, MM, Pericardial diseasesLibby P, et al, eds.. Braunwald’s heart disease. a textbook of cardiovascular medicine. ed 8. Saunders, Philadelphia, 2008.
![]() 6. O’Grady, NP, et al. Guidelines for the prevention of -intravascular catheter-related infections. Am J Infect -Control. 2002; 30(8):476–489.
6. O’Grady, NP, et al. Guidelines for the prevention of -intravascular catheter-related infections. Am J Infect -Control. 2002; 30(8):476–489.
![]() 7. Rifkin, RD, Mernoff, DB. Noninvasive evaluation of -pericardial effusion composition by computed -tomography. Am Heart J. 2005; 149:1120–1127.
7. Rifkin, RD, Mernoff, DB. Noninvasive evaluation of -pericardial effusion composition by computed -tomography. Am Heart J. 2005; 149:1120–1127.
![]() 8. Tsang, TS, et al, Echocardiographically guided pericardiocentesis. evolution and state-of-the-art technique. Mayo Clin Proc 1998; 73:647–652.
8. Tsang, TS, et al, Echocardiographically guided pericardiocentesis. evolution and state-of-the-art technique. Mayo Clin Proc 1998; 73:647–652.
Kuhn, B, Peters, J, Marx, GR, et al. Etiology, management and outcome of pediatric pericardial effusions. Pediatr Cardiol. 2008; 29:90–94.
![]() Mavroukakis, S, Stine, A. Nursing management of adults with disorders of the coronary arteries, myocardium,or pericardium. In: Beare PG, Myers JL, eds. Adult health nursing. St Louis: Mosby, 1998.
Mavroukakis, S, Stine, A. Nursing management of adults with disorders of the coronary arteries, myocardium,or pericardium. In: Beare PG, Myers JL, eds. Adult health nursing. St Louis: Mosby, 1998.