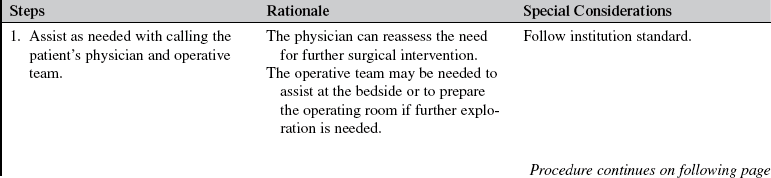
Emergent Open Sternotomy (Assist)
PREREQUISITE NURSING KNOWLEDGE
• Knowledge of the anatomy and physiology of the cardiovascular system is necessary.
• Advanced cardiac life support knowledge and skills are needed.
• Understanding of signs and symptoms of cardiac tamponade is necessary.
• Emergency open sternotomy is performed for patients who have undergone a median sternotomy, usually within the first 2 weeks of cardiac surgery.
• Emergent open sternotomy is indicated for exsanguinating hemorrhage or cardiac tamponade with imminent cardiac arrest.5,6
 The goal of mediastinal exploration for persistent hemorrhage is to stop the bleeding and retain circulating blood volume. The requirement for homologous blood transfusion and incidence of wound infection associated with an undrained mediastinal hematoma3 may be decreased.
The goal of mediastinal exploration for persistent hemorrhage is to stop the bleeding and retain circulating blood volume. The requirement for homologous blood transfusion and incidence of wound infection associated with an undrained mediastinal hematoma3 may be decreased.
 The goal of mediastinal exploration for cardiac tamponade is to relieve the pressure on the ventricles during diastole. The decreased pressure allows the ventricles to fill during diastole, which should increase contractility, stroke volume, and cardiac output to improve systemic perfusion.
The goal of mediastinal exploration for cardiac tamponade is to relieve the pressure on the ventricles during diastole. The decreased pressure allows the ventricles to fill during diastole, which should increase contractility, stroke volume, and cardiac output to improve systemic perfusion.
• Knowledge and skills related to aseptic and sterile technique are needed.
• Internal defibrillation may be necessary if life-threatening dysrhythmias occur (see Procedure 42).
EQUIPMENT
• Antiseptic solution (e.g., 2% chlorhexidine-based preparation)
• Head cover, masks, eye protection, sterile gown, sterile gloves, sterile drapes
• Sterile open-chest set and sternotomy tray
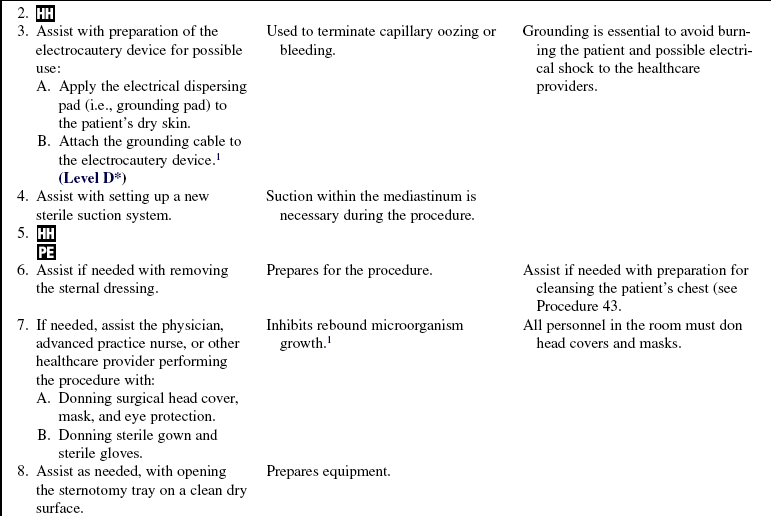
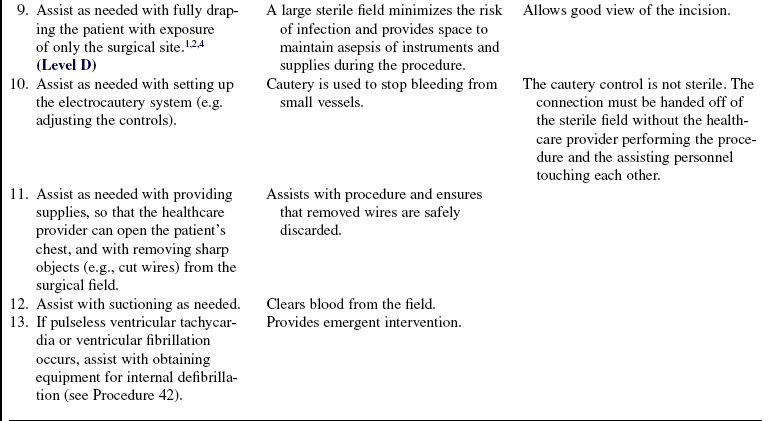
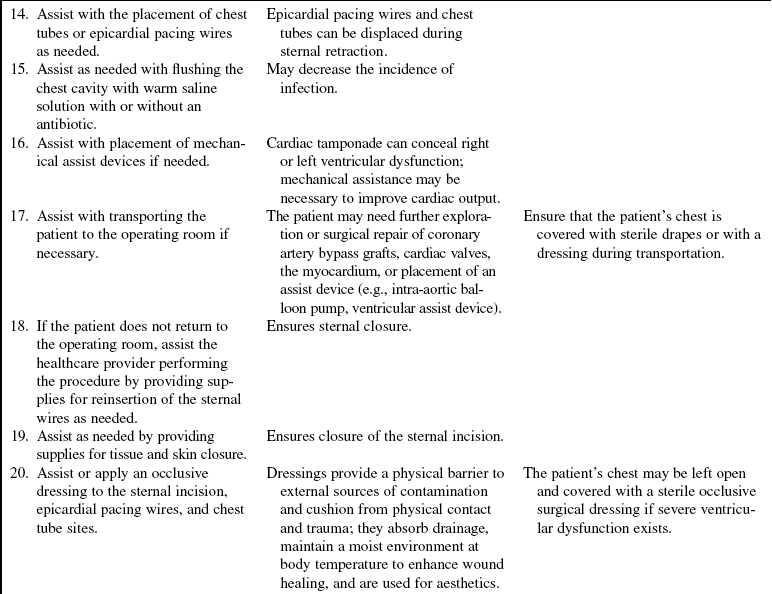
• Electrocautery equipment: Generator, cautery, electrical dispersing pad (e.g., grounding pad)
• Large sterile suction catheter (e.g., Yankauer)
• Suction containers, tubing, regulator, and suction source
• Radiopaque gauze or other surgical sponge materials
• Polypropylene (Prolene) suture (cutting needle), other suture material according to preference
• Syringes: 3 ml, 5 ml, 10 ml, and 20 ml
Additional equipment as needed includes the following:
• Prescribed analgesia and sedation
• Blood products and intravenous solutions as prescribed
• Defibrillator and compatible internal defibrillation paddles
• Warm saline solution with or without an antibiotic, as prescribed
• Chest tubes and chest tube drainage system
• Intra-aortic balloon pump or other mechanical assist device
• Peripheral nerve stimulator (used if paralytic agents are administered)
PATIENT AND FAMILY EDUCATION
• Teaching may not be provided until after the procedure.  Rationale: Internal defibrillation usually is performed in the face of sudden hemodynamic collapse.
Rationale: Internal defibrillation usually is performed in the face of sudden hemodynamic collapse.
• Explain the reason that the open sternotomy procedure was performed and its outcome or anticipated outcome.  Rationale: This explanation provides information and encourages the patient and family to ask questions and clarify details about the patient and procedure.
Rationale: This explanation provides information and encourages the patient and family to ask questions and clarify details about the patient and procedure.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess hemodynamic and neurologic status.  Rationale: This assessment identifies baseline data that may indicate the need for emergent open sternotomy and provides comparison data.
Rationale: This assessment identifies baseline data that may indicate the need for emergent open sternotomy and provides comparison data.
• Assess the patient’s medical history, specifically for coagulation disorders, renal disease with coexistent uremia, and functional status of the right and left ventricles.  Rationale: Baseline data are obtained.
Rationale: Baseline data are obtained.
• Assess current laboratory data, specifically complete blood cell count, platelet count, international normalized ratio, activated partial thromboplastin time, and fibrinogen.  Rationale: Near-normal baseline coagulation study results decrease the likelihood of coagulopathy as a possible cause for ongoing hemorrhage.
Rationale: Near-normal baseline coagulation study results decrease the likelihood of coagulopathy as a possible cause for ongoing hemorrhage.
• Assess for signs and symptoms of cardiac tamponade:
 Sudden decrease or cessation in chest tube drainage
Sudden decrease or cessation in chest tube drainage
 Hypotension (mean arterial blood pressure, <60 mm Hg)
Hypotension (mean arterial blood pressure, <60 mm Hg)
 Apical heart rate greater than 110 beats/min
Apical heart rate greater than 110 beats/min
 Equilibrium of intracardiac pressures, with right atrial, pulmonary artery diastolic, pulmonary artery occlusion, and (if measured) left atrial pressures
Equilibrium of intracardiac pressures, with right atrial, pulmonary artery diastolic, pulmonary artery occlusion, and (if measured) left atrial pressures
 Rationale: The presence of some or all of these signs and symptoms assists the healthcare team to decide whether an emergent open sternotomy is necessary.
Rationale: The presence of some or all of these signs and symptoms assists the healthcare team to decide whether an emergent open sternotomy is necessary.
• Assess for excessive chest tube drainage.  Rationale: Presence of bleeding assists with the determination of the need for mediastinal exploration. Follow institution guidelines regarding determination of the timing of mediastinal exploration. One recommendation is when chest tube drainage continues at equal to or greater than 3 mL/kg/hr for at least 3 hours.2
Rationale: Presence of bleeding assists with the determination of the need for mediastinal exploration. Follow institution guidelines regarding determination of the timing of mediastinal exploration. One recommendation is when chest tube drainage continues at equal to or greater than 3 mL/kg/hr for at least 3 hours.2
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand procedural teachings (if time available). Answer questions as they arise, and reinforce information as needed.  Rationale: Understanding of the information provided is evaluated and reinforced.
Rationale: Understanding of the information provided is evaluated and reinforced.
• Ensure that informed consent was obtained (may not be possible if the procedure is an emergency).  Rationale: Informed consent protects the rights of the patient and ensures a competent decision for the patient and the family.
Rationale: Informed consent protects the rights of the patient and ensures a competent decision for the patient and the family.
• Perform a pre-procedure verification and time out, if non-emergent.  Rationale: Ensures patient safety.
Rationale: Ensures patient safety.
• Ensure the patient’s airway is protected and that supplemental oxygen is delivered.  Rationale: Ensures adequate ventilation and oxygenation.
Rationale: Ensures adequate ventilation and oxygenation.
• Position the patient in the supine position with the head of the bed flat.  Rationale: This position ensures visualization of the chest and enhances hemodynamic stability.
Rationale: This position ensures visualization of the chest and enhances hemodynamic stability.
• Provide analgesics and/or sedatives as prescribed.  Rationale: Promotes patient comfort.
Rationale: Promotes patient comfort.
References
1. AORN, Association of periOperative Registered Nurses. Perioperative standards and recommended practices. AORN, Denver, 2008.
2. Chikwe, J, Beddow, E, Glenville, B. Cardiothoracic surgery. New York: Oxford University Press Inc; 2006.
![]() 3. Mason, RJ, Broaddus, VC, Murray, JF, et al. Murray & Nadel’s textbook of respiratory medicine, ed 4. St Louis: Saunders; 2005.
3. Mason, RJ, Broaddus, VC, Murray, JF, et al. Murray & Nadel’s textbook of respiratory medicine, ed 4. St Louis: Saunders; 2005.
4. Phillips, N. Berry & Kohn’s operating room technique, ed 11. St Louis: Mosby; 2007.
5. Sethares, K, Seifert, PC, Smith, H. Care of patients undergoing cardiac surgery. In: Moser DK, Riegel B, eds. Cardiac nursing: a companion to Braunwald’s heart -disease. St Louis: Saunders, 2008.
![]() 6. Soar, J, et al, European Resuscitation Council guidelines for resuscitation 2005 section 7. cardiac arrest in special -circumstances. Resuscitation. 2005; 67(Suppl 1):S135–S170.
6. Soar, J, et al, European Resuscitation Council guidelines for resuscitation 2005 section 7. cardiac arrest in special -circumstances. Resuscitation. 2005; 67(Suppl 1):S135–S170.
![]() Boyce, JM, Pittet, D. Guidelines for hand hygiene in health-care settings. MMWR. 2002; 51(RR16):1–44.
Boyce, JM, Pittet, D. Guidelines for hand hygiene in health-care settings. MMWR. 2002; 51(RR16):1–44.
Christie, SL, Sawatzky, JV, Acute cardiac tamponade. anticipate the complication. CACCN 2008; 19:13–17.
![]() Currey, J, Botti, M. The haemodynamic status of cardiac surgical patients in the initial 2-h recovery period. Eur J Cardiovasc Nurs. 2005; 4:207–214.
Currey, J, Botti, M. The haemodynamic status of cardiac surgical patients in the initial 2-h recovery period. Eur J Cardiovasc Nurs. 2005; 4:207–214.
Finkelmeier, BA. Cardiothoracic surgical nursing, ed 2. Philadelphia: Lippincott; 2000.
![]() Rothrock, JC. Alexander’s care of the patient in surgery, 13. St Louis: Mosby; 2007.
Rothrock, JC. Alexander’s care of the patient in surgery, 13. St Louis: Mosby; 2007.