CHAPTER 43. Otorhinolaryngological Care
Donna R. Mcewen
OBJECTIVES
At the conclusion of this chapter, the reader will be able to:
1. Identify the pathophysiological ear, nose, throat, and head and neck conditions requiring surgical interventions.
2. Describe surgical procedures with the preanesthesia, perianesthesia, and postanesthesia problems encountered in the ear, nose, throat, and head and neck patient and the nursing interventions required in the management of these problems.
3. Identify possible complications that can arise after ear, nose, throat, and head and neck procedures.
I. ANATOMY AND PHYSIOLOGY
A. Ear
1. Structure and function
a. Anatomy of ear (organ of hearing and equilibrium; Figure 43-1)
(1) Outer ear
(a) Visible portion consists of skin-covered flap of cartilage known as auricle or pinna.
(i) Collects sound waves
(ii) Directs sound waves to external acoustic meatus
(b) Auditory canal—external acoustic meatus
(i) Extends to tympanic membrane (eardrum)
(c) Tympanic membrane
(i) Thin, transparent, pearly gray, cone-shaped membrane
(ii) Stretches across the ear canal
(iii) Separates the middle ear (tympanic cavity) from the outer ear
(d) Nerve supply
(i) Auriculotemporal branch of the trigeminal nerve
[a] General sensory
[b] Innervates tympanic membrane, external acoustic meatus, anterior auricle
(2) Middle ear
(a) Structure
(i) Ossicles
[a] Malleus (hammer)
[1] Largest of the three ossicles
[b] Incus (anvil)
[1] Middle ossicle
[c] Stapes (stirrup)
[1] Innermost ossicle
(ii) Eustachian tube
[a] Channel connecting the tympanic cavity and the nasal part of the pharynx through which air reaches the middle ear
(b) Function
(i) Ossicles form a chain from tympanic membrane to the oval window.
(ii) Transmits vibrations to inner ear, conducting sound to the inner ear
(3) Inner ear
(a) Cochlea—spiral-shaped, forms the anterior part of the labyrinth of the inner ear; contains three compartments
(i) Scala vestibuli
[a] Part of the cochlea above the spiral lamina, which divides the canal
(ii) Scala tympani
[a] Part of the cochlea below the spiral lamina
(iii) Cochlear duct (scala media)
[a] Canal between the scala tympani and scala vestibuli
(b) Organ of Corti
(i) Organ lying against the basilar membrane in the cochlear duct
(ii) Contains special sensory receptors for hearing
(iii) Consists of neuroepithelial hair cells that respond to vibration from the ossicles, converting mechanical energy to electrochemical impulses
(c) Vestibular labyrinth—controls equilibrium
(i) Utricle
[a] Larger of the two divisions of the membranous labyrinth of the inner ear
(ii) Saccule
[a] Smaller of the two divisions of the membranous labyrinth of the vestibule
[b] Communicates with the cochlear duct by way of the ductus reuniens
(iii) Semicircular canals
[a] Description: three canals—anterior, lateral, and posterior
[b] Passages in the inner ear
[c] Located in the bony labyrinth
[d] Functions: control sense of balance
[e] Respond to movement of head
[f] Can cause feeling of dizziness or vertigo after spinning
[g] Motion sickness results from unusual movements of the head that result in stimulation of the semicircular canals.
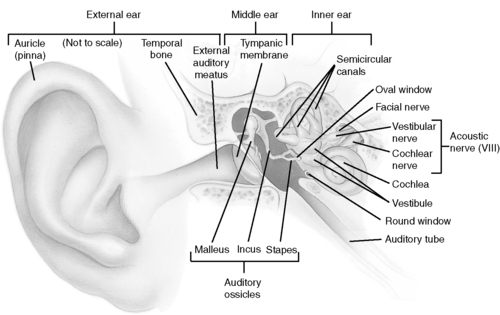 |
| FIGURE 43-1 ▪
The ear.
(From Thibodeau GA, Patton KT: Anatomy and physiology, ed 7, St Louis, 2010, Mosby.)
|
B. Nose
1. Structure and function
a. Anatomy of nose (organ of respiration and olfaction; Figure 43-2)
(1) External
(a) Upper—formed by nasal bones and maxilla
(b) Lower—formed by connective tissue
(c) Nares—separated by columella, formed from nasal cartilage
(d) Nasal septum
(i) Nasal cartilage
(ii) Vomer bone
(iii) Perpendicular plate of ethmoid bone
(2) Internal—nasal cavity
(a) Nares (nostrils)
(i) External opening of the nasal cavity
(b) Choanae
(i) Paired openings between nasal cavity and oropharynx
(c) Nasopharynx
(i) Part of the pharynx above the soft palate
(d) Eustachian tube
(i) Narrow channel that connects tympanum with nasopharynx
(e) Paranasal sinuses
(i) Arranged in four pairs
[a] Maxillary
[b] Frontal
[c] Sphenoid
[d] Ethmoid
(f) Nasal duct
(i) Extends from the lower part of the lacrimal sac to the inferior meatus of the nose
(ii) Channel through which tear fluid is conveyed into the cavity of the nose
(g) Turbinate bones
(i) Extend horizontally along the lateral wall of the nasal cavity
(ii) Separate the middle meatus of the nasal cavity from the inferior meatus
(h) Nasal septum
(i) Separates the nasal cavity into two fossae
(i) Nerve supply
(i) Trigeminal nerve
[a] Cranial nerve V
[b] General sensory, motor
[c] Face, teeth, mouth, nasal cavity
(ii) Cranial nerve I (olfactory)
[a] Special sensory
[b] Nerve of smell
(j) Other nerves to consider
(i) Cranial nerve II (optic)
[a] Special sensory
[b] Nerve of sight
[c] Can be damaged in endoscopic sinus surgery
(k) Arterial blood supply
(i) Internal maxillary
(ii) Anterior ethmoid
(iii) Sphenopalatine
(iv) Nasopalatine
(v) Pharyngeal
(vi) Posterior ethmoid
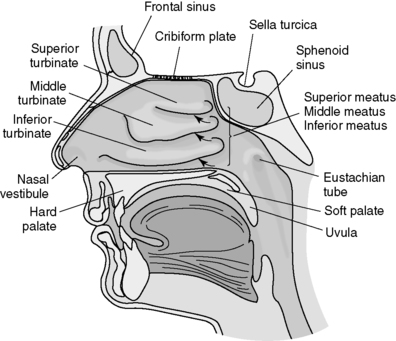 |
| FIGURE 43-2 ▪
Lateral wall of nose, showing superior, middle, and inferior turbinates.
(From Monahan FD, Sands JK, Neighbors M, et al: Phipps medical-surgical nursing, ed 8, St Louis, 2007, Mosby.)
|
C. Throat
1. Structure and function
a. Anatomy of oral cavity
(1) Mouth
(a) Lips
(b) Buccal cavity
(c) Lingual cavity
(i) Tongue
(ii) Hard palate
(iii) Soft palate
(2) Pharynx (Figure 43-3)
(a) Throat
(i) Nasopharynx
[a] Lies posterior to the nose and above the level of the soft palate
[b] Provides passageway for air
[c] Contains opening of the eustachian tubes
(ii) Oropharynx
[a] Extends from soft palate to the hyoid bone
[b] Provides passageway for both air and food
(iii) Laryngopharynx
[a] Extends from the hyoid bone to the lower border of the cricoid cartilage
[b] Continues with the esophagus
[c] Anterior entrance of the larynx is the epiglottis.
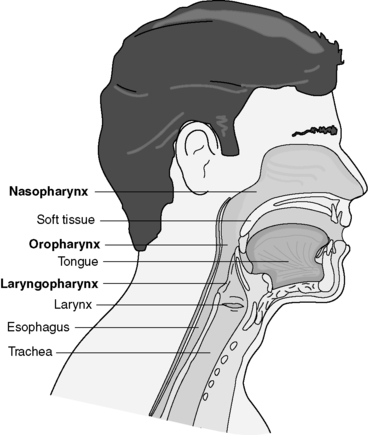 |
| FIGURE 43-3 ▪
Sagittal section of head showing pharynx and larynx.
(From Monahan FD, Sands JK, Neighbors M, et al: Phipps medical-surgical nursing, ed 8, St Louis, 2007, Mosby.)
|
(3) Tonsils
(a) Types
(i) Palatine tonsils
[a] Pair of oval-shaped structures
[b] Size of almonds
[c] Partially imbedded in mucous membrane
[d] One on each side of the throat
(ii) Lingual tonsils
[a] Below palatine tonsils
[b] At base of tongue
(iii) Pharyngeal tonsils (adenoids)
[a] Located in upper rear wall of oral cavity
[b] Fair size in childhood, shrink after puberty
(b) Functions
(i) Part of the lymphatic system
(ii) Assist in filtering the circulating lymph of bacteria and other foreign material that may enter body through mouth or nose
(c) Nerve supply
(i) Middle and posterior branches of the maxillary and glossopharyngeal nerves
(ii) Cranial nerve X (vagus)
[a] Parasympathetic, visceral, afferent, motor, general sensory
[b] Supplies sensory fibers to ear, tongue, pharynx, and larynx
[c] Supplies motor fibers to pharynx, larynx, and esophagus
(d) Blood supply
(i) External carotid branch (ascending palatine branch of facial artery)
(4) Larynx
(a) Thyroid cartilage
(i) Shield-shaped cartilage
(ii) Produces prominence on neck (“Adam’s apple”)
(b) Hyoid bone
(i) Horse-shaped bone
(ii) Situated at the base of the tongue, just below the thyroid cartilage
(c) Cricoid cartilage
(i) Ringlike cartilage
(ii) Forms lower and back part of larynx
(d) Epiglottis
(i) Lidlike cartilage structure
(ii) Hangs over the entrance to the larynx
(e) Arytenoid cartilages
(i) Jug-shaped cartilage of the larynx
(f) Corniculate cartilages
(i) Two small conical nodules of yellow elastic cartilage
(ii) Articulate with the arytenoid cartilages
(g) Cuneiform cartilage
(i) Elongated yellow elastic cartilage in the aryepiglottic fold
(h) Glottis
(i) Vocal apparatus of the larynx
(ii) Consists of true vocal cords (vocal folds) and opening between them
(i) Nerve supply
(i) Superior laryngeal nerve
[a] Motor, general sensory, visceral afferent, parasympathetic
[b] Cricothyroid muscle and inferior constrictor muscles of the pharynx, mucous membrane of back of tongue and larynx
(ii) Recurrent laryngeal nerve
[a] Parasympathetic, visceral afferent, motor
[b] Tracheal mucosa, esophagus, cardiac plexus
(5) Thyroid gland
(a) Located in anterior portion of the neck
(b) Consists of right and left lobes united by isthmus
(c) Vascular supply: superior and inferior thyroid arteries
(d) Nerves in proximity
(i) Recurrent laryngeal nerve
(ii) Superior laryngeal nerve
II. GENERAL NURSING CONCERNS
A. Preoperative concerns (see Chapter 15)
1. Medical history assessment
2. Nursing assessment
a. Chief complaint
b. Medications
(1) Allergies
(2) Current medications patient is taking, including over-the-counter and herbal medications
(3) Use of aspirin, nonsteroidal anti-inflammatory medications, or medications containing aspirin (increased risk of bleeding)
(4) Hormone therapy
(5) Preoperative medications
c. Patient’s understanding of surgical procedure and expected outcomes
d. Patient’s psychosocial status
e. Preexisting sensory deficits
3. Usual laboratory and radiological evaluations
a. Complete blood cell count
b. Electrolytes based on patient history
c. Urinalysis
d. Coagulation studies
e. Availability of designated blood products, type and crossmatch
f. Electrocardiogram
g. Chest radiograph
h. Radiograph of sinuses, neck, mastoid
i. Computed tomography
j. Magnetic resonance imaging
k. Pregnancy test for menstruating females
4. Preoperative instructions
a. Surgical procedure
b. Operative site verification
c. Expected outcomes
d. Environment
e. Alterations in lifestyle
f. Self-care
g. Suctioning
h. Deep breathing
i. Pain management
B. Intraoperative concerns
1. Nursing assessment
a. Assess respiratory status.
b. Determine patient’s comfort.
c. Identify positioning needs.
d. Establish priorities.
e. Reinforce preoperative teaching.
(1) Orient to perioperative environment.
(2) Instruct patient in postoperative dressings.
f. Determine patient’s anxiety or apprehension.
g. Operative site verification
2. Aseptic technique
3. Skin and tissue integrity
4. Correct counts
5. Medications given
6. Intake and output
7. Blood loss
8. Patient’s condition at time of transfer to post anesthesia care unit (PACU)
C. Postanesthesia concerns: phase I
1. Nursing assessment
a. Respiratory status
b. Cardiovascular status
c. Neurological status
d. Psychosocial status
2. Report from anesthesiologist or certified registered nurse anesthetist and/or operating room nurse
a. Procedure, extent of surgery; complications
b. Anesthetic agents and medications administered
c. Blood loss and fluid replacement
d. Placement of drains, packing
e. Pertinent history, allergies
3. Pain status
4. Intake and output
5. Patient’s position
6. Presence or absence of nausea
7. Patient’s ability to communicate
8. Integrity of dressings and incision
9. Patient’s temperature
10. Drainage from surgical site
D. Postanesthesia concerns: discharge from phase I
1. Patient
a. Conscious and able to maintain airway
b. Able to maintain oxygen saturation greater than 92% after 15 minutes breathing room air without being stimulated
c. Remains in this condition for 30 to 45 minutes after:
(1) Extubation
(2) Administration of narcotic or narcotic antagonist
2. No active bleeding from operative site or drains
E. Postanesthesia concerns: phase II
1. Prepare for discharge (criteria and policies vary among facilities).
a. Ensure adequate pain control.
b. Validate ability to retain fluids and maintain hydration status.
c. Validate patient’s ability to urinate or return to previous level of urinary status.
d. Assist patient with changing from hospital gown to personal clothing if necessary.
e. Provide discharge instructions to patient and caregiver.
f. Ensure that the patient is accompanied by responsible adult at discharge.
F. Pediatric otolaryngology patients
1. Special considerations
a. Preoperative concerns (see Chapter 11)
(1) Fear of separation, pain, injury, death: establish trust, reassure patient.
(2) Child’s feelings of “loss of control”: allow child to choose flavoring for anesthetic induction mask.
(3) Anxiety and fear of child and parents: prepare child and parents.
b. Intraoperative concerns
(1) Airway management: increased risk of laryngospasm and vomiting if anesthesia is induced while crying
(2) Maintenance of body temperature (pediatric patient loses temperature faster than adult): keep patient covered with warm blankets, insulated drapes, convection or forced air warming blanket to prevent loss of body heat.
c. Postoperative concerns
(1) Maintenance of body temperature: use of warm blankets, insulated drapes, keep patient covered to prevent further heat loss and restore body temperature.
(2) Increased risk for bleeding related to postoperative crying: administer pain medication as needed, provide reassurance to child and parents, allow family visitation postoperatively.
(3) Fluid balance (pediatric patient dehydrates easier than adult): encourage fluid intake postoperatively, monitor intravenous (IV) fluids and output.
III. SURGICAL PROCEDURES
A. Ear
1. Myringotomy with or without tympanostomy tubes
a. Purpose
(1) Relieves pressure and allows for drainage of purulent or serous secretions from middle ear
(2) Aerates middle ear
(3) Relieves eustachian tube obstruction (thick, mucoid fluid)
(4) May be short-term or long-term
b. Description
(1) Small incision made into posteroinferior aspect of tympanic membrane
(2) Polyethylene tube can be inserted into eardrum.
c. Indications
(1) Acute otitis media unresponsive to antibiotics
(2) Bulging tympanic membrane
(3) Multiple episodes of acute otitis media along with chronic otitis media
d. Preoperative concerns
(1) Frequently performed on children
(a) Preoperative medication provided in oral form
(b) Usually performed under mask anesthesia; no IV access established
e. Intraoperative concerns
(1) General anesthetic essential for children to ensure accurate incision of tympanic membrane and placement of tube
(2) Parents may be present in OR for induction of pediatric patients, depending on institutional policy and practice.
f. Postanesthesia priorities
(1) Phase I
(a) Standard phase I activities as previously described
(i) Nurse-to-patient ratio—1:1 until consciousness and reflexes return for pediatric patients
(ii) Children may struggle against face tent; provide humidified oxygen by placing tubing near mouth and nose.
(b) Depending on setting and institutional policy, patient may bypass phase I.
(2) Phase II
(a) Standard phase II activities as previously described
(b) Reunite parents with child as soon as possible to alleviate separation anxiety.
(c) Discharge instructions
(i) Avoid getting ears wet.
(ii) Change cotton balls as directed by physician.
(iii) Discuss pain management techniques.
(iv) Advise parents that tubes may fall out naturally.
g. Psychosocial concerns
(1) Children may experience separation anxiety.
(a) Allow for parent presence at induction if allowed by institutional policy.
(2) Allow child to assert control over situation when appropriate.
(a) Remain in pajamas or street clothes.
(b) Select flavor and scent of mask used for induction.
h. Complications
(1) Hearing loss
(2) Persistent otorrhea
(3) Chronic perforation
(4) Bleeding
(5) Premature tube extrusion
2. Tympanoplasty
a. Purpose
(1) Improve hearing.
(2) Prevent recurrent infection.
b. Description
(1) Refers to a variety of reconstructive surgical procedures performed on deformed or diseased middle ear components
(2) Some tympanoplasties carried out in two stages
(a) First procedure removes diseased tissue; second procedure involves reconstruction of hearing and middle ear function.
(3) Involves tissue grafts of cartilage, bone, fascia, skin, silicone, Teflon, or hydroxyapatite
(4) Types of tympanoplasty
(a) Type I (myringoplasty): repair of tympanic membrane
(b) Type II: graft rests on incus.
(c) Type III: graft attaches to head of stapes.
(d) Type IV: graft attaches to footplate of stapes.
c. Indications
(1) Defects in tympanic membrane
(2) Necrotic destruction of ossicles
(3) Cholesteatoma (epidermal pocket or cystlike sac filled with keratin debris)
(4) Chronic drainage from ear canal
(5) Conductive hearing loss
(6) Trauma
d. Preoperative concerns
(1) Hearing deficits may be present; adjust communication methods as appropriate.
(2) Shampoo hair morning of surgery or night before surgery.
(3) Advise patient that postoperative hearing may be diminished initially because of packing and dressing.
e. Intraoperative concerns
(1) Allow patient to wear hearing aids (if present) to the operating room (OR) to enhance communication.
(2) Involves use of microscope for work on minute, delicate structures
(3) Postauricular (behind ear) and/or endaural (through ear canal) approach used to expose structures of middle ear
(4) Facial nerve monitoring may be used.
(5) Positioning involves tilting OR bed at an angle to provide optimum exposure to operative ear; may cause pressure injury to dependent structures.
f. Postanesthesia concerns
(1) Phase I
(a) Standard phase I activities as previously described
(b) Elevate head of bed at least 30° to minimize eustachian tube edema; clarify positioning with surgeon for specific instructions.
(c) Position with operative ear upward to prevent pressure and graft displacement.
(d) Assess facial nerve function. Report any impairment to the surgeon. Assess facial symmetry by asking patient to:
(i) Smile enough to show teeth.
(ii) Wrinkle forehead.
(iii) Pucker lips.
(iv) Wrinkle nose.
(v) Squeeze eyelids shut.
(vi) Stick out tongue.
(e) Prepare to treat nausea, vomiting, vertigo.
(f) Avoid excess motion; transfer patient slowly and smoothly to minimize vertigo.
(2) Phase II
(a) Standard phase II activities as previously described if patient discharged to home
(b) Discharge instructions
(i) Avoid getting ears wet.
(ii) Avoid sudden turning; encourage slow, smooth motion.
(iii) Sneeze with mouth open to avoid pressure on eustachian tubes.
(iv) Gentle nose blowing only
(v) Noises such as popping and/or cracking may be heard in the ear by the patient and are considered normal.
g. Psychosocial concerns
(1) Anxiety related to hearing loss
h. Complications
(1) Facial nerve injury
(2) Hearing loss caused by drill trauma to ossicles
3. Stapedectomy
a. Purpose
(1) Restoration of stapes bone function
b. Description
(1) Removal of diseased stapes and replacement with prosthetic graft
c. Indications
(1) Treatment of otosclerosis, a condition of unknown etiology characterized by the formation of spongy bone around the round window, which causes stiffening and hardness of the stapes
d. Preoperative concerns
(1) Hearing deficits may be present; adjust communication methods as appropriate.
(2) Advise patient that postoperative hearing may be diminished initially because of packing and dressing.
e. Intraoperative concerns
(1) May be performed under local anesthesia with moderate sedation in adult patients
(2) Involves use of microscope
(3) May involve the use of the laser
(4) Profound intraoperative vertigo may be noted in patients under local anesthesia.
(5) Prosthesis fabricated from Teflon, stainless steel, or other synthetic material
f. Postanesthesia priorities
(1) Phase I
(a) Standard phase I activities as previously described
(b) Elevate head of bed at least 30° to minimize eustachian tube edema; clarify positioning with surgeon for specific instructions.
(c) Position with operative ear upward to prevent pressure and graft displacement.
(d) Nausea, vomiting, and vertigo should be anticipated.
(2) Phase II
(a) Standard phase II activities as previously described
(b) Discharge instructions
(i) Avoid getting ears wet.
(ii) Avoid sudden turning; encourage slow, smooth motion.
(iii) Sneeze with mouth open to avoid pressure on eustachian tubes.
(iv) Gentle nose blowing only
g. Psychosocial concerns
(1) Patient may report immediate improvement in hearing, but hearing may decrease postoperatively because of accumulation of drainage.
h. Complications
(1) If chorda tympani is removed to expose stapes and footplate, loss of taste to anterior two thirds of tongue will occur on the affected side.
(2) Facial nerve dehiscence
(3) Ossicular chain dislocation
(4) Perilymph leak
(5) Dizziness
4. Mastoidectomy
a. Purpose
(1) To eradicate infected or diseased mastoid air cells
b. Description
(1) Simple mastoidectomy
(a) Removal of mastoid air cells only
(2) Modified radical mastoidectomy
(a) Removal of mastoid cells, posterior and superior external bony canal walls
(b) Conversion of mastoid and epitympanic space into one common cavity
(3) Radical mastoidectomy
(a) Removal of mastoid cells, posterior wall of external auditory canal, remnants of tympanic membrane, ossicles (except stapes), and middle ear mucosa
(b) Removal of infected or diseased mucosa from middle ear orifice of the eustachian tube
(c) Conversion of middle ear and mastoid space into one cavity
c. Indications
(1) Acute or chronic infection
(2) Extension of cholesteatoma into mastoid cells
d. Preoperative concerns
(1) Hearing deficits may be present; adjust communication methods as appropriate.
(2) Advise patient that postoperative hearing may be diminished initially because of packing and dressing.
e. Intraoperative concerns
(1) Involves use of microscope
(2) Positioning involves tilting OR bed at an angle to provide optimum exposure to operative ear; may cause pressure injury to dependent structures.
f. Postanesthesia concerns
(1) Phase I
(a) Standard phase I activities as previously described
(b) Elevate head of bed at least 30°; clarify positioning with surgeon for specific instructions.
(c) Position with operative ear upward to prevent pressure.
(d) Assess facial nerve function. Report any impairment to the surgeon. Assess facial symmetry by asking patient to:
(i) Smile enough to show teeth.
(ii) Wrinkle forehead.
(iii) Pucker lips.
(iv) Wrinkle nose.
(v) Squeeze eyelids shut.
(vi) Stick out tongue.
(e) Prepare to treat nausea, vomiting, vertigo.
(f) Avoid excess motion; transfer patient slowly and smoothly to minimize vertigo.
(2) Phase II
(a) Standard phase II activities as previously described if patient discharged to home
(b) Discharge instructions
(i) Avoid getting ears wet.
(ii) Avoid sudden turning; encourage slow, smooth motion.
(iii) Sneeze with mouth open to avoid pressure on eustachian tubes.
(iv) Gentle nose blowing only
(v) Noises such as popping and/or cracking may be heard in the ear by the patient and are considered normal.
g. Psychosocial concerns
(1) Patient may report immediate improvement in hearing; hearing may decrease postoperatively from accumulation of drainage.
h. Complications
(1) Facial nerve dehiscence and damage
(2) Dizziness
5. Endolymphatic shunt
a. Purpose
(1) To relieve pressure in endolymphatic sac
b. Description
(1) Placement of shunt (commercially prepared or fashioned by surgeon) into endolymphatic sac via a mastoidectomy to allow for drainage of excess endolymph
c. Indications
(1) Treatment of Meniere’s disease
d. Preoperative concerns
(1) Vertigo may be present preoperatively; a quiet, dark environment is advised to minimize stimuli.
e. Intraoperative concerns
(1) Transfer patient slowly to avoid exacerbation of vertigo.
(2) See information on mastoidectomy (preceding section III.A.4.e).
f. Postanesthesia concerns
(1) Phase I
(a) Standard phase I activities as previously described
(b) Elevate head of bed at least 30°; clarify positioning with surgeon for specific instructions.
(c) Position with operative ear upward to prevent pressure.
(d) Prepare to treat nausea, vomiting, vertigo.
(e) Avoid excess motion; transfer patient slowly and smoothly to minimize vertigo.
(2) Phase II
(a) Standard phase II activities as previously described if patient discharged to home; patients may require 24-hour admission because of vertigo.
(b) Discharge instructions
(i) Avoid getting ears wet.
(ii) Avoid sudden turning; encourage slow, smooth motion.
(iii) Sneeze with mouth open to avoid pressure on eustachian tubes.
(iv) Gentle nose blowing only
(v) Noises such as pulsations, popping, and/or cracking may be heard in the ear by the patient and are considered normal.
g. Psychosocial concerns
(1) Patients with Meniere’s disease may experience feelings of
(a) Loss of control
(b) Depression
(c) Powerlessness related to the unpredictability of the condition
(2) Lifestyle modifications may be necessary to cope with vertigo and hearing deficits.
h. Complications
(1) Deafness or profound hearing loss
(2) Labyrinthitis
6. Vestibular neurectomy
a. Purpose
(1) To interrupt transmission of the vestibular branch of the acoustic nerve, reducing stimuli to the vestibule and alleviating vertigo
b. Description
(1) Resection of the vestibular portion of the acoustic nerve with preservation of the cochlear portion via transcochlear, translabyrinthine, middle fossa, retrolabyrinthine, or retrosigmoid approaches
c. Indications
(1) Meniere’s disease
(2) Traumatic labyrinthitis
(3) Vestibular neuronitis
d. Preoperative concerns
(1) Vertigo may be present preoperatively; a quiet, dark environment is advised to minimize stimuli.
e. Intraoperative concerns
(1) A fat graft is obtained from either the abdomen or lateral thigh to obliterate the mastoid cavity at the end of the procedure.
f. Postanesthesia concerns
(1) Phase I
(a) Standard phase I activities as previously described
(b) Elevate head of bed at least 30°; clarify positioning with surgeon for specific instructions.
(c) Position with operative ear upward to prevent pressure.
(d) Prepare to treat nausea, vomiting, vertigo.
(e) Avoid excess motion; transfer patient slowly and smoothly to minimize vertigo.
(f) Assess facial nerve function. Report any impairment to the surgeon. Assess facial symmetry by asking patient to:
(i) Smile enough to show teeth.
(ii) Wrinkle forehead.
(iii) Pucker lips.
(iv) Wrinkle nose.
(v) Squeeze eyelids shut.
(vi) Stick out tongue.
(2) Phase II
(a) Patient may be transferred to intensive care unit (ICU) if middle fossa approach used.
(b) Standard phase II activities as previously described if discharged home after transcochlear or translabyrinthine approaches; may require 24-hour admission
(c) Discharge instructions
(i) Avoid getting ears wet.
(ii) Avoid sudden turning; encourage slow, smooth motion.
(iii) Sneeze with mouth open to avoid pressure on eustachian tubes.
(iv) Gentle nose blowing only
(v) Noises such as pulsations, popping, and/or cracking may be heard in the ear by the patient and are considered normal.
g. Psychosocial concerns
(1) Patients with vertigo may experience feelings of loss of control, depression, and powerlessness related to the unpredictability of the condition.
(2) Lifestyle modifications may be necessary to cope with vertigo and hearing deficits.
h. Complications
(1) Cerebrospinal fluid (CSF) leak
(2) Dural herniation
7. Labyrinthectomy
a. Purpose
(1) Alleviation of severe vertigo
b. Description
(1) Destruction of the membranous labyrinth of the horizontal semicircular canal via transcanal or transmastoid approach
c. Indications
(1) Refractive unilateral Meniere’s disease in a deaf or near-deaf ear
d. Preoperative concerns
(1) Causes total deafness in operative ear
(2) Vertigo may be present preoperatively; a quiet, dark environment is advised to minimize stimuli.
e. Intraoperative concerns
(1) Transfer patient slowly to avoid exacerbation of vertigo.
(2) See information on tympanoplasty (preceding section III.A.2.e).
f. Postanesthesia priorities
(1) Phase I
(a) Standard phase I activities as previously described
(b) Elevate head of bed at least 30°; clarify positioning with surgeon for specific instructions.
(c) Position with operative ear upward to prevent pressure.
(d) Prepare to treat nausea, vomiting, vertigo.
(e) Avoid excess motion; transfer patient slowly and smoothly to minimize vertigo.
(f) Assess facial nerve function. Report any impairment to the surgeon. Assess facial symmetry by asking patient to:
(i) Smile enough to show teeth.
(ii) Wrinkle forehead.
(iii) Pucker lips.
(iv) Wrinkle nose.
(v) Squeeze eyelids shut.
(vi) Stick out tongue.
(2) Phase II
(a) Standard phase II activities as previously described if discharged to home; may require 24-hour admission
(b) Discharge instructions
(i) Avoid getting ears wet.
(ii) Avoid sudden turning; encourage slow, smooth motion.
(iii) Sneeze with mouth open to avoid pressure on eustachian tubes.
(iv) Gentle nose blowing only
(v) Noises such as pulsations, popping, and/or cracking may be heard in the ear by the patient and are considered normal.
(vi) Severe dizziness may be expected for several days as the brainstem must accommodate to labyrinth destruction and compensate.
(vii) Temporary taste disturbances can occur, but normal functioning will generally return.
g. Psychosocial concerns
(1) Patients with vertigo may experience feelings of loss of control, depression, and powerlessness related to the unpredictability of the condition.
(2) Lifestyle modifications may be necessary to cope with vertigo and hearing deficits.
h. Complications
(1) Meningitis
(2) CSF leak
(3) Tinnitus
(4) Facial nerve paralysis
(5) Taste disturbances
8. Facial nerve decompression and exploration
a. Purpose
(1) To relieve facial nerve pressure caused by edema or other compromise
(2) Repair of facial nerve transection
b. Description
(1) Incision of facial nerve sheath at area of compromise via transmastoid, translabyrinthine, or middle cranial fossa approach
(2) Repair of transected nerve with nerve graft
c. Indications
(1) Bell’s palsy: an idiopathic edema and inflammation of the facial nerve, possibly viral in origin
(2) Trauma: skull or mandibular fractures, gunshot wounds
d. Preoperative concerns
(1) Eye on affected side must be protected to guard against corneal dryness.
e. Intraoperative concerns
(1) Eye on affected side protected with ointment or tarsorrhaphy
(2) Nerve monitoring via electromyography
(3) Auditory brainstem evoked potentials may also be used.
f. Postanesthesia priorities
(1) Phase I
(a) Standard phase I activities as previously described
(b) Elevate head of bed at least 30°; clarify positioning with surgeon for specific instructions.
(c) Place patient on side to prevent aspiration.
(d) Assess facial nerve function. Report any impairment to the surgeon. Assess facial symmetry by asking patient to:
(i) Smile enough to show teeth.
(ii) Wrinkle forehead.
(iii) Pucker lips.
(iv) Wrinkle nose.
(v) Squeeze eyelids shut.
(vi) Stick out tongue.
(2) Phase II
(a) Patient may be transferred to ICU if middle fossa cranial approach is used.
(b) Discharge instructions
(i) Discuss aspiration risks and preventive measures.
(ii) Review oral care procedures.
(iii) Discuss importance of eye care and eye protection.
g. Psychosocial concerns
(1) Body image disturbances related to appearance
(2) Regeneration time of repaired nerves may be lengthy, resulting in slow changes to appearance and function.
h. Complications
(1) Scarring of nerve after repair
(2) CSF leak (if cranial approach used)
(3) Infection
(4) Dizziness
9. Removal of acoustic neuroma (vestibular schwannoma)
a. Purpose
(1) To remove tumor mass while preserving nerve function
b. Description
(1) Vestibular schwannomas are benign tumors arising from the Schwann cells of the vestibular portion of the acoustic nerve that may cause a myriad of symptoms including:
(a) Hearing loss
(b) Headache
(c) Vertigo
(d) Tinnitus
(e) Gait disturbance
(f) Ocular disorders
(2) Procedure involves resection of tumors usually via a translabyrinthine or middle cranial approach.
c. Indications
(1) Diagnosed vestibular schwannoma
(2) Neurofibromatosis
d. Preoperative concerns
(1) Hair removal may range from partial to complete head shave.
e. Intraoperative concerns
(1) Middle cranial approach may be performed in sitting or prone position.
(2) Risk for air embolism related to surgical positioning.
f. Postanesthesia priorities
(1) Phase I
(a) Standard phase I activities as previously described
(b) Elevate head of bed at least 30°; clarify positioning with surgeon for specific instructions.
(c) IV fluid infusion strictly monitored to prevent overload and possible cerebral edema
(d) Patient will be transferred to ICU after phase I care.
g. Psychosocial concerns
(1) Partial or total hearing loss will necessitate lifestyle adjustments.
(2) Possible body image disturbance related to hair removal
h. Complications
(1) CSF leak
(2) Dural herniation
(3) Air embolism
(4) Tinnitus
(5) Facial nerve paralysis
(6) Vertigo
(7) Hearing loss or dead ear
(8) Meningitis
B. Nose
1. Septoplasty, submucous resection
a. Purpose
(1) To repair acquired or congenital intranasal and septal defects that interferes with normal respiratory function
b. Description
(1) Excision of deviated septal cartilage and bone via intranasal incision
(2) Removal of polypoid tissue, if present
(3) May include turbinectomy (reduction of turbinate size)
(4) Restoration of functional septal architecture
c. Indications
(1) Deviated nasal septum
(2) Nasal polyps
(3) Hypertrophied nasal turbinates
d. Preoperative concerns
(1) Discuss expected postoperative events.
(a) Nasal packing may be in place and cause feeling of suffocation; patient will have to breathe through his or her mouth.
(b) Drip pad (moustache) dressing will be in place; will be changed as necessary.
e. Intraoperative concerns
(1) May be performed under local anesthesia or monitored anesthesia care for adults
(2) Nasal packing and/or nasal splints inserted
(a) Nasal packing prevents hematoma.
(b) Nasal splints help prevent synechiae (adhesions).
f. Postanesthesia priorities
(1) Phase I
(a) Standard phase I activities as previously described
(b) Progress from side lying to semi-Fowlers with head of bed elevated 30°.
(c) Monitor patient closely for hypoventilation and hypoxia related to nasal packing and mouth breathing.
(d) Apply ice packs as ordered to promote vasoconstriction and minimize edema.
(e) Change moustache dressing as needed.
(f) Observe for hemorrhage and/or septal hematoma.
(i) Frequent swallowing may indicate bleeding.
(ii) Blood from septal hematoma dissects into cheeks, upper lip, and nose.
(g) Excessive gagging may be indication that packing has dislodged and migrated to pharynx.
(i) Provide equipment for reinsertion.
[a] Bayonet forceps
[b] Nasal speculum
[c] Scissors
[d] Nasal packing
[e] Headlight
[f] Tongue depressor
(ii) Provide reassurance to patient.
(iii) Administer pain medications as necessary.
(2) Phase II
(a) Standard phase II activities as previously described
(b) Offer frequent mouth rinses to combat mouth dryness and rinse blood from oral cavity.
(c) Discharge instructions
(i) Change moustache dressing when soiled—maintain count of change frequency if excessively soiled.
(ii) Use a humidifier as ordered/needed to moisten the air.
(iii) No nose blowing; sniff secretions to the back of the nose; swallow or expectorate.
(iv) No bending, straining, or lifting
(v) Sneeze with the mouth open.
(vi) Bloody or tarry stools may be expected because of swallowed blood.
(vii) Nausea may be expected due to swallowed blood.
g. Psychosocial concerns
(1) Nasal packing may cause feelings of claustrophobia and anxiety.
h. Complications
(1) Bleeding
(2) Infection
(3) Edema
(4) Septal perforation
(5) Intranasal synechiae (adhesions)
(6) Septal hematoma
2. Rhinoplasty
a. Purpose
(1) Restoration and improvement of respiratory function
(2) Alteration of appearance of the nose
b. Description
(1) Nasal cartilage and bony structure reduced, realigned, or augmented via intranasal or small external skin incisions
(2) Surgical fracture of nasal bones
(3) May change appearance of sides, tip, or hump of nose
c. Indications
(1) Traumatic or congenital deformity
(2) Cosmetic appearance
d. Preoperative concerns
(1) Discuss expected postoperative events.
(a) Nasal packing may be in place and cause feeling of suffocation; patient will have to breathe through his or her mouth.
(b) Drip pad (moustache) dressing will be in place; will be changed as necessary.
(c) Facial edema and bruising may occur.
e. Intraoperative concerns
(1) May be combined with septoplasty to correct defects
(2) May be performed under local anesthesia or monitored anesthesia care in adult patients
(3) External nasal splint and dressing may be applied to maintain correction.
f. Postanesthesia priorities
(1) Phase I
(a) Standard phase I activities as previously described
(b) Progress from side lying to semi-Fowlers with head of bed elevated 30°.
(c) Monitor patient closely for hypoventilation and hypoxia related to nasal packing and mouth breathing.
(d) Apply ice packs as ordered to nose and eyes to promote vasoconstriction and minimize edema.
(e) Change moustache dressing as needed.
(f) Observe for hemorrhage.
(i) Frequent swallowing may indicate bleeding.
(g) Excessive gagging may be indication that packing has migrated to pharynx.
(i) See information on septoplasty (preceding section III.B.1.f).
(2) Phase II
(a) Standard phase II activities as previously described
(b) Offer frequent mouth rinses to combat mouth dryness and rinse blood from oral cavity.
(c) Discharge instructions
(i) Change moustache dressing when soiled. Maintain count of change frequency if excessively soiled.
(ii) Use a humidifier as ordered/needed to moisten the air.
(iii) No nose blowing; sniff secretions to the back of the nose; swallow or expectorate.
(iv) No bending, straining, or lifting
(v) Sneeze with the mouth open.
(vi) Bloody or tarry stools may be expected because of swallowed blood.
(vii) External splint should not be disturbed or removed by patient.
g. Psychosocial concerns
(1) Initial cosmetic results may not meet patient’s expectations.
(2) Mild edema may persist for several months, obscuring final results of surgery.
h. Complications
(1) CSF leak
(2) Bleeding
(3) Edema
(4) Undesirable or unanticipated cosmetic appearance
3. Reduction of nasal fracture
a. Purpose
(1) Restoration of nasal architecture
(2) Prevention of nasal deformity
b. Description
(1) Tactile manipulation of external nose to realign cartilaginous structures
(2) Intranasal reduction of fracture with instrumentation
c. Indications
(1) Nasal trauma
d. Preoperative concerns
(1) Procedure may be delayed to allow swelling from injury to subside.
e. Intraoperative concerns
(1) May be performed under local anesthesia or monitored anesthesia care in adult patients
(2) Generally does not require postoperative nasal packing
f. Postanesthesia priorities
(1) Phase I
(a) Standard phase I activities as previously described
(b) Progress from side lying to semi-Fowlers with head of bed elevated 30°.
(c) Apply ice packs as ordered to nose and eyes to promote vasoconstriction and minimize edema.
(2) Phase II
(a) Standard phase II activities as previously described
(b) Discharge instructions
(i) No nose blowing; sniff secretions to the back of the nose; swallow or expectorate.
(ii) No bending, straining, or lifting
(iii) Sneeze with the mouth open.
(iv) Bloody or tarry stools may be expected because of swallowed blood.
g. Psychosocial concerns
(1) Additional procedures may be necessary if acceptable cosmetic results not achieved.
h. Complications
(1) Incomplete reduction of fracture
(2) Septal hematoma
(3) CSF leak
C. Paranasal sinuses
1. Functional endoscopic sinus surgery
a. Purpose
(1) Removal of diseased sinus mucosa
(2) Establishment or reestablishment of airflow, mucociliary clearance, and drainage from osteomeatal complex (channel that connects the nasal passage to the sinus cavity)
b. Description
(1) Nasal cavity examined via a rigid telescope inserted through the nares
(2) Sinuses entered via fenestrations
(3) Under direct vision, mucosa and/or polyps stripped and removed
(4) Sinus osteomeatal complex enlarged as needed and bony structure altered to achieve functional drainage
(5) Mucopurulent fluid drained
c. Indications
(1) Nasal polyps
(2) Chronic sinusitis
(3) Mucocele
(4) Tumor masses
d. Preoperative concerns
(1) Discuss expected postoperative events.
(a) Nasal packing may be in place and cause feeling of suffocation; patient will have to breathe through his or her mouth.
(b) Drip pad (moustache) dressing will be in place; will be changed as necessary.
e. Intraoperative concerns
(1) May be performed under local anesthesia with sedation in adult patients
(2) Uses telescopes and video equipment to visualize intranasal structures
(3) Powered instrumentation may be used to remove diseased mucosa.
(4) Care taken to maintain integrity of orbit to avoid ophthalmic injury
(5) Packing may extend into sinus cavity.
f. Postanesthesia priorities
(1) Phase I
(a) Standard phase I activities as previously described
(b) Progress from side lying to semi-Fowlers with head of bed elevated 30°.
(c) Monitor patient closely for hypoventilation and hypoxia related to nasal packing and mouth breathing.
(d) Apply ice packs as ordered to nose and eyes to promote vasoconstriction and minimize edema.
(e) Change moustache dressing when soiled. Maintain count of change frequency if excessively soiled.
(f) Observe for hemorrhage.
(i) Frequent swallowing may indicate bleeding.
(g) Excessive gagging may be indication that packing has migrated to pharynx.
(i) See information on septoplasty (preceding section III.B.1.f).
(h) Observe for excessive orbital swelling, bruising, changes to visual acuity, impairment of extraocular movements.
(i) Observe for excessive clear rhinorrhea; could indicate possible CSF leak.
(2) Phase II
(a) Standard phase II activities as previously described
(b) Discharge instructions
(i) No nose blowing; sniff secretions to the back of the nose; swallow or expectorate.
(ii) No bending, straining, or lifting
(iii) Sneeze with the mouth open.
(iv) Change moustache dressing when soiled. Maintain count of change frequency if excessively soiled.
(v) Bloody or tarry stools may be expected because of swallowed blood.
g. Psychosocial concerns
(1) Patient may have altered postoperative appearance (orbital bruising [“raccoon eyes”]) if extensive surgery performed in ethmoid cavity.
h. Complications
(1) Orbital hematoma
(2) Optic nerve damage
(3) CSF leak
(4) Hemorrhage
(5) Infection
(6) Recurrence of nasal polyps
2. Caldwell Luc antrostomy
a. Purpose
(1) To access the maxillary sinus for removal of diseased sinus mucosa or polyps and/or to ligate the maxillary artery
(2) Establishment or reestablishment of drainage from osteomeatal complex
b. Description
(1) Sublabial and nasal mucosal incisions created
(2) Bone removed from antral wall to create opening for drainage
(3) Mucosal material stripped from walls of maxillary sinus
(4) Division and ligation of maxillary artery where indicated
(5) Packing placed in maxillary sinus cavity and nasal cavity
c. Indications
(1) Chronic sinusitis unresponsive to medical therapy
(2) Maxillary polyps
(3) Maxillary tumors
(4) Foreign bodies
(5) Acute or chronic epistaxis
d. Preoperative concerns
(1) Discuss expected postoperative events.
(a) Nasal packing may be in place and cause feeling of suffocation; patient will have to breathe through his or her mouth.
(b) Drip pad (moustache) dressing will be in place; will be changed as necessary.
(c) Facial edema may occur.
e. Intraoperative concerns
(1) May be performed under general or local anesthesia
f. Postanesthesia priorities
(1) Phase I
(a) Standard phase I activities as previously described
(b) Progress from side lying to semi-Fowlers with head of bed elevated 30°.
(c) Monitor patient closely for hypoventilation and hypoxia related to nasal packing and mouth breathing.
(d) Apply ice packs as ordered to face to promote vasoconstriction and minimize edema.
(e) Change moustache dressing as needed.
(f) Offer frequent mouth rinses to combat mouth dryness and eliminate bloody secretions from intraoral incisions.
(g) Observe for hemorrhage.
(i) Frequent swallowing may indicate bleeding.
(h) Excessive gagging may be indication that packing has migrated to pharynx.
(i) See information on septoplasty (preceding section III.B.1.f).
(2) Phase II
(a) Standard phase II activities as previously described
(b) Discharge instructions
(i) No nose blowing; sniff secretions to the back of the nose; swallow or expectorate.
(ii) No bending, straining, or lifting
(iii) Sneeze with the mouth open.
(iv) Continue to brush teeth, but avoid intraoral incisions; avoid excessive brushing pressure to teeth and gums. Use a soft toothbrush.
(v) Change moustache dressing when soiled. Maintain count of change frequency if excessively soiled.
(vi) Bloody or tarry stools may be expected because of swallowed blood.
g. Psychosocial concerns
(1) Numbness to lip may result in uneven smile or altered appearance to lip and mouth.
h. Complications
(1) Persistent numbness to cheek, upper lip, gums, and teeth
(2) Damage to maxillary division of the trigeminal nerve (cranial nerve V) will cause permanent loss of sensation to upper lip.
(3) Oral antral fistula
3. Ethmoidectomy
a. Purpose
(1) Promotion of drainage of the ethmoid sinus
(2) Used in conjunction with orbital decompression for exophthalmos
b. Description
(1) Intranasal or external medical canthal incision
(2) Removal of bony walls between ethmoid air cells
(3) Creation of common ethmoid cavity to promote drainage
c. Indications
(1) Chronic ethmoid sinusitis
(2) Mucoceles
(3) Polyps
d. Preoperative concerns
(1) Discuss expected postoperative events.
(a) Nasal packing may be in place and cause feeling of suffocation; patient will have to breathe through his or her mouth.
(b) Drip pad (moustache) dressing will be in place; will be changed as necessary.
(c) Facial edema and bruising may occur.
e. Intraoperative concerns
(1) May use operating microscope
(2) May use endoscopes
f. Postanesthesia priorities
(1) Phase I
(a) Standard phase I activities as previously described
(b) Progress from side lying to semi-Fowlers with head of bed elevated 30°.
(c) Monitor patient closely for hypoventilation and hypoxia related to nasal packing and mouth breathing.
(d) Apply ice packs as ordered to nose and eyes to promote vasoconstriction and minimize edema.
(e) Change moustache dressing as needed.
(f) Observe for hemorrhage.
(i) Frequent swallowing may indicate bleeding.
(g) Excessive gagging may be indication that packing has migrated to pharynx.
(i) See information on septoplasty (preceding section III.B.1.f).
(h) Observe for excessive orbital swelling, bruising, changes to visual acuity, impairment of extraocular movements.
(2) Phase II
(a) Standard phase II activities as previously described.
(b) Discharge instructions
(i) No nose blowing; sniff secretions to the back of the nose; swallow or expectorate.
(ii) No bending, straining, or lifting
(iii) Sneeze with the mouth open.
(iv) Sleep with head elevated to minimize edema.
(v) Apply ice packs as ordered to face to minimize bruising.
(vi) Bloody or tarry stools may be expected because of swallowed blood.
g. Psychosocial concerns
(1) If eye pads and eye dressings are applied in the OR, patient may experience panic because of inability to see.
(2) Patient will have altered postoperative appearance from edema and orbital bruising (“raccoon eyes”).
h. Complications
(1) CSF leak
(2) Orbital injury
(3) Optic nerve injury and loss of vision
(4) Diplopia
(5) Hemorrhage
4. Frontal sinusotomy and obliteration
a. Purpose
(1) To eradicate diseased mucosa from the frontal sinus and obliterate the space to prevent communication with the nasal cavity
(2) Reduction and management of frontal sinus fractures
(3) Removal of tumors
b. Description
(1) Approached through brow or scalp (bicoronal) incision
(2) Periosteum elevated; bone cut superiorly and laterally
(3) Fat graft removed from abdomen to pack sinus cavity
(4) Pressure dressing applied
c. Indications
(1) Chronic frontal sinusitis
d. Preoperative concerns
(1) May require hair removal to accomplish bicoronal incision
(2) Facial edema and bruising may occur.
e. Intraoperative concerns
(1) May require team approach from otorhinolaryngology and neurosurgery
f. Postanesthesia priorities
(1) Phase I
(a) Standard phase I activities as previously described
(b) Elevate head of bed at least 30°; clarify positioning with surgeon for specific instructions.
(c) Place patient on side to prevent aspiration.
(d) Monitor patient closely for hypoventilation and hypoxia related to nasal packing and mouth breathing.
(e) Apply ice packs as ordered to face to promote vasoconstriction and minimize edema.
(f) Observe for hemorrhage.
(i) Frequent swallowing may indicate bleeding.
(g) Excessive gagging may be indication that packing has migrated to pharynx.
(i) See information on septoplasty (preceding section III.B.1.f).
(2) Phase II
(a) Standard phase II activities as previously described if patient discharged to home; may require 24-hour admission
(b) Discharge instructions
(i) No nose blowing; sniff secretions to the back of the nose; swallow or expectorate.
(ii) No bending, straining, or lifting
(iii) Sneeze with the mouth open.
(iv) Sleep with head elevated to minimize edema.
(v) Report signs and symptoms of infection to surgeon.
g. Psychosocial concerns
(1) Unacceptable cosmetic appearance from hair removal, scarring, and/or prolonged edema
h. Complications
(1) CSF leak
(2) Meningitis
(3) Brain abscess
(4) Scalp hematoma
(5) Fat necrosis
(6) Infection to donor site
D. Oropharyngeal
1. Adenoidectomy
a. Purpose
(1) To remove infected or hypertrophied adenoidal tissue
b. Description
(1) Removal of adenoids with sharp and blunt dissection via intrapharyngeal incisions
c. Indications
(1) Chronic infection (adenoiditis or otitis media)
(2) Lymphoid hypertrophy
d. Preoperative concerns
(1) Discuss expected postoperative events.
(2) Frequently performed in pediatric population; use age-appropriate teaching techniques and interventions.
e. Intraoperative concerns
(1) Performed under general anesthesia
(2) Often performed in conjunction with tonsillectomy
(3) Parents may be present in OR for induction of pediatric patients, depending on institutional policy and practice.
f. Postanesthesia priorities
(1) Phase I
(a) Standard phase I activities as previously described
(b) Place patient on side to prevent aspiration; advance to semi-Fowlers with head of bed elevated 30° when patient awake.
(c) Monitor closely for hemorrhage.
(i) Bright red emesis
(ii) Frequent and repeated swallowing
(iii) Agitation and restlessness
(d) Pediatric considerations
(i) Nurse-to-patient ratio 1:1 until consciousness and reflexes return for pediatric patients
(ii) Children may struggle against face tent; provide humidified oxygen by placing tubing near mouth and nose.
(2) Phase II
(a) Standard phase II activities as previously described
(b) Discharge instructions
(i) Avoid throat clearing, coughing, vigorous nose blowing.
(ii) No bending, straining, or lifting
(iii) Bland and soft diet
(iv) Bloody or tarry stools may be expected because of swallowed blood
(v) Voice rest
(vi) Throat discomfort increases between postoperative days 4 and 8 because of separation of eschar from pharyngeal bed.
g. Psychosocial concerns
(1) Children may experience separation anxiety.
(a) Allow for parent presence at anesthesia induction if allowed by institutional policy.
(2) Allow child to assert control over situation when appropriate.
(a) Remain in pajamas or street clothes.
(b) Select flavor and scent of mask used for induction.
h. Complications
(1) Otalgia
(2) Velopharyngeal insufficiency
(3) Hemorrhage
(4) Hypernasality
(5) Nasopharyngeal stenosis
2. Tonsillectomy
a. Purpose
(1) To remove tonsillar tissue
b. Description
(1) Removal of tonsils with sharp and blunt dissection via intrapharyngeal incisions
c. Indications
(1) Chronic tonsillitis
(2) Peritonsillar abscess
(3) Tonsillar hypertrophy
(4) Ulcerations, lesions, and masses
(5) Obstructive sleep apnea
d. Preoperative concerns
(1) Discuss expected postoperative events.
(2) Frequently performed in pediatric population; use age-appropriate teaching techniques and interventions.
e. Intraoperative concerns
(1) May be performed with local anesthetic and monitored anesthesia care in adults
f. Postanesthesia priorities
(1) Phase I
(a) See information on adenoidectomy (preceding section III.D.1.f.[1]).
(2) Phase II
(a) See information on adenoidectomy (preceding section III.D.1.f.[2]).
g. Psychosocial concerns
(1) See information on adenoidectomy (preceding section III.D.1.g).
h. Complications
(1) Hemorrhage
(2) Postoperative airway obstruction secondary to edema
3. Uvulopalatopharyngoplasty
a. Purpose
(1) To reduce the amount of redundant pharyngopalatal mucosa
b. Description
(1) Removal of tissue, reduction of or removal of uvula via intrapharyngeal incisions; sharp and dull dissection
(2) Tonsillectomy may also be performed.
c. Indications
(1) Obstructive sleep apnea
(2) Snoring
d. Preoperative concerns
(1) Discuss expected postoperative events.
(a) Possibility of tracheostomy if edema is excessive; reinforce physician information regarding tracheostomy.
e. Intraoperative concerns
(1) May be intubated awake if obstruction and amount of redundant tissue is severe
(2) May be performed under local anesthesia with moderate sedation
(3) Laser may be used.
(4) Tracheostomy may be placed as temporary measure if extensive dissection performed or excessive airway edema is anticipated.
f. Postanesthesia priorities
(1) Phase I
(a) Standard phase I activities as previously described
(b) Progress from side lying to semi-Fowlers with head of bed elevated 30°.
(c) Monitor patient closely for hypoventilation and hypoxia related to edema.
(d) Perform intraoral suctioning with care to avoid trauma to mucosal incision lines.
(2) Phase II
(a) Often transferred to ICU for observation because of risk of airway edema and compromise
(b) Generally will be admitted for minimum of 24 hours because of risk of airway edema
(c) Discharge instructions
(i) Avoid throat clearing and coughing.
(ii) No bending, straining, or lifting
(iii) Bland or soft diet
(iv) Bloody or tarry stools may be expected because of swallowed blood.
(v) Use humidifier to moisten the air.
(vi) Maintain hydration.
(vii) Voice rest
g. Psychosocial concerns
(1) Tracheostomy will temporarily affect verbal communication.
(2) Patient and/or caregivers will require tracheostomy care instructions.
(3) Procedure may alleviate snoring, but sleep apnea may still be present.
h. Complications
(1) Airway edema
(2) Hemorrhage
(3) Infection
4. Salivary gland surgery
a. Purpose
(1) To remove infected salivary glands, sialoliths, cysts, or neoplasms
(2) Correction of ductal stenosis
b. Description
(1) Types
(a) Submandibular gland excision
(b) Parotidectomy
c. Indications
(1) Malignant and benign neoplasms
(2) Diagnostic biopsy
(3) Sialoliths and sialolithiasis
(4) Trauma causing stenosis of the duct
(5) Cysts
d. Preoperative concerns
(1) Discuss expected postoperative events.
e. Intraoperative concerns
(1) Facial nerve monitoring may be used.
f. Postanesthesia priorities
(1) Phase I
(a) Standard phase I activities as previously described
(b) Progress from side lying to semi-Fowlers with head of bed elevated 30°.
(c) Monitor patient closely for hemorrhage.
(d) Assess facial nerve function. Report any impairment to the surgeon. Assess facial symmetry by asking patient to:
(i) Smile enough to show teeth.
(ii) Wrinkle forehead.
(iii) Pucker lips.
(iv) Wrinkle nose.
(v) Squeeze eyelids shut.
(vi) Stick out tongue.
(2) Phase II
(a) Standard phase II activities as previously described if patient discharged to home; may require 24-hour admission
(b) Discharge instructions
(i) Avoid throat clearing and coughing.
(ii) No bending, straining, or lifting
(iii) Bland and soft diet
g. Psychosocial concerns
(1) Possible Frey’s syndrome (manifested by flushing and sweating on the cheek area appearing when the patient eats, sees, or thinks about or talks about certain kinds of food that produce salivation)
h. Complications
(1) Hemorrhage
(2) Facial nerve paralysis
(3) Gustatory sweating (Frey’s syndrome)
(4) Salivary fistula
5. Esophagoscopy
a. Purpose
(1) To assess the structure and function of the esophagus and cardia (e.g., junction of esophagus and stomach) of the stomach
(2) To obtain tissue biopsy to facilitate diagnoses
b. Description
(1) Direct visualization with a rigid or flexible scope
c. Indications
(1) Suspected carcinoma
(2) Stricture and stenosis
(3) Reflux
(4) Bleeding
d. Preoperative concerns
(1) Discuss expected postoperative events.
e. Intraoperative concerns
(1) May occasionally be performed under topical anesthesia and moderate sedation
f. Postanesthesia priorities
(1) Phase I
(a) Standard phase I activities as previously described
(b) Progress from side lying to semi-Fowlers with head of bed elevated 30°.
(c) Assess return of swallowing and gag reflex.
(d) Observe for perforation and hemorrhage. Symptoms include:
(i) Frank blood in emesis
(ii) Agitation and restlessness
(iii) Complaints of severe pain disproportionate to the procedure
(2) Phase II
(a) Standard phase II activities as previously described
(b) Discharge instructions
(i) Avoid throat clearing and coughing.
(ii) Bland and soft diet when gag reflex returned
(iii) Voice rest
(iv) Avoid lifting and straining.
g. Psychosocial concerns
(1) Anxiety related to diagnostic findings
h. Complications
(1) Bleeding
(2) Edema
(3) Esophageal perforation
E. Larynx
1. Tracheostomy
a. Purpose
(1) To create a surgical opening in the trachea for airway maintenance
b. Description
(1) Incision over the trachea
(2) Insertion of a catheter or cannula through tracheal rings
c. Indications
(1) Acute airway obstruction
(2) Prolonged ventilator dependency
(3) Prevention of aspiration
(4) Bypass of upper airway obstruction because of tumor
d. Preoperative concerns
(1) May be emergent procedure
e. Intraoperative concerns
(1) Send obturator and ventilator adaptors to PACU with patient.
f. Postanesthesia priorities
(1) Phase I
(a) Standard phase I activities as previously described
(b) Elevate head of bed 30°.
(c) Ensure that tracheostomy tube ties are secure.
(d) Prepare to reinsert tracheostomy tube or obturator if tube is coughed out.
(e) Observe for hemorrhage.
(f) Assess for pneumothorax.
(g) Provide alternate means of communication for patient (e.g., magic slate, pen and paper, communication board).
(2) Phase II
(a) May be transferred to ICU for observation; otherwise will require 24-hour admission at minimum
(b) Discharge instructions
(i) Discuss need for humidification.
(ii) Teach tracheostomy care to patient, family, and/or caregivers.
(iii) Discuss cardiopulmonary resuscitation needs with caregiver. Standard mouth-to-mouth rescue breathing will be ineffective.
g. Psychosocial concerns
(1) Reduces ability to communicate verbally; alternate methods of communication must be used unless speaking valve is in place.
(2) Body image disturbances
h. Complications
(1) Hemorrhage
(2) Dislodgement of tracheotomy tube
(3) Tracheoesophageal fistula
(4) Subcutaneous emphysema
(5) Pneumothorax
(6) Tracheostenosis
2. Laryngoscopy
a. Purpose
(1) To visualize the interior of the larynx
(2) Obtain tissue biopsy for diagnosis
(3) Removal of vocal cord lesions
b. Description
(1) Types
(a) Direct laryngoscopy
(i) Rigid
(ii) Flexible
(b) Microsuspension laryngoscopy
c. Indications
(1) Suspected carcinoma
(2) Vocal cord polyps and nodules
d. Preoperative concerns
(1) Discuss expected postoperative events.
e. Intraoperative concerns
(1) Prepare for laryngospasm on extubation.
f. Postanesthesia priorities
(1) Phase I
(a) Standard phase I activities as previously described
(b) Progress from side lying to semi-Fowlers with head of bed elevated 30°.
(c) Be alert to possibility of laryngospasm.
(d) Assess for return of swallowing and gag reflexes.
(e) Mild hemoptysis may be anticipated after vocal cord procedures or biopsies.
(2) Phase II
(a) Standard phase II activities as previously described
(b) Discharge instructions
(i) Avoid throat clearing.
(ii) Start bland and soft diet when gag reflex returned.
(iii) Avoid straining or lifting.
(iv) Voice rest as directed by physician
(v) Avoid whispering.
g. Psychosocial concerns
(1) Anxiety related to diagnostic findings
(2) Anxiety related to vocalization changes
h. Complications
(1) Vocal cord trauma and paralysis
(2) Laryngospasm
3. Phonosurgery
a. Purpose
(1) To improve voice quality and vocal cord mobility
b. Description
(1) Insertion of Silastic shim or prosthesis to maintain vocal cord position
(a) Type I
(i) Improves or changes voice quality
(b) Types II and III
(i) Improves or changes pitch
(ii) Alters vocal cord tension
c. Indications
(1) Vocal cord paralysis caused by:
(a) Trauma
(b) Neoplasms
(c) Thyroidectomy
(d) Mechanical dysfunction
d. Preoperative concerns
(1) Discuss expected postoperative events.
(2) Assess quality of patient’s voice.
e. Intraoperative concerns
(1) Performed under local anesthesia with light sedation to allow patient to speak as a test of voice quality
(2) Voice quality tested as shim or prosthesis manipulated to find best position to reapproximate vocal cords
f. Postanesthesia priorities
(1) Phase I
(a) Most patients have minimal sedation; may bypass phase I.
(2) Phase II
(a) Standard phase II activities as previously described
(b) Provide alternate means of communication for patient (e.g., magic slate, pen and paper, communication board) to allow patient to rest voice.
(c) Observe for laryngeal edema.
(d) Discharge instructions
(i) Voice rest as directed by physician
(ii) Avoid whispering.
g. Psychosocial concerns
(1) Speech therapy may be needed to improve quality of voice.
h. Complications
(1) Airway edema
(2) Infection
(3) Need for revision surgery
4. Laryngectomy
a. Purpose
(1) Removal of larynx
b. Description
(1) Types
(a) Hemilaryngectomy
(i) Removal of false vocal cord, arytenoids, and one side of thyroid cartilage
(ii) Patient has hoarse voice postoperatively.
(b) Supraglottic laryngectomy
(i) Removal of laryngeal tissues and structures above the epiglottis, hyoid bone, and false vocal cords
(ii) Normal to near-normal voice postoperatively
(c) Total laryngectomy
(i) Removal of larynx, hyoid bone, laryngeal muscles, and preepiglottic space
(ii) Permanent stoma
(iii) Loss of natural voice postoperatively
c. Indications
(1) Malignant neoplasm
d. Preoperative concerns
(1) Discuss expected postoperative events.
(2) Discuss method to be used for communication in postoperative period.
(3) Patients with the presenting disorder of laryngeal neoplasms may have other chronic health conditions (e.g., smoking, alcohol abuse, diabetes, pulmonary disease; adjust planned interventions accordingly).
e. Intraoperative concerns
(1) May be lengthy procedures; provide attention to patient positioning to avoid pressure injury.
(2) May involve multiple specimens and frozen sections
(3) May be combined with tracheoesophageal puncture to allow for postprocedure speech prosthesis
(a) Creates small fistula from superior wall of trachea to proximal wall of esophagus
(b) Postoperative catheter inserted to maintain integrity of passage; after healing, silicone voice prosthesis with one-way valve is inserted.
f. Postanesthesia priorities
(1) Phase I
(a) Standard phase I activities as previously described
(b) Elevate head of bed at least 30° to minimize edema; clarify positioning with surgeon for specific instructions.
(c) Provide alternate means of communication for patient (e.g., magic slate, pen and paper, communication board).
(d) Frequent oral care when patient awake and alert
(e) Promote coughing and deep breathing.
(2) Phase II
(a) May be transferred to ICU if patient has concomitant health problems; otherwise may be transferred to medical-surgical nursing unit
(b) Discharge instructions
(i) Discuss need for humidification.
(ii) Teach stoma care to patient, family, and/or caregivers.
g. Psychosocial concerns
(1) Depression related to alteration in body image and communication difficulties
(2) Esophageal or electronic speech (i.e., from mechanical larynx) may be difficult to understand.
(3) Patient will require speech rehabilitation.
(4) Provide referral to support groups (American Cancer Society, Lost Cord Club, etc.).
h. Complications
(1) Hemorrhage
(2) Pharyngocutaneous fistula
(3) Pneumothorax
F. Neck
1. Neck dissection
a. Purpose
(1) To remove cancerous and metastatic tissue and lymph nodes from the neck
b. Description
(1) Types
(a) Radical: removal of lymph nodes, soft tissue, sternocleidomastoid muscle, eleventh cranial nerve, and internal jugular vein
(b) Modified radical: removal of soft tissue of neck and lymph nodes with preservation of other structures
c. Indications
(1) Malignant neoplasms
(2) Prophylaxis against metastasis
d. Preoperative concerns
(1) Discuss expected postoperative events.
(2) Patients often have other preexisting health concerns (see Laryngectomy, section III.E.4.d).
e. Intraoperative concerns
(1) Usually combined with laryngectomy procedures
(2) May be lengthy procedures; provide attention to patient positioning to avoid pressure injury.
(3) May involve multiple specimens and frozen sections
f. Postanesthesia priorities
(1) Phase I
(a) See information on laryngectomy (section III.E.4.f).
(b) Support affected arm on pillow to minimize pain and edema.
(2) Phase II
(a) May be transferred to ICU for observation; otherwise will be transferred to general medical-surgical nursing unit
g. Psychosocial concerns
(1) Unacceptable cosmetic appearance (radical dissection)
(2) Depression related to appearance, concern about prognosis
(3) Physical therapy required to regain strength in remaining neck muscles
h. Complications
(1) Hemorrhage
(2) Impaired circulation to tissue flaps
(3) Pneumothorax
(4) Chyle (e.g., fluid composed of lymph and small fat globules) leak
(5) Infection
2. Thyroidectomy
a. Purpose
(1) To remove a hypertrophied thyroid gland and/or parathyroid glands
(2) Removal of thyroid tumors and nodules
b. Description
(1) Excision of thyroid gland and parathyroid gland via a neck incision
c. Indications
(1) Tumor and nodules
(2) Hyperthyroidism (Graves’ disease)
(3) Hashimoto’s thyroiditis
d. Preoperative concerns
(1) Discuss expected postoperative events.
(2) Hypothyroidism may predispose patient to skin breakdown and edema.
e. Intraoperative concerns
(1) May be performed as video-assisted procedure using harmonic scalpel
(2) Positioning is critical to expose gland. Neck is hyperextended with head resting on headrest.
(3) Electrocautery not used in vicinity of recurrent laryngeal nerve to avoid thermal damage to nerve
f. Postanesthesia priorities
(1) Phase I
(a) Standard phase I activities as previously described
(b) Elevate head of bed at least 30° to minimize edema; clarify positioning with surgeon for specific instructions.
(c) Obtain tracheostomy tray at bedside if signs and symptoms indicate respiratory distress.
(d) Encourage deep breathing.
(e) Observe for low calcium levels (have calcium gluconate at bedside).
(i) Cramping, tingling of extremities
(ii) Numbness around lips
(f) Monitor for thyroid storm.
(i) Rare if patient is euthyroid (normal) before surgery
(ii) Characterized by increased heart rate, increased blood pressure, heat intolerance, high oxygen consumption, sweating
(iii) Treated with beta-blockers, usually propranolol
(2) Phase II
(a) Standard phase II activities as previously described; will generally be admitted for 24-hour observation
(b) Discharge instructions
(i) Discuss symptoms of hypocalcemia and instruct patient to notify surgeon if these occur.
(ii) Keep all follow-up appointments; laboratory monitoring of thyroid levels and hypothyroidism imperative
(iii) Encourage range-of-motion exercises for neck.
(iv) Soft diet until dysphagia eases
(v) Avoid heavy lifting and straining.
(vi) Voice rest as directed by surgeon
g. Psychosocial concerns
(1) Alteration in body image due to neck scar
h. Complications
(1) Recurrent laryngeal nerve injury
(2) Hemorrhage
(3) Hypoparathyroidism
BIBLIOGRAPHY
1. Cummings, C.W.; Flint, P.W.; Haughey, B.H.; et al., Cummings: Otolaryngology: Head & neck surgery. ed 4 ( 2005)Mosby, Philadelphia.
2. Drain, C.; Odom-Forren, J., Perianesthesia nursing: A critical care approach. ed 5 ( 2009)Saunders, St Louis.
3. Ignatavicius, D.; Workman, L., Medical surgical nursing: Critical thinking for collaborative care. ed 5 ( 2006)Saunders, St Louis.
4. Linton, A., Introduction to medical surgical nursing. ed 4 ( 2007)Saunders, St Louis.
5. Rothrock, J.C., Alexander’s care of the patient in surgery. ed 13 ( 2007)Mosby, St Louis.
6. Patton, K.; Thibodeau, G., Anatomy & physiology. ed 7 ( 2010)Mosby, St Louis.



