Defibrillation (Internal)
Defibrillation (Internal)
PREREQUISITE NURSING KNOWLEDGE
• Understanding is needed of cardiovascular anatomy and physiology, principles of cardiac conduction, dysrhythmia interpretation, and electrical safety.
• Advanced cardiac life support knowledge and skills are needed.
• Clinical and technical competence in the use of the defibrillator is needed.
• Knowledge of aseptic and sterile technique is necessary.
• Knowledge of internal paddle placement and energy requirements for internal defibrillation is needed.
• Emergent open sternotomy or thoracotomy precedes internal defibrillation (see Procedures 43 and 44).
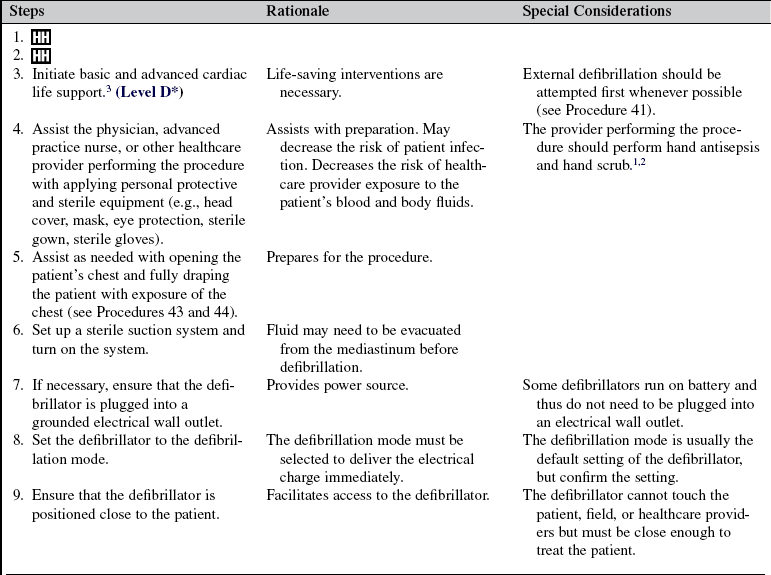
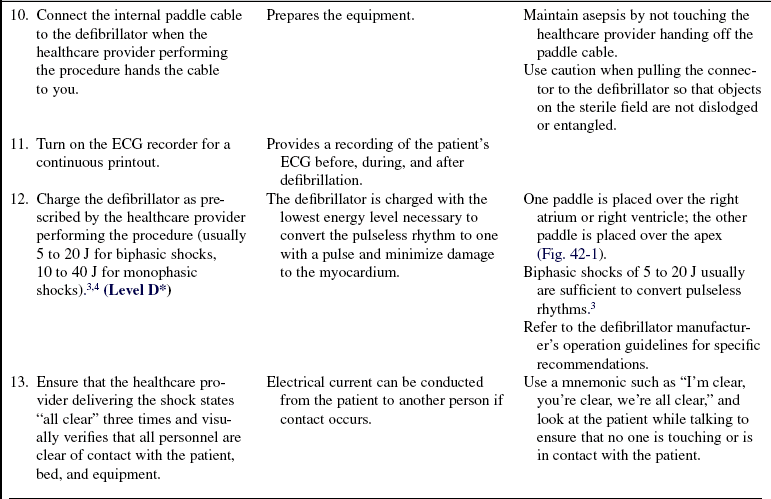
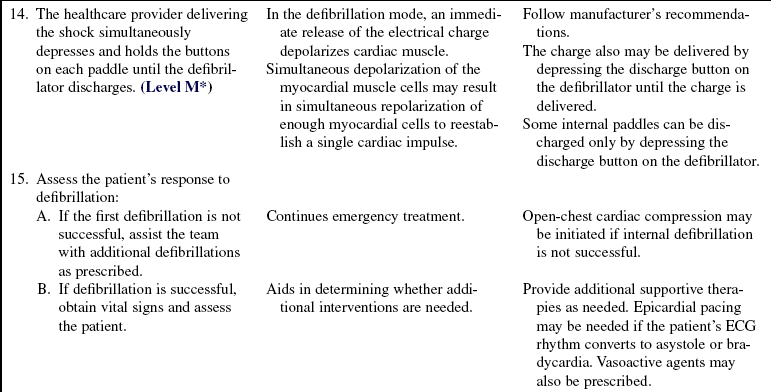
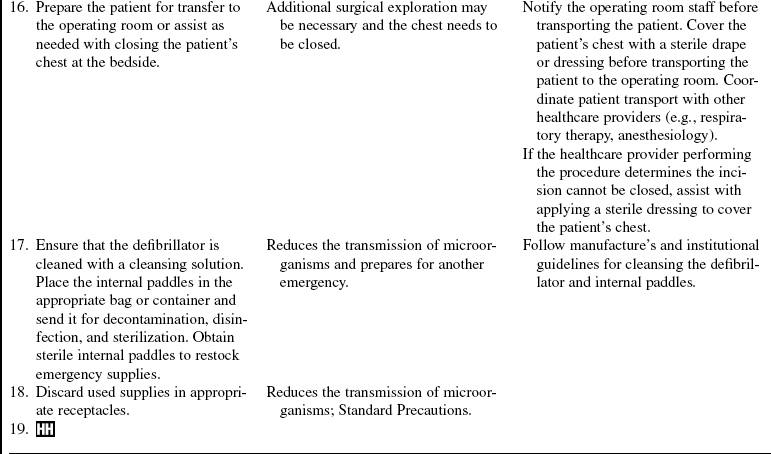
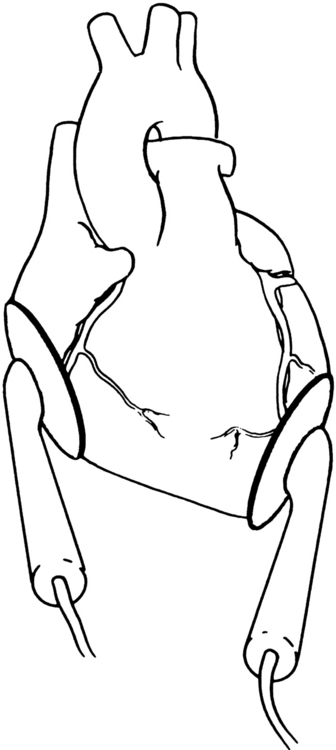
• Internal paddle placement should ensure that the axis of the heart is situated between the sources of current.
• Energy requirements for internal defibrillation usually range from 5 to 20 J for biphasic shocks and 10 to 40 J for monophasic shocks.3,4
EQUIPMENT
• Surgical head cover, mask, eye protection, sterile gown, sterile gloves
• Open sternotomy or thoracotomy tray
• Sterile internal paddles (ensure compatibility with the defibrillator)
• Defibrillator with electrocardiogram (ECG) oscilloscope and recorder
• Antiseptic solution (e.g., 2% chlorhexidine-based preparation)
• Large sterile suction catheter, tubing, suction canisters, suction regulator, and suction source
• Flow meter for oxygen administration
• Bag-valve device with mask capable of delivering 100% oxygen and at least 500-mL volumes
• Intravenous access and IV fluids (e.g., 500 mL of normal saline)
PATIENT AND FAMILY EDUCATION
• Teaching may need to be performed after the procedure.  Rationale: Internal defibrillation usually is performed in the face of sudden hemodynamic collapse.
Rationale: Internal defibrillation usually is performed in the face of sudden hemodynamic collapse.
• Explain to the family the need for internal defibrillation.  Rationale: This information keeps the family informed.
Rationale: This information keeps the family informed.
• Discuss with the patient and family the need for follow-up electrophysiologic studies (EPS), as applicable.  Rationale: This discussion enables the patient and family to understand the importance of EPS for diagnosis and treatment of the dysrhythmia and monitoring both the effects of the dysrhythmia and efficacy of the treatment plan.
Rationale: This discussion enables the patient and family to understand the importance of EPS for diagnosis and treatment of the dysrhythmia and monitoring both the effects of the dysrhythmia and efficacy of the treatment plan.
• Explain to the patient and family the underlying disease pathology.  Rationale: This explanation assists the patient and family with understanding the cause of the symptoms and the rationale for diagnostics, treatments, ongoing monitoring, and both expected and unexpected outcomes.
Rationale: This explanation assists the patient and family with understanding the cause of the symptoms and the rationale for diagnostics, treatments, ongoing monitoring, and both expected and unexpected outcomes.
• Explain to the patient and family the signs and symptoms of hemodynamic compromise associated with the cardiac dysrhythmia.  Rationale: This explanation helps the patient and family to recognize when the patient needs to contact healthcare providers.
Rationale: This explanation helps the patient and family to recognize when the patient needs to contact healthcare providers.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess for dysrhythmias, especially ventricular ectopy.  Rationale: Ventricular dysrhythmias may precede ventricular tachycardia and ventricular fibrillation.
Rationale: Ventricular dysrhythmias may precede ventricular tachycardia and ventricular fibrillation.
• Assess vital signs when dysrhythmias occur.  Rationale: This assessment provides data about the patient’s response to dysrhythmias.
Rationale: This assessment provides data about the patient’s response to dysrhythmias.
• Assess for pulseless ventricular tachycardia or ventricular fibrillation.  Rationale: Assessment determines the need for resuscitation, which may include internal cardiac defibrillation. If immediate intervention is not initiated, return of circulation may not be possible.
Rationale: Assessment determines the need for resuscitation, which may include internal cardiac defibrillation. If immediate intervention is not initiated, return of circulation may not be possible.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Place the patient in a flat supine position.  Rationale: This position provides the best access during the procedure and during intervention for management of adverse effects.
Rationale: This position provides the best access during the procedure and during intervention for management of adverse effects.
• Remove all metallic objects from the patient.  Rationale: Metallic objects are conductors of electrical current and may cause burns.
Rationale: Metallic objects are conductors of electrical current and may cause burns.
• Prepare the patient’s skin with antibacterial solution and drape the patient.  Rationale: This preparation decreases the potential for infection.
Rationale: This preparation decreases the potential for infection.
• Administer sedation and analgesia as prescribed.  Rationale: Promotes patient comfort during the procedure.
Rationale: Promotes patient comfort during the procedure.
• Assist with maintaining an airway and ventilation before the initiation of the procedure.  Rationale: The patient’s airway is protected and maintained, and a means for adequate ventilation and oxygenation is provided.
Rationale: The patient’s airway is protected and maintained, and a means for adequate ventilation and oxygenation is provided.
References
1. AORN, Association of periOperative Registered NursesPerioperative standards and recommended practices. Denver: AORN, 2008.
2. Phillips, N. Berry & Kohn’s operating room technique,, ed 11. St Louis: Mosby; 2007.
![]() 3. Soar, J, et al, European Resuscitation Council guidelines -for resuscitation 2005 section 7. cardiac arrest in special circumstances. Resuscitation. 2005; 67(Suppl 1):S135–S170.
3. Soar, J, et al, European Resuscitation Council guidelines -for resuscitation 2005 section 7. cardiac arrest in special circumstances. Resuscitation. 2005; 67(Suppl 1):S135–S170.
![]() 4. Winterhalter, M, et al. Effectiveness and safety of internal rectilinear biphasic versus monophasic defibrillation in -patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth. 2005; 19(6):739–745.
4. Winterhalter, M, et al. Effectiveness and safety of internal rectilinear biphasic versus monophasic defibrillation in -patients undergoing cardiac surgery. J Cardiothorac Vasc Anesth. 2005; 19(6):739–745.