CHAPTER 41. Oral/Maxillofacial/Dental Care
Denise O’Brien
OBJECTIVES
At the conclusion of this chapter, the reader will be able to:
1. Describe anatomy and physiology of oral cavity pertinent to the patient undergoing oral and maxillofacial procedures.
2. Identify assessment parameters for patients undergoing oral and maxillofacial operative procedures.
3. Define nursing care priorities in each postanesthesia phase.
4. Describe patient education after oral and maxillofacial procedures related to diet, pain management, oral care, activity, and follow-up.
I. OVERVIEW
A. Care of the oral or maxillofacial surgical patient presents many challenges.
1. Patients may experience feelings of suffocation.
a. Procedure may prevent normal breathing patterns (inability to breathe through mouth and/or nose).
2. Continuous reassurance and explanations assist the patients in understanding they are not in any danger.
3. Astute assessment skills are necessary.
a. Compromise of the airway can occur at any time.
b. Immediate corrective actions needed
II. ANATOMY AND PHYSIOLOGY
A. Mouth and oral cavity include the following structures:
1. Lips, teeth, gums, buccal mucosa, tongue, palate (hard and soft), tonsils, pharynx, temporomandibular joints (TMJs) (Figure 41-1)
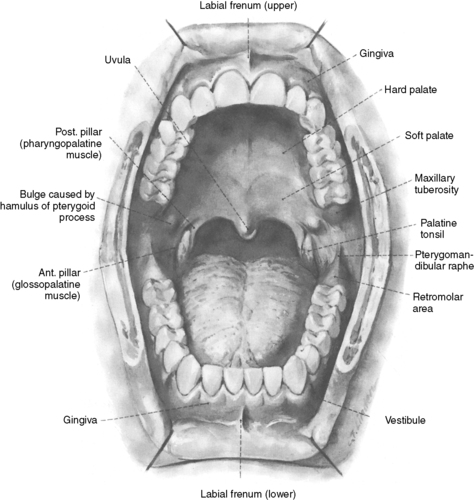 |
| FIGURE 41-1 ▪
The oral cavity.
(From Massler M, Schour I: Atlas of the mouth in health and disease, 1958, by permission of the American Dental Association, Chicago.)
|
B. Oral cavity is bounded by the jawbones and associated structures (muscles and mucosa) (Figures 41-2 and 41-3).
1. Includes
a. Cheek
b. Palate
c. Oral mucosa
d. Glands whose ducts open into the cavity
e. Teeth
f. Tongue
2. Except for the teeth, interior of mouth covered with mucous membrane, lined with salivary glands
a. Secrete saliva
b. Aid in first step of food digestion
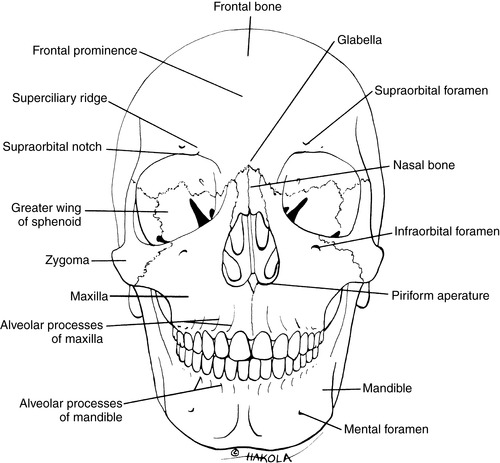 |
| FIGURE 41-2 ▪
The skull, anterior view.
(From Ferraro JW: Fundamentals of maxillofacial surgery, New York, 1997, Springer-Verlag.)
|
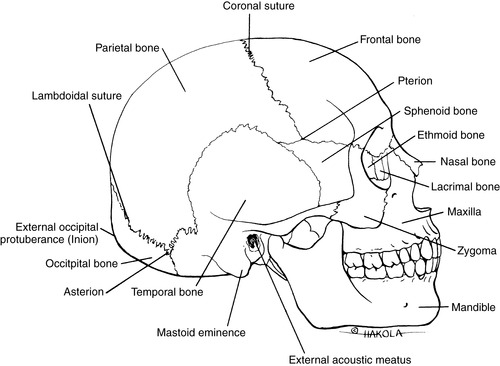 |
| FIGURE 41-3 ▪
Lateral view of the skull.
(From Ferraro JW: Fundamentals of maxillofacial surgery, New York, 1997, Springer-Verlag.)
|
C. Oral cavity forms beginning of the digestive system
1. Chewing occurs.
2. Site of the organs of taste
3. Mouth is entrance to the body for food, occasionally air.
4. Major organ of speech and emotional expression
D. Associated structures
1. Buccal: pertaining to or directed toward the cheek
2. Tooth:
a. Hard calcified structure set in the alveolar processes of the mandible and maxilla
b. Mastication of food
3. Gingiva: mucous membrane (the gum) surrounding the teeth
a. Covers the tooth-bearing border of the jaw
b. Overlies crowns of unerupted teeth
c. Encircles the necks of erupted teeth
d. Supporting structure for subjacent tissues
4. Mandible:
a. Horseshoe-shaped bone forming the lower jaw
b. Largest and strongest bone of the face
c. Articulates with skull at TMJs
5. Maxilla
a. Irregularly shaped bone that forms the upper jaw
b. Two identically shaped bones that are considered one
(1) Assists in the formation of the floor of the orbits, part of the lateral walls and floor of the nasal cavity, and the palate; contains the maxillary sinuses and tear ducts, which drain into the nasal cavity
(2) Supports the upper teeth
c. Described as the architectural key of the face; touches all facial bones, including the mandible, through the contact of upper and lower teeth
6. Palate—the roof of the mouth consists of:
a. Hard palate
(1) The rigid anterior portion
(2) Formed by the maxillae and the palatine bones
(3) Covered by mucous membrane
(4) Forms a bony partition between the oral and nasal cavities
(5) Hinged to the soft palate
b. Soft palate
(1) Posterior, fleshy part of the palate
(2) Arch-shaped muscular partition between the oropharynx and nasopharynx
(3) Lined by mucous membrane
(4) Flanked by tonsils
(5) Uvula is in the middle of the soft palate—a fleshy projection pointing down to the tongue.
(a) Forms seal posteriorly with the pharynx to help direct food to the esophagus and air to the trachea
(b) Critical to the development of normal speech patterns
7. Tongue
a. Movable muscular organ on the floor of the mouth
b. Accessory structure of the digestive system
c. Composed of skeletal muscle covered with mucous membrane
d. Location of organs of taste
e. Aids in chewing, swallowing (deglutition), cleansing tooth surfaces, and the articulation of sound (phonetics)
8. Nerves (Figure 41-4)
a. Sensation supplied to upper teeth and gingival by
(1) Maxillary division of the trigeminal nerve (cranial nerve V)
(a) Posterior superior alveolar
(b) Middle superior alveolar
(c) Anterior superior alveolar
b. Mandibular division gives off
(1) Lingual nerve (sensation of anterior two thirds of tongue, the floor of mouth, gums)
(2) Inferior alveolar nerve (sensation of premolar, molar teeth of mandible)
(3) Mental nerve (sensation of the lower lip and chin)
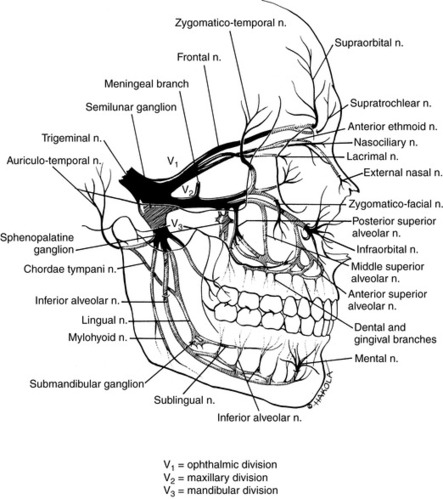 |
| FIGURE 41-4 ▪
The trigeminal nerve (cranial nerve V).
(From Ferraro JW: Fundamentals of maxillofacial surgery, New York, 1997, Springer-Verlag.)
|
9. TMJ: bicondylar joint formed by
a. Head of the mandible
b. Mandibular fossa
c. Articular tubercle of the temporal bone
III PREANESTHESIA ASSESSMENT AND PARAMETERS SPECIFIC TO PROCEDURES
A. Examination
1. Inspection and palpation of greatest use
a. Head and neck
(1) General appearance
(2) Facial appearance
(3) Trismus (limited degree of mouth opening)
(4) Neck lumps
(5) Gross facial swelling
(6) Skin color and texture
b. Intraoral
(1) Tongue: size, mobility, color, and texture
(2) Oral mucosa (palate, cheeks, labial mucosa, floor of mouth): examination for changes in color, texture, ulcers, lumps
(3) Alveolar ridges and gingivae: color, texture, gingival recession, ulcers, and lumps
(4) Teeth: number, position, restorations, crowns, caries, cracked, mobile and missing teeth, exposed structure
B. Increased risk associated with history or need to alter perioperative management
1. Cardiac: may require antibiotic prophylaxis
a. Endocarditis
b. Heart transplant
c. Valve implants
2. Implants: antibiotic prophylaxis may be needed
a. Joints (major replacements)
b. Grafts of artificial materials
3. Coagulation and bleeding disorders
a. Factor VIII deficiency (hemophilia)
b. Von Willebrand’s disease: following may be given just before procedure begins:
(1) Factor VIII
(2) Synthetic factor VIII
(3) Aminocaproic acid (EACA [Epsilon-aminocaproic acid] or Amicar)
(4) DDVAP (desmopressin acetate)
c. Anticoagulant therapy
(1) Coagulation testing may be required (prothrombin, partial thromboplastin time, platelet count) to determine coagulation status before proceeding with elective surgery.
4. Immunocompromised patient or immune disorders
a. Human immunodeficiency virus, acquired immunodeficiency syndrome
b. Patient with history of organ transplant
c. Universal precautions should be used with every patient.
d. Immunocompromised patient may require special care (isolation, scheduling, altered medication regimen).
5. Patients with cancer receiving radiation therapy to the head and neck region
a. Decreased salivary flow secondary to salivary gland atrophy requires saliva substitutes and aggressive anticaries management with
(1) Custom trays
(2) Topical fluoride applications
(3) Immaculate oral hygiene
b. Extractions usually completed before initiation of therapy to decrease the risk of development of osteoradionecrosis
(1) Debilitating complication
(a) Leaves a patient with painful exposed bone in the oral cavity
(b) Can progress to
(i) Pathological fractures
(ii) Recurrent infections
(iii) Raining sinus tracks
c. Hyperbaric oxygen treatment is indicated for surgical procedures if previous radiation dose totals >4500 cGy. (This is still used in some centers but has fallen out of favor because of poor efficacy and lack of literature supporting a benefit.)
6. Trauma
a. Edema present
(1) Recent injury
(2) May delay operative repair until edema diminishes
b. Disfigurement: may be significant and emotionally disturbing to patient and others
7. Chronic pain
a. Pain tolerance alterations
b. Chronic analgesic use may alter postoperative analgesic management.
8. Nutritional status changes
a. Difficulty chewing, swallowing
b. Pain may interfere with ability to eat and meet caloric demands and nutritional requirements.
9. Developmentally challenged
a. Potential behavioral problems (combative, disruptive, abusive)
b. Legal authorization appropriately obtained before treatment commences
C. Airway status evaluation
1. Evaluation of airway for ease of intubation in oral or maxillofacial surgery
a. Mobility of the neck—ability to touch chin to chest and each shoulder; flex and extend
b. Position of the trachea relative to the mandible—distance from thyroid cartilage to anterior bony chin; at least 6.5 cm acceptable
c. Ability of the patient to open the mouth—at least 3.6 cm in adults desirable
d. Structures visualized when the patient opens the mouth and vocalizes “ahh…”—see the uvula and surrounding pharyngeal structures.
D. Determine the educational needs of patient and caregiver.
1. Oral care, analgesia, preoperative anxiety
2. Discharge planning
IV INTRAOPERATIVE PRIORITIES
A. Anesthesia choice: fit of the teeth is one of the best templates a surgeon can use to restore the original form of patient’s face.
1. General
a. Nasal intubation desired for unobstructed visualization of orofacial structures
b. Allows reconstruction of the upper and lower jaws to be guided by the patient’s occlusion
2. Sedation and analgesia with local anesthesia
a. Midazolam, ketamine (glycopyrrolate to decrease oral secretions)
(1) Less risk of respiratory depression
(2) Reduced emergence delirium after ketamine with midazolam
b. Benzodiazepine with fentanyl
(1) Oxygen recommended when used with local anesthesia
(2) May use methohexital or propofol for additional sedation
3. Local anesthesia used alone for minor oral procedures or used as an adjunct during general anesthesia
a. Minimizes immediate postoperative pain
b. Minimizes bleeding in operative field
c. Helps separate tissue planes to ease dissection
d. Allows for less anesthetic agent because of reduced surgical stimulus
B. Intraoperative concerns
1. Hemostasis and intraoral bleeding
a. Hemostatic agent may be used.
b. Gelfoam, Surgicel, Avitene, topical thrombin, bone wax (for bone bleeders), Tisseel (fibrin sealant)
2. Airway
a. Loss of reflexes with excessive sedation
b. Positioning of endotracheal tube, potential displacement
c. Foreign body aspiration
V. POSTANESTHESIA PRIORITIES
A. Phase I
1. Airway
a. Spontaneous, unassisted breathing
b. Adjunct in place: nasal trumpet, oropharyngeal airway
c. Endotracheal tube: nasal insertion (most common)
d. Observe for respiratory complications.
2. Hemodynamic stability
a. Vital signs stable, consistent with baseline
b. Observe for cardiovascular complications.
3. Bleeding
a. Hemostasis may be difficult to obtain.
b. Risk for hemorrhage
c. Increases risk of nausea and vomiting
(1) Swallowed blood may precipitate nausea and vomiting from irritating effect of blood in stomach.
4. Report from anesthesia, oral surgeon, perioperative nurse (in addition to routine information)
a. Implants and prostheses inserted
b. Splints: location, type
c. Oral packing: location, plan for removal
d. Oral sutures: location, extreme care when suctioning
e. Maxillomandibular fixation (MMF)/intermaxillary fixation (IMF)—wired jaws
(1) Wire cutters and scissors immediately available
(2) Clear instructions from surgeon when appropriate to cut fixation wires and what wires to cut
(3) Usually cut for vomit and for respiratory distress (in extreme cases only)
5. Discomfort
a. Maximum pain intensity occurs about 3 hours after surgery: begin analgesics intraoperatively or immediately postoperatively.
b. Long-acting local anesthetic infiltrated into operative site; usually bupivacaine with epinephrine to provide 8 to 12 hours of analgesia
c. Opioids: decreasing use in ambulatory oral and maxillofacial surgery because increased use of nonsteroidal anti-inflammatory drugs (NSAIDs; ketorolac)
d. NSAIDs: ketorolac may provide superior analgesia after extractions.
6. Drainage from mouth
a. Position to facilitate drainage of saliva, bloody secretions.
b. Drooling or excessive salivation and unable to swallow (reflex absent or excessive pain)
c. Suction as needed with soft catheter.
7. Dressing
a. No dressing when incisions are intraoral
b. Internal dressing may be moistened gauze sponge.
(1) Best left with a “tail” hanging out of the patient’s mouth when the patient is obtunded.
(2) Tail facilitates removal and identification of potential airway obstruction in the early stages of emergence from anesthesia.
c. External dressing
(1) Pressure chin strap (Jobst type)
(2) Foam tape
(3) Head wrap with fluffs and cling wrap generally for 24 hours
8. Edema
a. Can be significant, especially in longer procedures
b. Position with head of bed elevated 30 °.
c. Administer steroid if ordered; continued controversy regarding effectiveness in reducing inflammatory reaction.
d. Ice packs may help reduce blood flow to operative site and subsequent inflammatory response.
(1) Check with surgeon before applying.
(a) May actually increase blood flow (rebound effect after ice pack removed)
(b) Can also be damaging to flaps through its vasoconstrictive effects
(c) Apply for 20 minutes on, 20 minutes off.
9. Fluids and nutrition
a. Clear to full liquid, high-caloric diet as tolerated and ordered
b. Do not force fluids, especially when nausea and vomiting present.
c. Causes of nausea and vomiting
(1) Opioid analgesics
(2) Blood in stomach
(3) Starvation leading to weakness, low blood sugar levels
d. Hydrate with intravenous fluids (replacement and maintenance).
(1) Lactated Ringer’s (Hartmann’s)
(2) Dextrose-containing solutions
e. When nausea and vomiting present
(1) Administer antiemetics as ordered; determine whether antiemetic prophylaxis given.
(2) Commonly used (see Chapter 25 for discussion on antiemetics)
(a) 5-hydroxytryptamine-3 (5-HT 3) serotonin antagonists
(i) Ondansetron (Zofran)
(ii) Dolasetron (Anzemet)
(iii) Granisetron (Kytril)
(b) Dexamethasone (Decadron)
(c) Diphenhydramine (Benadryl)
(d) Prochlorperazine (Compazine)
(3) Important not to ignore vomiting, as the expelled material will be forced against suture lines and risk their rupture
10. Reaction to local anesthetics (LAs)
a. What appears to be an allergic reaction to LA may actually be a reaction to preservative methylparaben or sulfite.
b. Allergy to LA rare
c. Traumatic penetration of a nerve (prolonged numbness), vein (hematoma), or artery (systemic toxic effects)
d. Systemic (cardiac) reactions to epinephrine (used to minimize bleeding) in LA, rather than LA itself
e. Toxicity caused by overdose leads to excitation of central nervous system (CNS) followed by
(1) Profound CNS depression
(2) Cardiovascular collapse
(3) Possible death
11. Oral hygiene
a. Take care not to disrupt clot.
(1) Gently swab the oral cavity.
(2) Hold saline rinse for 8 to 12 hours postprocedure.
b. Lubricate lips with
(1) Petroleum jelly or emollient cream
(2) Steroid (0.5% hydrocortisone) lip cream—for long procedures
(3) Expectance of significant edema of lips
12. Antibiotic as ordered
a. Common after trauma
b. Patients with cardiac valvular disease
c. History of rheumatic fever
d. Implants
e. Oral cavity laden with bacteria
(1) Bacteria enter the bloodstream through oral incisions
(2) Traumatic lacerations
f. Infections can lead to
(1) Loss of bone and teeth
(2) Distributive shock (septic)
(3) Damage to heart valves
(4) Endocarditis
(5) Loss of implants
(6) Scarring
(7) Large vessel complications (carotid erosion or venous thrombosis)
13. Provide patient with means of communication while in PACU.
a. Bell
b. Writing tools
(1) Pen or pencil, paper pad
(2) Magic slate and stylet
(3) Dry-erase board and marker
14. Reasons for admission after outpatient operative procedure
a. Airway obstruction
b. Unanticipated MMF/IMF
c. Severe postoperative nausea and vomiting
d. Excessive blood loss
e. Severe pain
f. Persistent bleeding from extraction sites
g. Slow recovery from anesthesia
B. Phase II
1. Operative site
a. Continued bleeding: tamponade by biting saline-moistened gauze for approximately 30 minutes
b. Epinephrine-soaked gauze or packs not recommended; rebound vasodilation can occur when a vasoconstrictor used, leading to increased bleeding.
c. Pressure packs may need to be maintained for 2 hours or some specified time postprocedure—determine appropriate time for removal and discharge.
2. Discomfort
a. Oral analgesic medications initiated in preparation for discharge home
(1) May have started in phase I
(2) Determine effectiveness of medication before patient discharged home on same analgesic.
(3) If ineffective, may need prescription changed or other follow-up (see Chapter 26 for more information on pain and comfort)
b. Continue ice pack as ordered.
3. Oral care
a. Oral suctioning initiated by patient when appropriate and patient capable
b. Begin oral fluids if desired and not already started in phase I.
c. Avoid extremes of heat.
4. Education (Box 41-1)
a. Includes patient, family, responsible adult companion
b. Instructions
(1) Oral hygiene
(2) Avoid temperature extremes in food and beverages.
(3) Avoid sucking motion, which creates negative pressure (i.e., do not use a straw, do not spit).
(4) Care of bands and wires
(5) For patient with MMF/IMF
(a) How and when to cut wires
(i) Airway distress
(ii) Vomiting
(6) Patients should keep wire cutters with them at all times.
(a) Transport should not be permitted without wire cutters.
(7) Pain-relief alternatives
(a) Dental wax may be used to protect oral mucosa and decrease irritation and discomfort from protruding wires or metal bands.
BOX 41-1
KEY PATIENT EDUCATIONAL OUTCOMES
Phase I: Patient Will:
Express feelings of lessened anxiety.
Describe minimal to tolerable pain.
Request analgesic to manage pain.
Perform oral suctioning and handle oral secretions unassisted.
Be able to communicate with nurse without using verbal skills.
Phase II: Patient Will:
Tolerate discomfort following administration of oral analgesics.
Describe oral hygiene following instruction with caregiver.
Demonstrate use of gauze sponge for tamponade of bleeding.
Demonstrate safe, gentle, and effective oral suctioning.
Verbally describe wire cutting (patients with MMF/IMF) with caregiver.
Progress to upright position with minimal orthostatic effects: dizziness, lightheadedness, nausea.
Discharge: Patient, Family, and Responsible Accompanying Adult Will:
Describe follow-up required.
Identify risks associated with operative procedure: infection, hemorrhage, pain, vomiting.
Describe oral care, activity, medications, and diet.
Demonstrate knowledge of medications (analgesics, antibiotics, antiemetics, etc.) by describing purpose and administration of each medication prescribed.
IMF, Intermaxillary fixation; MMF, maxillomandibular fixation.
C. After discharge
1. Oral hygiene
a. Brushing difficult if not impossible because of swelling and pain
(1) Swelling reaches maximum in 2 to 3 days, subsides gradually.
(2) Rinses may help in reducing swelling.
b. Saline rinses (1 teaspoon table salt in one-half glass hot water) for 2 minutes, three to six times a day, especially after meals
(1) No rinsing for at least 8 to 12 hours after procedure so as not to disturb clot (surgeon may order up to 24 hours before rinsing begins); disruption of the clot may lead to painful “dry socket” (localized osteitis).
(a) Most often develops from second to fifth postoperative day
(b) Chief complaint is pain; also may complain of odor or a bad taste.
(c) Treatment is conservative.
(i) Gentle warm saline irrigation of site
(ii) Sedative
(iii) Dressing over site until patient no longer symptomatic
(2) Antiseptic mouthwashes may also be prescribed.
(a) Most common is chlorhexidine 0.2%.
(b) Held over surgical site for 1 minute, then expectorated
(c) After a rinse, patients should have nothing by mouth for 30 minutes, as the chlorhexidine will bind to oral tissues if not rinsed away and continue to suppress bacterial regrowth.
c. Continued bleeding
(1) Instruct patient to replace gauze sponge over bleeding site and bite firmly for 20 to 30 minutes.
(2) If a bleeding tooth socket, a moist tea bag over the socket may be helpful.
(a) Tannic acid is a local vasoconstrictor.
(3) If bleeding persists, patient needs to be evaluated by surgeon.
2. Nutrition
a. Instruct patient regarding alcohol and smoking avoidance for at least 2 weeks.
b. Diet and food preparation
(1) Avoid hot foods and liquids for first 48 hours (soft and cool diet choices).
(2) Instruct patient to advance to soft foods or pureed diet (nutritional supplement) as tolerated or ordered by surgeon.
c. Encourage fluid intake, especially during hot weather.
3. Vomiting
a. Prepare patient and family for possibility of vomiting swallowed blood; suggest adequately sized receptacle for ride home and at home in case of emesis.
b. Caution patient and caregiver to call surgeon or facility:
(1) If vomiting persists for >6 hours
(2) If continuing to swallow blood: may require evaluation to determine source of bleeding
4. Pain: peaks approximately 12 hours postoperatively
a. Ice packs, heat application especially for TMJ procedures
b. Oral analgesics
(1) Suggest contacting surgeon if pain is not relieved by prescribed analgesics, intolerable, or increasing.
(2) Unrelieved or increasing pain may indicate
(a) Infection
(b) Retained root
(c) Bone
(d) Foreign body
(e) Maxillary sinus problems
c. Alternatives
(1) Dental wax may be applied to wires and bands to reduce mucosal irritation.
(2) Explore with patient and caregiver other potential pain management techniques (see Chapter 26).
5. Wound care
a. See oral hygiene instructions for intraoral incisions.
b. For external incisions
(1) Keep wound clean and dry for minimum of 24 to 48 hours.
(2) May be instructed to remove dressing after 24 to 48 hours
(3) Clean incision with saline or half-strength hydrogen peroxide
(4) Cover with antibiotic ointment.
(5) Observe incision for signs of infection: redness, swelling, drainage.
6. Activity
a. Rest
(1) Limit activity until pain and swelling subside.
(2) Sleep with head elevated on several pillows to reduce swelling and minimize bleeding.
(3) While taking opioid analgesics, avoid
(a) Operating machinery
(b) Driving automobiles
(c) Using sharp or potentially injurious articles
(d) Drinking alcohol
b. Exercise
(1) For first 24 hours, any exercise is discouraged.
(2) Defer vigorous activity; restrict until surgeon allows; may be up to 4 weeks after surgery.
(a) Aerobic activity may increase heart rate and blood pressure, leading to increased bleeding from operative site(s).
7. Follow-up care
a. Arrange for return visit with surgeon in specified time interval.
(1) Patients with drains, MMF/IMF, extensive procedures may require return visit on first postoperative day.
(2) Sutures removed in 5 to 7 days postoperatively
b. Return to work dependent on procedure, patient work
c. Risk for secondary hemorrhage
(1) Seven to 10 days after surgery
(2) Often caused by an infected wound and poor oral hygiene
d. Fever: contact surgeon if temperature greater than 100.4 ° F (38 ° C) or as ordered by surgeon.
VI. COMMON OPERATIVE PROCEDURES (see also Chapters 43 and 45)
A. Arch bars
1. Purpose: used for treatment of avulsed teeth, fractures of the mandible, or maxilla
2. Description: rigid metal bars used to splint and fix the teeth and/or maxilla or mandible; wire ligatures attach the bars to the teeth.
B. Closed reduction of mandibular (jaw) fracture
1. Purpose: used for alignment and stabilization of fractures to allow proper healing
2. Description: Erich-type arch bars ligated to teeth most common method of fixation; MMF (which is synonymous with IMF) using stainless steel loops or elastics for 3 to 8 weeks considered best for providing reduction and fixation
3. MMF/IMF acceptable for ambulatory surgery if there is no gross edema and/or bleeding
4. Postanesthesia priorities
a. Airway
b. Nausea and vomiting
c. Wire cutter at bedside, immediately available
5. Psychosocial concerns
a. Difficulty communicating
b. Dietary modifications
6. Complications
a. Severe airway distress, epistaxis, or emesis requiring wires to be cut
C. Dental examination
1. Purpose: oral cavity inspected and teeth and supporting structures probed for defects, lesions, mobility, and infection
2. Description: visual and instrument methods used for the examination
D. Dental implant
1. Purpose: replace a single missing tooth or multiple missing teeth, lost to injury or other reasons
2. Description: a prosthetic tooth with an anchoring structure surgically implanted beneath the mucosal or periosteal layer or in the bone
E. Dental prophylaxis
1. Purpose: cleansing of teeth (stains, materia alba, calculus, removal of plaque)
2. Description: dental instruments used to clean the teeth
F. Dental restoration
1. Purpose: replacing tooth structure by artificial means
2. Description: reforming lost tooth structure, missing, damaged, or diseased teeth with alloy of silver, gold, or acrylic resin
G. Genioplasty
1. Purpose: operative repair of chin deformities (microgenia, macrogenia, asymmetric chin are a few of the defects)
2. Description: repair done by open bone reduction, augmentation with synthetic or natural materials, or osteotomy with plate and screw fixation
H. Gingivectomy
1. Purpose: to eradicate periodontal infection and reduce the gingival sulcus depth
2. Description: excision of all loose infected and diseased gingival tissue
I. Implants
1. Purpose: used to stabilize or totally support tooth replacements; prostheses may be fixed or fixed and removable.
2. Description
a. Osseointegration screw technique (Branemark)
(1) Titanium screw inserted into jaw bone, grows into the bone (osseointegrates)
(2) After 4 months (mandible) or 6 months (maxilla), attached to and loaded with a prosthesis
b. Transmandibular implant/mandibular staple implant
(1) Consists of a base plate, screws to fix the plate to the mandible, and posts that attach to a bar (Dolder) in the mouth
(2) Lower prosthesis attached to the bar; prosthesis started 4 to 6 weeks after surgery
J. Intraoral biopsy
1. Purpose: removal of abnormal tissue for histopathological examination
2. Description
a. Excisional: complete removal of a lesion with primary closure
b. Incisional: small representative portion of a lesion is removed if the lesion is large and the defect left from its removal could not be closed primarily.
K. Multiple dental extractions
1. Purpose:
a. May follow trauma
b. Significant or recurring infection
c. Nonrestorable teeth
d. Preparation for prosthetic replacement
e. Often done in preparation for
(1) Solid organ transplant
(2) Chemotherapy
(3) Radiotherapy
(4) Large joint replacement
2. Description: surgical removal of teeth
L. Odontectomy: tooth extraction
M. Open reduction and internal fixation of zygomatic fracture
1. Purpose: to realign fractured bone fragments and restore facial contour
2. Description: by using a transconjunctival or lower eyelid subciliary incision with skin muscle flap and orbital floor exploration, the fracture reduced and fixated with wires or microplate system for the infraorbital rim and wires or miniplating fixation of the zygomaticomaxillary buttress
N. Osteotomy
1. Purpose: correct maxillofacial deformities.
2. Description
a. Le Fort osteotomy: osteotomy performed along the classic lines of fracture as described by Le Fort to correct a maxillary skeletal deformity classified as
(1) Le Fort osteotomy I, lower maxillary
(2) Le Fort osteotomy II, pyramidal nasoorbitomaxillary
(3) Le Fort osteotomy III, high maxillary/facial disarticulation (depending upon the location of the deformity)
(4) Maxilla sectioned transversely and repositioned (see Chapter 43)
b. Sagittal split mandibular osteotomy:
(1) Intraoral surgical procedure for correction of retrognathism, prognathism or open bite
(2) Mandibular rami and posterior body sectioned in the sagittal plane
c. Segmental alveolar osteotomy
(1) Intraoral surgical procedure in which segments of alveolar bone containing teeth are sectioned between, and apically to, the teeth for the repositioning of the alveolus and teeth
(2) It may be maxillary or mandibular.
(3) It may be combined with ostectomy.
d. Sliding oblique osteotomy
(1) Oral surgical procedure in which the mandibular ramus is cut vertically from the sigmoid notch to the angle; this facilitates posterior repositioning of the mandible in correction of mandibular prognathism.
(2) May be performed extraorally or intraorally
(3) Similar to vertical osteotomy
e. Vertical osteotomy: oral surgical procedure similar to sliding oblique osteotomy
3. Postanesthesia priorities
a. Airway
b. Bleeding
c. Nausea and vomiting
d. Swelling
e. Pain management
4. Psychosocial concerns
a. Facial swelling distorting appearance
b. Reason for procedure (trauma or cosmetic and functional appearance)
O. Splint
1. Purpose:
a. Stabilize the maxillomandibular position
(1) Secured to the maxilla and mandible
(2) Interlocked
(3) Retain the desired position of the osteotomized units
b. Reduce and stabilize maxillofacial fractures
c. May be used in the interim before MMF/IMF or plate and screw (rigid) fixation
2. Description:
a. Made of acrylic resin or metal
b. Used as space maintainer or fixator; to hold teeth in alignment
c. Temporary, permanent, or removable
P. TMJ arthroscopy
1. Purpose
a. Diagnosis of internal joint pathology
b. Lavage of joint
c. Lysis of adhesions
d. Biopsy of synovial tissue
2. Description: direct visual inspection and examination of interior TMJ structures using an endoscopic instrument
3. Postanesthesia priorities
a. Trismus may be problem.
b. TMJ physiotherapy initiated
c. Provide information on jaw-opening exercises.
4. Psychosocial concerns
a. Chronic pain may be an issue; ongoing assessment and pain management essential.
BIBLIOGRAPHY
1. Booth, P.W.; Schendel, S.A.; Hausamen, J.E., Maxillofacial surgery. ( 2007)Churchill Livingstone, St Louis.
2. Chung, W.L.; Sosovicka, M.F.; Costello, B.J., Contemporary ambulatory anesthesia in oral and maxillofacial surgery. ( 2004)University of Texas Southwestern Medical Center at Dallas, Dallas.
3. Dimitroulis, G., A synopsis of minor oral surgery. ( 1997)Reed Educational and Professional Publishing, Oxford, UK.
4. Donoff, R.B., Massachusetts General Hospital manual of oral and maxillofacial surgery. ed 3 ( 1997)Mosby, St Louis.
5. Dorland’s illustrated medical dictionary. ed 31 ( 2007)WB Saunders, Philadelphia.
6. Ferraro, J.W., Fundamentals of maxillofacial surgery. ( 1997)Springer-Verlag, New York.
7. Hupp, J.R.; Ellis, E.; Tucker, M.R., Contemporary oral and maxillofacial surgery. ( 2008)Mosby, St Louis.
8. Kaban, L.B.; Pogrel, M.A.; Perrott, D.H., Complications in oral and maxillofacial surgery. ( 1997)WB Saunders, Philadelphia.
9. Kwon, P.H.; Laskin, D.M., Clinician’s manual of oral and maxillofacial surgery. ed 3 ( 2001)Quintessence Publishing, Chicago.
10. O’Toole, M.T., Miller-Keane Encyclopedia and dictionary of medicine, nursing, and allied health. ed 7 ( 2003)WB Saunders, Philadelphia.
11. Riden, K., Key topics in oral and maxillofacial surgery. ( 1998)BIOS Scientific, Oxford, UK.
12. Stedman’s medical dictionary. ed 28 ( 2006)Lippincott Williams & Wilkins, Philadelphia.
13. In: (Editor: Yates, C.) A manual of oral and maxillofacial surgery for nurses ( 2000)Blackwell Science, Oxford, UK.



