CHAPTER 40. Ophthalmological Care
Seema Hussain and Kenneth Wichter
OBJECTIVES
At the conclusion of this chapter, the reader will be able to:
1. Identify the important functions of the eye.
2. Describe the structure of the eye.
3. Describe common ophthalmological surgical procedures.
4. List drugs frequently used for ophthalmological surgical procedures.
5. Identify possible complications of ophthalmological surgery.
6. Describe perianesthesia nursing care for the ophthalmological surgery patient.
I. ANATOMY AND PHYSIOLOGY OF THE EYE (Figure 40-1)
A. Orbit
1. Pyramid-shaped bony cavity that functions as protection for the eye
2. Consists of seven fused bones
a. Ethmoid
b. Sphenoid
c. Frontal
d. Lacrimal
e. Zygomatic
f. Palatine
g. Maxilla
3. Orbit contains
a. Eyeball
b. Six extraocular muscles
c. Ophthalmic artery veins
d. Cranial nerves
(1) The second (optic)
(2) Third (oculomotor)
(3) Fourth (trochlear)
(4) Fifth (trigeminal)
(5) Sixth (abducens)
e. Lacrimal gland
f. Lacrimal sac
g. Orbital fascia, fat and ligaments
B. Eyelids are continuous with the conjunctiva lining the inner aspect of the lid
1. Act as protection for
a. Anterior portion of the eyes
b. Epithelium of the lids
2. Spread lubricating solutions over globe
a. Keep eyes moist
b. Prevent evaporation of secretion
3. Eyelashes situated along the margins and act as protective fibers
4. Two muscle groups
a. Orbicularis oculi sphincter responsible for closing eye
b. Levator palpebrae responsible for raising eyelids
c. Movements can be both involuntary and voluntary.
5. Function of the eyelids
a. Cover eyes during sleep
b. Protect eyes from excessive light
c. Protect eye from injury
d. Protect eye from foreign objects
e. Lubricate the anterior surface of the eye
6. Lined with mucous membrane called palpebral conjunctiva
C. Conjunctiva
1. Thin, transparent mucous membrane covering sclera and inner lids
2. Lining upper and lower eyelids—palpebral conjunctiva
3. Extends over sclera to corneal margin—bulbar conjunctiva
4. Function of the conjunctiva
a. Produces the mucin layer of the tear film, reducing the rate of tear evaporation
b. Protects the eye against damage and infection
c. Facilitates movement by moistening the surface of the eye and lids
D. Lacrimal apparatus: produces and drains tears
1. Consists of:
a. Lacrimal gland—located in upper outer aspect of each orbit and produces tears that:
(1) Empty through lacrimal ducts onto conjunctiva of upper lid
(2) Spread across eyeball by blinking
(3) Enter lacrimal puncta
b. Lacrimal puncta—two small openings located in the inner canthus of each upper and lower eyelid
(1) Pass into lacrimal canals, lacrimal sac, nasolacrimal duct, and finally into inferior meatus of the turbinate bone of the nose
c. Lacrimal sac—collects tears
d. Nasolacrimal duct—drains tears from lacrimal sac to nose
2. Tears
a. Contains
(1) Water
(2) Protein
(3) Glucose
(4) Sodium
(5) Potassium
(6) Chloride
(7) Urea
(8) Lysozyme (bacterial enzyme)
b. Purpose of tears
(1) Aid refraction by providing an optically smooth corneal surface
(2) Lubricate the anterior surface of the eye to aid movement
(3) Clean dust particles from the eye
(4) Protect against infection by the action of lysozymes
c. Emotional stimulus of parasympathetic nervous system triggered
E. Muscles controlling the eye (Figure 40-2)
1. Extraocular muscles (six)
a. Attached to outside of eyeball and to bones of the orbit
b. Consist of voluntary skeletal muscle
(1) Four rectus
(a) Superior—oculomotor nerve
(b) Inferior—oculomotor nerve
(c) Medial—oculomotor nerve
(d) Lateral—abducens nerve
(2) Two oblique muscles
(a) Superior—trochlear nerve
(b) Inferior—oculomotor nerve
c. Action
(1) Muscles move eyeball through cranial nerves.
(a) Third (oculomotor)—moves eyeball and upper eyelid
(b) Size of iris (i.e., constriction and dilation of pupil to regulate amount of light admitted)
(c) Control of ciliary muscle to regulate degree of refraction by lens
(d) Fourth (trochlear)—movement of eyeball by superior oblique muscles
(e) Sixth (abducens)—movement of eyeball by lateral rectus muscle
(2) Muscles work in pairs.
(3) Movement caused by:
(a) Increase in tone of one set of muscles
(b) Decrease in tone of antagonistic (opposite set) muscles
2. Movement of upper eyelid
a. Raised (opened) by levator palpebrae superioris muscle
(1) Controlled by cranial nerve III and sympathetic nervous system
b. Closed by orbicularis oculi muscle
(1) Controlled by cranial nerve VII
3. Iris and ciliary muscles
a. Smooth, involuntary muscles
b. Work inside eyeball
(1) Regulate size of pupil
(2) Control shape of lens during accommodation
(3) Controlled through neural network
(a) Optic nerve (cranial nerve II)
(b) Oculomotor nerve (cranial nerve III)
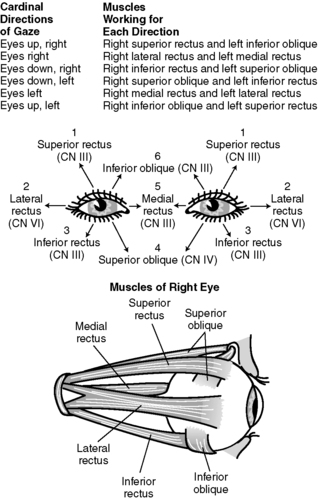 |
| FIGURE 40-2 ▪
The six cardinal directions of gaze and the muscles responsible for each. The six cardinal directions are (1) right, (2) left, (3) up and right, (4) up and left, (5) down and right, and (6) down and left.
(From Black JM, Matassarin-Jacobs E: Medical-surgical nursing clinical management for continuity of care, ed 5, Philadelphia, 1997, WB Saunders, p 936.)
|
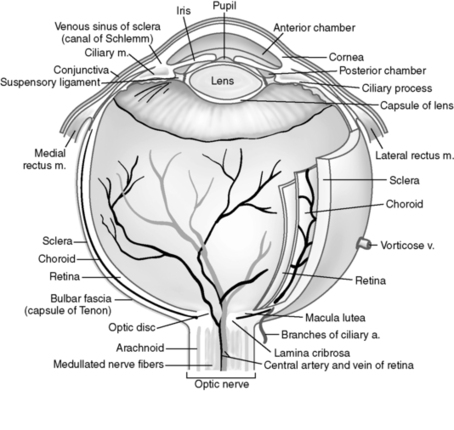 |
| FIGURE 40-1 ▪
Structure of the eyeball.
(From Drain CB, ed: Perianesthesia nursing: A critical care approach, ed 4, St Louis, 2003, WB Saunders, p 453.)
|
F. Globe (eyeball): supported in orbital cavity on a cushion of fat and fascia; composed of three layers
1. External, corneal-scleral layer (fibrous, protects other two layers)
a. Cornea
(1) Anterior, transparent, avascular part of the external layer
(2) Serves as a window through which light rays pass to retina
(3) Supplied by branches of ophthalmic division of fifth cranial nerve
(4) Composed of five layers
(a) Epithelium
(i) Cell layers and nerve endings
(ii) Account for corneal sensitivity
(b) Bowman’s membrane
(i) Composed of connective tissue fibers
(ii) Forms a barrier between trauma and infection
(iii) Does not regenerate if damaged
(iv) Will leave a permanent scar
(c) Stroma
(i) Accounts for 90% of corneal thickening
(ii) Composed of multiple lamellar fibers
(d) Descemet’s membrane
(i) Thin layer between endothelial layer of cornea and substantia propria (fibrous, tough, and transparent main part of the cornea)
(ii) If inflamed, called descemetitis
(iii) If protrudes, called descemetocele
(e) Endothelium
(i) Single layer of hexagonal cells
(ii) Does not regenerate
(iii) Responsible for proper state of dehydration that keeps cornea clear
(iv) Damage causes corneal edema and loss of transparency.
b. Sclera: posterior opaque part of the external layer; tough white outer coat of eyeball
(1) Portion of sclera can be seen through the conjunctiva as the white of the eye.
(2) Made up of collagenous fibers loosely connected with fascia, which receives the tendons of the muscles of the globe
2. Middle layer: middle covering of the eye comprises the choroid, ciliary body, and iris (referred to as uveal tract).
a. Choroid
(1) Most posterior portion of middle coat
(2) Contains many blood vessels; highly vascular
(3) Deeply pigmented
(4) Purpose
(a) Absorbs light rays
(b) Prevents reflection within eyeball
(c) Main source of nourishment to retina (through its blood supply)
b. Ciliary body
(1) Consists of an extension of the choroidal blood vessels, a mass of muscle tissue, and an extension of the neuroepithelium of the retina
(2) Composed of ciliary muscle and ciliary processes
(3) Ciliary muscle
(a) Affects accommodation
(b) Alters shape of lens as needed to focus light rays from near or distant objects on retina
(4) Ciliary processes
(a) Produce aqueous humor
c. Iris
(1) Colored area of eye
(2) Anterior portion of the middle layer
(a) Thin membrane situated in front of the lens
(3) Peripheral border attached to ciliary body
(4) Central border is free.
(5) Divides the space between the cornea and the lens
(a) Anterior and posterior chambers
(b) Chambers filled with aqueous humor
(6) Regulates the amount of light entering the eye
(a) Muscles contract and relax.
(b) Changes size of opening in center (pupil)
(c) Assists in obtaining clear images
3. Internal layer: innermost layer of neural coat (retina)
a. Retina
(1) A thin transparent membrane extending from the ora serrata to the optic disc
(2) Consists of network of nerve cells and fibers
(a) Receives images of external objects
(b) Transfers the impressions to the occipital lobe of cerebrum via
(i) Optic nerve
(ii) Optic tracts
(iii) Lateral geniculate body
(iv) Optic radiations
(c) Nerve fibers from retina converge to become optic nerve.
(i) Point at which optic nerve enters eyeball called optic disc (anatomic blind spot)
(3) Covers choroid
(4) Found only in back of eye
b. Retina composed of layers
(1) Outer pigment
(a) Stores vitamin A; needed to produce photopigment rhodopsin
(2) Inner neural
(a) Consists of photoreceptor cells (rods and cones)
(i) Visual receptors that develop generator potentials
(ii) Relays sensory information to ganglion cells of retina
(b) Rods
(i) Located in peripheral retina
(ii) Allow for vision in dim light
(iii) Responsible for perception of different shades of light and dark, shapes, and movement
(c) Cones
(i) Stimulated by bright light only
(ii) Responsible for color vision and visual acuity
G. Refractive apparatus (cornea, aqueous humor, lens, and vitreous body)
1. Cornea
a. Has greatest refractive power of the ocular structures
b. Variations in curvature of cornea change its refractive power.
2. Aqueous humor
a. Fluid responsible for maintaining intraocular pressure
b. Produced by ciliary processes
c. Secreted by ciliary body into posterior chamber
d. Flows from posterior chamber through pupil into anterior chamber
e. Flows into anterior chamber angle and is filtered out through the trabecular meshwork into Schlemm’s canal
f. Channeled into capillary network and into episcleral veins
g. Maintenance of normal intraocular pressure
(1) Occurs as long as there is a balance between:
(a) Aqueous production
(b) Aqueous humor outflow
3. Lens
a. Suspended behind the iris
b. Anterior and posterior surfaces separated by rounded border
c. Does not shed cells; as it grows, the cells compress and harden.
d. Lens expands and retracts through zonular fibers (accommodation).
e. Accommodation power lost with aging process
f. Hardening eventually causes opacity of lens (cataract).
4. Vitreous body
a. Glasslike transparent gelatinous mass (vitreous humor)
b. Composed of 99% water and 1% collagen and hyaluronic acid
c. Fills the posterior four fifths of the eyeball
d. Supports the posterior cavity
e. Keeps the retina in place
H. Nerve and blood supply
1. Optic nerve (second cranial nerve)
a. Extends between posterior eyeball and optic chiasma
b. Carries visual impulses and sensations of pain, touch, temperature from eye to brain
2. Muscle innervation
a. Oculomotor (third cranial nerve): primary motor nerve to all rectus muscles (except lateral rectus)
b. Abducens (sixth cranial nerve) innervates lateral rectus.
c. Trochlear (fourth cranial nerve) innervates superior oblique muscle.
3. Ophthalmic artery
a. Main arterial supply to orbit and globe
b. Branch of internal carotid artery
II. COMMON OPHTHALMIC SURGICAL PROCEDURES
A. Blepharoplasty—repair of the upper or lower eyelids to remove redundant skin; may be cosmetic or therapeutic when the eyelid interferes with vision
1. Types
a. Upper blepharoplasty (upper eyelid only)
b. Lower blepharoplasty (lower eyelid only)
c. Quadrilateral blepharoplasty (involving all four eyelids)
2. Preoperative considerations
a. Patient may be examined by ophthalmologist before procedure to rule out ocular symptomatology.
3. Surgical procedure
a. Excess skin and muscle resected; periorbital fat trimmed
b. Requires meticulous hemostasis
c. Closed using fine nonabsorbable or absorbable sutures
4. Postoperative considerations
a. Iced saline dressings applied immediately to control edema
B. Removal of chalazion—granulomatous inflammation of a meibomian gland in eyelid, frequently caused by Staphylococcus aureus
1. Surgical procedure
a. Surgical incision and curettage
b. Most commonly done under local anesthesia in physician’s office
c. Occasionally requires operating room (OR) setting
C. Repair of entropion
1. Entropion
a. Eyelid margins turn in, especially the lower lid
b. Caused by spasm of the orbicularis oculi muscle
c. Scarring of the conjunctiva
d. Lashes scrape across cornea with each eye blink, which is painful and results in
(1) Corneal abrasions
(2) Scarring
(3) Ulcer
2. Surgical procedure
a. Surgical removal of excision of skin and/or muscle and/or the tarsal plate
(1) Correction of the muscular fibers of the lid, everting the lid margins and eyelashes
(2) Performed under local or general anesthesia
b. Cryotherapy—may be used to freeze and remove lashes, which destroys lash follicle and prevents regrowth of lashes
(1) Preferred method of treatment
D. Repair of ectropion
1. Ectropion—outward turning or eversion of eyelid, usually bilateral
a. Caused by:
(1) Relaxation of orbicularis oculi muscle
(2) Scarring of the face near the eye
(3) Normal aging process
(4) Bell’s palsy
(5) Exposure of underlying conjunctiva
(6) Congenital
b. Can lead to keratitis (inflammation or infection of the cornea)
2. Surgical procedure
a. Shortening of lower lid in a horizontal direction
b. Mild case can be treated with deep electrocautery 4 to 5 mm from the lid margins.
(1) Resulting scar formation will draw lid to its normal position.
c. Lateral tarsal strip procedure—lateral canthal tightening
(1) Preferred method of treatment
(2) Performed under local anesthesia
d. Upper lid gold weight implantation for paralytic ectropion
E. Ptosis
1. Drooping of the upper eyelid; can affect one or both eyes; caused by weakness of levator muscle, or less frequently, Muller’s muscle
2. Three types of ptosis
a. Congenital—caused by failure of levator muscle to develop, weakness of superior rectal muscles
b. Acquired—associated with loss of superior visual field in primary gaze
(1) Causes
(a) Mechanical failure—weight of eyelid neoplasms
(b) Trauma—caused by laceration of third cranial nerve, the levator, or both
(c) Myogenic, by disease—muscular dystrophy
(d) Neurological disorders—myasthenia gravis
(e) May be caused by a tumor
(f) Aponeurotic ptosis—senescence, dehiscence, or chronic inflammation
(2) Treatment based on cause and severity
c. Senile
3. Surgical procedure
a. Objective is to create a good upper lid fold with elevation of the lid.
b. Surgical procedures based on advancement of
(1) Levator muscle
(2) Frontalis muscle
(3) Superior rectus muscle
F. Excision of pterygium
1. Thick triangular growth of epithelial tissue
a. Extends from corner of cornea to the inner canthus
b. Appearances may be pale or white.
c. May grow over the pupillary opening
d. Cause thought to be exposure to constant irritant such as
(1) Wind
(2) Dust, including sand
(3) Ultraviolet light
2. Surgical procedure
a. Growth dissected off the cornea and conjunctiva down to the sclera
b. Low-dose radiation on surgical wound may be used to prevent regrowth.
(1) Regrowth rate 20% to 40%
G. Lacrimal duct disorders
1. Dacryocystorhinostomy (DCR)—establishment of a new tear passageway for drainage directly into the nasal cavity
a. Dacryocystitis is an infection in the lacrimal sac and its mucous membranes that extends to the surrounding connective tissue, resulting in localized cellulitis.
b. Surgical procedure
(1) Nasal cavity anesthetized topically with cocaine preoperatively
(2) Usually performed under general anesthesia
(3) Lacrimal sac probed and opened
(4) A stent is placed through lacrimal duct drainage system to keep system open until epithelium forms around it and creates a new opening.
(5) Stent generally removed in 6 weeks
2. Conjunctivodacryocystorhinostomy
a. Description
(1) Variation of DCR
(2) Necessary if lacrimal sac
(a) Has been destroyed
(b) Must be recreated
(c) Canaliculi are absent.
b. Surgical procedure
(1) After completion of DCR, conjunctiva taken from lower lid and sutured to nasal mucosa to form lacrimal sac
(2) If canaliculus cannot be kept open or is absent
(a) Permanent stent (Pyrex tube) is placed.
(b) Patient teaching includes:
(i) How to place tube back in if it falls out
(ii) How to clean tube
(iii) How to hold tube in case of sneezing
3. Endoscopic DCR
a. Uses endonasal laser to open pathway into lacrimal sac
b. Uses endoscopic equipment
c. Benefits
(1) Eliminates external incision and scar
(2) Decreases amount of postoperative discomfort
(3) Provides hemostasis
(4) Increases healing time
(5) Decreased cost
H. Surgery for strabismus
1. Description
a. Inability to direct the two eyes at the same object because of lack of coordination of extraocular muscles
b. Misalignment of axes of the eyes in which one or both eyes turned inward or outward
c. Often accompanied by amblyopia (normal vision fails to develop despite absence of disease or refractive error)
d. Normally done on children younger than 6 years
e. May be done for cosmetic reasons for children older than 6 years
f. Indications for performing procedure on adults
(1) Bell’s palsy
(2) Muscular dystrophy
(3) Traumatic injury
(4) Untreated or unsatisfactory treatment of childhood strabismus
(5) Muscular paralysis resulting from stroke
2. Surgical procedure
a. Corrective surgery performed to change the relative strength of individual muscles and therefore improve coordination
(1) May require resection: the removal of a portion of muscle and attachment of cut ends
(2) May require recession: severance of the muscle from its original insertion with reattachment more posteriorly on the sclera
(3) May require transplanting a muscle to improve rotation of paralyzed muscle
b. Intraoperative consideration
(1) Manipulation of rectus muscle will cause transient bradycardia.
(a) Treated with atropine
(b) If severe, surgeon may have to stop manipulation of rectus muscle until heart rate returns to normal.
(2) Bradycardia caused by innervation of branch of vagus nerve
I. Removal of globe
1. Exenteration
a. Entire contents of orbit removed
b. Requires extensive plastic reconstruction
2. Evisceration
a. Removal of contents of the globe
b. Preserves sclera and muscular attachments
c. Prosthesis inserted to maintain shape of eye
(1) Sclera closed over prosthesis
(2) Conjunctiva closed over sclera
(3) Conformer placed under eyelids to maintain space until swelling subsides and artificial eye created
d. Advantages
(1) Natural attachment of eye muscles
(2) Normal eye movement
3. Enucleation
a. Removal of the diseased globe and a portion of the optic nerve
b. General anesthesia usually administered
c. Prosthesis may be inserted.
J. Corneal transplant (keratoplasty)
1. Description
a. Grafting of corneal tissue from one human eye to another
b. Performed when patient’s cornea thickened and opacified
c. Transparency of cornea may be impaired from infection, burns, complications related to laser-assisted in situ keratomileusis (LASIK), or certain diseases.
d. Corneal transplant performed to improve vision when basic visual structures of eye (optic nerve and retina) functioning properly
2. Types
a. Penetrating keratoplasty (full-thickness)
(1) Most common
(2) Performed with microscope
b. Lamellar keratoplasty (partial thickness)
(1) More difficult than penetrating keratoplasty, involving the removal and replacement of the anterior corneal stroma and Bowman’s membrane with donor material
(2) Higher success rate
(a) Success because of layered cellular arrangement of corneal tissue and avascularity
(b) Procedure preserves the host endothelium.
c. Keratectomy (peeling of the cornea)
d. Descemet’s stripping automated endothelial keratoplasty
(1) Procedure is a partial-thickness corneal transplant that replaces only the endothelial layer with donor cells.
e. Tattooing (simulation of a pupil)
(1) Rarely done
3. Postoperative considerations
a. Eye patch and shield remain in place until instructed to remove by surgeon.
b. Activity is light to as tolerated.
c. Resume preoperative diet.
d. Healing of cornea is very slow.
(1) Recovery of vision longer than after cataract surgery
4. Potential complications
a. Rejection of corneal transplant
(1) Cornea becomes opaque.
(2) Treated with steroids
(3) May require repeated keratoplasty
K. Radial keratotomy
1. Description
a. Used to reduce myopia in adults
b. Series of precise, partial-thickness radial incisions in the cornea
c. Results in flattening the cornea, reducing refractive error
2. Usually performed under topical anesthesia
3. Potential complications
a. Glaring from scars
b. Permanent scarring
c. Infection resulting in loss of vision
d. Cataract formation caused by injury to lens
e. Variations in level of correction
4. Correction with excimer laser
a. Ablates top of cornea
b. Fewer complications
(1) Minimal glare sensitivity problems
c. Performed with topical anesthesia
d. Complications
(1) Overcorrection
(2) Undercorrection
(3) Haze, glare, or halos
(4) Elevated intraocular pressure
e. Postprocedure treatment
(1) Instillation of
(a) Tobramycin
(b) Examethasone suspension drops
(c) 5% homatropine hydrobromide antibiotic
(d) Steroid drops
(2) Pain management with analgesics
(3) Placement of disposable soft contact lens for first 3 weeks
(a) Promotes epithelial growth
(4) Use of dark sunglasses
L. Cataract extraction
1. Description
a. Cataract: gradual developing opacity of the lens of the eye
(1) Can occur at any time
(a) Etiology in infants
(i) Heredity
(ii) Developmental abnormalities
(iii) Infection
(iv) Traumatic eye injury
(v) Chemical imbalances (galactosemia and diabetes)
(b) Etiology in adults
(i) Same as infant
(ii) Prolonged exposure to ultraviolet light
(iii) Medications (those used to treat glaucoma)
(iv) Most common cause: normal part of aging process
b. Cataract extraction is the removal of the opaque lens from the interior of the eye.
2. Types of procedures
a. Intracapsular cataract extraction (ICCE)
(1) Removal of lens as well as anterior and posterior capsule, cortex, and nucleus
(2) Method largely replaced by extracapsular cataract extraction
(3) Risk of vitreous humor loss
b. Extracapsular cataract extraction (ECCE)
(1) Anterior portion of the capsule is first ruptured, then removed.
(2) Lens cortex and nucleus are expressed from the eye, leaving the posterior capsule behind intact (posterior capsule is excellent support for intraocular lens implantation).
c. Phacoemulsification
(1) Lens removed by fragmenting it with ultrasonic vibrations
(2) Simultaneously, fragments irrigated and aspirated without loss of lens capsule
(3) Very small incision needed
3. Correction of aphakia (absence of lens)
a. Patient sees objects larger than normal.
b. Objects appear blurred and without detail.
c. Options available for correction
(1) Glasses
(a) Aphakia spectacles
(b) Fitted 6 to 8 weeks after lens extraction
(c) Acceptable only for binocular aphakia
(d) Distorts peripheral vision
(e) Produces enlarged images
(f) Clear image only in direct center of glasses
(2) Contact lens
(a) Better option for vision correction
(b) Can be used for monocular aphakia
(c) Patient has complete field of vision.
(d) Less magnification of image required
(3) Epikeratophakia
(a) Procedure considered for patients with low endothelial cell counts
(b) Form of refractive keratoplasty
(c) Description of procedure
(i) Piece of donor corneal tissue shaped to specific diopter on a cryolathe
(ii) Tissue sutured to recipient’s cornea
(iii) Changes corneal curvature
(iv) Results in change of refractive power of cornea
(4) Placement of intraocular lens (IOL)
(a) Most commonly used procedure today
(b) Description of lens
(i) Made of Plexiglas or polymethylmethacrylate, acrylic material, silicon
(ii) Center can be either biconvex or convexoplano and two haptics (spring-hook appendages).
[a] Polypropylene haptics break down over time.
[b] Should not be used on young patients
(iii) Lens cannot adjust anterior to posterior dimensions.
[a] Provides only myopic (nearsighted) or hyperopic (farsighted) vision
[b] Patient decides on need of glasses for distance or reading.
(5) Advantages of IOL
(a) Shorter rehabilitation period
(b) Lens used for monocular aphakic correction
(6) Lens placement
(a) Anterior chamber
(i) Used after ICCE
(ii) Used for secondary lens implantation
(b) Iris plane
(c) Sulcus fixated
(d) Posterior chamber
(i) Only when cataract removed by ECCE or phacoemulsification
(ii) Most physiological position for artificial lens
(7) Sutureless cataract technique
(a) Most common
(b) Rapid visual rehabilitation
4. Preoperative considerations
a. Inquire as to patient’s use of anticoagulants, nonsteroidal, and anti-inflammatory drugs (Motrin or aspirin); can cause increase in bleeding intraoperatively.
b. Identify adequate home support system; implement referrals if necessary.
c. Review preoperative instructions with patient.
(1) Provide instructions in large type.
(2) Use off-white paper to reduce glare.
d. Administer mydriatics and/or additional medications as ordered.
M. Procedures to treat glaucoma
1. Iridectomy
a. Description
(1) Removal of a section of iris tissue
(2) Peripheral iridectomy done in the treatment of acute, subacute, or chronic angle-closure glaucoma
(a) Extensive peripheral anterior synechiae not yet formed
(3) Reestablishes communication between posterior and anterior chambers
(4) Relieves pupillary block
(5) Facilitates movement of aqueous humor from posterior to anterior chamber
2. Trabeculectomy
a. Description
(1) Creation of a fistula between anterior chamber of eye and subconjunctival space
(2) Portion of the trabecular meshwork surgically excised
(3) Facilitates drainage of aqueous humor from the posterior chamber to the anterior chamber for treatment of glaucoma
b. Adjunctive medical therapy may be used to decrease postoperative fibrosis by applying 5-fluorouracil or mitomycin C under the conjunctival flap for 3 to 5 minutes.
N. Vitrectomy
1. Description
a. Removal of all or part of vitreous gel
2. Indications (anterior segment)
a. Vitreous loss during cataract extraction surgery
b. Anterior segment opacities
c. Miscellaneous causes
3. Indications (posterior segment)
a. Vitreous opacities
b. Advanced diabetic eye disease
c. Severe intraocular trauma
d. Retained foreign bodies
e. Endophthalmitis
4. Procedural considerations
a. Procedure varies according to location of pathological condition.
(1) Anterior
(2) Posterior
b. Requires use of operating microscope, illuminations system, and cutting-suction-infusion system
5. Intraoperative considerations
a. Procedure time varies from 1 hour to 6 hours.
b. Protect pressure area on patient.
c. May use elastic stockings
6. Postoperative considerations
a. May experience more postoperative pain than is generally associated with ophthalmological surgeries
(1) Strong analgesics may be necessary.
(2) Ice packs may help reduce pain.
O. Retinal detachment
1. Description
a. Separation of portion of retina from choroid
b. Goal of treatment aimed at repairing tears and returning retina to normal anatomical position
2. Causes
a. Intraocular neoplasms
b. Associated with injury (blow to head or previous ocular surgery)
c. Normal aging process
d. Severe myopia
e. Congenital
f. Inflammatory process
g. Vascular disease
3. Signs and symptoms
a. Patient may experience sudden onset of floaters (floating spots in front of eye).
b. Loss of vision without pain
c. Slow decrease in visual field (described as if someone were pulling a curtain in front of eye)
4. Types
a. Primary detachment—(rhegmatogenous) hole in retina permits fluid to enter space between retina and choroid.
b. Secondary detachment—fluid or tissue builds up between choroid and retina with no hole in retina.
5. Treatment
a. Diathermy
(1) Traditional method
(a) Insertion of microneedles or needle tip of a probe into sclera
(b) Shortwave radio frequency energy delivered through needles
(c) Causes thermal changes in tissue
(d) Results in scar formation and retinal reattachment at points of adhesion
(e) Procedure rarely used anymore
b. Cryotherapy
(1) More popular method; less invasive than diathermy
(2) Application of 80° C cryoprobe to scleral area of detachment
(3) Inflammation causes adhesion and reattaches retina.
(4) Fewer complications than diathermy
c. Pneumoretinopexy
(1) Injection of air or expansile gases into vitreous cavity
(2) Usually done in physician’s office
(3) Cryotherapy may be used to close and seal hole before gas is injected.
(4) Patient may be instructed to hold head in certain position until retina reattaches (usually 2 weeks).
d. Laser therapy
(1) Used to “spot weld” retina
(2) Requires retina to be flat over retinal pigment epithelium before chorioretinal adhesion can be formed
(3) Done in physician’s office
(4) Can be done in OR in conjunction with vitrectomy
e. Scleral buckling
(1) Description
(2) Procedure developed to create indentation in retina so that adherence between detached area and underlying tissues will result in permanent reattachment
f. Posterior vitrectomy
(1) Description
(a) Objective is to remove vitreous humor without pulling on retina; permits surgeon to work directly on retina
(b) Can be performed with all techniques for reattaching retina
6. Preoperative considerations
a. Instruct patient regarding activity limitations before surgery (reduces stress on area of detachment).
b. Inform patient and family of potential for lengthy surgery (decrease anxiety level).
7. Postoperative considerations
a. Patient usually on cycloplegic agents (atropine or cyclopentolate) to dilate pupil and rest muscles of accommodation
b. May be on antibiotic and steroid eye drops
c. Assess patient’s ability to instill eye drops.
d. Patients with an intraocular gas bubble should be instructed not to fly because gas bubble expands with changing atmospheric pressure.
P. Laser therapy
1. Description
a. Noninvasive ambulatory procedure in which a slit lamp is used to deliver the laser beam
b. May eliminate the need for more invasive procedures
c. Argon or yttrium aluminum garnet (YAG) lasers used in a procedure room
d. Topical anesthetic drops instilled
2. Procedures
a. Laser trabeculoplasty
(1) Treatment for open-angle glaucoma
b. Laser iridotomy
(1) Treatment for acute or chronic angle-closure glaucoma
c. Laser posterior capsulotomy
(1) May be required when patients experience decreased vision within 2 years after ECCE
(2) YAG laser used to create a window in the posterior capsule
(3) Patients may have pupils dilated.
(4) Iopidine may be used to prevent increased intraocular pressure.
III. ANESTHETIC CONSIDERATIONS
A. Types (overview)
1. Topical
a. Topical anesthetic eye drops used more frequently
b. Rapid onset with moderate duration of action
c. Decrease risk with retrobulba and infection
d. Continue anticoagulation therapy
2. Local anesthesia block
a. Used frequently
b. Contraindications
(1) Patients who have difficulty lying still
(2) Children
(3) Patients who have frequent cough
3. Moderate sedation and analgesia used in conjunction with block
4. General anesthesia
B. Topical anesthetic drops
1. Used frequently
a. Proparacaine hydrochloride 0.5%
b. Tetracaine hydrochloride 0.5%
c. Lidocaine hydrochloride 2%
C. Eye block
1. Types
a. Retrobulbar block
(1) Injection of anesthetic solution into base of eyelids at level of orbital margins or behind the eyeball to block the ciliary ganglion and nerves
b. Peribulbar block
(1) Local anesthetic deposited beside the globe instead of behind it
2. Performed in two stages
3. Stage I—blocks eyelid
a. Three methods
(1) Van Lint method—blocks peripheral branches of cranial nerve VII in the orbicularis oculi muscle
(2) Atkinson method—blocks temporal arborization of cranial nerve VII to the orbicularis muscle
(3) O’Brien method—blocks the main trunk of cranial nerve VII near the temporomandibular joint
4. Stage II—retrobulbar block
a. Provides anesthesia to globe and muscular attachments
b. Blocks branches of cranial nerves III, IV, V, and VI
c. Common medications used
(1) Lidocaine hydrochloride 2% or 4%; mixed with equal parts of 0.75% bupivacaine hydrochloride with hyaluronidase (used for diffusing local anesthetic to surrounding tissue)
(2) May add epinephrine hydrochloride to prolong effectiveness of agents
(3) May use as much as 6 mL for retrobulbar block and 10 mL for peripheral tissue
d. Nursing considerations
(1) Inform patient of possible burning sensation.
(2) Inform patient of possible feeling of pressure behind eye during injection of medication.
(3) Inform patient that physician may massage eye after injection of medication.
(a) Decreases intraocular pressure
(b) Aids in diffusing agents
(4) Patient frequently given intravenous sedation to decrease discomfort during the injection; administer medications per protocol.
(5) Monitor vital signs per protocol.
(6) Patient may be awake during procedure.
(a) Monitor noise level.
(b) Monitor patient’s anxiety level.
e. Nursing care after eye block
(1) Patient will not have blink reflex; must keep eyelid closed to protect the cornea.
(a) Tape the eyelid closed.
(b) Reassure patient that it is normal to be unable to open the eyelid.
f. Effectiveness of eye block
(1) Generally very effective
(2) Occasionally a block may be incomplete, and patient will experience pain.
(3) Instruct patient to use hand signal during surgery if he or she experiences pain or discomfort.
g. Potential complications—cancellation of surgical procedure strongly advised for any of the following complications:
(1) Retinal detachment (caused by insertion of needle through globe)
(2) Injection of anesthetic into optic nerve (irreparable damage)
(3) Retrobulbar hemorrhage (most common)
(a) Controlled by pressure to globe
D. General anesthesia
1. Indications
a. Children
b. Patients unable to tolerate local anesthetic with sedation
c. Extremely anxious patients
d. Patients with certain systemic diseases
e. Patients undergoing prolonged operations
2. Postanesthesia care
a. Same as any patient who has undergone general anesthesia
IV. DRUGS FREQUENTLY USED FOR OPHTHALMOLOGICAL SURGERY
A. Mydriatics
1. Action
a. Blocks cholinergic stimulation of sphincter muscle of iris (dilation of pupil)
b. Blocks accommodative ciliary muscle of lens (paralysis of accommodation)
2. Types
a. Phenylephrine hydrochloride (Alconefrin, Neo-Synephrine, Prefrin)
b. Hydroxyamphetamine (Paredrine)
B. Cycloplegics
1. Action
a. Dilate pupils and paralyze accommodation by acting on ciliary muscles (parasympatholytics)
2. Types
a. Atropine
b. Homatropine (AK-Homatropine, Isopto Homatropine, Minims Homatropine)
c. Cyclopentolate (Cyclogyl)
d. Scopolamine (Isopto Hyoscine, Mydramide)
e. Tropicamide (Mydriacyl)
C. Miotics
1. Action
a. Used to constrict the pupil (parasympathomimetics)
2. Types
a. Cholinergics
(1) Pilocarpine hydrochloride
(2) Carbachol (Miostat, Carbacel)
(3) Acetylcholine chloride (Miochol)
b. Anticholinesterase
(1) Physostigmine (Eserine)
(2) Isoflurophate (Floropryl)
(3) Echothiophate iodide (Phospholine Iodide)
D. Osmotic agents
1. Action
a. Parenteral agents used to lower intraocular pressure through the blood-ocular gradient
2. Types
a. Mannitol (Osmitrol)
b. Glycerin (glycerol, Glyrol, Osmoglyn)
E. Viscoelastic agents
1. Action
a. Used to maintain the intraocular chamber during surgery
2. Types
a. Sodium hyaluronate (Healon, Amvisc)
b. Ocucoat
F. Carbonic anhydrase inhibitors
1. Action
a. Parenteral agent used to decrease intraocular pressure; used for glaucoma
2. Types
a. Acetazolamide (Diamox)
b. Methazolamide (Neptazane)
G. Corticosteroids
1. Action
a. Anti-inflammatory agents
2. Types
a. Hydrocortisone (Solu-Cortef) ointment or eye drops
b. Dexamethasone (Decadron) eye drops
c. Prednisolone (Pred Forte, AK-Pred, Inflamase Mild, Inflamase Forte)
H. Topical antibiotics
1. Action
a. Used for prophylaxis of or treatment of infections; may be used in solutions or ointments
2. Types
a. Bacitracin, neomycin, erythromycin, tetracycline, gantrisin, tobramycin, gentamycin
b. Chloramphenicol
V. PREOPERATIVE CONSIDERATIONS
A. Assessment
1. Patient’s and family’s understanding of:
a. Eye disorder
b. Goal of surgery
c. What to expect before, during, and after surgery
d. Postoperative care and support
2. Assess in detail patient’s understanding of intraoperative procedure, local anesthesia and sedation versus general.
3. Identify patient’s reaction to scheduled surgery.
a. Unrealistic expectations regarding improved vision
b. Anxiety over potential loss of vision
4. Identify current visual status.
a. May need additional safety precautions if severely impaired
b. May need additional support postoperatively if visual status of unoperative eye is limited
B. General health assessment per routine protocol
1. Identify illnesses that can cause sneezing, coughing, history of postoperative nausea and vomiting, or increase in intraocular pressure.
a. Patient may not be a candidate for local anesthesia with sedation.
b. May require general anesthesia
2. Consider co-morbidities of patients scheduled for surgery.
C. Preoperative care
1. Relieve anxiety related to impending surgery (the eyes are very sensitive to pain and pressure).
a. Allow patient time to verbalize concerns.
(1) Patient may have misconceptions regarding eye surgery.
(2) Clarify misconceptions.
(3) Some patients may think they will actually see the procedure through the operative eye.
b. Involve the patient in the plan of care.
(1) Provide clear written instructions in large type.
(2) Reinforce physician’s orders regarding preoperative and postoperative medications and eye drop schedules.
c. Provide emotional support.
(1) Convey positive realistic attitude.
(2) Acknowledge validity of patient concerns.
2. Verify correct surgical eye.
a. Confirm with patient correct eye for surgery.
(1) Initiate time-out procedure.
(2) Document correct eye before preoperative sedation.
(3) Keep in mind many patients may be unable to accurately identify the operative eye because of age or mental status.
b. Document correct operative eye.
(1) Verify the surgical consent and the history and physical with the scheduled procedure.
(2) Investigate any discrepancy.
c. Clearly identify surgical eye with skin marker (facility policy outlines process).
(1) Visual marking should not be the sole way of identifying the correct surgical eye.
(2) Every perianesthesia nurse caring for the patient should verify the patient’s understanding, the consent, and the scheduled procedure before proceeding with care.
3. What to expect
a. Length of time (preoperatively, intraoperatively, postoperatively)
b. Eye patch (depending on surgical procedure)
c. Reinforcement that improved vision may require a period of time
4. Demonstrate proper method of eye drop instillation.
a. Explain ways to avoid contamination of eye medications.
b. Reinforce need to follow prescription instructions accurately.
c. Teach proper technique for instillation of eye drops.
(1) Confirm on bottle that drops are for ophthalmic use.
(2) Note the expiration date and discard if outdated.
(3) Wash hands before using eye drops.
(4) Confirm proper eye.
(5) Tilt head back for instillation.
(6) Keep eyes open, and look upward.
(7) Gently pull down tissue below the lower lid.
(8) Place correct number of eye drops into the conjunctival sac.
(9) Close eyes, and try to avoid excessive blinking or squeezing for several minutes.
(10) Gently blot any excess solution from beneath the eye.
(11) Wait 5 minutes before instilling a different type of eye drop.
(12) Do not touch tip of eye medication dispenser to the eyelid or with hands.
D. Review postoperative routine.
1. Include family and significant other as appropriate.
2. Things to avoid postoperatively
a. Quick movements
b. Bending over from the waist
c. Rubbing eyes
d. Heavy lifting
3. Moderation in activity
4. Proper hand washing before caring for the eye
E. Nursing considerations
1. Visually impaired patient
a. Approach from unaffected or least affected side.
b. Identify self.
c. Speak in normal tone.
d. Provide method for patient to obtain immediate assistance (call bell in reach).
e. Keep visual aids in close proximity.
f. Allow patient to keep assistive devices as long as possible.
g. Keep walking area clear of obstructions.
2. Administer preoperative medications as ordered.
a. Mydriatics to dilate pupil
b. Notify physician if expected dilation does not occur.
3. Encourage patient to void before procedure.
a. Patient will become restless in OR if he or she has a full bladder.
F. Overall assessment of patient’s ability to tolerate anesthesia plan
1. Procedure usually performed under local anesthesia with sedation (adults)
2. Assess patient’s ability to lie still under drapes for long period (1-3 hours).
3. Factors influencing decision include:
a. Chronic cough
b. Airway difficulties
c. Claustrophobia
d. Involuntary motions
VI. POSTOPERATIVE CONSIDERATIONS
A. Assessment
1. Routine assessment per protocol
B. Positioning
1. Assist patient to chair or recliner.
a. Avoid bumping or jarring.
2. Orient patient to surroundings.
3. Certain operations (vitreoretinal surgery) may require special positioning.
a. Surgeon should provide specific instructions as to positioning.
b. Patient may need to be on side or back.
4. Patient may have decreased pain with head of bed elevated.
C. Drainage
1. Type and amount; document.
2. Notify physician per protocol.
D. Pain and discomfort level—assess and document.
1. Varies with each procedure
a. Usually uncommon after most eye surgeries
2. Varies with type of anesthesia administered
3. Patient may feel stiff and sore.
a. Results from lying still and flat intraoperatively
4. Pain usually relieved by acetaminophen, propoxyphene hydrochloride, or similar analgesics
5. May experience significant pain after vitreoretinal surgery
a. Administer narcotic analgesic as indicated.
b. Apply ice pack.
c. Notify ophthalmologist if pain not relieved by analgesics.
E. Nausea
1. Caused by manipulation of eye and eye muscles during surgery
2. May be caused by sedation
3. Medicate immediately to prevent potential vomiting.
a. Vomiting results in increased intraocular pressure.
b. Instruct patient to notify nurse immediately if he or she begins to feel nauseous so that antiemetics may be given.
4. To avoid potential for nausea and vomiting, oral fluids may be held for a while if patient underwent general anesthesia.
F. Visual impairment from surgery
1. Ensure patient safety at all times.
2. Requires assistance at home
3. Verify arrangements before discharge.
G. Eye shields and dressings
1. Dressing or eye shields may remain in place until the patient’s first postoperative appointment at the physician’s office.
a. Instruct patient not to disturb or remove shield and dressing.
2. Alteration in depth perception may be expected when one eye is bandaged.
a. Evaluate patient for adequate balance before allowing him or her to ambulate unassisted.
3. Provide clear written instructions for postoperative care at home.
a. Wash hands before caring for eye.
b. Do not rub eye.
c. Surgeon will remove eye patch or shield during postoperative appointment.
d. Wear glasses or shield at all times to protect the eye.
e. Wear shield at night for sleeping.
f. Do not bend at the waist.
g. Avoid heavy lifting.
h. Avoid reading (operative eye muscles will move together with unoperative eye, causing discomfort).
i. Do not drive until after first postoperative appointment.
(1) Do not drive at all if experiencing double vision.
j. Take all eye medications as ordered.
k. Notify physician if any of the following occur:
(1) Pain not relieved by acetaminophen
(2) Sudden loss of vision
(3) Increasing double vision after surgery
(4) Temperature greater than 100° F
(5) Significant swelling or redness about the eye
(6) Unexpected drainage from the eye
H. Discharge instructions
1. Inform patient to use strict aseptic technique when caring for eye and administering medications.
2. Administer eye medications as directed by physician.
3. Avoid activities that increase intraocular pressure.
a. Bending
b. Sneezing or coughing
c. Sudden jarring or forceful movements
d. Forceful nose blowing
e. Sexual intercourse
f. Straining during stools
4. Wear sunglasses when outdoors.
5. Avoid use of eye makeup.
6. Responsible accompanying adult stays with patient for first 24 hours.
7. Notify physician if any increase in pain, vision changes, or signs and symptoms of infection (redness, increased swelling, purulent drainage).
VII. POSSIBLE COMPLICATIONS OF OPHTHALMIC SURGERY
A. Pain
1. Minimal in most ophthalmic surgeries
2. Causes: increased intraocular pressure, surgical manipulation, pressure from dressing
3. Treatment: mild analgesic; be aware that need for stronger medication may indicate possible complications.
B. Bleeding
1. Minimal for all ophthalmic surgeries
2. Cause: dressing too loose
3. Treatment: apply or reinforce dressing; notify physician.
C. Nausea and vomiting
1. Usually minimal after ophthalmic surgery
2. Causes: oculocardiac reflex, surgical manipulation, general anesthesia
3. Treatment: antiemetic; avoid potential vomiting.
D. Oculocardiac reflex (nervous response elicited by manipulation of extraocular muscles or surrounding ocular tissue)
1. Causes: decreased heart rate, blood pressure, and level of consciousness
2. Is seen immediately to 20 minutes postoperatively
3. May be seen with all types of ophthalmic surgeries
a. Risk increases with vitreoretinal and eye muscle surgeries.
b. May be stimulated by retrobulbar block
4. Treatment: intravenous atropine
BIBLIOGRAPHY
1. In: (Editor: Burden, N.) Ambulatory surgical nursinged 2 ( 2004)WB Saunders, Philadelphia.
2. In: (Editor: Dirckx, J.) Stedman’s concise medical dictionary for the health professionsed 4 ( 2001)Lippincott Williams & Wilkins, Philadelphia.
3. In: (Editors: Drain, C.; Odom-Forren, J.) Perianesthesia nursing: A critical care approached 5 ( 2009)WB Saunders, St Louis.
4. eMedicine from WebMD, Otolaryngology and facial plastic surgery articles. ( February 1, 2008) ; Available at:www.emedicine.com/ent; Accessed.
5. In: (Editor: Karch, A.) 2006 Lippincott’s nursing drug guide ( 2006)Lippincott Williams & Wilkins, Philadelphia.
6. Maloney, W., Beveled blades have simplified clear corneal technique, Ocul Surg News 15 (18) ( 1997) 11.
7. In: (Editor: Nettina, S.) The Lippincott manual of nursing practiceed 8 ( 2000)Lippincott, Philadelphia.
8. In: (Editors: Phippen, M.; Wells, M.) Patient care during operative and invasive procedures ( 2000)WB Saunders, Philadelphia.
9. In: (Editor: Pudner, R.) Nursing the surgical patiented 2 ( 2005)Elsevier, Edinburgh.
10. Rothrock, J., Alexander’s care of the patient in surgery. ed 13 ( 2007)Mosby, St Louis.




