Cardioversion
PREREQUISITE NURSING KNOWLEDGE
• Understanding of the anatomy and physiology of the cardiovascular system, principles of cardiac conduction, basic dysrhythmia interpretation, and electrical safety is needed.
• Basic and advanced cardiac life support knowledge and skills are essential.
• Clinical and technical competence in the use of the defibrillator is important.
• Synchronized cardioversion is recommended for termination of those dysrhythmias that result from a reentrant circuit, which include unstable supraventricular tachycardia, atrial fibrillation, atrial flutter, and unstable monomorphic ventricular tachycardia with a pulse.3,6 Because ventricular tachycardia is often a precursor to ventricular fibrillation, cardioversion has the potential to prevent this life-threatening dysrhythmia.
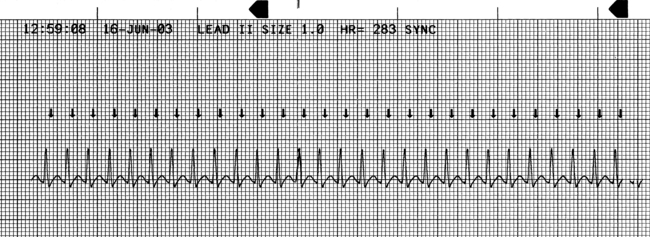
• The electrical current delivered with cardioversion depolarizes the myocardial tissue involved in the reentrant circuit. This depolarization renders the tissue refractory; thus, it is no longer able to initiate or sustain reentry.3,6 A countershock synchronized to the QRS complex allows for the electrical current to be delivered outside the heart’s vulnerable period in which a shock can precipitate ventricular fibrillation.2,3,5–7 This synchronization occurs a few milliseconds after the highest part of the R wave but before the vulnerable period associated with the T wave.3,5,6
• Cardioversion may be implemented in the patient with an emergent condition. The aforementioned dysrhythmias are converted with synchronized cardioversion when the patient develops symptoms from the rapid ventricular response. Symptoms may include hypotension, chest pressure, shortness of breath, dyspnea on exertion, decreased level of consciousness, pulmonary edema, crackles, rhonchi, jugular vein distention, peripheral edema, and ischemic electrocardiogram (ECG) changes.5
• Elective cardioversion may be used to convert hemodynamically stable atrial fibrillation or atrial flutter into normal sinus rhythm.1,2,7 With use to convert atrial fibrillation or atrial flutter, anticoagulation therapy is considered for 3 weeks before cardioversion to decrease the risk of thromboembolism.2,7,9 Anticoagulation therapy may not be necessary if atrial fibrillation or atrial flutter has been present for less than 48 hours.2,7 A physician or advanced practice nurse may choose to perform a transesophageal echocardiogram to exclude the possibility of an atrial thrombus before cardioversion for patients at high risk for thromboembolism. The patient is started on intravenous heparin, and the cardioversion is performed within 24 to 48 hours.1,2,7,9 Anticoagulation therapy should be continued for 4 weeks after cardioversion because of the possibility of delayed embolism.1,2,7,9
• Elective cardioversion also may be used in patients with hemodynamically stable ventricular or supraventricular tachydysrhythmias unresponsive to medication therapy.1
• If time and clinical condition permit, the patient should be given a combination of analgesia and sedation to minimize discomfort.2,3,5–7
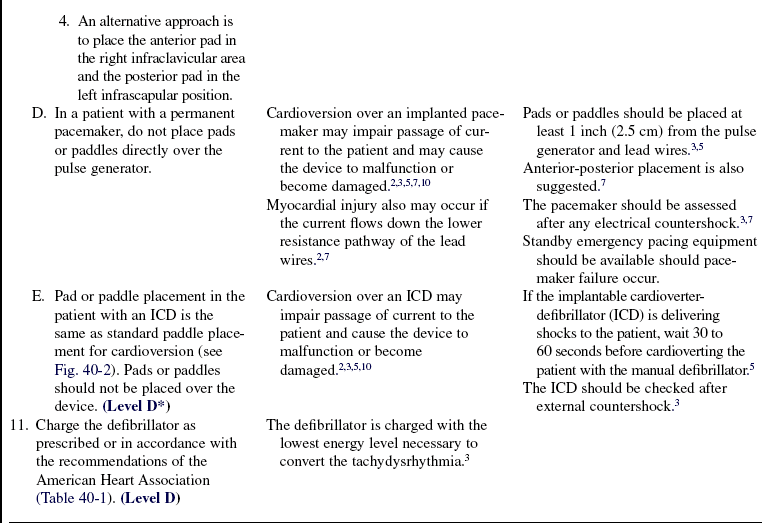
• Defibrillators deliver energy or current in waveform patterns. Delivered energy levels may differ among the various defibrillators and waveforms. Various types of monophasic waveforms are used in older defibrillators. Biphasic waveforms have been designed more recently and are used in implantable defibrillators, automatic external defibrillators, and most manual defibrillators.
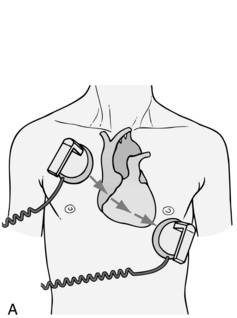
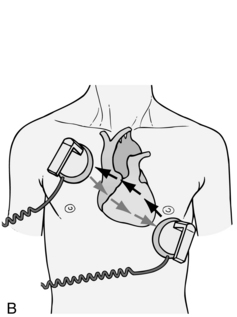
 Monophasic waveforms deliver energy in one direction. The energy travels through the heart from one paddle or pad to the other.3,6,10
Monophasic waveforms deliver energy in one direction. The energy travels through the heart from one paddle or pad to the other.3,6,10
 Biphasic waveforms deliver energy in two directions. The energy travels through the heart in a positive direction then reverses itself and flows back through the heart in a negative direction.3,6,10 Biphasic waveform technology is able to decrease the amount of current needed to terminate the dysrhythmia, decreasing the amount of potential damage to the myocardium.3 In more recent studies, atrial fibrillation was successfully cardioverted with biphasic waveform shocks that ranged from 100 to 120 J.3,11,12,14 More research is needed to determine a specific recommendation for biphasic waveform cardioversion.3 For that reason, the American Heart Association states that biphasic waveform shocks are acceptable if documented as clinically equivalent to reports of monophasic shocks.3,5
Biphasic waveforms deliver energy in two directions. The energy travels through the heart in a positive direction then reverses itself and flows back through the heart in a negative direction.3,6,10 Biphasic waveform technology is able to decrease the amount of current needed to terminate the dysrhythmia, decreasing the amount of potential damage to the myocardium.3 In more recent studies, atrial fibrillation was successfully cardioverted with biphasic waveform shocks that ranged from 100 to 120 J.3,11,12,14 More research is needed to determine a specific recommendation for biphasic waveform cardioversion.3 For that reason, the American Heart Association states that biphasic waveform shocks are acceptable if documented as clinically equivalent to reports of monophasic shocks.3,5
• Biphasic defibrillators measure and compensate for transthoracic impedance before the delivery of the shock, which allows the defibrillator to deliver the actual amount of energy selected by the rescuer.3,6
EQUIPMENT
• Defibrillator/monitor with ECG oscilloscope/recorder capable of delivering a synchronized shock
• Conductive gel or paste, prepackaged gelled conduction pads or self-adhesive defibrillation pads connected directly to the defibrillator
• Intravenous sedative or analgesic pharmacologic agents as prescribed
• Bag-valve device with mask and oxygen delivery
• Flow meter for oxygen administration, oxygen source
• Emergency suction and intubation equipment
Additional equipment to have available as needed includes the following:
PATIENT AND FAMILY EDUCATION
• Assess patient and family understanding of the etiology of the dysrhythmia.  Rationale: This assessment determines the patient and family understanding of the condition and additional educational needs.
Rationale: This assessment determines the patient and family understanding of the condition and additional educational needs.
• Explain the procedure to the patient and family.  Rationale: This explanation decreases anxiety and promotes patient cooperation.
Rationale: This explanation decreases anxiety and promotes patient cooperation.
• Explain the signs and symptoms of hemodynamic compromise associated with the preexisting cardiac dysrhythmias to the patient and family.  Rationale: This explanation enables the patient and family to recognize when the patient needs to notify the nurse or physician.
Rationale: This explanation enables the patient and family to recognize when the patient needs to notify the nurse or physician.
• Evaluate and discuss with the patient the need for long-term pharmacologic support.  Rationale: This discussion allows the nurse to anticipate educational needs of the patient and family regarding specific discharge medications.
Rationale: This discussion allows the nurse to anticipate educational needs of the patient and family regarding specific discharge medications.
• Assess and discuss with the patient the need for lifestyle changes.  Rationale: The underlying pathophysiology may necessitate alterations in the patient’s current lifestyle and require a plan for behavioral changes.
Rationale: The underlying pathophysiology may necessitate alterations in the patient’s current lifestyle and require a plan for behavioral changes.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess the patient’s ECG results for tachydysrhythmias, including paroxysmal supraventricular tachycardia, atrial fibrillation, atrial flutter, and ventricular tachycardia, which could require synchronized cardioversion.  Rationale: Tachydysrhythmias may precipitate deterioration of hemodynamic stability.3,5
Rationale: Tachydysrhythmias may precipitate deterioration of hemodynamic stability.3,5
• Assess the patient’s vital signs and any associated symptoms of hemodynamic compromise with each significant change in ECG rate and rhythm.  Rationale: Deterioration of vital signs or the presence of associated symptoms indicates hemodynamic compromise that could become life-threatening.3,5
Rationale: Deterioration of vital signs or the presence of associated symptoms indicates hemodynamic compromise that could become life-threatening.3,5
• Assess for the presence or absence of peripheral pulses and the patient’s level of consciousness.  Rationale: This baseline determination assists in the detection of cardioversion-induced peripheral embolization.2,6,7,9
Rationale: This baseline determination assists in the detection of cardioversion-induced peripheral embolization.2,6,7,9
• Obtain the patient’s serum potassium, magnesium, and digitalis levels and arterial blood gas results.  Rationale: Electrolyte imbalances, acid-base disturbances, and digitalis toxicity significantly contribute to electrical instability and may potentiate postconversion dysrhythmias.2 Hypokalemia should be corrected to prevent postconversion dysrhythmias. Although cardioversion is considered a safe practice in patients taking digitalis glycosides, they are generally held on the day of cardioversion.
Rationale: Electrolyte imbalances, acid-base disturbances, and digitalis toxicity significantly contribute to electrical instability and may potentiate postconversion dysrhythmias.2 Hypokalemia should be corrected to prevent postconversion dysrhythmias. Although cardioversion is considered a safe practice in patients taking digitalis glycosides, they are generally held on the day of cardioversion.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand preprocedural teaching. Answer questions as they arise, and reinforce information as needed.  Rationale: This communication evaluates and reinforces understanding of previously taught information.
Rationale: This communication evaluates and reinforces understanding of previously taught information.
• Ensure that informed consent is obtained.  Rationale: Informed consent protects the rights of the patient and makes competent decision-making possible for the patient, however, in emergency circumstances, time may not allow for the consent form to be signed.
Rationale: Informed consent protects the rights of the patient and makes competent decision-making possible for the patient, however, in emergency circumstances, time may not allow for the consent form to be signed.
• Perform a pre-procedure verification and time out if non-emergent.  Rationale: Ensures patient safety.
Rationale: Ensures patient safety.
• Obtain 12 lead ECG.  Rationale: Provides baseline data.
Rationale: Provides baseline data.
• Give the patient nothing by mouth per institution policy.  Rationale: Decreases the risk of aspiration.
Rationale: Decreases the risk of aspiration.
• Establish a patent intravenous access.  Rationale: Medication administration may be necessary.3,5
Rationale: Medication administration may be necessary.3,5
• Assist the patient to a supine position.  Rationale: Supine positioning provides the best access for procedure initiation, intervention, and management of possible adverse effects.
Rationale: Supine positioning provides the best access for procedure initiation, intervention, and management of possible adverse effects.
• Remove all metallic objects from the patient.  Rationale: Metallic objects are excellent conductors of electrical current and could result in burns.
Rationale: Metallic objects are excellent conductors of electrical current and could result in burns.
• Remove transdermal medication patches from the patient’s chest or ensure the defibrillator pads or paddles do not touch patches.  Rationale: Transdermal medication patches may block the transfer of energy from the pads or paddles to the patient and may produce a chest burn when the pads or paddles are placed over it.3,5,10
Rationale: Transdermal medication patches may block the transfer of energy from the pads or paddles to the patient and may produce a chest burn when the pads or paddles are placed over it.3,5,10
• Ensure that the patient is in a dry environment, and dry the patient’s chest, if it is wet.  Rationale: Water is a conductor of electricity. If the patient and rescuer are in contact with water, the rescuer may receive a shock or the patient may receive a skin burn. Also, if the patient’s chest is wet, the current may travel from one paddle across the water to the other, resulting in a decreased amount of energy to the myocardium.3,5
Rationale: Water is a conductor of electricity. If the patient and rescuer are in contact with water, the rescuer may receive a shock or the patient may receive a skin burn. Also, if the patient’s chest is wet, the current may travel from one paddle across the water to the other, resulting in a decreased amount of energy to the myocardium.3,5
• If the patient has a hairy chest, clipping or removing the hair from the chest (if time is available) may be necessary.  Rationale: This action allows the electrodes to adhere to the chest.3,5 Chest hair has been known to increase transthoracic impedance in patients.13,15
Rationale: This action allows the electrodes to adhere to the chest.3,5 Chest hair has been known to increase transthoracic impedance in patients.13,15
• Remove loose-fitting dentures, partial plates, or other mouth prostheses.  Rationale: Removal decreases the risk of airway obstruction during the procedure. Evaluate each individual situation (e.g., dentures may facilitate a tighter seal for airway management).
Rationale: Removal decreases the risk of airway obstruction during the procedure. Evaluate each individual situation (e.g., dentures may facilitate a tighter seal for airway management).
• Preoxygenate the patient as prescribed and appropriate to the condition.  Rationale: Adequate oxygenation of cardiac tissue diminishes the risk of cerebral and cardiac complications.5
Rationale: Adequate oxygenation of cardiac tissue diminishes the risk of cerebral and cardiac complications.5
• Maintain a patent airway with oxygenation throughout the procedure.  Rationale: Respiratory depression and hypoventilation can occur after administration of sedatives and analgesics.
Rationale: Respiratory depression and hypoventilation can occur after administration of sedatives and analgesics.
• If time allows, consider administration of sedation and analgesia as prescribed.  Rationale: These medications provide amnesia and decrease anxiety and pain during the procedure.2,3,5–7
Rationale: These medications provide amnesia and decrease anxiety and pain during the procedure.2,3,5–7
Table 40-1
American Heart Association Energy Level Recommendations for Treatment of Tachydysrhythmias
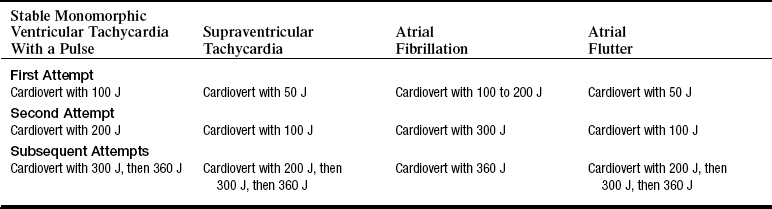
(From Field JM: Advanced cardiac life support provider manual, Dallas, 2006, American Heart Association.)
References
1. American College of Cardiology, American Heart -Association/American College of Physicians Task Force on Clinical Competence and Training. American College of Cardiology/American Heart Association 2006 update of the clinical competence statement on invasive electrophysiology studies, catheter ablation and cardioversion. Circulation 2006; 114:1654–1668.
2. American College of Cardiology, American Heart Association Task Force on Practice Guidelines and the European Society of Cardiology Committee for Practice Guidelines. American College of Cardiology/American Heart -Association/European Society of Cardiology 2006 guidelines for the management of atrial fibrillation. Circulation 2006; 114:e257–354.
![]() 3. American Heart Association, 2005 Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, circulation, part 5. electrical therapiesautomated -external defibrillators, defibrillation, cardioversion, and pacing. Circulation. 2005; 112(Suppl IV):35–46. [IV].
3. American Heart Association, 2005 Guidelines for cardiopulmonary resuscitation and emergency cardiovascular care, circulation, part 5. electrical therapiesautomated -external defibrillators, defibrillation, cardioversion, and pacing. Circulation. 2005; 112(Suppl IV):35–46. [IV].
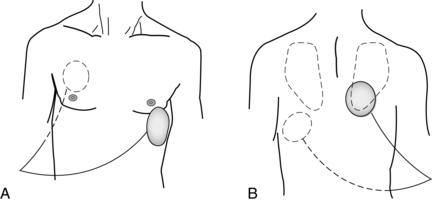
![]() 4. Botto, GI, et al, External cardioversion of atrial fibrillation. role of paddle position on technical efficacy and energy requirements. Heart 1999; 82:726–730.
4. Botto, GI, et al, External cardioversion of atrial fibrillation. role of paddle position on technical efficacy and energy requirements. Heart 1999; 82:726–730.
5. Field JM, ed. Advanced cardiac life support provider manual. Dallas: American Heart Association, 2006.
6. Gowda, SA, et al. Cardioversion of atrial fibrillation. Prog Cardiovasc Dis. 2005; 48(2):88–107.
![]() 7. Kim, SS, Knight, BP. Electrical and pharmacologic cardioversion for atrial fibrillation. Med Clin North Am. 2008; 92:101–120.
7. Kim, SS, Knight, BP. Electrical and pharmacologic cardioversion for atrial fibrillation. Med Clin North Am. 2008; 92:101–120.
![]() 8. Kirchhof, P, et al, Anterior-posterior versus anterior-lateral electrode positions for external cardioversion of atrial fibrillation. a randomized trial. Lancet 2002; 360:1275–1279.
8. Kirchhof, P, et al, Anterior-posterior versus anterior-lateral electrode positions for external cardioversion of atrial fibrillation. a randomized trial. Lancet 2002; 360:1275–1279.
9. Klein, AL, et al, Efficacy of transesophageal echocardiography-guided cardioversion of patients with atrial fibrillation at 6 months. a randomized controlled trial. Am Heart J 2006; 151:380–389.
![]() 10. Mair, M, Monophasic and biphasic defibrillators. the evolving technology of cardiac defibrillation. Am J Nurs 2003; 103:58–60.
10. Mair, M, Monophasic and biphasic defibrillators. the evolving technology of cardiac defibrillation. Am J Nurs 2003; 103:58–60.
![]() 11. Marinsek, M, et al. Efficacy and impact of monophasic versus biphasic countershocks for transthoracic cardioversion of persistent atrial fibrillation. Am J Cardiol. 2003; 92:988–991.
11. Marinsek, M, et al. Efficacy and impact of monophasic versus biphasic countershocks for transthoracic cardioversion of persistent atrial fibrillation. Am J Cardiol. 2003; 92:988–991.
![]() 12. Page, RL, et al. Biphasic versus monophasic shock -waveform for conversion of atrial fibrillation. J Am Coll -Cardiol. 2002; 39:1956–1963.
12. Page, RL, et al. Biphasic versus monophasic shock -waveform for conversion of atrial fibrillation. J Am Coll -Cardiol. 2002; 39:1956–1963.
![]() 13. Sado, DM, et al. Comparison of the effects of removal of chest hair with not doing so before external defibrillation on transthoracic impedance. Am J Cardiol. 2004; 93:98–100.
13. Sado, DM, et al. Comparison of the effects of removal of chest hair with not doing so before external defibrillation on transthoracic impedance. Am J Cardiol. 2004; 93:98–100.
![]() 14. Scholten, M, et al. Comparison of monophasic and -biphasic shocks for transthoracic cardioversion of atrial -fibrillation. Heart. 2003; 89:1032–1034.
14. Scholten, M, et al. Comparison of monophasic and -biphasic shocks for transthoracic cardioversion of atrial -fibrillation. Heart. 2003; 89:1032–1034.
![]() 15. White, RD, et al. Transthoracic impedance does not affect defibrillation, resuscitation or survival in patients with -out-of-hospital cardiac arrest treated with non-escalating biphasic waveform defibrillator. Resuscitation. 2005; 64:63–69.
15. White, RD, et al. Transthoracic impedance does not affect defibrillation, resuscitation or survival in patients with -out-of-hospital cardiac arrest treated with non-escalating biphasic waveform defibrillator. Resuscitation. 2005; 64:63–69.