Orthopaedic Emergencies
Edited by Anne-Maree Kelly and Anthony Brown
4.1 Injuries of the shoulder
Crispijn van den Brand and Anne-Maree Kelly
Fractures of the clavicle
Fractures of the clavicle account for 2.6–5% of all fractures and usually result from a direct blow on the point of the shoulder, but may also be due to a fall on the outstretched hand. The most common site of fracture is the middle third of the clavicle, which accounts for 69–82% of clavicular fractures. Most other clavicular fractures are in the outer third. There are varying degrees of displacement of the fracture ends, with overlapping fragments and shortening being common. Owing to the strategic location of the clavicle, injury to the pleura, axillary vessels and/or brachial plexus is possible but, fortunately, these complications are rare. They should be excluded by directed examination.
The clinical signs of clavicular fracture are a patient supporting the weight of their arm at the elbow coupled with local pain and tenderness, often accompanied by deformity.
In non-displaced or minimally displaced fractures, treatment consists of an elbow- supporting sling (e.g. broad arm sling) for 2–3 weeks. For comfort, this may be worn under clothes for the first few days. The sling may be discarded when local tenderness has subsided. Note that clinical union usually precedes radiological union by weeks. Early shoulder movement should be encouraged within the limits of pain and immobilization should be discontinued if clinical union has occurred, even if there is not yet radiological union. Non-union is rare.
Midshaft fractures with complete displacement, comminution or fractures in the elderly or women with osteoporosis have a higher rate of non-union and poorer functional outcome. Recent evidence suggests that this group may benefit from surgical stabilization with either plate-and-screw fixation or intramedullary devices.
Fractures of the outer third of the clavicle may involve the coracoclavicular ligaments. These fractures are generally displaced. If so, surgical management should be considered because these fractures have a high incidence of non-union (30%). Displaced fractures of the medial third of the clavicle are often associated with other serious injuries and warrant further examination. Early orthopaedic consultation is recommended for all (displaced) fractures of the medial and outer third of the clavicle.
Late complications of clavicular fractures include shoulder stiffness and a local lump at the site of fracture healing, which is rarely of cosmetic significance.
Acromioclavicular joint injuries
Acromioclavicular (AC) joint injuries usually result from a fall where the patient rolls onto his/her shoulder. The degree of the injury relates to the number of ligaments damaged; about two-thirds of AC injuries are incomplete and involve only part of the AC and coracoclavicular ligaments (CC) (types I and II).
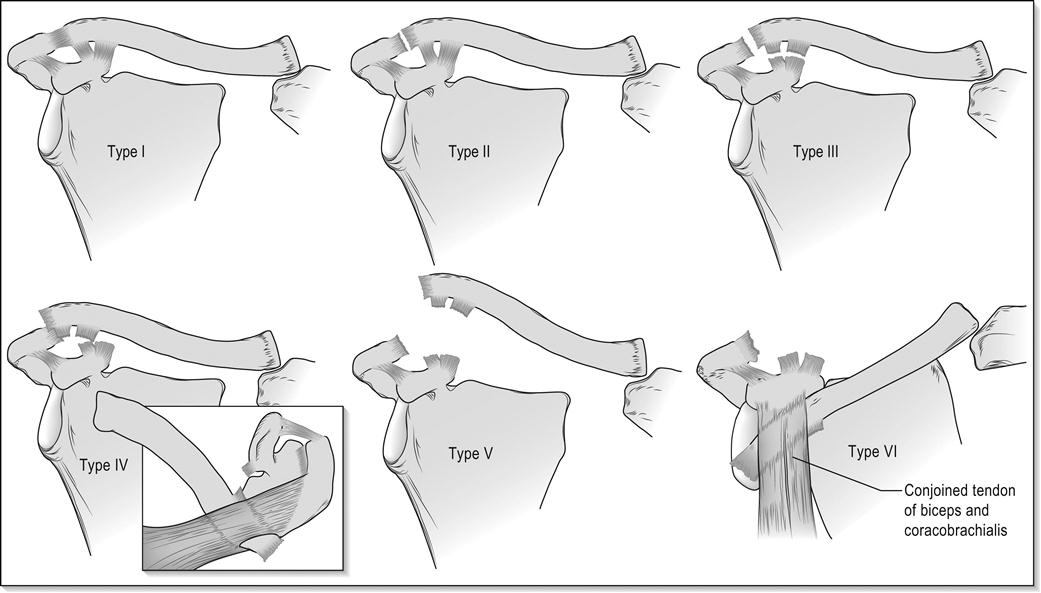
AC dislocations are classified according to the Tossy/Rockwood classification system (Fig. 4.1.1):
On clinical examination of the standing patient, the outer end of the affected clavicle may be prominent and there will be local tenderness over the AC joint. The degree of damage can be ascertained by taking standing X-rays of both shoulders with the patient holding weights in both hands (stress X-rays) and by ultrasound. Stress X-rays may be normal in mild strains, but dynamic ultrasonographic techniques may better define the injury.
Treatment is with a broad arm sling. For minor injuries (Rockwood type I/II) 1–2 weeks is usually sufficient. For type II injuries, heavy lifting and contact sports should be avoided for 4–6 weeks to avoid conversion to a type III injury. The treatment of type III injuries is controversial with some authors recommending conservative treatment and others surgery. Types IV to VI injuries are usually treated surgically.
Sternoclavicular subluxation and dislocation
Sternoclavicular dislocations are uncommon and usually due to a direct, high velocity blow to the medial clavicle or medial compression of the shoulder girdle. Subluxation is more common than dislocation, with the affected medial end of the clavicle displaced forwards and downwards. Dislocations may be anterior or, rarely, posterior. In the latter case, the great vessels or trachea may be damaged.
Clinical features include local tenderness and asymmetry of the medial ends of the clavicles. The diagnosis is essentially clinical. X-rays are difficult to interpret and are not necessary for subluxations. For dislocations, contrast enhanced CT scanning should be obtained.
Subluxations should be treated in a broad arm sling for 2–3 weeks. Anterior sternoclavicular joint instability should also be treated conservatively; however, there is a significant risk of ongoing instability that is usually well tolerated and of little, if any, functional impact. For patients with posterior dislocation, expeditious diagnosis and treatment are important. Closed reduction, performed under general anaesthesia, is usually stable and the joint can then be managed in a brace or sling for 4–6 weeks. Operative stabilization is required if closed reduction is unsuccessful or there is persistent instability.
Fractures of the scapula
Fractures of the scapula are uncommon, accounting for less than 1% of all fractures. They typically occur after high-energy trauma. Up to 90% of patients have other associated injuries.
Fractures of the blade of the scapula are most common and are usually due to direct violence. Clinical features are local tenderness, sometimes with marked swelling. Healing is usually rapid, even in the presence of comminution and displacement, with an excellent functional outcome. Treatment is usually non-operative, with a broad arm sling and early mobilization. There is growing acceptance of surgical treatment for highly displaced fractures. However, there is no evidence comparing outcome for surgical versus non-surgical treatment.
Fractures of the scapula neck are often comminuted and may involve the glenoid. Swelling and bruising of the shoulder may be marked. Clinical examination and X-rays should ensure that the humeral head is enlocated. Computed tomography (CT) scans may be useful in defining the anatomy and the degree of involvement of the glenoid, including any steps in the articular surface. Surgery is often indicated for fractures involving the scapular neck or glenoid.
The ‘floating shoulder’ is an uncommon injury pattern. Although it is usually defined as an ipsilateral fracture of the clavicle and scapular neck, recent studies suggest that ligamentous disruption associated with a scapular neck fracture can give the functional equivalent of this injury pattern, with or without an associated clavicle fracture. Because the degree of ligament disruption is difficult to assess, indications for non-surgical and surgical management are not well defined. Minimally displaced fractures typically do well with conservative management. The degree of fracture displacement and ligament disruption that results in poor outcome with conservative management is not well defined and the indications for surgery are controversial, as is choice of surgical technique. Options include fixation of the clavicular fracture, which often indirectly reduces the scapular fracture, or fixation of both fractures.
Supraspinatus tendon injuries
Rotator cuff tears most commonly affect the supraspinatus tendon and become more common with advancing age as degeneration weakens the cuff. Indeed, the presence of asymptomatic partial or complete tears identified on ultrasound or magnetic resonance imaging (MRI) may be as high as 40% in patients aged over 50.
Symptomatic injuries may follow minor trauma or the sudden application of traction to the arm. Many are acute or chronic in nature, rather than truly acute. This can be defined with ultrasound or MRI if required.
The clinical features of a strain include a painful arc of abduction centred at 90° of abduction, weakness in external rotation and tenderness under the acromion. If the tear is complete, no abduction at the glenohumeral joint will occur, although some abduction to 45–60% is possible by scapular rotation. In both partial and complete injuries, there is a full passive range of abduction. Another useful test to isolate the supraspinatus and test its integrity is the ‘empty can’ test. The patient abducts the arm to 30° with 30° of forward flexion and full internal rotation (i.e. thumb pointed down) and is then asked to forward flex the shoulder first without and then against resistance. Pain or weakness against resistance suggests supraspinatus injury.
The goals of emergency care for rotator cuff injuries are to provide pain relief and prevent further disability. For the acute symptoms, an arm sling can provide support but prolonged immobilization should be avoided. Treatment of supraspinatus tears is controversial, with no clear evidence guiding the choice of operative versus non-operative therapy or the components or duration of non-operative treatments. Most experts would still recommend a trial of non-operative therapy before considering surgery. An exception to this may be the patient with a previously asymptomatic shoulder who sustains trauma with resultant weakness (after the pain from the injury subsides) in whom imaging studies indicate an acute full-thickness tear.
Dislocation of the shoulder
Dislocation of the shoulder results in the humeral head lying anterior, posterior or inferior to the glenoid. Of these, anterior dislocation is the most common.
Anterior dislocation
Anterior glenohumeral dislocation is most often due to a fall resulting in external rotation of the shoulder, for example, the body rotating internally over a fixed arm. It is most common in young adults, often being related to sports. There is inevitable damage to the joint capsule (stretching or tearing) and there may be associated damage to the subscapularis.
Anterior dislocations are associated with several fractures including Hill–Sachs deformities, (bony) Bankart lesions and greater tuberosity fractures. A Hill–Sachs deformity is an impression fracture of the humeral head caused by the glenoid and is present in 35–100% of all anterior dislocations. It is unclear if this is prognostically important. Bony Bankart lesions are caused by a disruption of the glenoid labrum with an avulsion of the glenoid. These occur in about 5% of patients. Another common fracture is of the greater tuberosity of the humerus. Other complications may include damage to the axillary (circumflex) nerve (resulting in inability to contract deltoid and numbness over the insertion of deltoid) and, rarely, the axillary vessels and the brachial plexus.
Clinical features include severe pain, reluctance to move the shoulder and the affected arm being supported at the elbow, often in slight abduction. The contour of the shoulder is ‘flattened off’ and there is a palpable gap just under the acromion where the humeral head usually lies. The displaced humeral head may be palpable anteriorly in the hollow behind the pectoral muscles.
Dislocation is confirmed by X-ray. The dislocation may be evident on the AP film but cannot be ruled out on a single view. Additional views (e.g. an axial lateral, translateral, tangential lateral) are required. These may reveal an associated fracture of the greater trochanter, but this does not influence initial management.
The principles of management are the provision of adequate analgesia as soon as possible, reduction of the dislocation and immobilization followed by physiotherapy. There are more than 20 described methods for the reduction of anterior dislocations, with reported success rates ranging from 60 to 100%. These include the FARES technique, the Spaso technique, the modified Kocher’s manoeuvre, the Milch technique and scapular rotation techniques (www.youtube.com/watch?v=NXFPWxSTK5c). There is no high-quality evidence to assist in selecting the most effective method. That said, the Hippocratic method is not recommended as the traction involved may damage neurovascular structures. Gravitational traction (the Stimson technique), having the patient lie face down with a weight strapped to the limb, is occasionally successful and may be worthwhile if there will be a delay until reduction by another method. All reduction methods require adequate analgesia. Intra-articular local anaesthetic may also be useful. Sedation, in an appropriately controlled environment, may be of assistance in augmenting analgesia and providing a degree of muscle relaxation and amnesia, but is not required in most cases. Failure of reduction under analgesia/sedation is rare and mandates reduction under general anaesthesia.
If there is an associated fracture of the greater trochanter, it usually reduces when the shoulder is reduced. If it remains displaced, open reduction and internal fixation may be required.
Post-reduction X-rays confirm reduction and neurovascular status must be rechecked. Post-reduction care includes immobilization in a broad arm sling followed by physiotherapy. Available evidence suggests that there is no benefit from immobilization for more than 1 week. It was suggested that bracing in external rotation might reduce the incidence of recurrent dislocation but this has not been borne out in validation studies.
Primary surgery, usually by arthroscopic techniques, is recommended for patients having suffered recurrent dislocations and should be considered for first-time dislocators, especially those who are young, as surgery has been shown to significantly reduce the risk of recurrent dislocation.
Recurrence is rare in the elderly, but is common (64–68%) in young patients.
Reduction techniques (www.youtube.com/watch?v=NXFPWxSTK5c)
Most anterior glenohumeral dislocations can be reduced without anaesthesia or procedural sedation, although appropriate analgesia and a patient, gentle technique is required. Intra-articular lignocaine (lidocaine) has been shown to be a safe, effective alternative to procedural sedation for reduction of dislocated shoulders.
FARES technique
The patient may be in the supine or prone position. Hold the patient’s wrist and apply traction to the affected limb in a neutral position. Move the limb anteriorly and posteriorly in small oscillating movements (about 5–10 cm) while continuing to apply traction slowly abducting the limb. Once the limb is abducted to 90°, externally rotate the limb at the shoulder, with ongoing traction and oscillating anterior/posterior movements. Continue slowly to abduct the limb past this position. Reduction is usually achieved once the limb is abducted to about 120°. Success rate of the order of 89% has been reported.
Spaso technique
The patient is placed in the supine position. The affected arm is held by the forearm or wrist and gently lifted vertically, applying traction. While maintaining vertical traction, the shoulder is then externally rotated, resulting in reduction. If necessary, countertraction by downward pressure over the shoulder joint may be applied. Success rate of the order of 75% has been reported.
Modified Kocher’s manoeuvre
While applying traction to the arm by holding it at the elbow, the shoulder is slowly externally rotated, pausing if there is muscle spasm or resistance. External rotation to about 90° should be possible and reduction often occurs during this process. The elbow is then adducted until it starts to cross the chest and then internally rotated until the hand lies near the opposite shoulder.
Scapular rotation
This technique is traditionally performed with the patient prone, but can be performed on a seated patient. For both variations, the scapula is manipulated by adducting (medially displacing) the inferior tip using thumb pressure while stabilizing the superior aspect with the other hand.
Posterior dislocation
Posterior dislocation is frequently mentioned in medicolegal reports as it is easy to miss, especially in the unconscious patient. It may result from a fall on the outstretched or internally rotated hand or from a blow from the front. It is also associated with seizures and electrocution injuries, where it is not uncommonly bilateral. The dislocation is usually not apparent on an AP film, so additional views are required. Reduction is performed by traction on the limb in the position of 90° abduction, followed by external rotation. Aftercare is the same as for anterior dislocation.
Posterior dislocation is prone to recurrence. Good functional outcomes are associated with early detection and treatment, a small osseous defect and stability following closed reduction. Poor prognostic factors include late diagnosis, a large anterior defect in the humeral head, deformity or arthrosis of the humeral head, an associated fracture of the proximal part of the humerus and the need for an arthroplasty. The indications for surgery are controversial.
Inferior dislocation (luxatio erecta)
This type of dislocation is rare and usually obvious, as the arm is held in abduction. Neurovascular compromise is a significant risk requiring careful examination and prompt reduction. Reduction is by traction in abduction followed by swinging the arm into adduction. Aftercare is the same as for anterior dislocation.
4.2 Fractures of the humerus
Raymond Chi Hung Cheng and Timothy H Rainer
Introduction
The function of the upper limb depends on an intact shoulder girdle that is, in turn, affected by the integrity of muscles, tendons and ligaments, bones, joints, blood vessels and nerves. Fractures of the humerus severely limit efficient function of the upper limb and may be divided into proximal (proximal to the surgical neck), middle (shaft) and distal (supracondylar) segments.
Fractures of the proximal humerus
Patterns of injury
Fractures of the proximal humerus represent 5% of all fractures presenting to emergency departments (ED) and 25% of all humeral fractures. The fracture typically occurs as a result of an indirect mechanism in elderly, osteoporotic patients who fall on their outstretched hand with an extended elbow. The majority do not require surgical intervention and may initially be treated in the ED. A subset with a non-viable humeral head requires early surgical intervention and it is therefore important to identify this group. Fractures of the humerus may also occur in patients with multiple injuries or in the elderly with associated fractures of the neck of femur.
Clinical assessment
Patients typically present soon after injury holding their arm close to the chest wall. They complain of pain and exhibit swelling and tenderness of the shoulder and upper arm. Although crepitus and bruising may occur, the former should not be elicited because it causes excessive and unnecessary pain. Bruising is usually delayed, occurring several days after injury. It appears around the lower arm rather than at the fracture site as a result of gravity and blood tracking distally.
A neurovascular examination is essential as the axillary nerve, brachial plexus and/or axillary artery may be damaged. The axillary nerve is the most commonly injured and presents with altered sensation over the badge area (insertion of the deltoid) and reduced deltoid muscle contraction (which may be hard to assess because of pain). The axillary artery is the commonest vessel to be injured and may present with any combination of limb pain, pallor, paraesthesia, pulselessness and paralysis.
As these injuries frequently occur in elderly patients, careful attention must be paid to the reason for the fall, as an underlying acute medical condition may have precipitated the event and require management in its own right.
Clinical Investigations
Three radiographic views – anteroposterior, lateral and axillary – will allow most proximal humeral fractures to be correctly diagnosed.
Fracture classification
Although the majority of these fractures are easily managed in the ED, the challenge is to differentiate these from the minority that require orthopaedic intervention.
Neer classification system
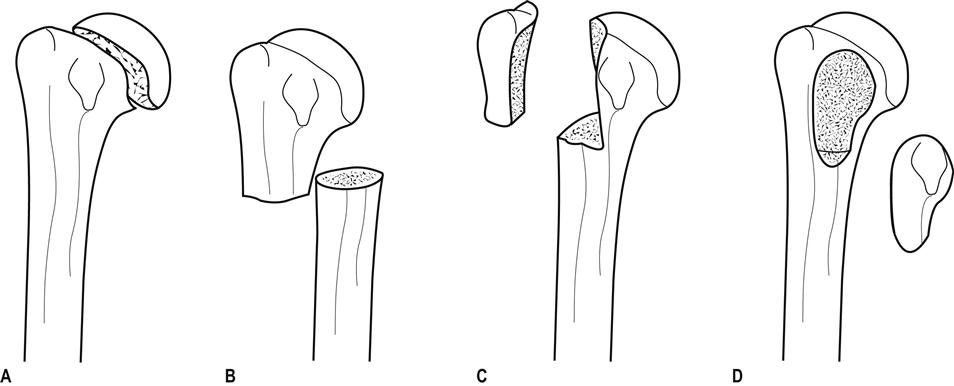
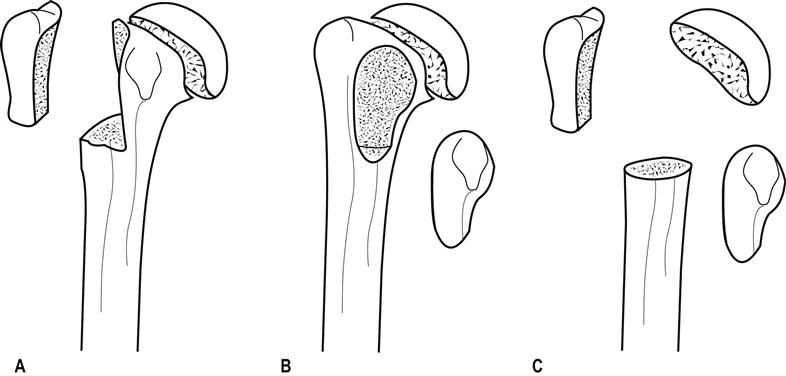
In this system, fractures are classified first according to the number of the four anatomical sites (humeral head, humeral shaft, greater and lesser tuberosities) that were involved in the injury; second, according to the degree of fracture displacement, defined as 1 cm separation or>45° angulation (Figs 4.2.1 and 4.2.2).
One-part fracture One-part fractures account for 80% of proximal humeral fractures. Any number of fracture lines may exist, but none are significantly displaced.
Two-part fracture Two-part fractures account for 10% of proximal humeral fractures and one fragment is significantly displaced or angulated. Two-part fractures of the humerus may involve the anatomical neck (see Fig. 4.2.1A), the surgical neck (see Fig. 4.2.1B), the greater tuberosity (see Fig. 4.2.1C) or the lesser tuberosity (see Fig. 4.2.1D).
Three- and four-part fractures Three-and four-part fractures account for the remaining 10% of proximal humeral fractures, with two or three significantly displaced or angulated fragments (see Fig. 4.2.2A–C).
Treatment
One-part fractures and two-part fractures can be treated with a collar and cuff sling, adequate analgesia and follow up. Early mobilization is important and the prognosis is good.
Definitive management of the displaced fragment in two-part fractures may include open or closed reduction depending upon neurovascular injury, rotator cuff integrity, associated dislocations, likelihood of union and function. Early orthopaedic assessment is recommended.
For three- and four-part fractures, the consensus is for open reduction and internal fixation. However, a review has suggested that there is little evidence that surgery is superior to the non-operative approach.
For displaced proximal humeral fractures, surgical management remains varied and controversial. A recent systematic review suggested that non-operative treatment of proximal humerus fractures has a high rate of radiological healing, good functional outcomes but a lower complication rate when compared with the operative approach. Small, randomized controlled trials suggest that external fixation may confer some benefit over closed manipulation and that conservative treatment is better than tension band osteosynthesis. Another study suggests that the decision should be made according to the viability of the humeral head. Locking plate technology may also provide better outcomes in patients with unstable displaced humeral fractures having a viable humeral head. Other small-scale studies suggest that some bandaging styles may be better than others and that early physiotherapy may improve functional outcome.
Special cases
Fracture of the anatomical neck and articular surface
Fractures at these sites are uncommon, but are important to recognize as they have a high incidence of compromised blood supply to the articular segment, may result in avascular necrosis and may require a humeral hemiarthroplasty.
Fracture dislocations
Fractures of the greater tuberosity accompany 15% of anterior glenohumeral dislocations and may be associated with rotator cuff tears. Although the fracture may be grossly displaced, reduction of the dislocated shoulder usually also reduces the fracture. In patients who require the full range of movement of their shoulders, surgical repair of the cuff may be required.
Fractures of the lesser tuberosity are associated with posterior glenohumeral dislocations.
Disposition
Most patients with undisplaced one- and two-part fractures may be discharged from the ED with a collar and cuff sling, analgesia, early mobilization and appropriate follow up. High-risk cases, including displaced three- and four-part fractures, all open fractures and the special proximal humeral fractures described above, require orthopaedic consultation and admission, as do those with medical problems requiring investigation or treatment.
Low-energy fractures, especially in the elderly, suggest the presence of osteoporosis. ‘At-risk’ patients not already identified as having osteoporosis should be referred for bone density scans, vitamin D testing and treatment.
Fractures of the shaft of humerus
Patterns of injury
Fractures of the humeral shaft commonly occur in the third decade (active young men) and in the seventh decade of life (osteoporotic elderly women). The commonest site is the middle third, which accounts for 60% of humeral fractures. The close proximity of the fracture to the radial nerve and brachial artery commonly leads to neurovascular deficits.
Direct blows tend to produce transverse fractures, whereas falls on the outstretched hand produce torsion forces and hence spiral fractures. Combinations of the two mechanisms may produce a butterfly segment. Pathological fractures are also common, most resulting from metastatic breast cancer.
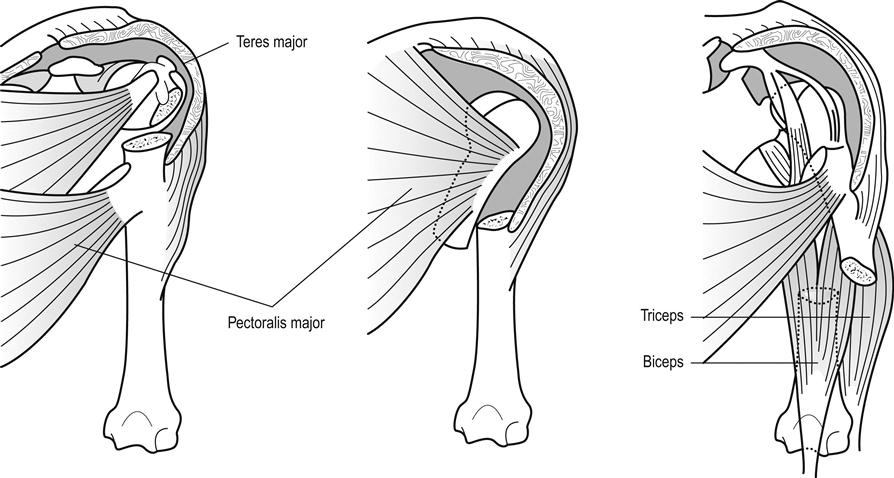
The angle and degree of displacement of the fracture depends on the site of injury and its relationship to the action and attachment of muscles on either side of the injury (Fig. 4.2.3).
Clinical assessment
Patients typically present complaining of pain and supporting the forearm of the injured limb, flexed at the elbow, and held close to the chest wall. Examination of the limb reveals tenderness, swelling, shortening and possibly deformity. The skin should be assessed for tension or disruption and particular attention should be paid to the shoulder and elbow regions for associated fractures or dislocations. Initial and post-reduction assessments of the brachial artery and vein and ulnar, median and radial nerves are essential.
The commonest complication is radial nerve injury resulting either from the injury itself or reduction of the fracture and is evidenced by wrist drop and altered sensation in the first dorsal web space. A recent systemic review reported that radial nerve injury occurs in 11% of midshaft humerus fractures.
Clinical investigations
Two radiographic views – anteroposterior and lateral – will allow the correct diagnosis in most cases.
Treatment and disposition
Uncomplicated, closed fractures account for the majority of injuries and may be treated conservatively by immobilization and analgesia. Immobilization can be by a hanging cast, U-shaped cast or with functional bracing and a broad arm or collar and cuff sling. The acceptable deformity is 20° anterior/posterior angulation and 30° valus/valgus deformity. The rate of fracture union is usually higher than 90%. Early specialist follow up is recommended.
Some authors prefer a functional humeral brace rather than U-shaped plaster for immobilization, as the former may permit greater functional use without affecting healing or fracture alignment. For oblique/spiral fractures, some orthopaedic surgeons prefer an operative approach for a better functional outcome.
Open fractures and complications affecting the vessels require surgical repair. Although the majority of radial nerve injuries are neuropraxia and recover without surgical intervention, each case should be considered individually by an orthopaedic surgeon with a view to possible operative exploration.
Fractures of the distal humerus
Classification and patterns of injury
Unlike in children, fractures of the distal humerus in adults are very uncommon and patterns of injury tend to reflect the anatomical two-column construction (condyles) of the humerus. Several classification methods have been used, such as the Riseborough and Radin, Mehne and Matta classifications, but the simplest and most commonly used are the AO/ASIF classifications. These classify injuries into three categories: type A are extra-articular fractures, type B are partial articular and type C are complete articular fractures. Practically, distal humeral fractures may be classified into supracondylar, intercondylar and other types. Supracondylar fractures lie transversely, whereas intercondylar T or Y fractures include an additional vertical extension between the condyles.
Mechanisms of injury usually involve a direct blow to the flexed or extended elbow. In the former, the olecranon is driven upwards, thereby either splitting the condyles apart producing a ‘T’ or a ‘Y’ pattern, or shearing off one condyle.
Clinical assessment
Patients typically present with a swollen, tender, deformed elbow. As very little subcutaneous or other tissue separates the bone from skin, any disruption of the skin should be carefully examined for the possibility of a compound fracture. Distal neurological and vascular injury must be assessed carefully, as the possibility of nerve injury has been reported to be as high as 12–20%.
Clinical investigations
Two radiographic views – anteroposterior and lateral – should be obtained. Some authors suggest that an internal oblique view may improve the diagnostic accuracy. Pain and inability to extend the elbow often result in poor-quality radiographs. Although high-quality radiographs are essential for operative planning, repeat films should not be attempted in the ED as they rarely provide the desired result. When there is any suspicion of severe injury, either from the history or from gross soft- tissue swelling, early computed tomography (CT) scanning should be considered to give better detail, especially of intra-articular fractures.
Undisplaced fractures may not be visible on radiography but may be suggested by posterior or anterior fat pad signs, which result from fat displaced by an underlying haemarthrosis. Ultrasonography, CT and magnetic resonance imaging may all improve diagnostic precision. They alter management and improve outcome in patients with occult fractures, mostly of the intra-articular type.
Treatment and disposition
Uncomplicated, undisplaced, closed fractures with minimal swelling should be immobilized for 3 weeks in 90° flexion with an above-elbow cast and a broad arm sling, followed by active mobilization.
Patients with severe swelling, compound fractures, displaced fractures or neurovascular compromise require orthopaedic intervention.
4.3 Dislocations of the elbow
Raymond Chi Hung Cheng and Timothy H Rainer
Introduction
Elbow dislocation, along with glenohumeral and patellofemoral joint dislocations, is one of the three most common large joint dislocations. The elbow joint is a hinge-like articulation involving the distal humerus and proximal radius and ulna. Owing to its strong muscular and ligamentous supports, the joint is normally quite stable and rarely requires operative intervention, even for acute instability after dislocation.
Elbow dislocations can be classified as either anterior or posterior. Posterior dislocation is the most common type and can be further divided into posteromedial or posterolateral. It usually results from a fall on the outstretched hand with some degree of flexion or hyperextension at the elbow. The radius and ulna commonly dislocate together. Similarly, anterior dislocation can also be divided into anteromedial or anterolateral. This type is less common and is usually due to a direct blow to the dorsal side of the elbow.
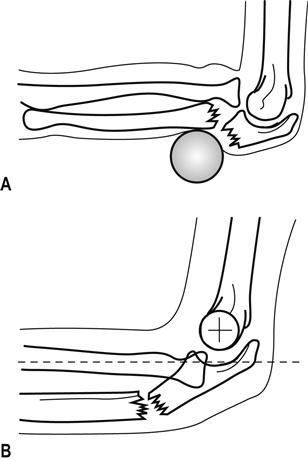
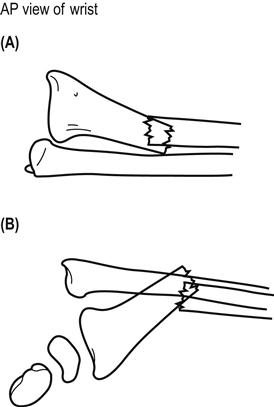
Uncommonly, the radius or ulna alone may dislocate at the elbow. In such cases, there is always a fracture of the other bone. One common example is in Monteggia fractures, where anterior or posterior radio-humeral dislocation occurs alongside a fracture of the proximal one third of the ulna shaft (Fig. 4.3.1). A rarer example is a posterior ulna-humeral dislocation with fracture of the radial shaft. So, although elbow dislocations may appear to be isolated, it is essential to look for associated intra-articular or shaft fractures.
Clinical assessment
History and examination
Patients typically present holding the lower arm at 45° to the upper arm and there is swelling, tenderness and deformity of the elbow joint. The three-point anatomical triangle of olecranon, medial and lateral epicondyles should be assessed for abnormal alignment, as this strongly suggests dislocation.
The commonest neurovascular injury involves the ulnar nerve, reported in 10–15% of elbow dislocations, but the median and radial nerves and the brachial artery may also be affected.
The differential diagnosis is a complex distal humerus fracture which, in a swollen elbow, may be hard to differentiate clinically from an elbow dislocation.
Clinical investigations
Anteroposterior and lateral radiographic views should be obtained and scrutinized for associated fractures of the coronoid process, radial head, capitellum and olecranon.
Magnetic resonance imaging (MRI) characterizes bony injury more accurately than radiography in children with elbow injuries, but its potential role for diagnosis and guiding management in adults has not been well evaluated. Duplex Doppler ultrasound can be use to identify early brachial artery injury.
Treatment
Simple dislocation can be reduced using a closed method. With adequate sedation, gentle traction and counter-traction, the joint relocates quite easily. Medial and posterolateral dislocations may also require sideways correction. Dislocation of the stable elbow joint produces severe soft-tissue injury and resultant instability, therefore, after reduction, signs and symptoms of compartment syndrome should be sought.
Joint instability should be tested by valgus and varus testing and by lateral pivot-shift test. The reduced elbow joint should move smoothly. Any crepitation or resistance, particularly during the mid-range, suggests incongruent reduction or soft tissue interposition, which is commonly associated with coronoid process or epicondylar fractures. Inability to fully flex or extend the elbow suggests a loose bone or cartilaginous fragment or a capsular tear.
Post-reduction films should be assessed, not only for correct joint relocation, but also for associated fractures. After successful reduction, the elbow should be placed in a posterior plaster slab in 90° of flexion. Cylinder casts are contraindicated because of the likelihood of severe soft-tissue swelling.
There is little evidence that surgical intervention improves outcome in patients with medial or lateral elbow instability after dislocation. A recent systematic review found that there is no difference in outcome between surgical repair of the ligament and plaster immobilization for simple elbow dislocation. Patients with functional treatment have a better range of movement, less pain, better functional scores, shorter disability and shorter treatment time when compared with plaster immobilization. The management of Monteggia fracture- dislocation is discussed in Chapter 4.4. Compound fracture dislocation should be reduced by the open method. Patients with irreducible dislocations, neurovascular complications, associated fractures or open dislocations require orthopaedic intervention.
Ulnar nerve injuries can occur both before and after closed reduction. The reported rate varies between 10 and 15%. Most of them are neuropraxia and will recover with conservative measures. The most sensitive sign and symptoms are numbness over the little fingers.
Disposition
Current practice is that most patients may be discharged from the emergency department with analgesia, pressure bandage for stable joints and plaster immobilization for unstable joints. A broad arm sling with appropriate follow up should be arranged after reduction.
A recent prospective, randomized study suggested that early mobilization is superior to plaster immobilization in terms of functional recovery, without any increased instability or a recurrence of dislocation for patients with uncomplicated posterior dislocations. The duration of immobilization should not be longer then 14 days to prevent joint stiffness. Patients with irreducible dislocations, neurovascular complications, associated fractures or open dislocations require admission.
4.4 Fractures of the forearm and carpal bones
Crispijn van den Brand
Radial head fractures
Clinical features
History
Radial head fractures occur frequently, usually as a result of a fall onto an outstretched hand or, less frequently, following a direct blow to the lateral side of the elbow. Radial head fractures present with pain and restricted movement at the elbow.
Examination
Usually, there is swelling and tenderness over the radial head. Sometimes, with more subtle injuries, rotating the forearm while palpating the radial head may be necessary to elicit tenderness. Elbow extension and forearm rotation are limited. Severely comminuted fractures may have proximal displacement of the radius, which can be associated with disruption of the interosseous membrane and subluxation of the distal radioulnar joint (Essex–Lopresti fracture dislocation).
Clinical investigations
Imaging
Standard anteroposterior (AP) and lateral X-rays of the elbow are required. A radiocapitellar view may be necessary if the fracture is subtle. The presence of an anterior fat pad sign alone on X-ray is associated with an underlying radial head or neck fracture in up to 50% of patients. In this case, a fracture should be assumed to be present if there is an appropriate mechanism and local signs. A follow-up X-ray or computed tomography (CT) scan is indicated only in the presence or persistent pain, stiffness or locking.
Classification
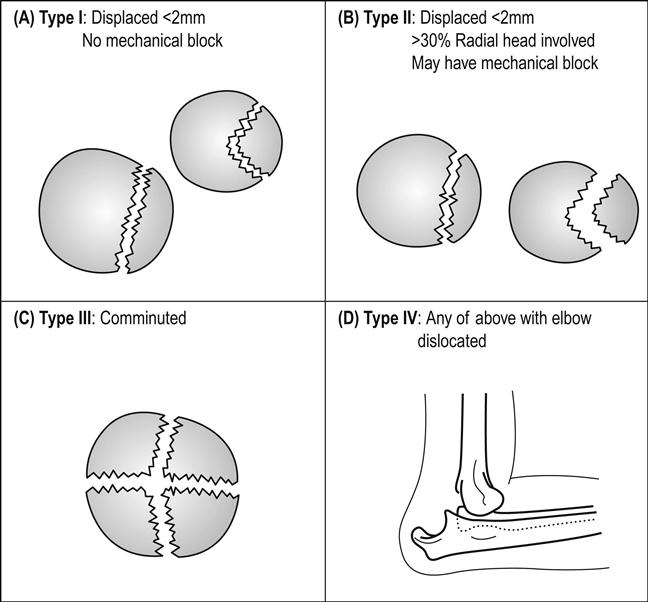
Radial head fractures are usually classified according to the (modified) Mason classification (Fig. 4.4.1). About two-thirds of fractures are Mason type I.
Treatment
All non-displaced (type I) radial head fractures and those type II fractures without mechanical block may be managed with a bandage and sling. Mobilization should be started as early as possible. If there is severe pain, a posterior splint may be useful but should not be applied for more than 2 days. Prognosis is good, but full extension may not be possible for many months.
Displaced or complex radial head fractures (type II or III) may be treated in the acute setting with a sling or posterior splint. These patients should have early orthopaedic review (within days). The treatment of displaced or complex radial head fractures remains controversial and should be determined by an orthopaedic surgeon.
Mechanical block can be difficult to assess acutely due to pain. Intra-articular injection of bupivacaine may assist early assessment or assessment may be deferred until pain has settled. Surgical options include open reduction and internal fixation and excision of the radial head with or without implantation of a prosthesis.
Radial neck fractures with up to 20° tilts can be managed conservatively. More severe tilt can be reduced using intra-articular local aneasthesia. The forearm is pronated until the most prominent part of the radial head is felt. Then traction is applied to the forearm and pressure applied to the radial head. Open reduction is indicated if closed methods fail or displacement is severe.
Complications
Neurovascular complications and compartment syndrome are uncommon. Most complications relate to disturbance of the relationships of the proximal radio-ulnar and radiocapitellar articular surfaces causing limitation of movement. This is uncommon with minor fractures.
Shaft fractures
Clinical features
History
This type of injury requires great force, typically from a motor-vehicle accident, a fall from a height or a direct blow. These fractures are commonly open and nearly always displaced.
Examination
The forearm is swollen and tender and may be angulated and rotated. Examination looking for an open wound, local neurovascular compromise, compartment syndrome or musculotendinous injury is required. Given the mechanism of injury, other injuries should also be sought.
Clinical investigations
Imaging
AP and lateral X-rays of the forearm, including the wrist and elbow joints, are needed. Displacement and angulation are easily determined, but torsional deformity may be subtle. Because the ulna and radius are rectangular in cross-section rather than circular, a change in bone width at the fracture site indicates rotation. The radial and ulnar styloid processes normally point in opposite directions to the bicipital tuberosity and coronoid process, respectively. A change in this alignment also suggests torsion.
Treatment
Adult forearm fractures are less stable than those in children and lack of remodelling limits tolerance to incomplete reduction. Undisplaced fractures may be managed with an above- elbow cast, but must be reviewed at 1 week for displacement and angulation. Most fractures, however, are displaced and require open reduction and internal fixation.
Complications
Early complications include wound infection, osteomyelitis, neurovascular injury and compartment syndrome. Later, non-union, malunion, reduced forearm rotation and reflex sympathetic dystrophy are possible complications.
Specific fracture types
Isolated fracture of the ulnar shaft
These fractures are due to a direct blow to the ulna, often when raised in defence; hence they are also known as ‘nightstick’ fractures. Patients present with localized pain and swelling. AP and lateral X-rays delineate the location of the fracture and degree of angulation. Look for associated dislocation of the radial head if displacement is present (Monteggia fracture dislocation).
Fractures displaced less than 50% of the ulna width heal well with a non-union rate of 0–4%. Traditional treatment involves fixing the forearm in mid-pronation with a plaster cast, extended above elbow if the middle or proximal thirds of the ulna are fractured. The cast is removed once union occurs, usually in about 8 weeks. Other proven options include a below-elbow plaster (BEPOP) for proximal fractures, early mobilization with bandage after 1–2 weeks in BEPOP or functional bracing after 3–5 days, which allows movement at wrist and elbow.
Fractures with more than 10° of angulation or displaced more than 50% of the diameter of the ulna require surgical intervention.
Monteggia fracture dislocation
This is a rare fracture of the proximal ulna with dislocation of the radial head. It occurs either through a fall onto the outstretched hand with hyperpronation or through a force applied to the posterior aspect of the proximal ulna. Patients present with pain, swelling and reduced elbow movement. The forearm may appear shortened and the radial head may be palpable in the antecubital fossa. Associated posterior interosseous nerve injury is common.
On X-ray the fracture is obvious, but the dislocation is commonly missed. Check that a line through the radial shaft bisects the capitellum on both views. There are four types of Monteggia fracture depending upon displacement of the radial head (Bado classification). Dislocation is anterior in 60% (Bado type I), but may be lateral or posterior.
All Monteggia fractures require open reduction and internal fixation. Common complications include malunion and non-union of the ulnar fracture and an unstable radial head.
Isolated radial shaft fracture
Isolated fractures of the proximal two-thirds of the radial shaft are uncommon and are usually displaced. Rare undisplaced fractures can be treated similarly to isolated ulnar shaft fractures. Displaced fractures require open reduction and internal fixation.
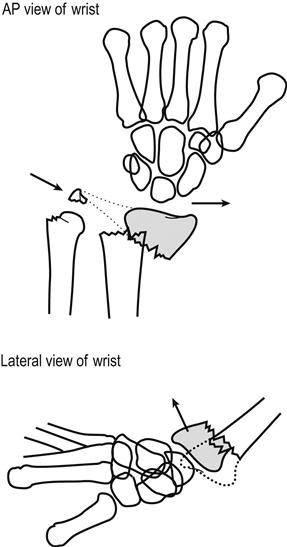
Galeazzi fracture dislocation
Fractures of the distal third of the radial shaft occur as a result of a fall onto the outstretched hand or a direct blow. There may be an associated subluxation or dislocation of the distal radioulnar joint (DRUJ), known as the Galeazzi fracture dislocation. Patients have pain and swelling at the radial fracture site. Those with a Galeazzi injury will also have pain and swelling at the DRUJ and a prominent ulnar head.
X-rays show the radial fracture, which is tilted ventrolaterally. Widening of the DRUJ space on the AP X-ray and dorsal displacement of the ulnar head on the lateral X-ray are seen (Fig. 4.4.2). An ulnar styloid fracture is seen in 60% of cases.
All Galeazzi fracture dislocations require surgical management. Complications include malunion or non-union of the radial fracture and subsequent instability of the DRUJ.
Fractures of the distal radius and ulna
Fractures of the distal radius and ulna are common, particularly in children and elderly women. Fractures in the latter group are indications for evaluation of bone-mineral density.
Clinical features
History and examination
Fractures usually occur after a fall onto the outstretched hand resulting in bending, shearing or impaction forces being applied to the distal metaphysis, or from a direct blow. Patients present with pain, tenderness and variable degrees of swelling and deformity. It is important to examine for associated injuries to carpal bones, radial and ulnar shafts, elbow and shoulder joints, for median nerve injury, vascular compromise and for extensor tendon injury.
Clinical investigations
Imaging
Anteroposterior and lateral X-rays of the wrist demonstrate most injuries. For patients with significant symptoms or signs and a normal X-ray, consider an occult undisplaced fracture or ligamentous injury.
Although this chapter uses eponymous names, it is important to be aware that orthopaedic circles have moved to more formal classification systems for distal radial fractures. Several have been proposed and are beyond the scope of this text. The author recommends being familiar with anatomical descriptions and fracture features associated with need for reduction, instability of reduction and indications for operative intervention.
Treatment
Management
Prompt attention to analgesia, splinting and elevation is essential while awaiting X-rays.
Reduction is indicated in the following circumstances to improve long-term function:
 visible deformity of the wrist
visible deformity of the wrist
 loss of volar tilt of the distal radial articular surface beyond neutral
loss of volar tilt of the distal radial articular surface beyond neutral
 loss of>5° of the radial inclination of the distal radius (normally approximately 20°)
loss of>5° of the radial inclination of the distal radius (normally approximately 20°)
Greater deformity can be accepted in low-demand, elderly patients.
Anaesthetic options for reduction include haematoma block, Bier’s block and procedural sedation. Reduction is traditionally maintained with an encircling plaster cast moulded to oppose displacement forces and extending from volar metacarpal crease to proximal forearm for 6 weeks. Displaced or comminuted fractures at high risk of swelling, especially in the elderly or coagulopathic patients, are immobilized with non-encircling splints.
Factors associated with instability of the distal fragment and failure to maintain reduction include:
 intra-articular component (especially involving the distal radio-ulnar joint)
intra-articular component (especially involving the distal radio-ulnar joint)
 shearing fractures (Barton-, Hutchinson’s type)
shearing fractures (Barton-, Hutchinson’s type)
Weekly X-rays for 2–3 weeks with orthopaedic follow up are recommended for all displaced fractures, those with intra-articular extension and potentially unstable fractures.
Stable, undisplaced, extra-articular fractures can be managed more conservatively with splinting and referral to a family doctor for early mobilization after 4 weeks.
Indications for operative management are debated, but should be considered for:
Complications
Median nerve injury may occur acutely due to the injury, as a result of reduction or later due to pressure effects from the plaster. Median nerve function must be documented before and after reduction.
Loss of reduction may require delayed surgical intervention. Malunion with chronic wrist pain, arthritis and secondary radioulnar and radiocarpal instability are associated with intra-articular extension of the fracture.
Long-term complications include osteoarthritis, residual disability and complex regional pain syndrome (CRPS). The incidence of CRPS following distal radius fractures ranges in the literature from less than 1% to 22%. Prophylactic vitamin C may reduce the incidence of CRPS, the advised dose is 500 mg/day for 50 days.
Specific fractures
Colles’ fracture
Colles’ fracture is a metaphyseal bending fracture. The wrist has a classic ‘dinner-fork’ appearance, often with significant swelling of the soft tissues. This appearance is reflected in the radiographs (Fig. 4.4.3). There is often associated damage to the radio-ulnar fibrocartilage. There may be comminution, commonly dorsally, which can extend into the radiocarpal or radio-ulnar joints.
The aim of reduction is to restore radial length, volar tilt and radial angulation. A minimum of 0° tilt is acceptable if full reduction is not possible. Reduction is achieved by first disimpacting the fracture with traction in the line of the forearm. If this fails, traction in extension or hyperextension should be tried. Volar tilt is then restored with volar pressure over the dorsum of the distal fragment while traction is maintained. Lastly, correct radial tilt and radial displacement with ulnar pressure over the radial side of the distal fragment. Reduction is successful in 87%, but almost two-thirds lose reduction over 5 weeks, most of this occurring during cast immobilization.
The commonly accepted cast immobilization position is with the wrist joint in 15° palmar flexion, 10–15° ulnar deviation and slight pronation. However, some evidence suggests better outcomes are achieved with the wrist in dorsiflexion and mid-supination. The cast must be carefully moulded over the dorsum of the distal fragment and the anteromedial forearm. Functional bracing allowing wrist movement has also shown good outcomes.
Smith’s fracture
This metaphyseal bending fracture of the distal radius occurs through a direct blow or fall onto the back of the hand or a fall backward onto the outstretched hand in supination.
AP and lateral X-rays of the wrist show a ‘reverse Colles’ fracture’ with a similar AP appearance, but with volar displacement and tilt on the lateral X-ray view.
Closed reduction to achieve anatomical radial length and volar tilt should be attempted. Traction is first applied to restore length, followed by dorsal pressure over the volar surface of the distal radius to reverse displacement and angulation. A full above-elbow cast is applied with the wrist in supination and dorsiflexion to prevent loss of reduction. However, most Smith’s fractures are unstable and require operative management. Early orthopaedic follow up is mandatory.
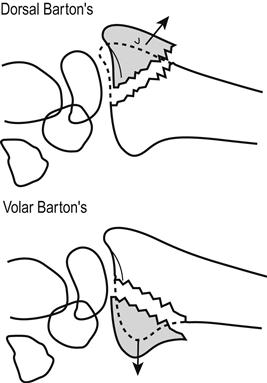
Barton’s fracture
Barton’s fractures are dorsal or volar intra- articular fractures of the distal radial rim (Fig. 4.4.4). The mechanisms of injury are similar to those seen with Colles’ and Smith’s fractures, respectively. There is often significant soft-tissue injury and the carpus is usually dislocated or subluxed along with the distal fragment. These fractures are complicated by arthritis of the radiocarpal joints and carpal instability.
Minimally displaced fractures involving less than 50% of the joint surface and without carpal displacement may be reduced along the lines of a Colles’ or Smith’s fracture. Immobilization should occur with wrist flexed for dorsal Barton’s and extended for volar Barton’s. However, most fractures are unstable and potentially disabling, requiring early operative management, especially in younger patients. Early orthopaedic follow up is mandatory.
Radial styloid (Hutchison’s or chauffeur’s) fracture
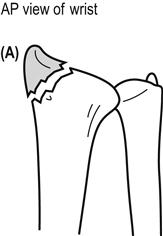
This oblique intra-articular fracture of the radial styloid is caused by a direct blow or fall onto the hand. Displacement is associated with carpal instability and long-term arthritis. The fracture is seen best on AP X-rays of the wrist (Fig. 4.4.5). Undisplaced fractures can be treated with a cast for 4–6 weeks. Displaced fractures should be referred to an orthopaedic surgeon for anatomical reduction and fixation.
Ulnar styloid fracture
An isolated fracture can occur through forced radial deviation, dorsiflexion, rotation or a direct blow. Avulsion fractures involving the lesser portion of the ulnar styloid are not associated with significant instability of the distal radio- ulnar joint (DRUJ). In contrast, fractures involving the base of the ulnar styloid disrupt the major stabilizing ligaments of the distal ulna and the triangular fibrocartilage complex (TFCC) and may lead to subsequent DRUJ instability. Fractures should be treated with a splint or cast with the wrist in mid-supination and ulnar deviation, patients should be referred to an orthopaedic surgeon to assess DRUJ stability.
Carpal fractures and dislocations
Carpal fractures predominantly occur in young men. The bones in the proximal carpal row are more commonly involved, especially scaphoid fractures which account for 82–89% of all carpal fractures. Most other isolated carpal fractures are triquetral fractures. Management depends on the degree of displacement and damage and stability. Generally, undisplaced fractures with minimal comminution can be managed by cast immobilization. Given the importance of wrist function, early orthopaedic review should be sought for patients with displaced or comminuted fractures or where instability or an associated carpal dislocation is suspected.
Specific fractures
Scaphoid fracture
The most common mechanism of injury is a fall on the outstretched hand with the wrist in radial deviation. This mechanism also puts the distal radius and the scaphoid-lunatum (SL) ligament at risk. Clinical features include wrist pain and local swelling and tenderness over the scaphoid, palpated dorsally or via the anatomical snuffbox. Imaging with AP, lateral and scaphoid views will detect at most 70% of all scaphoid fractures.
Fractures of the scaphoid are classified by their location (proximal third, waist, distal third or tubercle) and by their stability. Stable fractures are undisplaced with little comminution and unstable fractures are displaced with considerable comminution. Stable fractures are generally treated with a below-elbow cast for 10–12 weeks. There is no evidence that cast immobilization with inclusion of the thumb leads to better outcome. Unstable fractures require surgical intervention. Complications include non-union and avascular necrosis of the proximal segment.
Some patients have clinical features suggestive of scaphoid fracture without confirmatory X-ray evidence. In the past, cast immobilization for 1–2 weeks followed by repeat X-ray was advocated. Although this is still advocated by some, it is not recommended. The additional sensitivity is low and scaphoid fractures are often missed. A number of alternative diagnostic approaches have been suggested, including bandaging with clinical review at 7–10 days followed by CT if clinical features persist, or early primary CT, magnetic resonance imaging (MRI) or bone scintigraphy. All of these imaging modalities have their advantages and shortcomings. Bone scintigraphy is recommended as a useful diagnostic modality to rule out occult scaphoid fractures. Bone scintigraphy can rule out scaphoid fracture with a sensitivity close to 100% but with the disadvantage of up to 25% false positives.
Dislocations of the wrist
Dislocations involving the wrist usually result from high-energy falls on the outstretched hand (such as from a height) that result in forced hyperextension. The distal row of carpal bones is commonly displaced dorsal to the proximal row as a result of a scaphoid fracture, a scapholunate dislocation or a perilunate dislocation. Trans-scaphoid perilunate fracture dislocation is slightly more common than perilunate dislocation.
Clinical features
Clinical features include mechanism of injury, wrist pain, swelling and tenderness and possibly reduced grip strength.
Clinical investigations
Imaging requires PA and lateral X-rays. The normal PA view should show two rows of carpal bones in a normal anatomic position with uniform joint spaces of no more than 1–2 mm. No overlap should be seen between the carpal bones or between the distal ulna and the radius. On the lateral film, a longitudinal axis should align the radius, the lunate, the capitate and the third metacarpal bone.
Radiographic features include:
Treatment
All wrist dislocations require orthopaedic consultation and prompt reduction.
4.5 Hand injuries
Peter Freeman
Introduction
Hand injuries are common and up to 10% of emergency department (ED) attendances involve injury to the hand. Presentations may be due to wounds (≈35%), contusions (≈20%), fractures (≈20%), sprains (≈10%) or infections (≈5%). Males injure their hands more than females. The complex anatomy and tactile function of the hand mean that hand injuries can profoundly affect an individual. The importance of correct assessment and care of hand injuries cannot be overstated. Apart from the initial pain and trauma, occupational and psychological concerns play a major role in the aftermath of these injuries. Even a relatively minor fingertip injury can result in an individual being away from work for several days, with consequent loss of earnings and concerns for long-term function and appearance. It is therefore essential that initial assessment and management are appropriate. The role of ED management is as much about identifying cases that require specialist referral as it is about treating straightforward injuries.
Clinical features
History
Time taken eliciting a focused history of the mechanism of injury is essential in cases of hand injury. Key questions include:
 What was the position of the hand at the time?
What was the position of the hand at the time?
 What was the environment of the injury?
What was the environment of the injury?
 Is it likely that the wound is contaminated or contains foreign material, such as glass?
Is it likely that the wound is contaminated or contains foreign material, such as glass?
Injury to the dominant hand should be noted as well as occupation and key leisure activities. It is also important to record medications and allergies to guide analgesia and antibiotic choice. Tetanus prophylaxis status should be determined.
Examination
The injured hand must be examined in a well-lit area. Temporary dressings may need to be soaked off if they have been allowed to dry out and become adherent. At triage, an initial moist dressing is preferred, with firm pressure and elevation if there is significant bleeding.
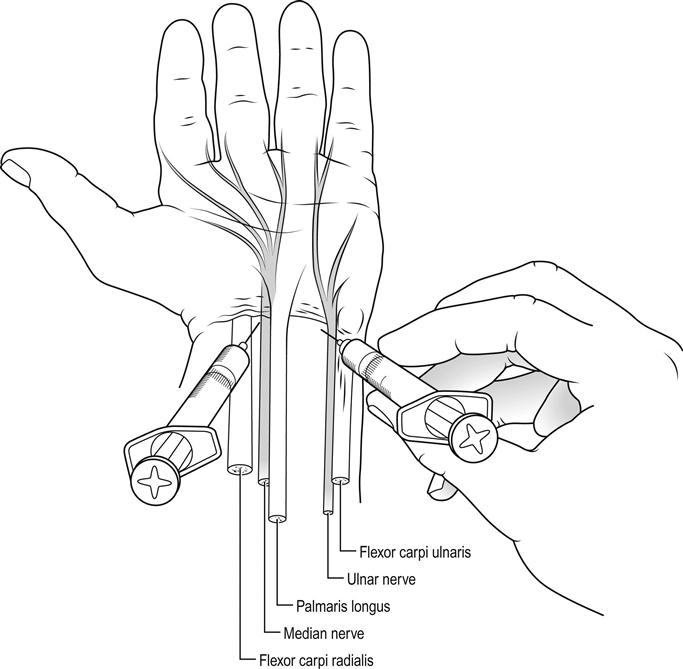
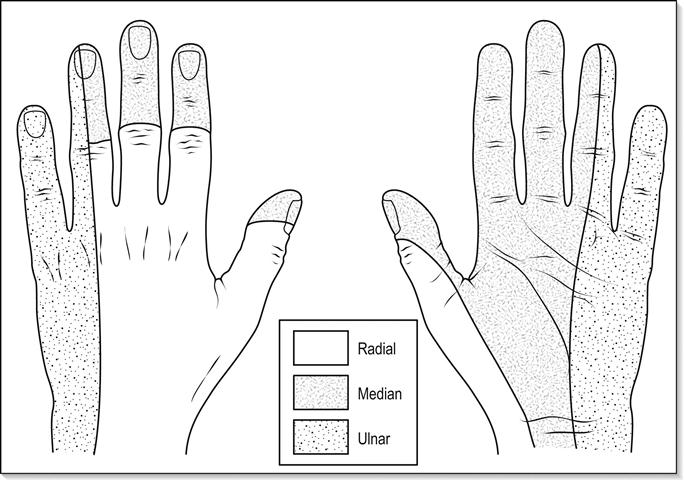
Hand and finger injuries are painful and suitable analgesia should be given prior to full examination. Local infiltration of local anaesthetic without adrenaline around a wound or as a digital nerve block will allow examination of all aspects except sensation, which must be tested and recorded prior to anaesthesia. A wrist block is useful when some or all of the hand needs to be anaesthetized (Fig. 4.5.1). In this instance, longer-acting local anaesthetic is generally used to prolong the effect.
Testing sensation is achieved by point touch in the distribution of the three main nerves that supply the hand (Fig. 4.5.2). The median nerve supplies the palmar aspect of the thumb, index, middle and half of the ring finger, extending to supply the fingertip and nailbed. The ulnar nerve supplies both palmar and dorsal aspects of the other half of the ring finger and the little finger. The radial nerve supplies the radial dorsum of the hand, thumb, index, middle and radial aspects of the ring finger. If the patient is unable to describe sensation because they are too young or unconscious, it is useful to remember that the digital nerves also carry the sympathetic supply to the fingers and that division will cause a dry finger in the distribution of the digital nerve.
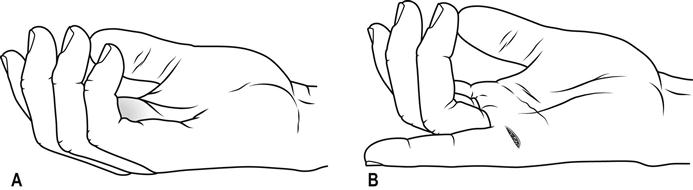
The hand examination should be holistic and not just concentrate on the obvious injury. Inspection of the hand will provide information about the perfusion of the tissues, local swelling and position of wounds. The resting position of the hand may be a clue to tendon injury, as the normal uninjured position is held with the fingers in increasing flexion from the index to the little finger (Fig. 4.5.3A). A pointing finger may indicate a flexor tendon injury (Fig. 4.5.3B). Testing for pinch grip is important if there is concern about the stability of the first metacarpal. Obvious bone or joint deformity should be recorded. The metacarpals and phalanges are all easily palpable subcutaneously and local tenderness may indicate underlying fracture.
Functional testing should be performed for all injured hands. Tendon integrity is tested by asking the patient to perform specific movements. Some tendon injuries may be obvious, however, two flexor tendons supply each finger and simply asking the patient to flex the finger will not exclude a divided flexor digitorum superficialis tendon. The profundus tendon flexes the distal interphalangeal joint and is tested by asking the patient to flex the tip of each finger in turn while the examiner holds the proximal interphalangeal joint in extension. The superficialis flexor tendon is tested by asking the patient to flex each finger individually, while the examiner holds the other fingers straight. The extensor tendons to the fingers are tested by asking the patient to extend the fingers against resistance. It is important to remember that the broad interconnections between the extensor tendons make it possible to extend to near neutral in the presence of a divided tendon. Partial tendon injuries may still exist despite normal functioning of the fingers. A functioning hand should allow full extension of all fingers and comfortable flexion of the fingers into the palm.
Displaced fractures or dislocations may be apparent as deformity. More subtle rotational deformity will be detected by a finger crossing its neighbour when flexed.
Clinical investigations
Most information will be obtained from a focused history and examination. Radiology of the hand and fingers will be necessary if bone/joint deformity or tenderness is elicited. Even obvious dislocations should be X-rayed prior to correction as post-reduction X-rays may be overly reassuring despite significant soft-tissue damage. Glass is radiopaque to a varying degree and, if a wound is caused by glass, an X-ray should be done prior to closure. Organic foreign bodies and infections may be detected by ultrasound using a small-parts soft-tissue probe and this modality is becoming increasingly available in the ED. Ultrasound is also useful to establish tendon integrity but this is a more specialized examination.
Laboratory investigations are rarely of use in the injured hand unless there are signs of infection.
Magnetic resonance imaging (MRI) can be useful in selected injuries as it shows the soft tissues of the hand clearly, but it is relatively unavailable acutely and should be reserved for conditions where emergent treatment is dependent on the integrity of the soft structures in the hand which are not apparent on examination alone.
Treatment
Appropriate analgesia should be provided as previously described. Rings should be removed from injured fingers to prevent subsequent compromise of circulation as the finger swells. Irrigating wounds with tap water does not increase the risk of infection and is economic. Simple hand and finger wounds can be treated along conventional lines with judicious use of local anaesthetic and skin approximation with fine (5.0) sutures or skin closures. Hand wounds generally heal well and a recent randomized controlled trial showed similar cosmetic and functional outcomes from either conservative treatment or suturing of small, uncomplicated hand wounds. Digital nerve block is useful for managing finger injuries. This technique involves infiltrating local anaesthetic around the digital nerve at the base of the finger or in the palm. Approaching the digital nerve from the dorsum of the finger is less painful but the palmar approach is more accurate as the digital nerves lie just deep to the palmar aponeurosis. A short, fine gauge (e.g. 30 gauge) needle is used with small amounts (≈1 mL) of local anaesthetic for each nerve. Choice of anaesthetic will depend on the desired length of effect and consideration should be given to using long-acting agents for crush or bone injury when a prolonged analgesic effect is desirable. Studies have shown that the use of adrenaline with lignocaine is safe and also prolongs the anaesthetic effect.
Hand dressings can be held in place with a conforming crepe bandage to provide a degree of compression. Stable injuries to the fingers can be managed with ‘buddy’ strapping which allows for some joint movement. Elevation is essential after hand injury to reduce swelling. Minor injuries can be successfully managed in the ED, but more significant injuries usually require referral for surgical opinion.
Fingertip injuries
The fingertips have an excellent blood supply and will usually heal with good cosmetic and tactile function if basic wound care principles are followed. Fingertip injuries may involve skin, subcutaneous tissue, nail or terminal phalanx.
The most complex to manage is when the terminal phalanx is exposed and, in these cases, referral for surgical treatment is advised. If there is injury involving less than 50% of the nail and no bone is exposed conservative treatment is often the best option. Small tuft fractures of the underlying terminal phalanx are stable and will be supported by the dressing or nailbed repair.
Care of the fingertip will require haemostasis followed by a non-adherent dressing. There is good evidence that this kind of dressing promotes healing and re-epithelialization of the fingertip. Occlusive fingertip dressings are quick to apply, easily removed and comfortable for the patient. Most other dressings adhere to the wound and pull epithelial cells off when removed. Alternatives to conservative management include full-thickness skin grafts to the fingertips, advancement flaps and cross-finger flaps. These should be performed by surgeons trained in the specialist techniques and reserved for injuries involving large areas of tissue loss.
Major amputations of the fingertip or crush injuries may require terminalization of the finger. This should be fully discussed with the patient, who may be prepared to forgo finger length in exchange for early return of function. Patients requiring terminalization of a finger should be referred to a specialist hand service. Occasionally, patients will bring amputated pieces of the injured fingertip with them into the ED. Recently amputated fingers can be wrapped in moist gauze and then placed in a bag and packed with ice if re-implantation is being considered by specialist hand surgeons. If there is any doubt about the viability of fingertip tissue, the patient should be referred to a specialized hand service. No attempt should ever be made to resuture avascular tissue.
Digital nerve injuries
Nerve repairs distal to the distal interphalangeal joint are rarely required as the terminal branches are very fine. Any sensory loss with these distal injuries is minimal and improves with time. More proximal injuries can be repaired by hand or plastic surgeons using microsurgery. Good results are achieved with early repair of digital nerves when the ends can be approximated without tension using a fine (>8/0) suture. The return of protective sensation depends on the extent of damage, level of repair and axon regeneration.
Nailbed injuries
These injuries are frequently underestimated, often because of a reluctance to remove the nail. A displaced fracture or growth-plate slip of the terminal phalanx will usually be associated with nailbed disruption. Current practice is to leave a nail when the nail remains adherent to the underlying bed. Small painful subungual haematomas can be released using a hot paperclip or trephine burr. Often, damage to the nailbed results in spontaneous separation of the nail, followed by new nail growth which pushes any residual nail off. Assuming the nail root is intact, a new nail will grow back at a rate of 1 mm per week; thus full growth of a new nail takes approximately 80 days.
If required, removal of a displaced nail is achieved under digital nerve block using blunt dissection with a pair of fine forceps or scissors. The nail should be retained for use as a dressing later. Underlying fractures should be reduced with pressure and fracture haematoma irrigated away to achieve anatomical approximation of the bone ends. Fractures distal to the insertion of the profundus tendon are stable. Repair of the fragmented nailbed can be performed with fine (5/0 or 6/0) absorbable suture on an atraumatic needle. Care needs to be taken not to cut out with the needle as the nailbed is extremely friable. A prospective, randomized controlled trial has shown nailbed repair using tissue ‘glue’ provides similar cosmetic and function results to suture and is faster. Procedural haemostasis can be achieved with the prior application of a finger tourniquet or firm pressure over the digital arteries. Ideally, the nail is trimmed and reapplied as an organic splint and dressing.
Distal interphalangeal joint injuries
Acute flexion injuries of the terminal phalanx may either rupture the extensor tendon at the level of the distal interphalangeal joint (DIPJ) or avulse its insertion into the terminal phalanx. This produces an acute flexion deformity of the DIPJ, known as a mallet finger. An X-ray of the finger should be taken, as an intra-articular fracture involving more than one-third of the joint surface may require internal fixation. Small avulsion fractures and tendon ruptures are best treated by the application of a correctly fitting mallet finger splint, which should be retained for at least 8 weeks. Persisting mallet finger deformity after treatment or late presentations are best treated conservatively as the finger is still functional despite the mallet deformity and operative repair is usually less than satisfactory.
Hyperextension of the DIPJ can cause avulsion of the profundus tendon from the terminal phalanx and requires operative repair. In this injury, there is an inability to flex the DIPJ.
Simple dislocations of the DIPJ can be reduced in the ED and rarely cause long-term instability. However, prior radiography should be performed to differentiate dislocation from the more complicated intra-articular fractures. When associated with a palmar wound, copious irrigation is required prior to closure. Follow up is required and a course of antibiotics.
Middle phalangeal injuries
The middle phalanx takes the insertion of the flexor superficialis tendon slips through which passes the profundus tendon. Fracture of the middle phalanx can disrupt the fibrous tunnel of the profundus tendon and cause adhesions. These fractures need to be accurately reduced and may require internal fixation. They are usually unstable owing to the pull of the tendons. Palmar wounds at this level are likely to divide the profundus tendon or digital nerves and should be explored by a specialized hand service if these injuries are suspected on clinical grounds.
Proximal interphalangeal joint injuries
This is the joint that causes most long-term complications, owing to stiffness and joint contracture. It is also the most commonly dislocated joint in the hand. The proximal interphalangeal joint (PIPJ) is mechanically complex and is supported dorsally by the extensor apparatus and, on the palmar aspect, by the strong fibrous volar plate. Lateral stability is provided by the collateral ligaments. Rupture of either the extensor apparatus or the volar plate will result in joint instability and potential long-term disability. Tears in the extensor apparatus may result from relatively minor blunt trauma. Dislocations of the PIPJ invariably displace both structures. Hyperextension of the PIPJ, often from basketball or netball injuries, can result in an avulsion injury of the volar plate and a small fragment from the middle phalanx may be visible on lateral finger X-ray. Reduction of dislocations should be followed by extension splinting and early follow up. The boutonnière deformity (flexion of the PIPJ accompanied by hyperextension of the DIPJ) is a hand surgeon’s nightmare and, ideally, should be prevented by careful attention to the extensor apparatus at the level of the PIPJ. These injuries should not be underestimated. Ultrasound can be used to aid in early diagnosis.
Proximal phalangeal injuries
Both flexor tendons pass along the palmar aspect of the proximal phalanx and, therefore, fractures of this bone tend to be unstable. Rotational deformity is particularly disabling and may not be noticeable with the finger held straight. These fractures usually require internal fixation. The lateral X-ray will often be the most useful in determining the degree of angulation or displacement. Wounds may damage digital nerves or either or both of the flexor tendons. Examination of the finger should detect these injuries and referral to a specialized hand service will be required.
Metacarpophalangeal joint injuries
Subluxation of the metacarpophalangeal (MCPJ) may occur in the older patient after a fall on the outstretched hand. The clinical appearances are subtle and the injury is easy to miss on X-ray. The clue is the inability of the finger to extend fully. In recent injuries, reduction is achieved by traction on the finger, although once the displacement is established, reduction becomes difficult even with open procedures.
MCPJ injuries caused by a fist and tooth impact (fight bite) are common and should be assumed to be infected. The extensor tendon may be divided and X-ray may show fracture of the metacarpal head. These injuries should be treated aggressively by joint irrigation, splinting and antibiotics.
Rupture of the ulnar collateral ligament (gamekeeper’s or skier’s thumb) results from an abduction injury of the thumb and, when complete, results in MCPJ instability. The ligament when completely ruptured may become folded back outside the adductor aponeurosis which prevents healing. X-rays may be taken to identify avulsion fractures of the base of the proximal phalanx. Stress X-ray views can demonstrate joint instability, but MRI will confirm injury. Treat suspected ulnar collateral ligament injuries in a thumb spica splint and refer for specialist assessment as early surgical repair gives the best outcome.
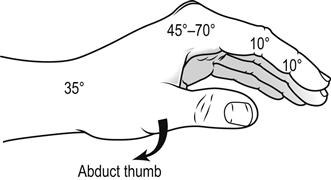
Metacarpal injuries
These injuries can be caused by punching, crush injury or falls onto the closed fist. The commonest injury is fracture of the neck of the fifth metacarpal, which is often treated conservatively. Correction of significant angulation (>45°) should be attempted but it is rare to achieve complete correction. Spiral fractures of the shaft of a metacarpal will result in shortening of the bone and loss of the contour of the knuckle. Angulation of index and middle finger metacarpal fractures should be corrected, but up to 20° of angulation in the ring and little fingers is acceptable. Conservative management of these fractures should involve splinting the hand in intrinsic plus position (Fig. 4.5.4) with the metacarpophalangeal joint flexed to 70%. The fingers must be splinted almost straight, with support extending to the fingertip. Abduction injuries of the thumb may cause a Bennett’s fracture, which is an intra-articular fracture of the base of the thumb metacarpal. Bennett fractures, when displaced, should be referred for specialist opinion.
Dorsal hand injuries
Wounds on the dorsum of the hand may divide the extensor tendons, which are relatively superficial. Complete division may be apparent by loss of full extension of a digit (extensor lag). Extensor tendons have extensive cross-insertions, so over 50% of the tendon can be divided without extensor lag. Visualization of the intact tendon gliding throughout its range of movement in a wound is the only safe way to exclude damage. Repair of these tendons is relatively straightforward as both ends of the tendon are usually visible within the wound. It should, however, only be performed by clinicians with appropriate training and experience. The extensor pollicis longus tendon can retract and, therefore, should be treated in a similar manner to divided flexor tendons and be referred for specialist repair.
Palmar hand injuries
Penetrating wounds on the palm of the hand are likely to divide flexor tendons or main digital nerves. These injuries should be detected by examination of the function of the individual fingers as mentioned previously. Briskly bleeding wounds proximal to an area of anaesthesia are a clue to digital nerve injury because of coexisting damage to both neurovascular structures. Neurovascular and flexor tendon damage will require referral for specialist repair.
Foreign bodies in the hand can be notoriously difficult to find and damage to other structures can result from injudicious exploration. The best results are achieved in a bloodless field with full anaesthesia. Nail-gun injuries require an X-ray prior to removal of the nail to establish its location with respect to bone and to see whether the nail has barbs that will make removal difficult. High-pressure grease or paint-gun injuries result in extensive tissue penetration and should not be underestimated. The extent of penetration may be seen on X-ray. Wide exposure and decompression of the tract will require the care of a specialist hand service.
Disposition
Many minor hand injuries can be well managed in an appropriately equipped ED ambulatory care area. No attempt should be made to operate surgically on a hand without experience, good instruments, adequate lighting and fine sutures. After treatment, the hand should be elevated in a high arm sling and suitable analgesia provided. More complex injuries will require access to a specialized plastic or orthopaedic hand service. When in doubt, early consultation is advisable.
Prognosis
Hand injuries recover best with early definitive treatment, as badly managed injuries can be very difficult to salvage at a later date. Stiffness and loss of function can be avoided if good surgical principles of wound management are adhered to. Appropriate initial splinting and guarded mobilization are the cornerstones of rehabilitation. The injured hand recovers best when splinting has been in a functional position. Whenever possible, the hand should be immobilized with the fingers straight and the MCPJ flexed to 70°. This can be achieved in even the most swollen hand by careful application of a volar plaster slab. Early referral for definitive surgery and subsequent rehabilitation will be essential for severe or complex injuries. An explanation to the patient of the need to prevent joint stiffness is important when the finger requires dressings for more than 3 weeks.
Prevention
Hand and finger injuries can be prevented. Strategies for prevention involve providing data for public awareness, identifying strategies (e.g. safety equipment, machinery modification) to prevent occupational injuries and lobbying officials to legislate for sensible measures to prevent injury.
4.6 Pelvic injuries
Peter Allely and Michael Cadogan
Anatomy
The pelvic ring is formed by two innominate bones and the sacrum. The innominate bones are made up of the ileum, ischium and pubis and are joined anteriorly at the symphysis pubis and posteriorly at the left and right sacroiliac joints. The lateral surface of the innominate bone forms a socket, the acetabulum, contributed to by the ileum, ischium and pubis.
Stability of the pelvic ring is dependent on the strong posterior sacroiliac, sacrotuberous and sacrospinous ligaments. Disruption of the ring can result in significant trauma to the neurovascular and soft tissue structures it protects.
Classification of pelvic fractures
Pelvic fractures can be open or closed, major or minor, stable or unstable, depending on the degree of ring disruption and may be associated with haemodynamic compromise and/or hollow viscus or neurological injury.
Young and Resnik classification
The Young and Resnik pelvic fracture classification (also outlined in Chapter 3.8) classifies pelvic fractures by the mechanism of injury and the direction of the causative force. It does not include isolated fractures outside the bony pelvic ring or acetabular fractures, which are discussed later.
Most pelvic fractures result from lateral compression, anteroposterior compression or vertical shear forces. These injuries may be suggested by the history mechanism and are confirmed radiographically.
Lateral compression injuries
Lateral compression accounts for 50% of pelvic fractures and commonly occurs when a pedestrian or motor vehicle occupant is struck from the side. Most of these injuries are stable but, as a result of the considerable forces involved, there is a high potential for associated injury. This mechanism of injury can produce several fracture patterns involving anterior and posterior pathology.
Anteriorly, there is a transverse fracture of at least one set of pubic rami. These fractures may be unilateral or bilateral and can include disruption of the pubic symphysis. The posterior element of lateral compression fractures is important, but may be overlooked when concentrating on the anterior findings. However, it is critical in determining the functional stability of the pelvic ring and defining associated injuries.
Type 1 fractures
Type 1 fractures are the most common and involve compression injury to the sacrum posteriorly and oblique pubic rami fractures anteriorly.
These injuries occur on the side of impact and are usually stable, involving impaction of the cancellous bone of the sacrum without ligamentous disruption. X-rays confirm discontinuity of the sacral foramina posteriorly.
Type 2 fractures
Type 2 fractures result from greater lateral compressive forces. The iliac wing is fractured posteriorly, with the fracture line often extending to involve part of the sacroiliac joint. This leaves part of the ileum firmly attached to the sacrum.
Anteriorly, there are associated fractures of the pubic rami. Stability is determined by the degree of sacroiliac joint disruption and mobility of the anterior hemi-pelvis involved. These fractures are usually stable to external rotation and vertical movement, but are more mobile to internal rotation.
Type 3 fractures
Type 3 fractures usually occur when one hemi-pelvis is trapped against the ground and a lateral force rolls over the mobile hemi-pelvis. This produces a lateral compression injury to the side of primary impact and an unstable anteroposterior compressive injury to the contralateral sacroiliac joint.
Anteroposterior compression injuries
Anteroposterior compression injuries of the pelvis account for 25% of pelvic fractures. They result from anterior forces applied directly to the pelvis or indirectly via the lower extremities to produce an open-book type injury.
Type 1 injuries
Type 1 injuries result from low-energy forces that stretch the ligamentous constraints of the pelvic ring. The pubic symphysis is disrupted anteriorly, but with less than 2.5 cm diastasis seen radiographically. These fractures are stable and there is usually no significant posterior pelvic injury.
Type 2 injuries
Type 2 injuries classically cause an open-book fracture. They involve rupture of the anterior sacroiliac, sacrospinous and sacrotuberous ligaments posteriorly and disruption of the pubic symphysis anteriorly. There is widening of the anterior sacroiliac joint with diastasis of the pubic symphysis by more than 2.5 cm on radiology; occasionally, there is avulsion of the lateral border of the lower sacral segments.
Considerable force is involved to disrupt these ligaments and neurovascular injuries and complications are common. The pelvis is unstable to external rotation and external compression will ‘spring’ the pelvis, although this manoeuvre is no longer recommended diagnostically.
Type 3 injuries
Type 3 injuries occur when an even greater force is applied and involves disruption of all the pelvic ligaments on the affected side. Rupture of the posterior sacroiliac ligaments leads to lateral displacement and disconnection of the affected hemi-pelvis from the sacrum. They are grossly unstable and associated with the highest rate of haemorrhage and neurological injury and haemorrhage (Fig. 4.6.1).
Vertical shear injury (Malgaigne fracture)
These injuries account for only 5% of pelvic fractures. They usually occur following a fall from a height or during a motor vehicle accident, when the victim reflexly extends their leg against the brake pedal before impact. These mechanisms force the hemi-pelvis in a vertical direction and result in complete ligamentous or bony disruption, with cephaloposterior hemi-pelvis displacement.
Anterior disruption occurs through the pubic symphysis or pubic rami. Posteriorly, dissociation usually occurs through the sacroiliac joint, but may occur vertically through the sacrum. These fractures are usually unilateral, but may be bilateral and are associated with significant bleeding and/or intra-abdominal injury.
Clinical assessment
A standard trauma management protocol is adhered to in managing the multitrauma patient, with usual attention being paid initially to the airway, breathing and circulation (ABCs) in the primary survey and resuscitation phases of care (see Chapter 3.1).
General examination
The back is examined to assess for external evidence of injury to the lumbar spine, sacroiliac regions and coccyx, with inspection and palpation. Abdominal, perineal, rectal and a vaginal examination are performed according to suspected injury. The rectal examination in the absence of overt urethral trauma includes observation for fresh blood and an assessment of anal sphincter tone and position of the prostate. A thorough perianal and lower limb neurovascular examination is performed.
Pelvic examination
The pelvis is briefly examined as part of the cardiovascular assessment in the ABC approach to trauma. The suprapubic, pelvic and urogenital regions are inspected for signs of bruising, abrasions, open wound and obvious deformity. In males, the urethral meatus is assessed for the presence of frank blood and the scrotum for bruising. Flank bruising may indicate retroperitoneal haemorrhage.
Pelvic compression or ‘pelvic springing’ has been in widespread use ostensibly as a means to assess for pelvic injury and to assess the stability of a fracture. It adds little to the assessment of a patient beyond gentle palpation. As it may dislodge clots in an injured pelvic venous plexus resulting in catastrophic bleeding, it is no longer recommended in anyone with haemodynamic compromise and/or an obvious pelvic fracture.
Radiology
The AP pelvic X-ray is an initial film that will usually rapidly alert clinicians to anterior fractures, such as pubic rami, diastasis and suggest complex hemi-pelvic injuries. Posterior fractures are difficult to visualize and further plain X-rays or usually a computed tomography (CT) scan are needed.
Injuries associated with pelvic fractures
Haemorrhage
Haemorrhage is the most serious complication of a pelvic fracture. It may result from bleeding at fracture sites, local venous or arterial tears and/or disruption of a major vessel. Catastrophic bleeding can result from disruption of the internal iliac arteries, their tributaries and accompanying veins as they pass over the anterior aspect of the sacroiliac joint.
Severe hypovolaemia due to persistent haemorrhage without major vessel disruption is a significant cause of mortality. Up to 4 L of blood may be lost into the retroperitoneal space before tamponade occurs. Anteroposterior type 3 injuries and vertical shear injuries disrupt the sacroiliac joint and are associated with significant haemorrhage.
Treatment to minimize or stop haemorrhage associated with a pelvic fracture includes the early application of a pelvic binder across the level of the greater trochanters. Treatment beyond that is complex and best led by a senior specialist team leader using a pre-agreed algorithm. This will vary between institutions and involve any combination of external fixation, interventional radiology with angiography and embolization, ‘damage control’ laparotomy with pelvic packing and/or open reduction with internal fixation.
Genitourinary and bladder injuries
Pelvic fractures are associated with injury to the lower urinary tract in up to 16% of cases. These are more prevalent in males who sustain a higher rate of urethral injury. Pelvic trauma may also result in bladder rupture. The bladder is normally protected by the pelvis and rupture usually indicates significant disruption of the pelvic ring.
Almost 90% of blunt trauma patients with bladder rupture have an associated pelvic fracture. Patients are usually hypotensive with frank haematuria, although gross haematuria is a non-specific sign of genitourinary trauma and does not necessarily indicate bladder rupture. Therefore, a retrograde urethrogram is performed to delineate any urethral trauma prior to performing retrograde cystography. However, this should be not performed before other emergent advanced imaging, such as CT scan of the abdomen and pelvis, as the contrast or spillage may obscure other important injuries.
Urethral and genital injuries
Urethral rupture is rare in females. Rupture of the urethra secondary to blunt trauma commonly occurs to the anterior bulbous urethra just distal to the urogenital diaphragm. It is associated with bilateral fractures of the pubic rami, pubic symphysis disruption and vertical shear injuries.
Suspect a urethral rupture in the adult male with a pelvic fracture, blood at the urethral meatus, perineal haematoma and urinary retention. A ‘high-riding prostate’ may be found on rectal examination, however, not all these signs may be present. A retrograde urethrogram is diagnostic and must be performed prior to urethral (Foley) catheterization when indicated clinically (see above).
Injury to the female genitalia is uncommon and often overlooked. Vaginal laceration is associated with a pelvic fracture in 4% of cases. These normally present with bleeding, but may be occult. A bimanual pelvic examination is necessary in women with a pelvic fracture, which may necessitate anaesthesia due to patient discomfort. Complications, such as abscess formation and sepsis, are severe, particularly if the injury is missed.
Management of the unstable pelvic fracture
The mainstay of pelvic fracture management in the emergency department (ED) is to identify and assess the degree of pelvic injury, to provide pain relief and to provide fluid resuscitation to minimize life-threatening haemorrhagic shock. Early identification of major pelvic trauma with mobilization of general surgical, orthopaedic, vascular, interventional radiology and intensive care specialties is essential, ideally using a pre-agreed algorithm approach.
Fluid resuscitation
Commence initial fluid resuscitation with intravenous crystalloid in the hypotensive patient with pelvic trauma using two large-bore peripheral intravenous cannulae, but rapidly change to blood and blood products if the hypotension is not immediately reversed. An average blood transfusion requirement for anteroposterior compression fractures is 15 units, for a vertical shear injury is 9 units and for lateral compression injuries is 3.5 units.
Therefore, activate a Major Transfusion Protocol (MTP) with blood and blood products, such as fresh frozen plasma (FFP) and platelets in a ratio that may approach 1:1:1 according to local protocol. Also give 1 g tranexamic acid IV in 100 mL normal saline over 10 min, followed by 1 g infusion over 8 h, providing these are commenced within a maximum of 3 h of injury.
Pelvic immobilization
Pelvic binder or sling
Immobilization of the pelvis with attempted reapproximation of bony fragments creates a tamponade effect that reduces the risk of haemorrhage prior to definitive treatment. This is best achieved using a proprietary radiolucent pelvic binder device with ratchet mechanism or pelvic sling to apply compression. Alternatively, simply brace the pelvis in a sheet, support it laterally with sandbags and internally rotate the hips with the lower legs splayed apart.
External fixation
External fixation is a rapid and simple procedure designed to immobilize and stabilize the anterior pelvis in the ED to reduce pelvic haemorrhage prior to definitive treatment. Three pins are placed through each iliac crest and are then clamped to an external frame to reduce the displaced pelvic ring injury.
The advantages of external fixation are that it is quick, effective and can proceed in the ED without delaying the continued management of the multiply injured patient. Disadvantages include a lack of support for the posterior component of the pelvic ring fracture, difficulty of placement in the obese patient and reduced pelvic surgical access in the event of laparotomy being required.
Embolization
Life-threatening arterial haemorrhage is estimated to occur in 5–20% of patients with blunt pelvic fracture. Emergency angiography is both diagnostic and therapeutic to control primary haemorrhage and (where available) has become the treatment of choice in patients with haemodynamic instability due to a pelvic fracture, particularly where a CT scan has shown an ‘arterial blush’ indicating ongoing bleeding.
Early recognition of these patients with organization of transfer to a hospital with angiography capabilities and mobilizing an interventional radiologist reduce mortality, but is a logistical challenge. The success of the procedure is operator dependent, time-consuming and does not address venous blood loss, which still requires appropriate replacement of blood and blood products and consideration of laparotomy with pelvic packing.
Laparotomy with pelvic packing
Continuing pelvic bleeding with haemodynamic instability when due to venous haemorrhage and/or when interventional radiology is unavailable or delayed may require laparotomy with pelvic packing, with continued blood and component therapy to prevent or treat coagulopathy paying attention to base deficit, coagulation profile and temperature; followed by admission for intensive-care monitoring. Surgical expertise is necessary to perform this temporizing procedure, prior to subsequent pack removal and definitive management that may include later open reduction with internal fixation.
Open pelvic fracture
Open pelvic fractures are rare and associated with increased morbidity and mortality of up to 40–50%. Open fractures with pelvic ring disruption lose any tamponade effect and can result in massive and fatal haemorrhage, as well as high risk of intra-abdominal injury and/or late sepsis.
Management
Control of haemorrhage is the priority in an open pelvic injury, with early surgery to avoid the increased risk of infection. Sterile gauze packed into the wound applies direct pressure tamponade. Urgent repair of associated open bowel and/or bladder injuries and to debride bleeding wounds is paramount, with stabilization of the pelvic fracture as the last step in treatment. The mortality remains high despite advances in imaging and aggressive treatment.
Acetabular fractures
Acetabular fractures account for 20% of pelvic fractures and are usually associated with lateral compression forces. They also occur with posterior forces applied distally through the femur. Their classification is complex.
Clinical features
Acetabular fractures are caused by direct impaction of the femoral head that may be associated with a central hip dislocation. These fractures are associated with sciatic and femoral nerve injury, depending on the position of the hip dislocation. A thorough neurovascular examination is mandatory.
In addition, these fractures are often associated with other pelvic injuries, knee injury, hip fractures and dislocations, which should all be looked for.
Management
Standard radiographs of the hip and pelvis may define the fracture, but a CT scan is necessary, particularly to show the anterior and posterior fragments and involvement of the ilioischial and iliopubic columns. All fractures are referred for inpatient orthopaedic management.
Stable fracture of the pelvis
Isolated pubic ramus fracture
These injuries are commonly seen in the elderly with direct trauma following a fall. The patient has difficulty in weight bearing and there is local pain and tenderness in the groin. These should be carefully looked for in any patient unable to bear weight with a suspected hip fracture, particularly when X-ray of the hip is normal.
Pain is usually reproduced with the FABER test. The ipsilateral foot is placed on the contralateral knee, forcing the ipsilateral hip to be Flexed, ABducted and Externally Rotated, which exacerbates the pain. Pelvic radiographs confirm the diagnosis.
Iliac wing fracture (Duverney fracture)
Direct lateral trauma may result in an isolated iliac wing fracture, known as the Duverney fracture. Patients complain of severe pain on weight bearing and walk with a waddling gait. Localized tenderness and bruising occur over the site of injury, associated with abdominal guarding, ileus and lower quadrant tenderness.
These fractures are usually minimally displaced, rarely comminuted and are readily visualized on AP pelvic X-ray.
Isolated avulsion fractures
These are often sustained by young adults following acute stress to the muscular and ligamentous insertions onto the bony pelvis. They include anterior superior iliac spine fracture, anterior inferior iliac spine fracture and the ischial tuberosity fracture.
Anterior superior iliac spine fracture
The anterior superior iliac spine may be fractured in jumping activities due to powerful contraction of the sartorius muscle and tensor fascia lata. Such injuries cause pain on weight bearing, with local tenderness and swelling at the fracture site. Active flexion and abduction of the thigh reproduces the pain. There is usually minimal displacement of the avulsed fracture on the AP film of the pelvis. Treatment is usually conservative, although operative management is possible for significant displacement.
Anterior inferior iliac spine fracture
Forceful contraction of the rectus femoris muscle in sports that involve sprinting or kicking (forceful hip extension) may avulse the anterior inferior iliac spine. These patients complain of a sharp pain in the groin and are unable actively to flex the hip. The fracture is usually evident on plain AP pelvic views, with the fragment being displaced distally. Conservative treatment is common.
Ischial tuberosity fracture
Fracture of the ischial tuberosity is rare and occurs with forceful contraction of the hamstrings, usually in young adults whose apophyses are not fully united. They are associated with hurdling and other jumping activities. Pain may be reproduced by local palpation and by active flexion of the hip with the knee extended. Plain X-rays of the pelvis reveal minimal displacement of the apophysis from the ischium. Conservative treatment is common.
Coccyx fracture
These fractures are more frequent in women and are caused by a fall onto the buttocks with both hips flexed. Patients have difficulty in mobilizing and have local pain, swelling, bruising and tenderness over the lower sacral region. X-ray confirmation is unnecessary if physical examination confirms an isolated injury.
Management of isolated stable fractures
Pubic ramus fractures, iliac wing fractures and avulsion fractures are treated conservatively with non-steroidal anti-inflammatory drugs (NSAIDs) and non-weight-bearing crutches for 10 days. Mobilization and physiotherapy allow resumption of normal activities in 3–4 weeks, followed by graduated return to high impact sporting activities. Coccygeal fractures require rest, analgesia and stool softeners. As sitting is painful, a doughnut-ring foam cushion is helpful.
4.7 Hip injuries
Peter Allely and Michael Cadogan
Anatomy
The hip joint is a large ball and socket articulation encompassing the acetabulum and proximal femur. The hip joint provides a high degree of stability and mobility.
Blood supply
The head and intracapsular portion of the femoral neck receive the majority of their blood supply from the extracapsular trochanteric anastomosis arterial ring, with a minor supply arising from the foveal branch of the obturator artery, via the ligamentum teres to the femoral head.
Retinacular arteries from the extracapsular ring pass under the reflection of the hip capsule to supply the femoral neck and head in a retrograde manner. Intracapsular fractures disrupt this ‘distal to proximal flow’ and so may result in avascular necrosis of the femoral head.
Avascular necrosis
Avascular necrosis (AVN) following hip injury refers to ischaemic bone death within the femoral head due to compromise of its blood supply. Increased bone density of the femoral head is the radiographic feature of AVN, but this may take up to 6 months to become manifest.
AVN results primarily from the disruption of the trochanteric anastomosis in femoral neck fractures and is the commonest early complication of these fractures. Traumatic haemarthrosis, with or without a fracture, may also result in intracapsular tamponade. AVN occurs when the intracapsular pressure exceeds the diastolic blood pressure.
AVN is also seen following posterior dislocation and is related to the degree of trauma and the length of time the femoral head is out of the joint. Early management is thus an orthopaedic emergency, as reduction within 6 h results in an AVN rate of less than 10%.
In addition, chronic pancreatitis, alcohol abuse, sickle cell anaemia, vasculitis, irradiation, decompression illness (DCI) and the prolonged use of corticosteroids may all result in AVN.
Classification of hip fractures
Hip fractures are either intracapsular or extracapsular. Intracapsular fractures involve the femoral neck or head. Extracapsular fractures include intertrochanteric, trochanteric and subtrochanteric types and are four times more common than intracapsular fractures.
The incidence of hip fractures increases exponentially with age, with the fracture rate doubling for every decade over 50 years. Hip fractures occur most frequently in white postmenopausal women as 50% of 65-year-old women and 100% of women over the age of 85 have a bone mineral density below fracture threshold level (osteoporosis).
Intracapsular fractures
Femoral head
Femoral head fractures are uncommon and are usually associated with dislocations of the hip. They often occur in young patients, 75% of cases being associated with motor vehicle incidents.
Classification
Fractures of the superior aspect of the femoral head are usually associated with anterior dislocation, whereas inferior femoral head fractures occur with posterior dislocation. Fractures may involve a single fragment (type 1) or comminution (type 2).
Clinical evaluation
Symptoms and signs of femoral head injuries are usually those of the associated dislocation rather than the fracture itself. Femoral head fractures are not always picked up on initial X-rays. In the absence of abnormality on plain radiography, further imaging with a computed tomography (CT) scan should be performed in the presence of persistent pain following reduction of a hip dislocation.
Management
Immediate orthopaedic referral is essential as prompt reduction of the dislocation and appropriate stabilization of the fracture reduce the risk of AVN, increasing the chances of a return to full mobility. The prognosis is related to the severity of the initial trauma, time to definitive reduction and the number of failed closed relocation attempts.
Complications
AVN occurs in 15–20% of cases, post-traumatic arthritis in 40% and myositis ossificans in 2%.
Femoral neck fractures
Intracapsular fractures are four times more common in females than males. There are four main causes of this type of injury:
 elderly, with minimal trauma following a fall onto the greater trochanter (pathological fracture)
elderly, with minimal trauma following a fall onto the greater trochanter (pathological fracture)
 elderly, with torsion or twisting injury prior to fall (pathological fracture)
elderly, with torsion or twisting injury prior to fall (pathological fracture)
 young person involved in high-energy trauma (excessive loading)
young person involved in high-energy trauma (excessive loading)
 repetitive stress or cyclical loading injuries (stress fracture).
repetitive stress or cyclical loading injuries (stress fracture).
Classification
The Garden classification system is commonly used to describe intracapsular neck of femur fractures.
Garden I: incomplete, impacted or stress fractures that are stable. Trabeculae of the inferior neck are still intact and, although they may be angulated, they are still congruous.
Garden II: undisplaced fracture across the entire femoral neck. The weight-bearing trabeculae are interrupted, without displacement. These fractures are inherently unstable and must be fixed.
Garden III: complete femoral neck fracture with partial displacement. There is associated rotation of the femoral head, with non-congruity of the head and acetabular trabeculae.
Garden IV: complete subcapital fracture with total displacement of fracture fragments. There is no congruity between proximal and distal fragments, but the femoral head maintains a normal relationship with the acetabulum.
These fractures may be further simplified into non-displaced (Garden I and II) and displaced (Garden III and IV).
Clinical assessment and management
Non-displaced fractures
Non-displaced fractures include stress fractures, Garden I and Garden II fractures. Stress fractures are usually the result of repetitive abnormal forces on normal bone in fit, active young people, such as military recruits or marathon runners, but may occur with repetitive normal stresses on abnormal bones, such as in rheumatoid arthritis or patients taking long-term steroids.
These present with pain that is gradual in onset and worse after activity, radiating from the groin to the medial aspect of the knee. Patients walk with a limp and often present late. Physical examination reveals no obvious deformity, although there is mild discomfort on passive movement at the extremes of motion and percussion tenderness over the greater trochanter.
Additional radiological examination with a bone scan and/or MRI is indicated when initial X-rays are normal but there is persistent pain. MRI is the investigation of choice, being more sensitive than bone scans in the first 24 hours. It is of similar accuracy to bone scans in fracture assessment at 72 hours.
Stress fractures and Garden I impacted fractures are considered stable and may be treated conservatively under close orthopaedic supervision. Garden II fractures, although non- displaced, are inherently unstable and must be fixed internally.
Displaced fractures
Elderly patients with displaced fractures usually present with pain in the hip area and markedly reduced hip movement. The lower limb is shortened, abducted and externally rotated distal to the fracture, albeit less than with intertrochanteric fractures.
X-ray reveals the fracture and the degree of posterior comminution of the proximal fragment. Parenteral analgesia and a femoral nerve block reduce discomfort. Skin traction will also reduce pain and helps preserve femoral head vascularity.
Traumatic femoral neck fractures in the young adult are uncommon and usually involve normal bone. These fractures are outside of the Garden classification. They follow a large degree of force and have up to a 35% risk of AVN and up to a 57% risk of non-union.
Complications
Mortality
Femoral neck fractures are associated with a mortality of 14–36% in the first year after injury, with the rate returning to the pre-fracture level after this. Mortality is increased threefold in those who were institutionalized prior to the fracture, with increased risk factors for mortality being male gender, older age, malnutrition, multiple medical problems and end-stage renal failure.
Morbidity
AVN is the most common complication despite optimal treatment. Non-union, postoperative infection and osteomyelitis are also seen.
Extracapsular femur fractures
Intertrochanteric femur fractures
Fractures of the proximal femur that occur along a line between the greater and lesser trochanters are referred to as intertrochanteric. They are usually pathological, occur in the elderly and have a female preponderance.
Mechanism
A simple fall with a direct force applied to the greater trochanter in the elderly is enough to cause an intertrochanteric femoral fracture. In young adults, they are associated with high-speed motor vehicle incidents or falls from a height.
Clinical assessment
Patients sustaining an intertrochanteric fracture are unable to bear weight and have significant pain on hip movement. There is often a large haematoma overlying the greater trochanter, owing to the highly vascular bone that is fractured without any intracapsular containment. Examination reveals a markedly shortened, abducted, significantly externally rotated lower limb.
X-rays confirm the fracture in most cases. However, internal rotation of the hip on the AP view may obscure the fracture. The lateral view depicts the size, location and degree of comminution of the fracture fragments and determines stability.
Classification
Numerous classification systems are available for intertrochanteric fractures, the simplest of which is by Evans. This divides intertrochanteric fractures into stable and unstable. However, for the emergency physician, an anatomical description of the fracture detailing the degree of comminution, subtrochanteric extension and the presence of displaced posterior fragments is adequate (Fig. 4.7.1).
Management
A complete evaluation is essential to formulate an early treatment plan as intertrochanteric fractures occur most frequently in the elderly. Patients may lose up to 1.5 L of blood from a comminuted fracture and are often dehydrated, malnourished and in significant pain on arrival in the emergency department (ED). Parenteral analgesia and fluid resuscitation are important in preparation for theatre.
Skin traction or immobilization with sandbags prevents further soft-tissue damage and bony comminution and reduces blood loss. Full preoperative evaluation requires a search for associated injuries, such as rib fractures, distal radial fractures and vertebral compression fractures at the level of T12 and L1.
An ECG, bloods and chest X-ray help elucidate the cause of the fall and may indicate the need for associated medical treatment.
Treatment is with open reduction with internal fixation (ORIF) which produces better anatomical alignment, a shorter hospital stay and improved function with reduced mortality by comparison with conservative management.
Complications
Survival is directly related to the patient’s age and pre-existing medical factors.
Greater trochanteric fracture
Mechanism
Isolated fractures of the greater trochanter are uncommon. They usually occur between 7 and 17 years of age and involve true epiphyseal separation secondary to indirect trauma. Forceful muscular contraction by the gluteus medius causes avulsion of the apophysis. The displaced, non-comminuted fragment may be separated by up to 6 cm.
Greater trochanteric fractures in adults are rare and usually result from direct trauma, causing a comminuted fracture whose fragments are rarely displaced and usually involve only part of the trochanter.
Clinical assessment
Patients with a greater trochanter injury are tender to palpation over the area of avulsion or comminution, but bruising is uncommon. There is often an associated flexion deformity of the hip as a result of pain and muscle spasm and weight bearing causes a limp.
Management
The prognosis is good after these fractures. Most are treated with bed rest for 3 days, followed by non-weight bearing and crutches for 4 weeks. Open reduction and internal fixation are indicated for marked separation of the bony fragment.
Lesser trochanteric fracture
Isolated fractures of the lesser trochanter usually occur in children and young athletes, with 85% occurring before the age of 20.
Mechanism
Lesser trochanter fractures are usually an apophyseal avulsion injury secondary to forceful contraction of iliopsoas.
Clinical assessment
Patients complain of pain on flexion and internal rotation of the hip. Examination reveals tenderness in the femoral triangle. The patient is unable to flex the hip and raise the foot off the ground in a seated position (Ludloff sign specific for the iliopsoas muscle).
Radiology is often inconclusive, as there may not be complete separation of the bony fragment; comparison views may be required.
Management
Ten days of bed rest and slow mobilization result in full recovery. Open reduction and internal fixation are not indicated, even with wide apophyseal separation.
Subtrochanteric femoral fractures
The subtrochanteric region of the femur lies between the lesser trochanter and a point 5 cm distally. Fractures in this region are termed subtrochanteric. They account for 11% of hip fractures and occur in the elderly with osteoporosis, bone metastases or end-stage renal failure. High-energy injuries in young adults with normal bone are less common.
Mechanism
Ninety per cent of these fractures result from blunt trauma, either due to a simple fall in the elderly or following a high-speed motor vehicle accident (MVA) or fall from a height in young adults. In some countries, up to 10% are due to high-energy gunshot wounds.
Classification
A variety of classification systems is available, but none is widely used. As with intertrochanteric fractures, it is best to describe the location, presence of comminution and the position of the lesser trochanter proximal or distal to the fracture line.
Clinical assessment
A subtrochanteric fracture is usually isolated in the elderly. However, as substantial force is required in young adults, the presence of other injuries must be sought. The limb distal to the fracture is usually held in abduction, flexion and external rotation. Haemorrhage from a comminuted subtrochanteric fracture may be up to 2 L. Assess the patient’s circulatory status and commence fluid and blood.
Management
The affected limb is immobilized in a splint following parenteral analgesia and a femoral nerve block. Suitable splints include proprietary splints, such as the Donway or Hare. Fluid resuscitation is started as required. The older, more laborious Thomas splint is now rarely used.
Orthopaedic referral is essential for open reduction and internal fixation of these fractures.
Complications
There is up to a 20% mortality associated with these fractures within the first year in the elderly. They are associated with a higher rate of non-union and implant failure as subtrochanteric bone is cortical thus, unlike the cancellous bone involved in intertrochanteric fractures, these fractures often lack the vascularity for adequate new bone growth and repair. The further down the shaft of femur the fracture line is located, the greater the degree of non-union and implant failure.
Hip dislocation
The hip joint is inherently stable and considerable force is required to produce a dislocation. Associated injuries must always be sought. Hip dislocations are classified anatomically into anterior and posterior, depending on the final position of the femoral head relative to the acetabular rim.
Non-prosthetic hip dislocations are an orthopaedic emergency as the femoral head’s blood supply is precarious and also due to the proximity of the sciatic nerve. Failure to reduce a hip dislocation within 6 hours dramatically increases the risk of AVN and sciatic nerve ischaemic damage.
Posterior hip dislocation
Mechanism
Posterior dislocations represent 85–90% of traumatic hip dislocations. Classically, a direct distal force applied to the flexed knee, with the hip in varying degrees of flexion as when seated in the front of a car, causes a posterior dislocation of the hip. The hip and knee are usually flexed to 90° and the hip adducted, which is the least stable position for the hip to be in.
The force applied by the dashboard in a head-on collision to a seated individual may produce an isolated posterior dislocation. The abducted and partially flexed hip in the same scenario is more stable and, if the force of impact is great enough, will result in a posterior dislocation with displaced acetabular fracture.
Clinical assessment
Examination of the affected limb reveals shortening, adduction, internal rotation and some degree of flexion. A single AP pelvis radiograph is usually adequate to confirm a posterior dislocation. However, as up to half of these dislocations are associated with an acetabular, femoral head or femur fracture, further radiological imaging is essential. Judet views, AP hip with internal rotation and AP and lateral femoral views have been used extensively in the past, but are now largely superseded by CT.
Neurological examination
Neurological examination is essential in a posterior dislocation, particularly with marked internal rotation which may compress the sciatic nerve and its branches. This results in neurological deficit particularly in the peroneal nerve distribution. Associated injuries, such as ipsilateral knee ligament disruption with a posterior cruciate rupture, must be looked for as well.
Management
The orthopaedic team is consulted early. A thorough search for associated periarticular and distal limb injuries, neurological evaluation and adequate imaging are essential in the ED.
Closed reduction
Closed reduction of a posterior hip dislocation may be performed in the ED under procedural sedation, unless there is immediate access to an operating theatre (see Chapter 22.3).
Allis manoeuvre
There are numerous methods of relocation, many requiring significant physical strength. The most common is the Allis manoeuvre, whereby the patient lies supine with assistants on either side stabilizing the pelvis by downward pressure on the anterior superior iliac spines. The operator applies longitudinal traction to the lower leg with the hip slightly flexed in the line of the femur and knee in 90° of flexion. The leg is internally and externally rotated until the femoral head is rearticulated with the acetabulum. Lateral traction to the inside of the thigh may assist.
Other techniques include the lateral traction–countertraction method and the Whistler technique.
Complications
The risk of developing AVN is directly proportional to the length of time the hip remains dislocated and increases dramatically if the dislocation is not reduced within 6 hours of injury. Sciatic nerve neuropraxia may occur in 15% of cases but is usually relieved by reduction.
Permanent ischaemic changes with neurological deficit secondary to pressure necrosis have been reported in up to 3% of cases, usually in the peroneal nerve distribution. Missed knee injuries occur in up to 15% of cases as well as patellar, tibial plateau and posterior cruciate injuries.
Anterior hip dislocation
Anterior dislocations account for 10–15% of traumatic hip dislocations and are associated with femoral neurovascular injury and occult hip joint fracture. They usually result from a direct blow to the abducted and externally rotated hip. When the hip is in abduction, the femoral neck or greater trochanter impinges on the rim of the acetabulum. A direct force applied distally can lever the head out of the acetabulum and tear the anterior capsule of the hip.
Classification
Anterior dislocations may be superior or inferior. Type I or superior dislocations occur when the hip is extended at the time of injury. These are also known as iliac dislocations. Type II or inferior dislocations occur when the hip is flexed at injury and are also known as obturator dislocations.
They may be further subclassified as simple dislocation, associated femoral neck fracture or associated acetabular fracture.
Clinical assessment
The superior type of injury causes an extended, externally rotated and slightly abducted distal limb. The distal limb in the inferior type of dislocation is externally rotated, abducted and in flexion. The femoral head may be palpated around the anterior superior iliac spine in superior types and in the obturator foramen in inferior types.
A neurovascular examination is essential in anterior dislocation, particularly the superior type, where trauma to the femoral artery, vein and nerve is common. Hip and pelvis radiographs must be studied carefully for associated fractures of the acetabulum and femoral head. Further imaging with CT is indicated, particularly for persistent post-reduction pain.
Management
General examination looking for associated life-threatening injuries is essential as this type of hip dislocation is usually associated with high-energy trauma. Orthopaedic consultation is mandatory because of the high probability of vascular injury and the need for closed reduction under general anaesthesia.
Complications
Early complications in superior dislocations result from direct pressure on the femoral vessels with the potential for distal neurovascular compromise. Late complications include post-traumatic arthritis and AVN. Recurrent dislocation is common when anterior capsular healing is incomplete following inadequate immobilization after reduction.
4.8 Femur injuries
Peter Allely and Michael Cadogan
Femoral shaft fracture
Mechanism
Considerable force is required to break the adult femur in the absence of osteoporosis or metastatic disease with a bony secondary. The majority of femoral shaft injuries occur in young adults following road traffic incidents, falls from a height or a gunshot wound.
Classification
No universally accepted classification system exists for fermoral shaft fractures. A precise description of the fracture provides the orthopaedic specialist with an indication of the potential for blood loss and the urgency of definitive management.
Femoral fractures are either open or closed and may be transverse, oblique, spiral or segmental. They may occur within the proximal third, midshaft or distal third of the femur. The degree of fracture comminution, soft-tissue involvement and neurovascular status should also be described.
The majority of fractures occur in young adults with healthy bones and are transverse. Greater mechanical force usually results in comminution (Fig. 4.8.1). Minimal force with pathological bone tends to produce metaphyseal fractures with propagation into the shaft.

Stress fractures
Stress fractures of the femoral shaft are becoming increasingly common. They occur when repetitive mechanical forces are applied to the femur, such as in marathon running or military recruits. They are associated with pain in the midthigh and apparently normal X-rays, although a bone scan will detect the fracture. Low-impact training, such as cycling, is used in rehabilitation. They are rarely displaced.
Clinical evaluation
The clinical diagnosis of femoral shaft fracture is usually straightforward. The thigh is shortened and externally rotated, with the hip held in slight abduction. Palpation reveals tenderness over the fracture site and extreme pain on attempted movement. Neurovascular injuries are rare, but the distal pulses, capillary refill and distal sensation must be carefully examined.
Vascular damage
Vascular damage is usually limited to rupture of the profunda femoris perforating branches in closed fractures. The resulting tense, swollen haematoma is limited to the thigh and is not associated with distal circulatory compromise. However, penetrating trauma from gunshot wound and open fractures may cause femoral artery disruption with distal circulatory compromise, so repeated vascular evaluations are important.
Any evidence of an expanding haematoma or diminished distal pulses requires further investigation with Doppler imaging or arteriography.
Associated injuries
Commonly associated injuries include fractures of the pelvis, the femoral head and neck, dislocation of the hip and soft-tissue disruption of the knee. Up to 50% of closed femur injuries are associated with meniscal and collateral ligament injuries in the knee, although it is usually impossible to evaluate reliably these injuries in the acute setting. Up to 1.5 L of blood may extravasate into the surrounding soft tissues.
Management
The treatment of any associated multitrauma to the head, neck, thoracic or pelvic injury should take priority. However, early reduction of a femoral fracture is an important part of haemorrhage control. Administration of analgesia, fluid resuscitation and fracture reduction and splinting are ideally performed prior to X-ray of the lower limb, unless this is immediately available.
Analgesia
Adequate pain relief is essential in the emergency department (ED). Intravenous opioid analgesia is necessary, and titrated to effect. A femoral nerve block is an important adjunct that should be performed prior to fracture reduction and splinting (see Chapter 22.2).
Reduction and splinting
Early fracture reduction and splinting in traction decreases overall mortality and pain, limits blood loss and reduces the risk of fat embolism. Fractures are returned to near anatomical alignment using longitudinal traction following appropriate analgesia with the knee in extension.
Proprietary splints, such as the pneumatic Donway or Hare traction splint, have replaced the old skin traction (Thomas) splint in the ED.
Traction is an interim procedure prior to definitive management as it cannot hold a constant force of sufficient magnitude to maintain the length and alignment of an adult femur fracture.
Fluid resuscitation
Haemorrhagic shock is a major complication with an average blood loss from a closed femoral fracture of 1200 mL. All patients must be resuscitated with intravenous fluid and blood, kept fasted and an indwelling catheter inserted to monitor fluid balance.
Orthopaedic management
Early operative fixation, typically intramedullary nailing, is indicated in adults within 8 hours. Open fractures require immediate operative debridement with antibiotic cover such as flucloxacillin 2 g IV or cephazolin 2 g IV, followed by delayed intramedullary nailing.
Complications
Complications include fat embolus syndrome, haemorrhagic shock and adult respiratory distress syndrome, with a higher incidence in comminuted fractures. Long-term complications of shortening, malalignment and non-union may result in post-traumatic arthritis.
Early mobilization following intramedullary nailing greatly reduces complications associated with prolonged immobilization. Patients older than 60 years with closed femoral fractures have a complication rate of 54% and a mortality of 17%.
4.9 Knee injuries
Michael Baker and Michael Cadogan
Anatomy
The knee is the largest, most complicated joint in the body. It is a synovial, complex hinge joint comprising the patellofemoral and tibiofemoral joints. Movement ranges from 10° of extension to 140° of hyperflexion, with up to 12° of rotation present through the full arc.
The ligaments of the knee are classified as extracapsular or intracapsular. The main extracapsular ligaments are the medial and lateral collaterals (MCL and LCL). The main intracapsular ligaments are the anterior and posterior cruciate ligaments (ACL and PCL), which are extrasynovial. The collateral ligaments provide lateral stability and stability in extension, whereas the cruciate ligaments provide knee stability in flexion.
Knee stability is further enhanced by muscular extensions, such as the vastus medialis giving patella stability, the fibrous extension of vastus lateralis and medialis (the patellar retinaculum) strengthening the knee anteriorly and the iliotibial tract strengthening the knee in slight flexion.
Clinical assessment
An exact history of the mechanism of injury, degree of force, presence of immediate swelling and the ability to bear weight straight after the injury are essential to guide the diagnosis of soft-tissue injuries. Injury may be due to direct or indirect trauma and may involve valgus or varus stress.
Knee physical examination
Always examine both legs with the patient undressed and lying supine on a trolley (not sitting). Visual inspection may reveal swelling, bruising, erythema, deformity and/or an associated wound.
Swelling appearing within the first few hours of trauma is usually associated with a haemarthrosis due to a vascular response to subchondral, bone or synovial injury. Swelling developing gradually over several hours to days is more likely due to a serous effusion from a synovial reaction.
Knee palpation
Start palpation away from the point of trauma to detect warmth, swelling, crepitus, muscle mass and neurovascular status and then to localize the areas of maximal tenderness to define the underlying pathology. Assess the insertion points of the quadriceps tendon, patellar tendon, collateral ligaments and the medial and lateral joint lines, as well as the bony structures of the knee joint.
Assess active and passive movements of the knee joint, noting the degree of flexion, extension and internal and external rotation. Always test for the ability to straight leg raise while supine, to assess for potential damage to the extensor mechanism of the knee.
Anterior and posterior drawer tests
Complete the examination with an assessment of the knee’s functional stability. The stability of the anterior and posterior cruciate ligaments may be crudely determined with the anterior and posterior drawer tests. Ligamentous laxity decreases with age, so comparison with the opposite knee is more important than absolute laxity.
The patient must be supine with the hip flexed at 45°, the knee flexed at 90° and the hamstrings relaxed. The examiner sits on the patient’s foot to stabilize the limb and attempts to demonstrate abnormal forward movement of the tibia on the femoral condyles (positive anterior drawer test) and/or abnormal backward movement of the tibia on the femoral condyles (positive posterior drawer test). However, the accuracy of the anterior drawer test, as defined by subsequent arthroscopy, is only 56% for rupture of the ACL, whereas posterior displacement of the tibia by more than 5 mm is indicative of PCL ruptures with a specificity of 85%.
Lachman’s test
Lachman’s test is a more sensitive manoeuvre in the acute setting for testing ACL integrity, with a sensitivity of 86% and specificity of 91% [1]. The operator supports the distal femur with one hand with the knee in 20–30° of flexion and uses the other hand to draw the tibia forwards on the femoral condyles. Increased anterior displacement of the proximal tibia compared to the unaffected limb indicates a positive test.
Collateral laxity
The collateral ligaments are assessed by applying a varus or valgus stress to the knee in 0° and 30° of flexion. The degree of ligamentous laxity is determined by the amount of movement produced between the tibia and fibula, compared to the normal side.
McMurray’s test
McMurray’s test is used to demonstrate a meniscal injury. The patient lies supine and the knee is passively flexed and extended. One hand is placed over the knee to feel for crepitus while the other hand rotates the tibia on the femur. Internal rotation tests the lateral meniscus and external rotation tests the medial meniscus. Pain and crepitus at the extremes of movement indicate a positive test.
Apley’s test
Apley’s test is also used to demonstrate a meniscal injury. This is performed with the patient lying prone with the knee flexed to 90°. The tibia is rotated on the femur with downward pressure on the heel. Meniscal tears are associated with pain on downward pressure at the extremes of movement, and relieved by the release of pressure.
Radiology
Clinical decision rules to determine the requirement for knee radiography aim to reduce emergency department (ED) radiographs, waiting times and costs. The most widely used is the Ottawa knee rule.
Ottawa knee rule
The Ottawa knee rule states an X-ray is indicated for acute knee injury in adults with any of the following:
 tenderness at the head of the fibula
tenderness at the head of the fibula
 isolated tenderness of the patella
isolated tenderness of the patella
 inability to bear weight (take four steps) immediately and in the ED.
inability to bear weight (take four steps) immediately and in the ED.
This rule has been validated in a number of studies, with a pooled sensitivity of 98.5% and specificity of 48.6% [2].
Standard knee X-rays
Standard knee X-ray evaluation includes AP and lateral views. The AP view assesses for the integrity of the medial and lateral joint spaces and the femoral tibial angle. It also shows the size, position and integrity of the patella.
Lateral view may identify a lipohaemarthrosis effusion, seen as a horizontal line demarcating darker, more radiolucent fat floating on lighter, more radiodense blood. This is indicative of an intra-articular fracture and is most helpful when the actual injury is hard to see, such as with an undisplaced condylar fracture, patellar or tibial spine fracture.
Oblique X-rays are helpful in elucidating a tibial plateau fracture. The tunnel view enhances the intercondylar region.
A skyline X-ray is taken to evaluate further the patella and patellofemoral joint, particularly following reduction of a patellar dislocation. It can identify undisplaced vertical fractures of the patella and subtle subluxation not seen on the conventional views.
Computed tomography
Computed tomography (CT) is important to define fractures, such as those of the tibial plateau. Magnetic resonance imaging (MRI) is reserved for evaluation of complex soft-tissue knee injuries, unless arthroscopy is preferred.
Fractures around the knee joint
Distal femur
Distal femoral fractures account for 4% of femoral fractures. They are usually associated with high-energy injuries secondary to a fall or a direct blow to the femur in a motor vehicle incident.
Classification
Distal femoral fractures are divided anatomically into supracondylar, intercondylar and isolated condylar fractures. Supracondylar fractures are extra-articular and occur immediately above the femoral condyles. Intercondylar fractures involve separation of the femoral condyles. Although the fracture line may extend through the supracondylar region, in general, these are treated as intra-articular fractures.
Isolated condylar fractures are uncommon and occur when a varus or valgus force is applied to a weight-bearing, extended knee. The tibial eminence is driven into the femoral intercondylar notch, creating an intra-articular fracture associated with significant ligamentous disruption.
Clinical assessment
Patients with an injury to the distal femur are in significant pain and unable to bear weight. Examination may reveal swelling, deformity, rotation and shortening. The joint is tender to palpate along the medial or lateral joint lines and an acute haemarthrosis secondary to associated ligamentous injury or intra-articular involvement is common.
Examine the whole lower limb to exclude ipsilateral hip dislocation, associated tibial fracture and quadriceps damage. Assess for any neurovascular deficit, including loss of sensation in the web space between the first and second toes due to deep peroneal nerve injury.
Anteroposterior and lateral X-rays of the femur and knee reveal the fracture and its degree of displacement or comminution. A pelvic X-ray is necessary to exclude an associated proximal femur fracture or hip dislocation.
Management
Administer adequate analgesia and apply a splint in the ED to prevent movement at the fracture site. Distal femoral fractures are a complex orthopaedic problem and long-term complications of malunion, quadriceps adhesion and osteoarthritis are common.
Early orthopaedic input is required in all cases. Fractures with joint incongruity or displacement require open reduction and internal fixation. Cast immobilization alone may be sufficient for undisplaced or impacted fractures without joint involvement, particularly in the elderly patient [3].