Procedure 4 Odontoid Screw Fixation
Indications
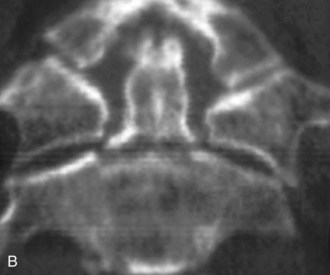
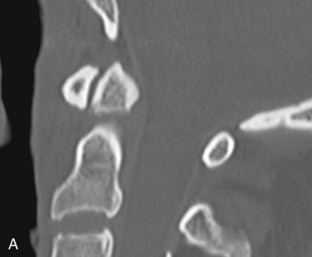
 For surgical fixation of recent (less than 6 months old) type II and some high type III odontoid fractures (Figure 4-1, A and B)
For surgical fixation of recent (less than 6 months old) type II and some high type III odontoid fractures (Figure 4-1, A and B)
Indications Pitfalls
• Type III fractures with significant vertebral body involvement because of poor proximal screw fixation
• Transverse ligament disruption (atlantodental interval [ADI] >3 mm). Although magnetic resonance imaging (MRI) has been recommended by some for evaluation of transverse ligament rupture, the authors do not recommend this modality unless neurologic deficits or increased ADI are identified. In the authors’ experience, transverse ligament rupture in the setting of odontoid fracture is very rare.
• Chronic nonunion. Fractures older than 6 months or fractures with sclerotic margins have a much lower fusion rate and should be treated by posterior atlantoaxial arthrodesis.
• Nonreducible canal compromise. Intraoperative reduction has been considered more feasible by a posterior approach in combination with atlantoaxial arthrodesis; however, the guide-tube system to be described allows realignment intraoperatively before placement of an odontoid screw. In the authors’ experience, almost all acute fractures are reducible with traction or intraoperatively.
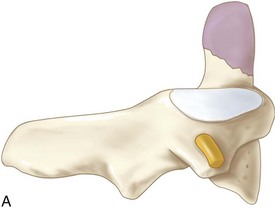
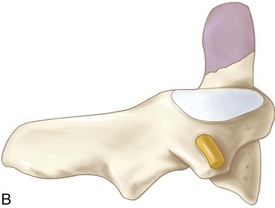
• Anterior oblique fractures (posterior superior to anterior inferior) can be difficult to reduce and maintain in good alignment with odontoid screw fixation (Figure 4-2, A). Because the screw crosses the fracture line at an angle, and thus tends to pull the odontoid anteriorly, these fractures have lower fusion rates. In the authors’ previously reported series, patients with anterior oblique fractures had an approximately twofold greater risk of nonunion after odontoid screw fixation than did those with horizontal or posterior oblique fractures (anterior superior to posterior inferior) (Figure 4-2, B). By fixing these fractures with the odontoid positioned in a slightly posterior position and using a hard collar type of external orthosis, the authors have usually been able to achieve successful fixation and healing in these patients.
Indications Controversies
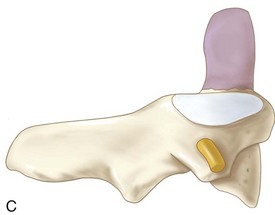
• Type III fractures (Figure 4-2, C)
• Chronic nonunion. Although it has been reported that chronic nonunion can be treated with curettage and odontoid screw fixation, the fusion rates are very low, and this fracture is probably better treated with posterior C1-C2 fusion.
• Treatment of the elderly. In the authors’ experience, this procedure is well tolerated in older patients and allows for early mobilization with fewer general medical complications. The incidence of temporary postoperative dysphagia is greater in this group.
• Most cost-effective alternative
• Procedure is suited for patients of all ages, including the elderly.
Examination/Imaging
 Neurologic and musculoskeletal examination
Neurologic and musculoskeletal examination
 Anteroposterior (AP), lateral, and open-mouth cervical spine radiographs to assess alignment and other fractures. Note that plain films alone are only 65% to 95% sensitive for axis fractures.
Anteroposterior (AP), lateral, and open-mouth cervical spine radiographs to assess alignment and other fractures. Note that plain films alone are only 65% to 95% sensitive for axis fractures.
Treatment Options
• Nontreatment may be considered for severely debilitated elderly patients.
• External orthoses have poor fusion rates except in younger patients. The worst fusion rates occur in older patients, patients with fractures with large gaps or subluxations, and those with comminuted fractures.
• Treatment with all forms of external orthosis requires close follow-up and 3 to 6 months of significant activity restrictions.
Surgical Anatomy
Anatomy Pearls
• Biplanar fluoroscopy is advantageous (Figure 4-4, A).
• A folded blanket is placed behind the patient’s shoulders to allow maximal cervical extension, which may be needed to obtain an appropriate odontoid screw trajectory.
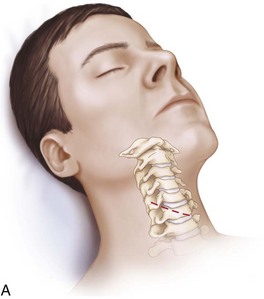
• The head is initially kept in neutral position until reduction can be achieved. Halter traction with 10 lb of traction is used to stabilize the head and neck and elevate the chin (Figure 4-4, C).
Positioning
Portals/Exposures
 The initial approach is a standard Cloward or Smith-Robinson approach to the C5-6 level.
The initial approach is a standard Cloward or Smith-Robinson approach to the C5-6 level.
 A small unilateral skin incision is made along the natural skin crease at approximately C5. Either side can be approached, but the right side is often preferred by right-handed surgeons.
A small unilateral skin incision is made along the natural skin crease at approximately C5. Either side can be approached, but the right side is often preferred by right-handed surgeons.
 The platysma muscle is divided horizontally.
The platysma muscle is divided horizontally.
 The sternocleidomastoid muscle is identified and the fascia along the medial border of this muscle is opened sharply.
The sternocleidomastoid muscle is identified and the fascia along the medial border of this muscle is opened sharply.
 The carotid artery is palpated to ensure that the approach is continued medial to this structure.
The carotid artery is palpated to ensure that the approach is continued medial to this structure.
 Blunt dissection of natural tissue planes provides easy access to the prevertebral space. The trachea and esophagus are retracted medially.
Blunt dissection of natural tissue planes provides easy access to the prevertebral space. The trachea and esophagus are retracted medially.
 The prevertebral fascia is incised in the midline at the C5-6 level, and the longus colli muscles are elevated to allow retractor placement.
The prevertebral fascia is incised in the midline at the C5-6 level, and the longus colli muscles are elevated to allow retractor placement.
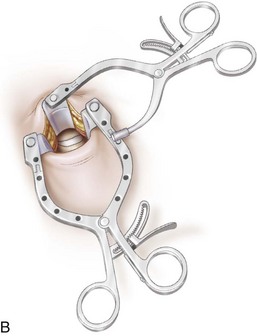
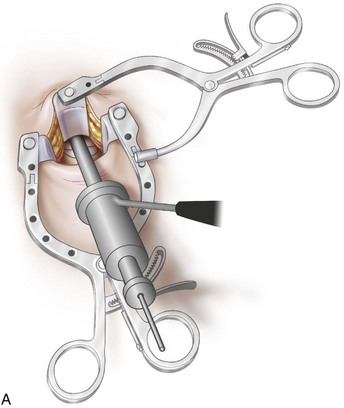
 Caspar sharp-toothed retractor blades are inserted under the longus colli bilaterally at approximately C5 and attached to a modified retractor blade holder (Figure 4-5).
Caspar sharp-toothed retractor blades are inserted under the longus colli bilaterally at approximately C5 and attached to a modified retractor blade holder (Figure 4-5).
 Blunt dissection with a Kittner dissector in the prevertebral fascial plane is carried out to C1 and confirmed on lateral fluoroscopy.
Blunt dissection with a Kittner dissector in the prevertebral fascial plane is carried out to C1 and confirmed on lateral fluoroscopy.
 A superior angled retractor blade is inserted to retract the pharyngeal tissues off the anterior upper cervical spine and protect them (see Figure 4-5). This superior retractor is secured to the modified Caspar retractor (Apfelbaum odontoid retractor system).
A superior angled retractor blade is inserted to retract the pharyngeal tissues off the anterior upper cervical spine and protect them (see Figure 4-5). This superior retractor is secured to the modified Caspar retractor (Apfelbaum odontoid retractor system).
Portals/Exposures Pearls
• Under fluoroscopy, a straight instrument can be placed alongside the neck for optimal location of the skin incision.
• Firm fixation of the Caspar blades beneath the longus muscles is crucial for proper fixation of the retractors during the procedure.
• Deflation and reinflation of the endotracheal tube cuff after placing the lateral retractor allows the endotracheal tube to be recentralized within the larynx, which may reduce the risk of recurrent laryngeal nerve injury.
Procedure
Step 1
 An entry site on the anterior inferior edge of C2 is chosen and confirmed on AP and lateral fluoroscopy.
An entry site on the anterior inferior edge of C2 is chosen and confirmed on AP and lateral fluoroscopy.
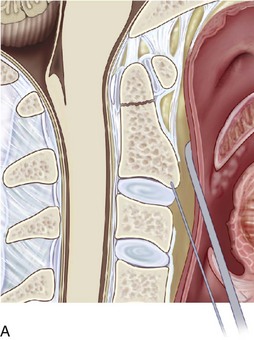
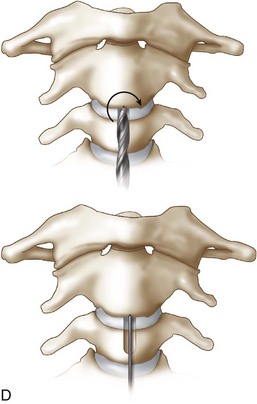
 A 2-mm Kirschner wire (K-wire) is impacted 3 to 5 mm into the desired entry site (Figure 4-6, A).
A 2-mm Kirschner wire (K-wire) is impacted 3 to 5 mm into the desired entry site (Figure 4-6, A).
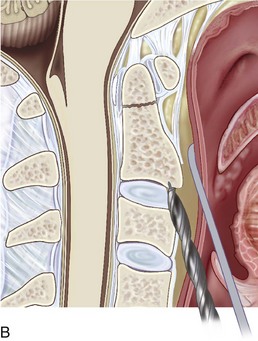
 A 7-mm hollow-core hand-twist drill is passed over the K-wire. A groove to accommodate the drill guide is drilled into the anterior face of C3 and the annulus of C2-3 (Figure 4-6, B-D).
A 7-mm hollow-core hand-twist drill is passed over the K-wire. A groove to accommodate the drill guide is drilled into the anterior face of C3 and the annulus of C2-3 (Figure 4-6, B-D).
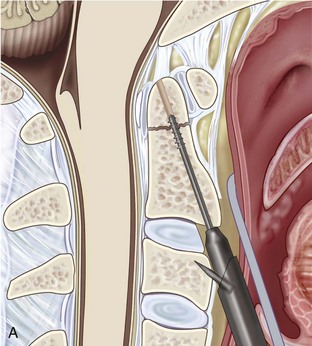
 The inner and outer drill guides are mated and placed over the K-wire.
The inner and outer drill guides are mated and placed over the K-wire.
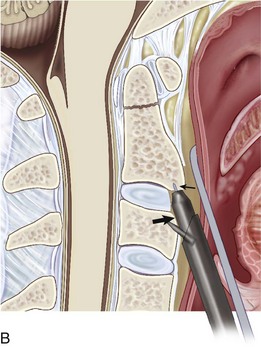
 The outer guide has forward-projecting spikes that are walked up the vertebral column, under live fluoroscopy, to overlie the C3 body.
The outer guide has forward-projecting spikes that are walked up the vertebral column, under live fluoroscopy, to overlie the C3 body.
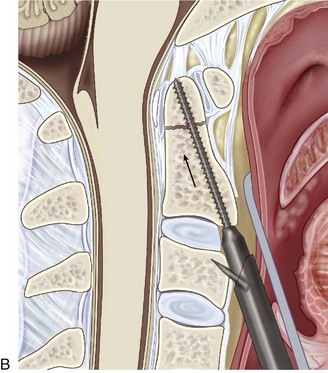
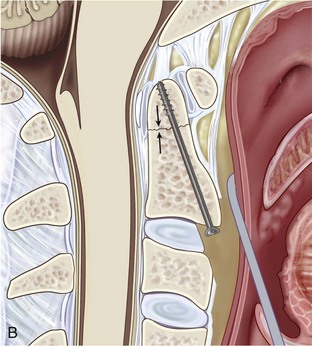
 The inner guide tube is then advanced in the previously created groove (see Figure 4-7, B, large arrow) up to the bottom of C2 (see Figure 4-7, B, small arrow). At this stage, the K-wire can be removed.
The inner guide tube is then advanced in the previously created groove (see Figure 4-7, B, large arrow) up to the bottom of C2 (see Figure 4-7, B, small arrow). At this stage, the K-wire can be removed.
Step 2
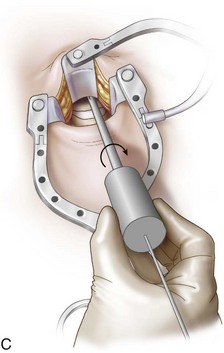
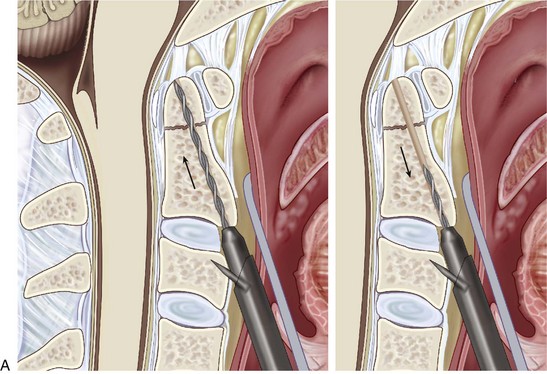
 A pilot hole is drilled through the body of C2, across the fracture gap, and into the odontoid fragment using a calibrated drill bit, with attention to drill the distal cortex of the odontoid (Figure 4-8, A).
A pilot hole is drilled through the body of C2, across the fracture gap, and into the odontoid fragment using a calibrated drill bit, with attention to drill the distal cortex of the odontoid (Figure 4-8, A).
 The inner guide is removed, and the calibrated tap is inserted into the outer guide tube.
The inner guide is removed, and the calibrated tap is inserted into the outer guide tube.
 A 4-mm, buttress-threaded cortical titanium lag screw (threaded distally only) is inserted into the guide tube and the tapped hole.
A 4-mm, buttress-threaded cortical titanium lag screw (threaded distally only) is inserted into the guide tube and the tapped hole.
 A second screw can placed in the same fashion if anatomy allows.
A second screw can placed in the same fashion if anatomy allows.
 Stability can be confirmed by flexing and extending the patient’s neck under fluoroscopy.
Stability can be confirmed by flexing and extending the patient’s neck under fluoroscopy.
 The retractors are removed, the wound is irrigated, hemostasis is ensured, and the wound is closed in layers.
The retractors are removed, the wound is irrigated, hemostasis is ensured, and the wound is closed in layers.
Postoperative Care and Expected Outcomes
 The authors observe all patients in a monitored setting overnight for acute complications, including hematoma development and respiratory compromise.
The authors observe all patients in a monitored setting overnight for acute complications, including hematoma development and respiratory compromise.
 The authors do not use external orthoses in most cases. They recommend the use of a rigid collar in the case of an anterior oblique fracture (posterior superior to anterior inferior) and in patients who are very osteoporotic.
The authors do not use external orthoses in most cases. They recommend the use of a rigid collar in the case of an anterior oblique fracture (posterior superior to anterior inferior) and in patients who are very osteoporotic.
 AP and lateral plain radiographs are sufficient, but CT scanning should be considered if any concern exists about screw placement.
AP and lateral plain radiographs are sufficient, but CT scanning should be considered if any concern exists about screw placement.
 Early ambulation is critical, especially in elderly patients.
Early ambulation is critical, especially in elderly patients.
 Fusion rates of 85% to 95% have been demonstrated in numerous studies.
Fusion rates of 85% to 95% have been demonstrated in numerous studies.
 Full range of cervical motion was present in 83% of patients after fusion.
Full range of cervical motion was present in 83% of patients after fusion.
Apfelbaum RI, Kriskovich MD, Haller JR. On the incidence, cause and prevention of recurrent laryngeal nerve palsies during anterior cervical spine surgery. Spine. 2000;25:2906-2912.
Apfelbaum RI, Lonser RR, Veres R, Casey A. Direct anterior screw fixation for recent and remote odontoid fractures. J Neurosurg. 2000;93(Suppl 2):227-236.
Dailey AT, Hart D, Finn MA, Schmidt MH, Apfelbaum RI. Anterior fixation of odontoid fractures in an elderly population. J Neurosurg Spine. 2010;12:1-8.
Fountas KN, Kapsalaki EZ, Karampelas I, et al. Results of long-term follow-up in patients undergoing anterior screw fixation for type II and rostral type III odontoid fractures. Spine. 2005;30:661-669.
Greene KA, Dickman CA, Marciano FF, et al. Acute axis fractures: analysis of management and outcome of 340 consecutive cases. Spine. 1997;22:1843-1852.
Jenkins JD, Coric D, Branch CLJr. A clinical comparison of one- and two-screw odontoid fixation. J Neurosurg. 1998;89:366-370.
Majercik S, Tashjian RZ, Biffl WL, Harrington DT, Cioffi WG. Halo vest immobilization in the elderly: a death sentence? J Trauma. 2005;59:350-357.
Montesano PX, Anderson PA, Schlehr F, Thalgott JS, Lowrey G. Odontoid fractures treated by anterior odontoid screw fixation. Spine. 1991;16(Suppl 3):S33-S37.
Sasso R, Doherty BJ, Crawford MJ, Heggeness MH. Biomechanics of odontoid fracture fixation: comparison of the one- and two-screw technique. Spine. 1993;18:1950-1953.
Subach BR, Morone MA, Haid RWJr, et al. Management of acute odontoid fractures with single-screw anterior fixation. Neurosurgery. 1999;45:812-819. discussion 819-20