Procedure 39 Lumbar Internal Laminectomy
Indications
 Lumbar stenosis in the setting of unilateral disk herniation
Lumbar stenosis in the setting of unilateral disk herniation
 Low-grade degenerative spondylolisthesis without gross instability on flexion-extension views
Low-grade degenerative spondylolisthesis without gross instability on flexion-extension views
Surgical Anatomy
 The pars interarticularis should be identified, because violation of this structure may predispose to instability.
The pars interarticularis should be identified, because violation of this structure may predispose to instability.
 The location of the pedicle should be established early in the procedure. Localization is based on the pedicle of the inferior level being decompressed (e.g., the L5 pedicle in an L4-5 decompression.
The location of the pedicle should be established early in the procedure. Localization is based on the pedicle of the inferior level being decompressed (e.g., the L5 pedicle in an L4-5 decompression.
 Certain anatomic configurations of the lumbar spine facilitate easier decompression by this approach. If the transverse diameter of the lumbar spinal canal is congenitally narrowed, then the position of the posterior osseous roof of the spinal canal will be relatively vertical. This configuration will allow easy achievement of an optimal working angle of the microscope, which will facilitate contralateral decompression of bone and ligamentum flavum. Conversely, if the anteroposterior diameter of the spinal canal is congenitally narrowed, then the position of the osseous canal roof will be relatively horizontal. In this case, achieving an optimal working angle for the visualization of the contralateral structures will be more difficult.
Certain anatomic configurations of the lumbar spine facilitate easier decompression by this approach. If the transverse diameter of the lumbar spinal canal is congenitally narrowed, then the position of the posterior osseous roof of the spinal canal will be relatively vertical. This configuration will allow easy achievement of an optimal working angle of the microscope, which will facilitate contralateral decompression of bone and ligamentum flavum. Conversely, if the anteroposterior diameter of the spinal canal is congenitally narrowed, then the position of the osseous canal roof will be relatively horizontal. In this case, achieving an optimal working angle for the visualization of the contralateral structures will be more difficult.
Positioning
Portals/Exposures
 This technique is theoretically advantageous to bilateral microdecompression as well as standard laminectomy, because unilateral exposure may result in reduction of risk for disruption of spinal stability and less postoperative pain.
This technique is theoretically advantageous to bilateral microdecompression as well as standard laminectomy, because unilateral exposure may result in reduction of risk for disruption of spinal stability and less postoperative pain.
 Because only the ipsilateral paraspinal musculature is dissected unilaterally, the contralateral paraspinal musculature remains intact, resulting in the preservation of the contralateral bone/muscle complex. This conceivably results in added postoperative stability compared with a bilateral approach.
Because only the ipsilateral paraspinal musculature is dissected unilaterally, the contralateral paraspinal musculature remains intact, resulting in the preservation of the contralateral bone/muscle complex. This conceivably results in added postoperative stability compared with a bilateral approach.
 A study by Adams and associates suggested that the muscular attachments to the posterior arch and the insertions of the muscular slips on the facet capsule serve to brace the facets, improving their ability to resist displacement.
A study by Adams and associates suggested that the muscular attachments to the posterior arch and the insertions of the muscular slips on the facet capsule serve to brace the facets, improving their ability to resist displacement.
 Because dissection and retraction of the multifidus muscle is carried out unilaterally with this technique, less postoperative dead space results.
Because dissection and retraction of the multifidus muscle is carried out unilaterally with this technique, less postoperative dead space results.
 Postoperative dead space can have significant consequences. Increased volume of the dead space may result in increased blood loss. Moreover, increased dead space provides an ideal bacterial culture medium, with the potential for increasing the chance of a postoperative infection.
Postoperative dead space can have significant consequences. Increased volume of the dead space may result in increased blood loss. Moreover, increased dead space provides an ideal bacterial culture medium, with the potential for increasing the chance of a postoperative infection.
Procedure
Step 1
 A longitudinal skin incision is made over the affected segment.
A longitudinal skin incision is made over the affected segment.
 Subsequently, the lumbodorsal fascia incision is made ipsilaterally, approximately 1 cm off midline on the side that is more symptomatic.
Subsequently, the lumbodorsal fascia incision is made ipsilaterally, approximately 1 cm off midline on the side that is more symptomatic.
 The multifidus muscle is subsequently retracted off the spinous process and lamina.
The multifidus muscle is subsequently retracted off the spinous process and lamina.
 Alternatively, the approach using a tubular retractor system has also been described.
Alternatively, the approach using a tubular retractor system has also been described.
Step 2
 A laminotomy is subsequently performed on the ipsilateral side, with the ipsilateral cephalad lamina partially removed using a high-speed drill and Kerrison rongeurs. The resection of the cephalad lamina should be extended until the insertion of the ligamentum flavum and the dura are visible. This may be performed in a “trumpeted” fashion to preserve as much of the lamina as possible by angling the microscope. The ligamentum flavum is exposed.
A laminotomy is subsequently performed on the ipsilateral side, with the ipsilateral cephalad lamina partially removed using a high-speed drill and Kerrison rongeurs. The resection of the cephalad lamina should be extended until the insertion of the ligamentum flavum and the dura are visible. This may be performed in a “trumpeted” fashion to preserve as much of the lamina as possible by angling the microscope. The ligamentum flavum is exposed.
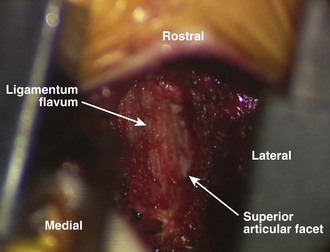
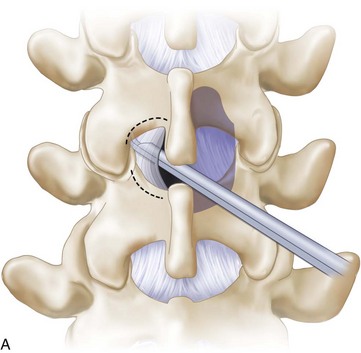
 The mesial inferior facet is drilled so that the superior articular facet can be visualized. Figure 39-1 is a postlaminotomy intraoperative photograph that shows removal of the mesial surface of the inferior facet. Note the exposed superior articular facet.
The mesial inferior facet is drilled so that the superior articular facet can be visualized. Figure 39-1 is a postlaminotomy intraoperative photograph that shows removal of the mesial surface of the inferior facet. Note the exposed superior articular facet.
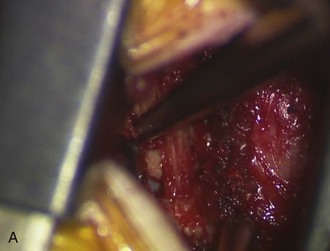
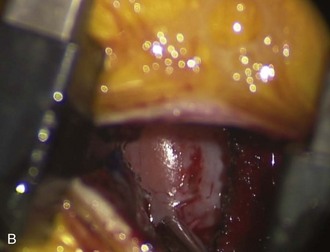
 The ligamentum flavum is then elevated using curettes and dissectors. A curette is used to release the ligamentum flavum, first medially (Figure 39-2, A), then laterally (Figure 39-2, B). Note that the curette stays in the plane between the bone and the ligamentum.
The ligamentum flavum is then elevated using curettes and dissectors. A curette is used to release the ligamentum flavum, first medially (Figure 39-2, A), then laterally (Figure 39-2, B). Note that the curette stays in the plane between the bone and the ligamentum.
 The ligamentum flavum is subsequently resected. The ligamentum flavum is elevated with a dental tool (Figure 39-3, A) and then resected with a Kerrison rongeur (Figure 39-3, B). The microscope is then angled toward the ipsilateral facet and subarticular zone.
The ligamentum flavum is subsequently resected. The ligamentum flavum is elevated with a dental tool (Figure 39-3, A) and then resected with a Kerrison rongeur (Figure 39-3, B). The microscope is then angled toward the ipsilateral facet and subarticular zone.
 After entering the spinal canal, the first structure to be identified should be the pedicle. The pedicle serves as a reference point for the decompression and orients the surgeon both in terms of locating the foramen and locating neural structures. Descending nerve roots are always medial to the pedicle.
After entering the spinal canal, the first structure to be identified should be the pedicle. The pedicle serves as a reference point for the decompression and orients the surgeon both in terms of locating the foramen and locating neural structures. Descending nerve roots are always medial to the pedicle.
Step 2 Pearls
• The authors use a straight curette to detach the ligamentum flavum from the inferior lamina and the superior articular facet. This is followed by use of a curved curette to ensure the ligamentum is detached.
• Afterward, a no. 2 Kerrison rongeur is used to perform the initial bite of bone to minimize the risk of compressive neural injury.
• The authors generally attempt to avoid removal of bone from the inferior lamina rostral edge, because this may predispose to pars fracture.
Step 3
 Using Kerrison rongeurs, the ipsilateral lateral recess and foramen is decompressed (Figure 39-4). All soft tissue and bony stenosing pathology is resected from the recess and foramen.
Using Kerrison rongeurs, the ipsilateral lateral recess and foramen is decompressed (Figure 39-4). All soft tissue and bony stenosing pathology is resected from the recess and foramen.
 A Murphy probe or a Woodson dissector should be easily passable through and out the foramen.
A Murphy probe or a Woodson dissector should be easily passable through and out the foramen.
 The facetectomy should also be performed in a “trumpeted” manner to preserve the pars interarticularis and facet joint.
The facetectomy should also be performed in a “trumpeted” manner to preserve the pars interarticularis and facet joint.
 Using a high-speed burr, the facet complex is undercut to avoid destabilizing the joint.
Using a high-speed burr, the facet complex is undercut to avoid destabilizing the joint.
Step 4
 Attention is then turned toward the contralateral side.
Attention is then turned toward the contralateral side.
 The microscope is angled toward the opposite side, and the patient can also be tilted contralaterally to allow visualization underneath the deepest portion of the interspinous ligament.
The microscope is angled toward the opposite side, and the patient can also be tilted contralaterally to allow visualization underneath the deepest portion of the interspinous ligament.
 The base of the spinous process, as well as the deepest portion of the interspinous ligament, is then undercut with the drill, taking care to avoid detaching the spinous process. The base of the spinous process must be adequately undercut to achieve sufficient contralateral visualization. In many cases, the “wishbone” portion of the cephalad and caudal lamina, that is, the junction of the lamina with the spinous process, must be resected. A high-speed burr is used to undercut the spinous process and drill the undersurface of the contralateral lamina (Figure 39-5).
The base of the spinous process, as well as the deepest portion of the interspinous ligament, is then undercut with the drill, taking care to avoid detaching the spinous process. The base of the spinous process must be adequately undercut to achieve sufficient contralateral visualization. In many cases, the “wishbone” portion of the cephalad and caudal lamina, that is, the junction of the lamina with the spinous process, must be resected. A high-speed burr is used to undercut the spinous process and drill the undersurface of the contralateral lamina (Figure 39-5).
 Once the contralateral ligamentum flavum can be visualized adequately, a dissector is used to confirm that the anterior surface of the ligamentum flavum is free from the underlying dura. A curette is used to separate dura from ligamentum flavum (Figure 39-6).
Once the contralateral ligamentum flavum can be visualized adequately, a dissector is used to confirm that the anterior surface of the ligamentum flavum is free from the underlying dura. A curette is used to separate dura from ligamentum flavum (Figure 39-6).
 The ligamentum flavum can then be removed using Kerrison rongeurs and curettes. Figure 39-7, A is an illustration showing contralateral ligamentum flavum being removed with Kerrison rongeurs. In Figure 39-7, B, the contralateral ligamentum flavum is being resected under the operating microscope.
The ligamentum flavum can then be removed using Kerrison rongeurs and curettes. Figure 39-7, A is an illustration showing contralateral ligamentum flavum being removed with Kerrison rongeurs. In Figure 39-7, B, the contralateral ligamentum flavum is being resected under the operating microscope.
 A malleable retractor or a Penfield dissector may be placed underneath the spinous process to protect the underlying dura and neural elements during decompression (Figure 39-8).
A malleable retractor or a Penfield dissector may be placed underneath the spinous process to protect the underlying dura and neural elements during decompression (Figure 39-8).
 Finally, the decompression is completed by undercutting of the contralateral medial facet using Kerrison rongeurs until a probe can be passed freely into the foramen. Figure 39-9 shows decompression of the contralateral lateral recess and foramen with a Kerrison. Figure 39-10 shows use of a dental tool (also known as a hockey stick) dissector to assess adequacy of contralateral and lateral recess decompression.
Finally, the decompression is completed by undercutting of the contralateral medial facet using Kerrison rongeurs until a probe can be passed freely into the foramen. Figure 39-9 shows decompression of the contralateral lateral recess and foramen with a Kerrison. Figure 39-10 shows use of a dental tool (also known as a hockey stick) dissector to assess adequacy of contralateral and lateral recess decompression.
Step 4 Pearls
• In areas of tight adhesions between ligamentum and dura, small pieces of ligamentum flavum can be left behind.
• The removal of the ligamentum flavum and medial facetectomies bilaterally serves to effectively increase the cross-sectional area of the spinal canal.
• See Figure 39-11, A and B for a schematic and photograph, respectively, showing the spinal canal after bilateral decompression by unilateral laminotomy.
Step 4 Pitfalls
• Unintentional durotomy is perhaps the most common complication seen with this procedure. Any dorsal durotomy should be repaired in a watertight manner with suture and a collagen overlay. The authors use fibrin glue, but hydrogel polymers are an alternative.
• Occasionally, a durotomy occurs over a root sleeve or is not sewable because of an extremely thin dura. On those occasions, the authors repair the dura with a collagen overlay and glue without suturing.
Postoperative Care and Expected Outcomes
 Complications associated with this procedure include infection, unintended durotomy and possible cerebrospinal fluid leak, nerve root injury, and postoperative instability.
Complications associated with this procedure include infection, unintended durotomy and possible cerebrospinal fluid leak, nerve root injury, and postoperative instability.
 The risk of progression of instability after such a decompression has been estimated at 10% to 15%.
The risk of progression of instability after such a decompression has been estimated at 10% to 15%.
 In cases of spondylolisthesis or deformity, there is a higher chance of surgical failure. Patients should be counseled about this preoperatively.
In cases of spondylolisthesis or deformity, there is a higher chance of surgical failure. Patients should be counseled about this preoperatively.
Adams M, Hutton W, Stott J. The resistance to flexion of the lumbar intervertebral joint. Spine. 1980;5:245-253.
Oertel M, Ryang Y, Korinth M, et al. Long-term results of microsurgical treatment of lumbar spinal stenosis by unilateral laminotomy for bilateral decompression. Neurosurgery. 2006;59:1264-1269.
Orpen N, Corner J, Shetty R, et al. Micro-decompression for lumbar spinal stenosis: the early outcome using a modified surgical technique. J Bone Joint Surg Br. 2010;92:550-554.
Spetzger U, Bertalanffy H, Reinges M, et al. Unilateral laminotomy for bilateral decompression of lumbar spinal stenosis. Part II: clinical experiences. Acta Neurochirugica. 1997;139:397-403.
Weiner B, Walker M, Brower R, McCulloch JA. Microdecompression for lumbar spinal canal stenosis. Spine. 1999;24:2268-2272.