Peripheral Nerve Stimulators
PREREQUISITE NURSING KNOWLEDGE
• Peripheral nerve stimulators (PNSs) are used in association with the administration of neuromuscular blocking drugs (NMBDs) to block skeletal muscle activity.
• NMBDs are given in the intensive care unit, along with sedatives and opioids, most commonly to coordinate contemporary modes of mechanical ventilation with breathing in patients with severe lung injury. Neuromuscular blocking agents are also used to assist with the management of increased intracranial pressure after a head injury; for severe muscle spasms associated with seizures, tetanus, and drug overdose; to reduce intraabdominal hypertension1; in hypothermia protocols for cardiac arrest6; and for preservation of delicate reconstructive surgery.
• NMBDs do not affect sensation or level of consciousness. Because NMBDs lack amnesic, sedative, and analgesic properties, sedatives and analgesics should always be given concurrently to minimize the patient’s awareness of blocked muscle activity and discomfort. Sedatives and analgesics should be initiated before NMBDs because neuromuscular blockade hinders the assessment of anxiety and pain.5
• Numerous medications, such as aminoglycosides and other antibiotics, beta blockers, calcium channel blockers, corticosteroids, and anesthetics, and conditions, such as acidosis and various electrolyte imbalances, potentiate the effects of neuromuscular blocking agents. Thus, the level of blockade is subject to variation, which necessitates vigilant monitoring with a PNS and titration of the NMBD.6
• The muscle twitch response to a small electrical stimulus delivered by the PNS corresponds to an estimated number of nerve receptors blocked by the NMBDs and assists the clinician in the assessment and titration of the medication dosage. The level of blockade is estimated by observing the muscle twitch after stimulating the appropriate nerve with a small electrical current delivered by the PNS.
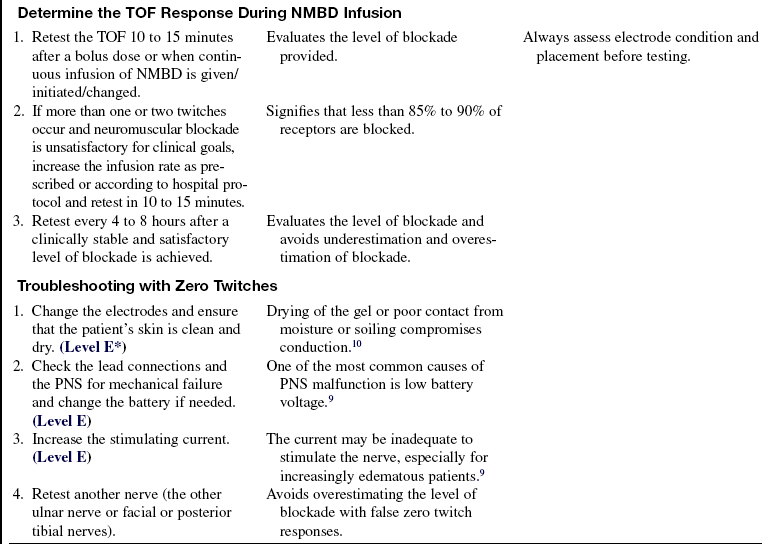
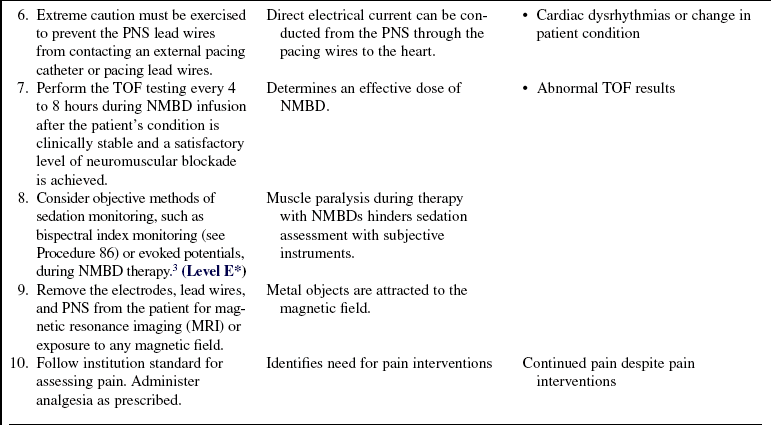
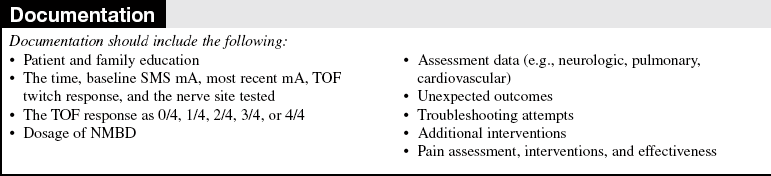
• The train-of-four (TOF) method of stimulation is most commonly used for ongoing monitoring of NMBD use. After delivery of four successive stimulating currents to a select peripheral nerve with the PNS, in the absence of significant neuromuscular blockade, four muscle twitches follow. The four twitches signify that 75% or fewer of the receptors are blocked. Three twitches correspond to approximately 80% blockade, and two to one twitches in response to four stimulating currents correlate with approximately 85% to 90% blockade of the neuromuscular junction receptors.9 One to two twitches is the recommended level of block, although the appropriate level has not yet been determined through research in the critically ill population.5 Absence of twitches may indicate that 100% of receptors are blocked, which exceeds the desired level of blockade (Table 38-1).
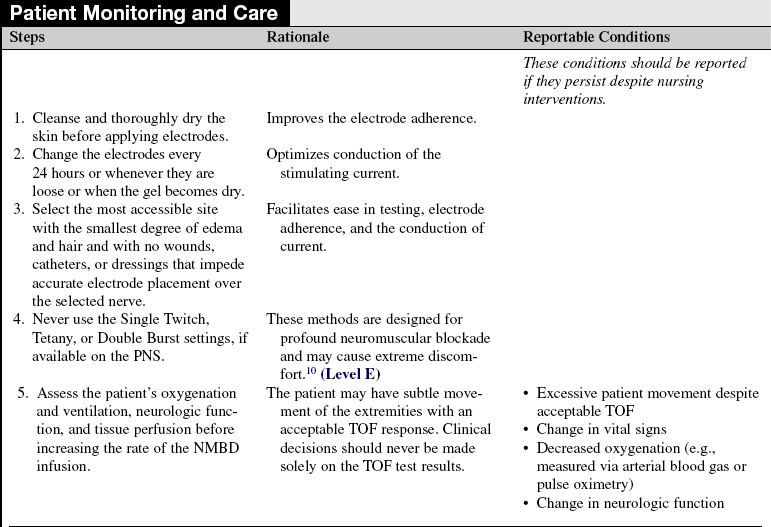
Table 38-1
Train-of-Four Stimulation as a Correlation of Blocked Nerve Receptors
| TOF (No. of Twitches) | Percent of Receptors Blocked (Approximately)7 |
| 0/4 | 100 |
| 1/4 | 90 |
| 2/4 | 85 |
| 3/4 | 80 |
| 4/4 | 75 or less |
Nagelhout JJ, Naglaniczny KL: Nurse anesthesia, ed 3, Philadelphia, 2004, Saunders.
• The stimulating current is measured in milliamperes (mA). The usual range of mA required to stimulate a peripheral nerve and elicit a muscle twitch is 20 to 50 mA, although increasing the current to 70 or 80 mA may be necessary, especially in the obese patient.9
• Some stimulators do not indicate the mA. Instead, digital or dialed numbers ranging from 1 to 10 represent the range of mA from 20 to 80 mA. With use of these instruments, the usual setting is 2 to 5, although a setting of 10 is sometimes necessary. Other stimulators (with and without digital displays) automatically adjust the voltage output relative to resistance and deliver the current accordingly.10
• The ulnar nerve in the wrist is recommended for testing, although the facial and the posterior tibial nerves may also be used.
• Peripheral nerve monitoring is used in conjunction with the assessment of clinical goals, and clinical decisions should never be made solely on the basis of the twitch response.
• Titration of the drugs according to clinical assessment and muscle twitch response may help provide a sufficient level of blockade without overshooting the goal. Overshooting the level of blockade with use of excessive doses of NMBDs is of special concern in the critically ill patient because it may predispose the patient to prolonged paralysis and muscle weakness, reported extensively in the literature.6 Monitoring with a PNS during the administration of NMBDs results in the use of less medication, hastens recovery of spontaneous ventilation, and accelerates restoration of neuromuscular transmission (NMT),2 which is necessary for resumption of muscle activity. Although some patients have severe muscle weakness after neuromuscular blockade, peripheral nerve monitoring during NMBD therapy facilitates prompt recovery of NMT when therapy is terminated.2
EQUIPMENT
PATIENT AND FAMILY EDUCATION
• Explain the purpose of peripheral nerve monitoring, for example, assessing the effect and guiding the dosage of drug.  Rationale: This explanation may decrease anxiety.
Rationale: This explanation may decrease anxiety.
• Describe the equipment to be used.  Rationale: This description may decrease anxiety.
Rationale: This description may decrease anxiety.
• Reassure the patient and family that medications for sedation and analgesia are provided throughout this therapy so the patient is comfortable while paralyzed.  Rationale: Reassurance that the patient’s pain and anxiety will be treated during therapy is provided.
Rationale: Reassurance that the patient’s pain and anxiety will be treated during therapy is provided.
• Describe the experience of the stimuli as a slight prickly sensation.  Rationale: The use of sensation descriptors is effective in reducing anxiety.
Rationale: The use of sensation descriptors is effective in reducing anxiety.
• Explain that the electrodes require periodic changing, which feels like removing an adhesive-backed bandage.  Rationale: This explanation may elicit decreased anxiety.
Rationale: This explanation may elicit decreased anxiety.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Assess the patient for the best location for electrode placement. Consider criteria such as edema, fat, hair, diaphoresis, wounds, dressings, and arterial and venous catheters.  Rationale: This assessment improves conduction of stimulating current through dermal tissue.
Rationale: This assessment improves conduction of stimulating current through dermal tissue.
• Assess the patient for history or presence of hemiplegia, hemiparesis, or peripheral neuropathy.  Rationale: Motor response to nerve stimulation of the affected limb may be diminished; receptors may be resistant to NMBDs and lead to excess doses.9
Rationale: Motor response to nerve stimulation of the affected limb may be diminished; receptors may be resistant to NMBDs and lead to excess doses.9
• Assess whether burns are present or whether topical ointments are being used.  Rationale: In patients with burns or topical ointments, for whom electrode adherence is difficult, a bipolar touch probe may be more effective than the electrode pads and lead wires. Poor electrode adherence interferes with the conduction of the stimulating current.
Rationale: In patients with burns or topical ointments, for whom electrode adherence is difficult, a bipolar touch probe may be more effective than the electrode pads and lead wires. Poor electrode adherence interferes with the conduction of the stimulating current.
Patient Preparation
• Ensure that the patient and family understand pre-procedural teachings. Answer questions as they arise and reinforce information as needed.  Rationale: Evaluates and reinforces understanding of previously taught information.
Rationale: Evaluates and reinforces understanding of previously taught information.
• Clip hair at the electrode placement sites if necessary.  Rationale: This action improves electrode contact, which facilitates current flow to the nerve.
Rationale: This action improves electrode contact, which facilitates current flow to the nerve.
• Cleanse skin and degrease with alcohol.  Rationale: Cleansing improves electrode contact, which facilitates current flow to the nerve
Rationale: Cleansing improves electrode contact, which facilitates current flow to the nerve
• Apply the electrodes and test the TOF response to determine the adequacy of the location before initiating administration of an NMBD. In an emergent situation, testing the TOF response before the administration of an NMBD may not be possible.  Rationale: Testing improves the reliability of the interpretation of the TOF response.
Rationale: Testing improves the reliability of the interpretation of the TOF response.
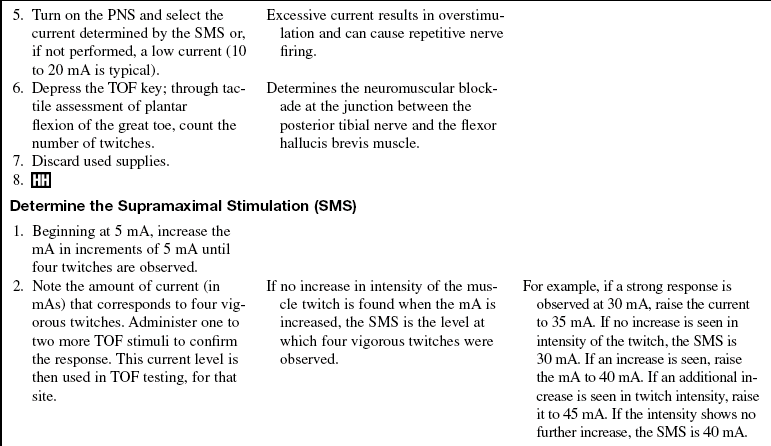
• Whenever possible, determine the supramaximal stimulation (SMS) level before initiating NMBDs. The SMS is the level at which additional stimulating current elicits no further increase in the intensity of the four twitches. In an emergent situation, determination of the SMS level before the administration of an NMBD may not be possible.  Rationale: This determination helps establish adequate stimulating current and improves reliability of testing.
Rationale: This determination helps establish adequate stimulating current and improves reliability of testing.
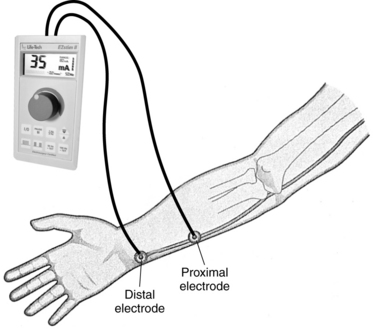
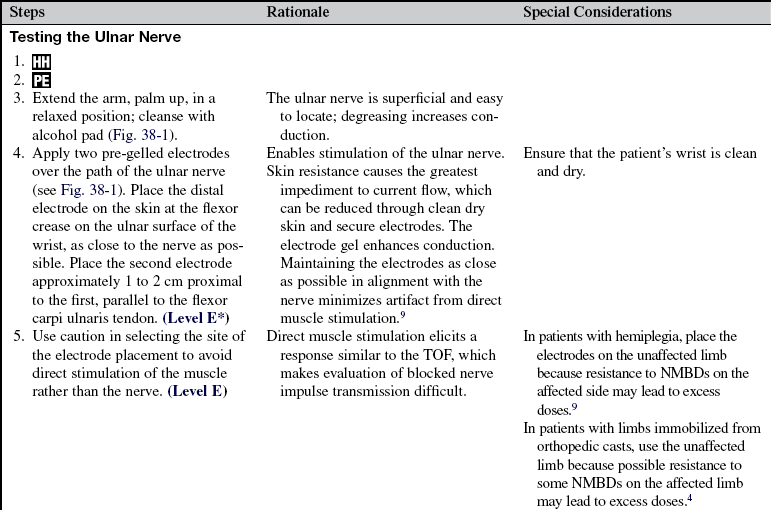
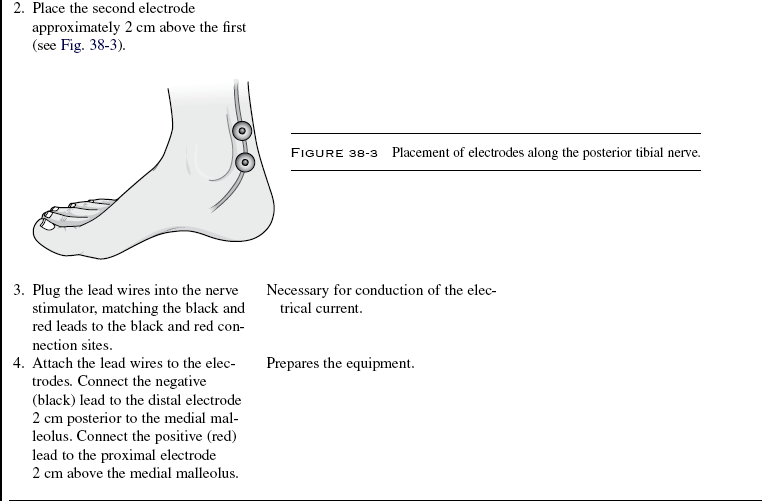
FIGURE 38-1 Placement of electrodes along the ulnar nerve.
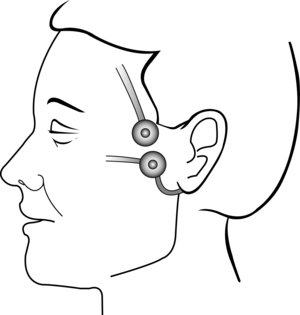
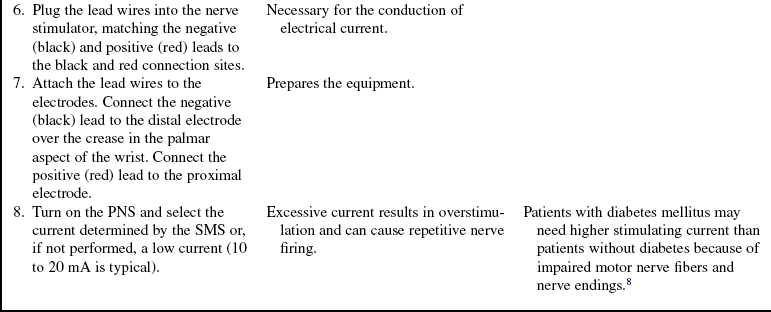
FIGURE 38-2 Placement of electrodes along the facial nerve.
References
1. De Laet I, Hoste, E, Verholen, E, et al, The effect of neuromuscular blockers in patients with intra-abdominal hypertension. Intensive Care Med. 2007; 33(10):1811–1814 [Epub June 27, 2007].
2. Foster, J, Clark, AP. Functional recovery after neuromuscular blockade in mechanically ventilated critically ill -patients. Heart Lung. 2006; 35(3):178–189.
![]() 3. Jacobi, J, et al. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med. 2002; 30:119–140.
3. Jacobi, J, et al. Clinical practice guidelines for the sustained use of sedatives and analgesics in the critically ill adult. Crit Care Med. 2002; 30:119–140.
![]() 4. Kim, KS, et al. The duration of immobilization causes the changing pharmacodynamics of mivacurium and rocuronium in rabbits. Anesth Analg. 2003; 96:438–442.
4. Kim, KS, et al. The duration of immobilization causes the changing pharmacodynamics of mivacurium and rocuronium in rabbits. Anesth Analg. 2003; 96:438–442.
![]() 5. Murray, M, et al. Clinical guidelines for sustained neuromuscular blockade in the adult critically ill patient. Crit Care Med. 2002; 30:142–156.
5. Murray, M, et al. Clinical guidelines for sustained neuromuscular blockade in the adult critically ill patient. Crit Care Med. 2002; 30:142–156.
6. Murray, MJ, Brull, SJ, Bolton, CF, Brief review. nondepolarizing neuromuscular blocking drugs and critical -illness myopathy. Can J Anaesth. 2006; 53(11):1148–1156.
![]() 7. Nagelhout, JJ, Naglaniczny, KL. Nurse anesthesia, ed 3. Philadelphia: Saunders; 2004.
7. Nagelhout, JJ, Naglaniczny, KL. Nurse anesthesia, ed 3. Philadelphia: Saunders; 2004.
![]() 8. Saitoh, Y, et al. Monitoring of neuromuscular block after administration of vecuronium in patients with diabetes mellitus. Br J Anaesth. 2003; 90:480–486.
8. Saitoh, Y, et al. Monitoring of neuromuscular block after administration of vecuronium in patients with diabetes mellitus. Br J Anaesth. 2003; 90:480–486.
9. Thompson, C, Monitoring the neuromuscular junction. www.usyd.edu.au/su/anaes/lectures/nmj_monitoring_clt/nmjonitoring.html, August 5, 2008 [retrieved, from].
10. Viamed, Operator’s Manual Microstim. www.viamed.co.uk/products/microstim/microstim.htm, August 4, 2008 [retrieved, from].