CHAPTER 38. Gynecological and Reproductive Care
Laura Krieger
OBJECTIVES
After completion of this chapter, the reader will be able to:
1. Describe the anatomical and physiological aspects of the female reproductive organs and structures as they pertain to patients undergoing gynecological and reproductive diagnostic or operative procedures.
2. Identify assessment parameters for patients undergoing gynecological and reproductive operative or diagnostic procedures.
3. Define nursing priorities, concerns, and complications in each operative phase.
4. Define nursing care assessments, nursing diagnoses, nursing interventions, and expected patient outcomes.
5. List pertinent patient education and health maintenance tools.
I. OVERVIEW
A. Patients undergo gynecological operative or diagnostic procedures for:
1. Acute or chronic reasons
2. Elective or emergent reasons
B. Surgical interventions required for a variety of indications ranging from:
1. Simple diagnostic procedures
2. Radical excisions for malignancy
C. Nursing intervention strategies are discussed as they relate to specific diagnostic or operative situations.
II. ANATOMY AND PHYSIOLOGY
A. External genitalia (Figure 38-1)
1. Collectively called the vulva
2. Mons pubis
a. Mound of adipose tissue overlying symphysis pubis
b. Covered with pubic hair in the adult
3. Labia majora
a. Outer vulval lips
(1) Two rounded folds of adipose tissue
(2) Extend from the mons pubis to the perineum
(3) Covered with hair
(4) Protect perineum
(5) Contain large sebaceous glands that maintain lubrication
4. Labia minora
a. Inner vulval lips
b. Anterolateral medial parts
(1) Join to form prepuce and frenulum
(2) Folds of skin that cap the clitoris
c. Posterior union called the fourchette
5. Clitoris
a. Small, protuberant organ located beneath the arch of mons pubis
b. Composed of:
(1) Erectile tissue
(2) Venous cavernous spaces
(3) Specialized sensory corpuscles that are stimulated during coitus
c. Urethral opening is a slit below the clitoris.
d. Homologous to the male penis
6. Vestibule
a. Oval space bordered by:
(1) Clitoris
(2) Labia minora
(3) Fourchette
(a) Posterior junction of labia majora and labia minora
(b) Glands lubricate vestibule.
(4) Skene’s glands
(a) Open on both sides of urethral meatus
(b) Contain 6 to 31 ducts
(c) Known as paraurethral glands
(d) Becomes infected usually from organisms that cause sexually transmitted infections (STIs)
(5) Bartholin glands
(a) Open on both sides of vaginal meatus
(b) Can be palpated when enlarged
(c) Can become infected usually from organisms that cause STIs
b. Hymen: thin membrane partially covering vaginal orifice
c. Perineum
(1) Anteriorly bordered by top of labial fold
(2) Posteriorly bordered by anus
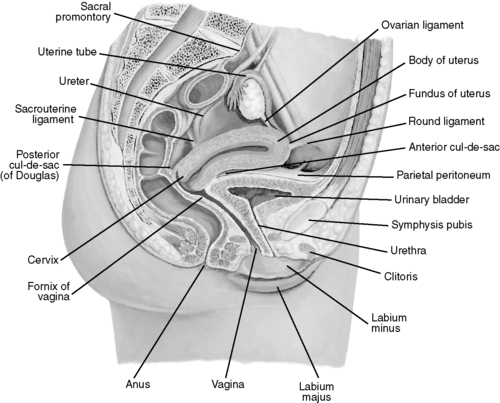 |
| FIGURE 38-1 ▪
Midsagittal section of the female pelvis.
(From Thibodeau GA, Patton KT: Anatomy & physiology, ed 6, St Louis, 2007, Mosby.)
|
B. Internal structures (Figure 38-2)
1. Vagina
a. Occupies space between bladder and rectum
b. Connects uterus with vestibule
c. Lined with mucous membranes
d. Conduit for menstrual fluid discharge
e. Birth canal
2. Cervix
a. Narrow neck of uterus
b. Provides passageway between:
(1) Uterine cavity
(2) Vagina
3. Uterus
a. Hollow, pear-shaped muscular organ
b. Conceptus grows during pregnancy.
c. Uterine wall consists of:
(1) Inner mucosal lining (endometrium)
(a) Undergoes cyclic changes based on hormonal activity
(b) Facilitates and maintains pregnancy
(2) Middle muscular lining (myometrium)
(a) Interlaces uterine and ovarian arteries and veins
(b) During pregnancy, vasculature expands dramatically.
(3) Outer serous layer (parietal peritoneum)
(a) Covers:
(i) All of the fundus
(ii) Part of the corpus
(iii) Not the cervix
d. Divided into fundus and cervix, which protrudes into vagina
e. Lining sheds (menstruation) in monthly cycle in the absence of:
(1) Fertilization
(2) Implantation of embryo
4. Fallopian tubes (uterine tubes)
a. Extend from sides of fundus
b. Terminate near ovaries
c. Carry ova to uterus
d. Facilitate movement of sperm toward ovaries
e. Move zygote (fertilized ovum) to uterus
5. Ovaries
a. Two almond-shaped organs
b. Attached to posterior surface of broad ligament
c. Produce:
(1) Ova
(2) Estrogen
(3) Progesterone
(4) Small amounts of androgen
d. Fully developed after puberty
e. Shrink after menopause
6. Ligaments of uterus
a. Wide fold of periosteum that holds the uterus in place
b. Eight in number
(1) Two cardinal ligaments
(a) Fibrous sheets that extend to lateral pelvic wall from:
(i) Cervix
(ii) Vagina
(b) Help prevent prolapse of uterus
(2) Two lateral or broad ligaments
(a) Attach uterus to either side of pelvic cavity
(b) Divide cavity into two portions
(i) Anterior part—bladder
(ii) Posterior part—rectum
(c) Keep uterus in position
(3) Two uterosacral ligaments
(a) Lie on either side of rectum
(b) Connect uterus to sacrum
(4) Two round ligaments
(a) Flattened bands between 10 and 12 cm in length
(b) Situated between layers of the broad ligaments
(i) In front of uterine tubes
(ii) Below uterine tubes
7. Peritoneal folds of uterus
a. One anterior
(1) Vesicouterine fold of periosteum
(2) Reflected onto bladder from front of uterus
b. One posterior
(1) Rectovaginal fold of periosteum
(2) Reflected from back of posterior fornix of vagina to front of rectum
8. Vasculature
a. External genital blood supply
(1) Vulva
(a) Blood supply
(i) External pudendal arteries
(ii) Internal pudendal arteries
(b) Venous drainage
(i) Internal pudendal veins
b. Internal genital organs
(1) Vagina
(a) Blood supply
(i) Uterine arteries
(ii) Vaginal arteries
(iii) Internal pudendal arteries
(b) Venous drainage
(i) Vaginal venous plexus
(ii) Uterine venous plexus
(2) Uterus
(a) Blood supply
(i) Uterine arteries
(b) Venous drainage
(i) Uterine venous plexus into internal iliac vein
(3) Ovaries and fallopian (uterine) tubes
(a) Blood supply
(i) Ovarian arteries from abdominal aorta
(ii) Uterine arteries from internal iliac artery
(b) Venous drainage
(i) Right ovarian vein into inferior vena cava
(ii) Left ovarian vein into left renal vein
(iii) Tubal veins drain into:
[a] Ovarian veins
[b] Uterine venous plexus
9. Nerves
a. Superior hypogastric plexus
(1) Carries sympathetic fibers
(2) Responsible for innervation of:
(a) Fundus uteri
(b) Cervix
(c) Vagina
b. Inferior hypogastric plexus
(1) Three portions representing viscera innervation
(a) Vesical plexus
(i) Bladder
(ii) Urethra
(b) Hemorrhoidal plexus
(i) Rectum
(c) Ureterovaginal plexus
(i) Uterus
(ii) Vagina
(iii) Clitoris
(iv) Vestibular bulbs
c. Iliohypogastric
(1) Innervates skin near iliac crest just above symphysis pubis
d. Ilioinguinal
(1) Sensory innervation
(a) Upper medial thigh
(b) Mons
(c) Labia majora
e. Genitofemoral
(1) Sensory innervation
(a) Anterior vulva
(b) Middle and upper anterior thigh
f. Posterior femoral cutaneous
(1) Sensory innervation
(a) Vulva
(b) Perineum
g. Pudendal
(1) Sensory innervation
(a) Perianal skin
(b) Vulva
(c) Perineum
(d) Clitoris
(e) Urethra
(f) Vaginal vestibule
(2) Motor innervation
(a) External anal sphincter
(b) Perineal muscles
(c) Urogenital diaphragm
10. Associated structures
a. Genitourinary
(1) Bladder
(2) Ureters
(3) Urethra
b. Sigmoid colon and rectum
c. Pelvic floor muscles
d. Lymph nodes
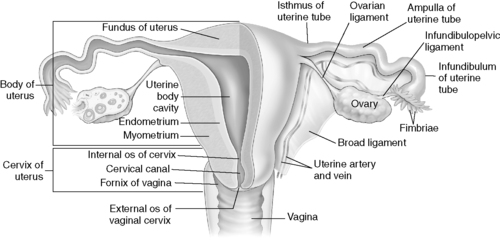 |
| FIGURE 38-2 ▪
Uterus and uterine tubes.
(From Thibodeau GA, Patton KT: Anatomy & physiology, ed 6, St Louis, 2007, Mosby.)
|
III. PATHOPHYSIOLOGY
A. Congenital or anatomical abnormalities
1. Imperforate hymen
a. Completely closed hymen
2. Herniations
a. Abnormal bulging/pouching of organs/tissues
b. Cystocele
(1) Herniation of bladder
(2) Causes anterior vaginal wall to bulge downward
c. Rectocele
(1) Formed by protrusion of anterior rectal wall (posterior vaginal wall) into vagina
d. Enterocele
(1) Herniation of cud-de-sac of Douglas
(2) Contains loops of small intestine
e. Urethrocele
(1) Pouch-like protrusion of urethral wall
(2) Thickening of connective tissue around urethra
3. Uterine displacement
a. Abnormal position or shape of uterus
b. Prolapsed uterus
(1) Collapsed uterus into vaginal opening
4. Bicornuate uterus
a. Usually two separate “horns” that form the top of uterus
5. Septate uterus
a. Uterine cavity divided by a wall (septum)
b. Septum may extend only part of the way.
c. Septum may extend as far as the cervix.
6. Tubal incompetency: a blockage of one or both fallopian tubes
a. Complete
b. Partial
B. Endocrine (hormonal) dysfunction
1. Abundant, low, or no secretions of necessary reproductive hormones
2. Endometriosis (growth of endometrial tissue outside the endometrium)
3. Dysfunctional uterine bleeding
4. Stein-Leventhal syndrome (polycystic ovary syndrome)
C. Growths and neoplasms
1. Cysts (closed sack or pouch with definite walls that contains fluid, semifluid, or solid material)
a. Bartholin
b. Ovarian
2. Uterine fibroids, myomatas, or leiomyomas—tumors containing muscle tissues
3. Carcinomas (malignant tumor growth in epithelial tissue)
a. Vulvar
b. Cervical
c. Uterine
d. Ovarian
4. Polyps (benign tumors with pediclea). Removed if possibility that it will become malignant
a. Prone to bleeding (hemorrhage)
b. Cervical
c. Uterine
5. Condylomata (wartlike growths of the skin)
a. External genitalia
b. Anal region
D. Infections and inflammatory processes
1. Pelvic inflammatory disease (PID)
a. Affects abdominal organs
b. May result in infertility
2. Abscesses (encapsulated infective material)
a. Perineal region
b. Abdominal organs
3. Fistulas (abnormal connection or passageway between two epithelium-lined organs)
a. Urethrovaginal
b. Rectovaginal
E. Pregnancy related (see Chapter 39)
1. Abortion
a. Incomplete
(1) Abortion in which parts of products of conception have been retained in uterus
b. Missed
(1) Abortion in which fetus has died before twentieth completed week of gestation
(2) Products of conception retained in uterus for 8 weeks or longer
c. Therapeutic
(1) Abortion performed when mental or physical health of mother is endangered by continuation of pregnancy
2. Incompetent cervix
3. Ectopic pregnancy (pregnancy occurring outside uterine cavity)
a. Commonly occurs in fallopian tube
b. Life-threatening if ruptured
(1) Hemorrhage
(2) Loss of fallopian tube and/or ovary
4. Hydatidiform mole—degenerative process in chorionic villi that gives rise to:
a. Multiple cysts
b. Rapid growth of uterus
c. Possible hemorrhage
d. Surgical removal by laparotomy
IV. DIAGNOSTIC/PREOPERATIVE EVALUATION
A. Physical examination of external genitalia
1. Pelvic
a. Inspection of external genitalia and pubic hair to assess sexual maturity
2. Labia
a. Gently spread the labia majora and minora and inspect area.
b. Area should be free from moisture and free from lesions.
c. May detect a normal discharge that should be:
(1) Odorless
(2) Nonirritating to the mucosa
3. Vestibule
a. Inspect the area around Bartholin’s and Skene’s glands.
b. Check for:
(1) Swelling
(2) Redness
(3) Lesions
(4) Discharge
(5) Unusual odor
c. Inspect the vaginal opening, noting whether hymen:
(1) Intact
(2) Perforated
4. External genitalia
a. Spread labia with one hand and palpate with the other.
b. Labia should feel soft.
c. Note swelling, hardness, or tenderness.
d. If mass or lesion detected:
(1) Palpate it to determine its size, shape, and consistency.
B. Physical examination of internal genitalia
1. Speculum examination of vagina and cervix
2. Obtain a specimen for a Papanicolaou’s test (Pap smear).
a. Detection and diagnosis of malignant and premalignant conditions
(1) Vagina
(2) Cervix
(3) Endometrium
b. Obtain wet preparation.
(1) Yeast infection
(2) Bacterial infection
(3) Trichomonas
c. Cultures for STIs
(1) Gonorrhea
(2) Chlamydia
3. Palpating the internal genitalia
a. Note tenderness or nodularity in vaginal wall.
b. Bulging of vaginal walls during “bearing down” may indicate:
(1) Cystocele
(2) Rectocele
4. Bimanual palpation of uterus and ovaries
a. Performed by advanced practitioners
b. Allows evaluation of:
(1) Rectovaginal area
(2) Posterior part of uterus and pelvic cavity
(3) Rectum
(4) Feel the edges of the cervix and lower posterior wall of the uterus.
C. Subjective data
1. Characteristics (Box 38-1)
a. Menstrual history
b. Onset of menses
c. Length of cycles
d. Regularity of cycles
e. Duration, amount, and content of flow
f. Date of last menstrual cycle
g. Contraceptive use or absence
BOX 38-1
DEFINITIONS
Gravidity: pregnancies, full-term deliveries, preterm deliveries
Menarche: beginning of menstrual function
Amenorrhea: absence or abnormal stoppage of menses
Oligomenorrhea: infrequent menstrual flow occurring at intervals of 35 to 180 days
Menorrhagia: hypermenorrhea
Menometrorrhagia: excessive uterine bleeding occurring both during menses and at irregular intervals
Terminations: spontaneous, elective
2. Sexual activity, sexual partners
3. Virilizing features
a. Hair growth
b. Irregular or absent periods
4. Emotional status
a. Evaluation of adequacies or deficiencies
5. Psychosocial
a. Maintain sympathetic and understanding approach.
6. Special situations
a. Infertility
(1) May be associated with:
(a) Specific psychological problems
(b) Stress
(c) Anxiety
(d) Compulsive-obsessive neurosis
b. Loss of desired pregnancy
c. Surgically induced hormonal changes
d. Concerns or fears for invasion of privacy
e. History of sexual abuse and violence
D. Additional assessment factors
1. Laboratory data
a. Hematology values
(1) Complete blood cell count
(2) Type and screen
b. Chemistry values
(1) Serum electrolytes
(2) Glucose
(3) Beta human chorionic gonadotropin (hCG; pregnancy hormone)
c. Urinalysis
(1) Bacteria
(2) Glucose
(3) Protein
(4) Ketones
(5) Red blood cells
(6) hCG
d. Cytological studies
(1) Pap smear
(2) Previous cryotherapy
(3) Biopsy reports
2. Radiological studies
3. Ultrasonography
4. Electrocardiography
5. Physical limitations
a. May result in alteration of:
(1) Anesthesia techniques/performance
(2) Patient positioning
(3) Immediate- and long-term recovery time and healing
b. Arthritis
c. Musculoskeletal disorders
d. Implanted joints
e. Autoimmune diseases
f. Obesity (obese = body mass index [BMI] of 30, morbid obesity = BMI >40)
6. Allergies to dyes
E. Risk factor assessment
1. Deep vein thrombosis or other embolisms
2. Obesity; level of obesity
3. Tobacco
4. Pregnancy
5. Chronic or acute pain
6. Pain tolerance alterations
7. Chronic analgesic use
8. Developmentally challenged
a. Potential behavioral problems
b. Legal authorization appropriately obtained before treatment
c. Determination of individual learning capability and education needs of patient and caregiver
F. Pain assessment
G. Outcome on sexual activity/fertility
H. Discharge planning
1. Outpatient versus inpatient
2. Address:
a. Clothing
b. Equipment
c. Supplies
d. Medications
e. Caregiver
f. Miscellaneous
V. OPERATIVE PROCEDURES
A. External
1. Hymenectomy
a. Purpose: to enlarge the vaginal orifice
b. Description: surgical excision of hymen membrane
2. Hymenotomy
a. Purpose: to open the vaginal orifice; used to drain hematocolpos
b. Description: surgical incision of hymen membrane
3. Excision and drainage of Bartholin cysts
a. Purpose: surgical drainage of Bartholin gland for relief of pain and/or infection
b. Description: removal by cutting or systematic withdrawal of fluids or discharges with placement of Word catheter
4. Bartholinectomy: excision of Bartholin gland
a. Marsupialization of Bartholin cyst
b. Purpose: facilitates drainage and healing
c. Description: creation of open pouch around excised Bartholin gland and cyst
5. Excision external lesion
a. Purpose: removal of lesions
(1) Warts (condylomata)
(2) Papilloma
(3) Malignant growths
b. Description: lesions removed by cutting
(1) Laser therapy (carbon dioxide [CO 2], neodymium:yttrium-aluminum-garnet [Nd:YAG], argon)
(2) Electrocautery methods
6. Vulvectomy
a. Purpose: treatment for premalignant or malignant lesions of the vulva
b. Description—excision of:
(1) Labia majora
(2) Labia minora
(3) Surrounding structures
(4) Requires skin graft
7. Postanesthesia priorities
a. Perineal care
b. Sitz baths may be ordered.
c. Pain management
B. Transvaginal
1. Cervical conization and colposcopy
a. Purpose: diagnosis or treatment of cervical infection or carcinoma in situ
b. Description: removal of a cone of cervical tissue (partial excision)
2. Loop electrosurgical excision procedure (LEEP)
a. Purpose: allows entire specimen to be sectioned for diagnosis
b. Description: removes intact tissue
(1) Advantage over CO 2 laser for:
(a) Diagnostic excision
(b) Small biopsies
(c) Ablations of human papillomavirus–related lesions of anogenital tract
(2) Primarily used for cervical lesions, but may also be used for:
(a) External warts
(b) Flat lesions
(i) Vaginal
(ii) Vulvar
(iii) Anal
3. Laser therapy (CO 2, Nd:YAG, argon)
a. Cervical cancer in situ
4. Dilatation and curettage
a. Purpose: removal of growths and other materials from uterine cavity
b. Description
(1) Stretching the cervix beyond normal dimensions
(2) Removal of contents from walls of uterine cavity with a curet (spoon-shaped, sharp-edged instrument)
c. Often performed in conjunction with hysteroscopy
5. Dilatation and evacuation
a. Purpose: uterine aspiration and emptying
b. Description: stretching the cervix beyond normal dimensions and removing contents of the uterus by curettage, suction
6. Endometrial ablation and resection
a. Purpose: treatment of dysfunctional uterine bleeding
b. Description
(1) Nd:YAG laser with a hysteroscope
(2) Roller ball
(3) Loop electrode with a modified resectoscope
7. Fertility procedures
a. Cerclage
(1) Purpose: preservation of uterine contents
(2) Description: encircling an incompetent cervix uteri with a ring or loop (or a stitch into the cervix)
b. In vitro fertilization (IVF)
(1) Purpose: pregnancy
(2) Description—using transvaginal ultrasound-guided follicle aspiration:
(a) Healthy, mature oocytes retrieved
(b) Oocytes and sperm mixed
(c) Resultant embryo transferred to uterine fundus after 2 days
c. Transcervical balloon tuboplasty
(1) Purpose: open obstructed fallopian tubes
(2) Description: performed under fluoroscopy, sonography, hysteroscopy
(a) A catheter is passed through the cervix.
(b) After injection of dye to detect obstruction, the balloon attached to the catheter is inflated inside the fallopian tube.
(c) Interior of fallopian tube is dilated until recanalization is achieved.
8. Tension-free vaginal tape (TVT)
a. Purpose: correction of stress incontinence
b. Description: placement of a synthetic mesh tape under midurethra
(1) Local anesthesia most commonly used
(2) General or regional anesthesia used if additional procedures needed
c. Preanesthesia assessment and concerns
(1) Patient taught self-catheterization
(2) May need to self-catheterize postoperatively
d. Postanesthesia priorities
(1) Phase II—standard voiding trial before discharge
(a) May be discharged with indwelling (e.g., Foley) catheter in place
(b) Patient education: catheter care and removal
e. Complications
(1) Bladder perforation
(2) Hematoma
(3) Postoperative voiding dysfunction
(a) Incomplete bladder emptying
(b) Persistent urgency and urge incontinence
(4) Urinary tract infection
9. Vaginal hysterectomy
a. Purpose: removal of uterus
b. Description: excision of uterus through vagina
c. Postanesthesia priorities
(1) May require 23-hour stay (extended recovery) after procedure
10. Anterior colporrhaphy
a. Purpose: tightens vaginal wall; prevents or corrects bladder herniation into vagina
b. Description: removal of excess anterior vaginal tissue
11. Posterior colporrhaphy
a. Purpose: tightens vaginal wall; prevents or corrects rectal herniation into vagina
b. Description: removal of excess posterior vaginal tissue
12. Culdoscopy: direct visualization of uterus and adnexa through endoscope passed through posterior vaginal wall
13. Culdocentesis
a. Purpose: used to detect intraperitoneal bleeding or cul-de-sac hematoma
b. Description: aspiration through vaginal wall of blood or pus from cul-de-sac
c. Good diagnostic tool to rule out ruptured ectopic pregnancy
C. Endoscopic procedures—laparoscopy
1. Laparoscopy
a. Purpose: diagnostic or therapeutic procedures may be performed.
(1) Biopsies
(2) Lysis of adhesions
(3) Sterilization
(4) Treatment of endometriosis
(5) Nerve ablative procedures
(6) Hysterectomy
(7) Myomectomy
(8) Cystectomy
(9) Pelvic reconstructive procedures
b. Description: examination of interior of abdomen (abdominal and pelvic organs) by means of a lighted endoscope (laparoscope) through small incision(s) in the abdominal wall
(1) Pneumoperitoneum created using CO 2 to enhance visualization by lifting the abdominal wall
2. Tubal ligation
a. Purpose: obliteration of fallopian tubes to cause infertility (sterilization)
b. Description
(1) Rings
(2) Clips
(3) Ligation (ties)
(4) Cauterization
3. Tubal lavage (chromopertubation)
a. Purpose: ascertains fallopian tube patency
b. Description: dye injected through fallopian tubes
(1) Spillage of dye indicates patent tubes.
4. Fertility procedures
a. Gamete intrafallopian transfer (GIFT)
(1) Purpose: pregnancy
(2) Description: follicle stimulation and oocyte retrieval same as for IVF
(a) Gametes (oocytes and sperm) replaced through the distal fallopian tube
(b) Via laparoscopically or sonographically guided tubal cannulation
b. Zygote intrafallopian transfer) (ZIFT—also known as tubal embryo transfer (TET)
(1) Purpose: pregnancy
(2) Description: follicle stimulation and oocyte retrieval same as for IVF
(a) Zygote replaced through the distal fallopian tube
(b) Via laparoscopically or sonographically guided tubal cannulation
5. Laparoscopic-assisted vaginal hysterectomy (LAVH)
a. Purpose
(1) Removal of uterus for myomata
(2) Abnormal uterine bleeding
(3) Adenomyosis
(4) Malignancy
(5) Pelvic pain
(6) Endometriosis
b. Description: hysterectomy begun by laparoscopy and completed vaginally.
6. Myomectomy
a. Purpose: surgical removal of a myoma (leiomyoma, “fibroids”) to preserve uterine integrity and fertility
b. Description: accomplished by laparoscopic or hysteroscopic technique
7. Oophorectomy: removal of an ovary or ovaries
8. Ovarian cystectomy: excision of ovarian cyst, leaving functioning ovary
9. Salpingectomy: removal of fallopian tube
10. Neosalpingostomy: surgical restoration of patency of fallopian tube
11. Salpingoplasty (tuboplasty)
a. Purpose: restore patency of fallopian tube
b. Description: microscopic reconstructive surgery of fallopian tube
(1) Obstructed portion of fallopian tube may be removed.
(2) Tube reconstructed to create patency to promote fertilization
(3) Reversal of tubal ligation
(4) PID surgery
(a) Treat tubo-ovarian abscess—drain or remove an abscess
(b) Treat adhesions—incise scar tissue that cause pain
(c) Diagnose problem when
(i) Other tests not done
(ii) Antibiotic treatment not working
(5) Adhesions
12. Intraoperative concerns
a. Considerations unique to laparoscopic procedures
(1) Pulmonary and cardiovascular changes
(a) Pneumoperitoneum creates increased intra-abdominal pressures.
(b) Pulmonary inspiratory pressure increases.
(c) Compliance decreases.
(d) Atelectasis develops.
(e) Functional residual capacity decreases.
(2) CO 2 absorption from peritoneal cavity into blood can cause:
(a) Hypercarbia
(b) Respiratory acidosis
(3) Trendelenburg positioning can lead to increased:
(a) Mean arterial pressure
(b) Pulmonary artery pressure
(c) Aortic compression
(d) Systemic vascular resistance
(e) Parameters accompanied by a drop in cardiac output
(4) Marked hemodynamic changes may be brought about during the procedure by a significant release of:
(a) Catecholamines
(b) Prostaglandins
(c) Vasopressin
(5) Stretching of peritoneum and manipulation of viscera can lead to bradycardia, which responds to atropine.
(6) Pulmonary aspiration is a risk with abdominal insufflation.
13. Postanesthesia priorities—phase I
a. Pain
(1) Shoulder pain common after laparoscopy
(a) Referred pain caused by diaphragmatic irritation from residual CO 2 in abdomen
(2) Peritoneal surface inflammation after laparoscopy may:
(a) Be caused by the formation of carbonic acid (reaction between CO 2 and intraperitoneal fluid)
(b) Persist for 2 to 3 days postoperatively.
(3) Nonsteroidal anti-inflammatory drugs (NSAIDs) effective in managing postlaparoscopic pain
D. Endoscopic procedures
1. Hysteroscopy
a. Purpose
(1) Examine the endometrium.
(2) Secure specimens for biopsy.
(3) Remove foreign bodies (e.g., intrauterine device).
(4) Remove polyps.
(5) Remove intrauterine adhesions or submucous fibroids.
(6) Ablation
(7) Diagnose uterine abnormalities.
b. Description: inspection of interior of uterus with an endoscope, using either a liquid or a gaseous distending medium
c. Intraoperative concerns
(1) Considerations unique to hysteroscopic procedures
(a) Fluid (saline, glycine, dextran) used as distending media
(b) Absorption and resultant circulatory overload
(c) Dilution can lead to:
(i) Hyponatremia
(ii) Hypoproteinemia
(iii) Transurethral resection syndrome (glycine absorption)
(d) Disseminated intravascular coagulation (dextran)
(e) Anaphylaxis (dextran)
(2) CO 2 used as distending medium
(a) Abdominal distention from leak via fallopian tubes
(b) CO 2 absorption leading to acidosis, dysrhythmias
(c) CO 2 embolism
(3) Uterine perforation
(4) Vaginal bleeding
(5) Careful attention should be paid to:
(a) Amount of fluid instilled and removed
(b) Excessive administration can lead to the preceding complications.
d. Complications
(1) Fluid overload
(a) May be result of significant absorption of irrigant through tissue and blood vessels
(b) May lead to:
(i) Pulmonary edema
(ii) Hyponatremia
(iii) Cerebral edema and subsequent seizures
(iv) Respiratory arrest
(v) Coma
(vi) Death
(2) Treatment of fluid overload
(a) Monitor respiratory status.
(b) Check serum electrolyte levels.
(c) Diuretics and intravenous (IV) fluid restriction may be needed.
E. Laparotomy (vertical, transverse)
1. Laparotomy
a. Purpose: allows for exploration of abdominal cavity
b. Description—incision of abdominal wall; incision may be:
(1) Vertical
(2) Transverse
2. Abdominal suspension procedures for stress urinary incontinence
a. Purpose: surgical treatment for relief of stress incontinence
b. Description
(1) Marshall-Marchetti-Krantz (MMK)
(2) Burch procedure
(a) Preferred
(b) Paravaginal fascia on each side of urethra, near bladder neck, sutured to the ligaments (Cooper’s) attached to the pubic bone
(c) May be performed:
(i) With a low transverse incision
(ii) Laparoscopically
3. Metroplasty
a. Purpose: repair of septate uterus
b. Description: reconstructive surgery on the uterus
4. Hysterectomy
a. Purpose: excision of uterus
b. Description: surgical approaches
(1) Vaginally
(2) Laparoscopic-assisted vaginal hysterectomy
(3) Abdominally
5. Hysterosalpingo-oophorectomy: removal of uterus, fallopian tubes, and ovaries
6. Radical hysterectomy and lymph node dissection
a. Purpose: to remove uterus for cervical cancer, preserving the ovaries
b. Description—laparotomy to remove:
(1) Uterus
(2) Tubes
(3) Upper vagina
(4) Supporting ligaments
(5) Pelvic lymph nodes
(6) Extensive dissection of ureters and bladder
c. Portions of this procedure may be performed by laparoscopy (e.g., pelvic lymph node dissection).
7. Radical vulvectomy
a. Purpose: to treat invasive vulvar carcinoma
b. Description: en bloc dissection of inguinal-femoral region and vulva
(1) Skin or myocutaneous graft may be needed for closure of wound.
8. Pelvic exenteration
a. Purpose: curative; to remove all cancer tissue and reconstruction of diversions for urine and possibly colon
b. Description—pelvic tissues, including:
(1) Uterus
(2) Cervix
(3) Vagina
(4) Bladder
(5) Rectum
c. Preanesthesia assessment and concerns
(1) Full and thorough mechanical and antibiotic bowel preparation
(2) Deep vein thrombosis prophylaxis initiated
d. Postanesthesia priorities—phase I
(1) Drain and stoma care
(2) Potential for significant fluid loss and third spacing
(3) Pain management
(4) Psychosocial concerns
(a) Prepare for altered body image.
(b) Issues associated with cancer diagnosis and prognosis
e. Complications
(1) Fluid overload
(2) Bleeding
(3) Coagulopathy
(4) Trauma to kidneys
VI. NURSING PRIORITIES
A. Anesthesia choice
1. Depends on operative procedure, patient’s needs and physical habitus
2. Airway used
a. Endotracheal tube
b. Laryngeal mask airway
c. Mask
3. Use of total IV techniques (propofol and an opioid analgesic)
a. Can reduce the incidence of postoperative nausea and vomiting (PONV)
4. Regional; spinal or epidural
5. Monitored anesthesia care
6. Sedation and analgesia with local anesthesia
7. Local anesthesia used alone for minor or office procedures
a. Paracervical block
b. Pudendal block
B. Intraoperative concerns
1. Lithotomy position
a. Elevate and lower legs together to avoid strain of back and leg muscles.
b. Avoid any abnormal movement of the knee or pressure on the knee.
c. Avoid extreme flexion of hips or popliteal pressure.
d. Pad lumbar region to prevent pressure.
e. After positioning, assess neuromuscular status and reposition if compromised.
2. Arms and hands are safely positioned and shoulders are padded during Trendelenburg position.
3. Fingers need protection from impingement, especially when positioning and at end of procedure when repositioning for transfer.
4. Maintain patient’s dignity.
5. Skin integrity (Braden Scale) can be compromised if iodine-based preparation solutions are allowed to pool under the patient; can lead to burns of the skin.
C. Procedural techniques
1. Special cautions and care required with each technique
2. Refer to equipment training and maintenance literature for specific information on precautions, hazards, and safe use of equipment in operating room environment.
3. Microsurgical
4. Endoscopic
a. Laparoscope
(1) Usually use CO 2 gas as insufflating medium for creation of pneumoperitoneum
(2) Gasless: uses a mechanical lift method
b. Hysteroscope
(1) Rigid scope most commonly used
(2) Flexible scopes available, not widely used
5. Laser, cautery, cryotherapy
6. Transvaginal ultrasonography
7. Transvaginal fluoroscopy: used infrequently because of risk of radiation exposure to reproductive organs
D. Intraoperative complications
1. Gas embolism
2. Fluid overload, dilutional hyponatremia
3. Hemorrhage
4. Perforation of hollow organs or vessels
5. Thermal injuries
6. Aspiration
7. Perioperative neuropathy
VII. POSTANESTHESIA PRIORITIES
A. Phase I priorities (Box 38-2)
1. Airway
a. Spontaneous, unassisted breathing
b. Adjunct or endotracheal tube in place
c. Observe for respiratory complications.
(1) Risk for pulmonary edema after hysteroscopy if excessive irrigant or distending media used
(2) If intubated, assess location of tube by auscultating chest (dislocation of tube can occur from pneumoperitoneum).
2. Hemodynamic stability
a. Vital signs stable, consistent with baseline
b. Observe for cardiovascular complications.
3. Bleeding
a. Vaginal
(1) Cervical
(2) Uterine
(a) Assess uterine firmness after dilatation and evacuation.
(i) Oxytocin (Pitocin) may be needed in advanced pregnancy termination to control bleeding.
(b) Methylergonovine (Methergine) for prevention and treatment of postpartum and postabortion hemorrhage
(c) Rh factor identified for Rh-negative patients to receive Rh immune globulin injection
(d) Observe for passage of clots.
b. Incisional
(1) Oozing or frank bleeding
(2) Hematoma beneath incision
c. Internal
(1) Perforation of organ or vessel
(2) Operative hemostasis not achieved or oozing
4. Report from anesthesia, surgeon, perioperative nurse
a. Positioning of patient intraoperatively
b. Estimated blood loss
c. Complications
(1) Perforation
(2) Burn
(3) Excessive fluid administration
5. Discomfort
a. Incisional
b. Cramping
c. Significant pain after procedure—suspect:
(1) Perforation
(2) Hematoma formation
(3) Intra-abdominal trauma
d. Cervical and intrauterine manipulation may result in prostaglandin release.
(1) Can result in continued postoperative pain
6. Dressing and drains
a. Abdominal incisions
(1) Adhesive bandages or no dressing over trocar insertion sites after laparoscopic procedures
(2) Gauze and tape dressing over longer incisions
b. Perineal pad in place after cervical, uterine procedures
(1) Assess on arrival and regularly for type and amount of bleeding.
(2) Notify surgeon of bleeding—saturating more than a pad an hour.
c. Vaginal packing: removable, absorbable, hemostatic material
(1) Observe minimal perineal bleeding.
(2) Patient may have urge to defecate from pressure of packing.
d. Drains
(1) Bartholin cyst incision and drainage or marsupialization
(2) Vaginal drains include T-tube, Malecot.
(3) Grenade (Jackson-Pratt)
(4) Maintain patency of drains.
7. Edema
a. May observe subcutaneous edema from laparoscopic CO 2 insufflation
b. External vulvar lesions—swelling may be reduced with application of:
(1) Ice
(2) Cold therapy
8. Fluids and nutrition
a. Do not force fluids, especially when nausea and vomiting present.
b. Causes of nausea and vomiting (see Chapter 25)
(1) Opioid analgesics
(2) Neuromuscular reversal (neostigmine and pyridostigmine have been associated with increased PONV)
(3) Pain also major cause of nausea after gynecological surgery
(4) Starvation leading to weakness, low blood sugar levels
(5) Controversy exists regarding effect of menstrual cycle and timing of operative procedure on PONV.
c. Hydrate with IV fluids (replacement and maintenance).
(1) Usual lactated Ringer’s (Hartmann’s) or dextrose-containing solutions
(2) Long laparoscopic procedures with dry insufflating gases may increase patient’s fluid replacement needs.
d. When nausea or vomiting are present:
(1) Administer antiemetics as ordered; determine whether antiemetic prophylaxis given.
(2) Commonly use:
(a) Promethazine
(b) 5-Hydroxytryptamine (serotonin) type 3 (5-HT 3) receptor antagonists
(i) Ondansetron
(ii) Dolasetron
(iii) Kytril
9. Postlithotomy and postlaparoscopy neurovascular checks
a. Nerve damage secondary to:
(1) Positioning
(2) Retractor injuries
(3) Surgical transection
b. Pain, numbness, tingling of extremities, and loss of motor function in a given muscle group should be reported.
10. Urinary distention
a. Risk after gynecological procedures, which either results in edema surrounding the urethra or injury to urethra and related structures (e.g., vaginal hysterectomy)
b. Overdistention can cause temporary paralysis of the detrusor muscle, taking several days to resolve.
c. May require indwelling catheter or intermittent catheterization
11. Emotional support needed
a. Adolescents and young adults embarrassed
b. Pregnancy loss
c. Negative findings and outcomes
BOX 38-2
PATIENT EDUCATION AND HEALTH OUTCOMES
Phase I: Patient Will:
▪ Express feelings of lessened anxiety.
▪ Describe minimal to tolerable pain.
▪ Request analgesic to manage pain.
Phase II: Patient Will:
▪ Tolerate discomfort after administration of oral analgesics.
▪ Describe wound care after instruction.
▪ Progress to upright position with minimal orthostatic effects: dizziness, lightheadedness, nausea.
Extended Observation: Patient, Family, and Responsible Adult Accompanying Patient Will:
▪ Describe follow-up required.
▪ Identify risks associated with operative procedure: infection, hemorrhage, pain, vomiting.
▪ Describe wound observation, hand washing, how to change dressing and pads, how to cleanse wounds, and expected drainage.
▪ Describe at-home activity, restrictions, diet, and pain management.
▪ Demonstrate knowledge of medications (analgesics, antibiotics, antiemetics, etc.) by describing purpose and administration of each medication prescribed.
▪ Express understanding of necessity to report uncontrolled bleeding or pain.
B. Phase II priorities (see Box 38-2)
1. Determine nursing diagnoses.
2. Nursing interventions
a. Operative site
(1) Observe for bleeding, superficial hematoma formation around trocar insertion sites.
(2) Change or reinforce dressing as necessary.
(3) Monitor perineal pad drainage every hour and when patient ambulates first time.
(a) Note amount and type of drainage.
(b) Notify surgeon of:
(i) Significant bleeding
(ii) Passage of clots
(iii) Excessive cramping
b. Discomfort
(1) Gently palpate abdomen.
(a) Expect soft, slightly tender to touch, slightly distended.
(b) Notify surgeon of:
(i) Excessive tenderness
(ii) Firmness
(iii) Swelling
(iv) Suspected hematoma formation
c. Oral analgesic medications initiated in preparation for discharge home
(1) May have started in post anesthesia care unit phase I
(2) Combination of opioid medication and NSAIDs can provide effective analgesia after gynecological procedures.
(3) Determine effectiveness of medications before patient discharged home on same analgesics.
(4) Patient with history of chronic pain or analgesia use may require greater support and alteration of usual pain management protocols.
(5) If ineffective, may need prescription changed or other follow-up
d. Comfort measures
(1) Positioning and repositioning to relieve or diminish discomfort
(2) Back rub or massage may be comforting.
(3) Continue ice therapy as ordered.
(4) Promote relaxation techniques.
3. Urinary retention
a. Assess bladder status.
b. Avoid overdistention.
c. Determine adequate fluid replacement.
d. May need intermittent catheterization until able to void
4. Fluids and nutrition
a. Avoid forced fluid intake if nausea and/or vomiting present.
b. Dry crackers may help ease nausea.
c. Maintain IV fluids to ensure adequate hydration.
5. Education
a. Includes patient, family, and responsible accompanying adult
b. Instructions
(1) Infections—signs and symptoms
(2) Persistent pain or bleeding
(3) Be alert for complications.
(4) Pain relief alternatives
C. Extended observation (see Box 38-2)
1. Nutrition and diet
a. Eat lightly after the procedure.
b. If foods do not sound good, avoid and continue to drink fluids.
c. Usually can begin regular diet after 24 hours, if not earlier
d. Encourage fluid intake especially during hot weather.
e. Avoid constipation through increased dietary fiber, bulking agents.
2. Nausea and vomiting (see Chapter 25)
a. Prepare patient, family, and responsible adult for possibility of nausea and vomiting.
b. Caution patient, family, and responsible accompanying adult to call surgeon or facility if nausea and/or vomiting persists for >6 hours.
3. Pain
a. Oral analgesics
(1) Suggest contacting surgeon if pain:
(a) Not relieved by prescribed analgesics
(b) Intolerable
(c) Increasing
(2) Unrelieved or increasing pain may indicate:
(a) Infection
(b) Peritonitis
(c) Perforation
(d) Hematoma
b. Postoperative deep vein thrombosis can develop after hysterectomy or lengthy lithotomy procedures.
(1) The following may indicate deep vein thrombosis:
(a) Lower extremity pain
(b) Edema
(c) Erythema
(d) Prominent vascular pattern of the superficial veins
(2) The following are diagnostic of pulmonary embolism:
(a) Pleuritic chest pain
(b) Hemoptysis
(c) Shortness of breath
(d) Tachycardia
(e) Tachypnea
(3) Patient should call surgeon immediately and proceed to the nearest medical facility for diagnosis and treatment.
c. Alternatives
(1) Intermittent ice for external lesions to help reduce:
(a) Swelling
(b) Hematoma development
(c) Pain
(2) Sitz baths for easing discomfort of external lesion
(3) Explore with patient, family, or responsible adult other potential pain management techniques.
4. Medications: instruct on administration and how to apply.
a. Antibiotics
b. Analgesics
c. Vaginal applications
d. Topical sprays and creams
5. Wound care
a. Instruct the patient to wash hands before and after:
(1) Changing pads
(2) Dressing changes
(3) Applying medications
b. Perineal care
(1) Change pads every 4 hours or as needed.
(2) Note drainage: type, amount, and color.
(3) Gently wash the perineum with mild soap and warm water, rinse, and pat dry.
(4) Sitz baths or perineal wash as prescribed
c. Incisional care
(1) Keep wound clean and dry for minimum of 24 to 48 hours.
(2) May be instructed to remove dressing after 24 to 48 hours
(3) Observe incision for signs of infection.
(a) Redness
(b) Swelling
(c) Drainage
(4) Replace original dressing with fresh gauze or adhesive bandage as needed or as ordered.
(5) Report signs and symptoms of infection to surgeon or nurse practitioner.
d. Persistent vaginal bleeding
(1) Heavier than a menstrual period must be reported to surgeon.
(2) Bleeding may increase 7 to 10 days after cone biopsy and cervical conization.
6. Urinary care
a. Indwelling catheter (e.g., Foley) left in for continued urinary drainage
b. Wash carefully around urinary meatus with gentle soap and warm water, and pat dry.
c. Keep drainage bag below level of bladder to prevent backflow.
d. Remove at home if ordered by surgeon.
(1) Send with 10-mL syringe.
(2) Instruct how to aspirate balloon and pull catheter.
e. Arrange return appointment for catheter removal.
7. Activity
a. Rest
(1) Limit activity until pain, nausea, and dizziness subside.
(2) While taking opioid analgesics avoid:
(a) Operating machinery, automobiles
(b) Using sharp or potentially injurious articles
(c) Drinking alcohol
b. Exercise
(1) For first 24 hours, exercise is discouraged.
(2) Defer vigorous activity, heavy lifting.
(a) Restrict until surgeon allows.
(i) May be up to 4 weeks after surgery
(b) Aerobic activity increases heart rate and blood pressure, leading to increased bleeding.
c. Sexual activity
(1) Depending on location of incision, operative procedure
(2) May be advised to avoid douching and coitus for up to 6 weeks
8. Follow-up care
a. Arrange for return visit with surgeon in specified time interval.
b. Return to work dependent on:
(1) Procedure
(2) Patient’s work type
(3) Usually next day for minor procedures
(4) After hysterectomy
(a) Return in 1 to 2 weeks
(b) When capable
c. Home visit by a registered nurse may be arranged by the surgeon after certain procedures.
d. Fever
(1) Contact surgeon if temperature greater than 100.4° F (38° C).
(2) As ordered by surgeon
(3) Check temperature every 4 hours for:
(a) Two days after procedures such as hysterectomy
(b) Twice a day after laparoscopic procedures (risk for development of peritonitis)
e. Particularly with endoscopic procedures, patient should continue to get better every day.
(1) If not, an injury should be suspected.
f. Keep surgeon’s and surgery facility’s telephone number available when questions or concerns arise.
BIBLIOGRAPHY
1. Benrubi, G., Handbook of obstetric emergencies. ed 3 ( 2005)Lippincott Williams & Wilkins, Philadelphia.
2. Braveman, F., Obstetric and gynecologic anesthesia: The requisites in anaesthesiology. ( 2006)Mosby, Philadelphia.
3. Jenkins, G.; Kemnitz, C.; Tortora, G., Anatomy and physiology from science to life. ( 2007)John Wiley & Sons, Hoboken, NJ.
4. Moore, K.; Dalley, A., Clinically oriented anatomy. ed 5 ( 2006)Lippincott Williams & Wilkins, Philadelphia.
5. Nagelhout, J.; Plaus, K., Nurse anesthesia. ed 4 ( 2010)Saunders, St Louis.
6. McCann, J.S., Anatomy & physiology made incredibly easy. ed 3 ( 2009)Wolters Kluwer/Lippincott Williams & Wilkins, Philadelphia.
7. Rothrock, J.C., Alexander’s care of the patient in surgery. ed 13 ( 2007)Mosby, St Louis.
8. Scanlon, V.; Sanders, T., Essentials of anatomy and physiology. ed 4 ( 2003)FA Davis, Philadelphia.




