Invasive Mechanical Ventilation (Through an Artificial Airway): Volume and Pressure Modes
PREREQUISITE NURSING KNOWLEDGE
• Indications for the initiation of mechanical ventilation include the following:
 Apnea (e.g., neuromuscular or cardiopulmonary collapse)
Apnea (e.g., neuromuscular or cardiopulmonary collapse)
 Acute ventilatory failure, which is generally defined as a pH of less than or equal to 7.25 with an arterial partial pressure of carbon dioxide (PaCO2) greater than or equal to 50 mm Hg
Acute ventilatory failure, which is generally defined as a pH of less than or equal to 7.25 with an arterial partial pressure of carbon dioxide (PaCO2) greater than or equal to 50 mm Hg
 Impending ventilatory failure (serial decrement of arterial blood gas [ABG] values or progressive increase in signs and symptoms of increased work of breathing)
Impending ventilatory failure (serial decrement of arterial blood gas [ABG] values or progressive increase in signs and symptoms of increased work of breathing)
 Severe hypoxemia: An arterial partial pressure of oxygen (PaO2) of less than or equal to 50 mm Hg on room air indicates a critical level of oxygen in the blood. Although oxygen delivery devices may be used before intubation, the refractory nature of shunt (perfusion without ventilation) may necessitate that positive pressure be applied to reexpand closed alveoli. Restoration of functional residual capacity (FRC; lung volume that remains at the end of a passive exhalation) is the goal.
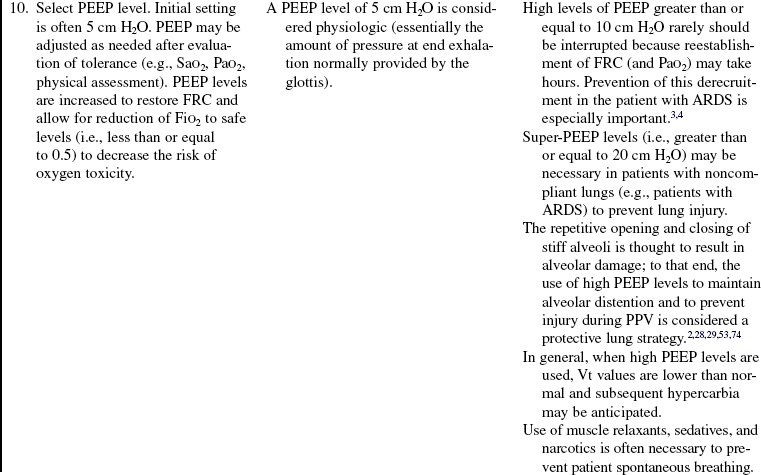
Severe hypoxemia: An arterial partial pressure of oxygen (PaO2) of less than or equal to 50 mm Hg on room air indicates a critical level of oxygen in the blood. Although oxygen delivery devices may be used before intubation, the refractory nature of shunt (perfusion without ventilation) may necessitate that positive pressure be applied to reexpand closed alveoli. Restoration of functional residual capacity (FRC; lung volume that remains at the end of a passive exhalation) is the goal.
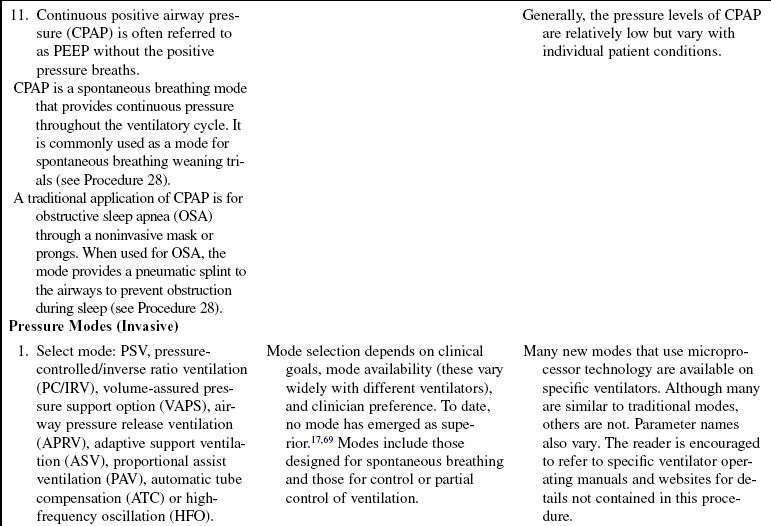
 Respiratory muscle fatigue: The muscles of respiration can become fatigued if they are made to contract repetitively at high workloads.87 Fatigue occurs when muscle energy stores become depleted. Weakness, hypermetabolic states, and chronic lung disease are examples of conditions in which patients are especially prone to fatigue. When fatigue occurs, the muscles no longer contract optimally and hypercarbia results.8,20 Twelve to 24 hours of rest are typically needed to rest the muscles. Respiratory muscle rest requires that the workload of the muscles (or muscle loading) be offset so that mitochondrial energy stores can be repleted.8,20 Respiratory work and rest vary with different modes and the application of the same. In general, when hypercarbia is present, mechanical ventilation is necessary to relieve the work of breathing. Muscle unloading is accomplished differently and depends on patient-ventilator interaction and the mode.13,14,55,57,61,68
Respiratory muscle fatigue: The muscles of respiration can become fatigued if they are made to contract repetitively at high workloads.87 Fatigue occurs when muscle energy stores become depleted. Weakness, hypermetabolic states, and chronic lung disease are examples of conditions in which patients are especially prone to fatigue. When fatigue occurs, the muscles no longer contract optimally and hypercarbia results.8,20 Twelve to 24 hours of rest are typically needed to rest the muscles. Respiratory muscle rest requires that the workload of the muscles (or muscle loading) be offset so that mitochondrial energy stores can be repleted.8,20 Respiratory work and rest vary with different modes and the application of the same. In general, when hypercarbia is present, mechanical ventilation is necessary to relieve the work of breathing. Muscle unloading is accomplished differently and depends on patient-ventilator interaction and the mode.13,14,55,57,61,68
• Ventilators are categorized as either negative or positive pressure. Although negative-pressure ventilation (i.e., the iron lung) was used extensively in the 1940s, introduction of the cuffed endotracheal tube resulted in the dominance of positive-pressure ventilation (PPV) in clinical practice during the second half of the 20th century. Although sporadic interest in negative-pressure ventilation continues, the cumbersome nature of the ventilators and the lack of airway protection associated with this form of ventilation preclude a serious resurgence of this mode of ventilation.
 Positive pressure ventilation: Positive-pressure modes of ventilation have traditionally been categorized into volume and pressure. However, with the advent of microprocessor technology, sophisticated iterations of traditional volume and pressure modes of ventilation have evolved.69 Many of the modes have names that are different from traditional volume and pressure modes, but they are similar in many cases. Little data exist to show that the newer modes improve outcomes.17,69 A wide variety of modes described in this procedure are actually a combination of volume and pressure but for ease of learning are classified into specific categories.
Positive pressure ventilation: Positive-pressure modes of ventilation have traditionally been categorized into volume and pressure. However, with the advent of microprocessor technology, sophisticated iterations of traditional volume and pressure modes of ventilation have evolved.69 Many of the modes have names that are different from traditional volume and pressure modes, but they are similar in many cases. Little data exist to show that the newer modes improve outcomes.17,69 A wide variety of modes described in this procedure are actually a combination of volume and pressure but for ease of learning are classified into specific categories.
 Volume ventilation has traditionally been the most popular form of PPV, largely because tidal volume (Vt) and minute ventilation (MV) are ensured, which is an essential goal in the patient with acute illness. With volume ventilation, a predetermined Vt is delivered with each breath regardless of resistance and compliance. Vt is stable from breath to breath, but airway pressure may vary. To rest the respiratory muscles with volume ventilation, the ventilator rate must be increased until spontaneous respiratory effort ceases. When spontaneous effort is present, such as with initiation of an assist/control (A/C) breath, respiratory muscle work continues throughout the breath.61
Volume ventilation has traditionally been the most popular form of PPV, largely because tidal volume (Vt) and minute ventilation (MV) are ensured, which is an essential goal in the patient with acute illness. With volume ventilation, a predetermined Vt is delivered with each breath regardless of resistance and compliance. Vt is stable from breath to breath, but airway pressure may vary. To rest the respiratory muscles with volume ventilation, the ventilator rate must be increased until spontaneous respiratory effort ceases. When spontaneous effort is present, such as with initiation of an assist/control (A/C) breath, respiratory muscle work continues throughout the breath.61
 With traditional pressure ventilation, the practitioner selects the desired pressure level and the Vt is determined by the selected pressure level, resistance, and compliance. This characteristic is important to note in caring for a patient with an unstable condition on a pressure mode of ventilation. Careful attention to Vt is necessary to prevent inadvertent hyperventilation or hypoventilation. To ensure respiratory muscle rest on pressure-support ventilation (PSV), workload must be offset with the appropriate adjustment of the pressure-support (PS) level. To accomplish this adjustment, the PS level is increased to lower the spontaneous respiratory rate to less than or equal to 20 breaths/min and to attain a Vt of 6 to 10 mm/kg.13,14,55
With traditional pressure ventilation, the practitioner selects the desired pressure level and the Vt is determined by the selected pressure level, resistance, and compliance. This characteristic is important to note in caring for a patient with an unstable condition on a pressure mode of ventilation. Careful attention to Vt is necessary to prevent inadvertent hyperventilation or hypoventilation. To ensure respiratory muscle rest on pressure-support ventilation (PSV), workload must be offset with the appropriate adjustment of the pressure-support (PS) level. To accomplish this adjustment, the PS level is increased to lower the spontaneous respiratory rate to less than or equal to 20 breaths/min and to attain a Vt of 6 to 10 mm/kg.13,14,55
 Pressure ventilation provides for an augmented inspiration (pressure is maintained throughout inspiration). The flow pattern (speed of the gas) is described as decelerating; that is, gas flow delivery is high at the beginning of the breath and tapers off toward the end of the breath. This pattern is in contrast to volume ventilation, in which the flow rate is typically more consistent during inspiration (i.e., the same at the beginning of the breath as at the end of the breath). The decelerating flow pattern associated with pressure ventilation is thought to provide better gas distribution and more efficient ventilation.14,55,56
Pressure ventilation provides for an augmented inspiration (pressure is maintained throughout inspiration). The flow pattern (speed of the gas) is described as decelerating; that is, gas flow delivery is high at the beginning of the breath and tapers off toward the end of the breath. This pattern is in contrast to volume ventilation, in which the flow rate is typically more consistent during inspiration (i.e., the same at the beginning of the breath as at the end of the breath). The decelerating flow pattern associated with pressure ventilation is thought to provide better gas distribution and more efficient ventilation.14,55,56
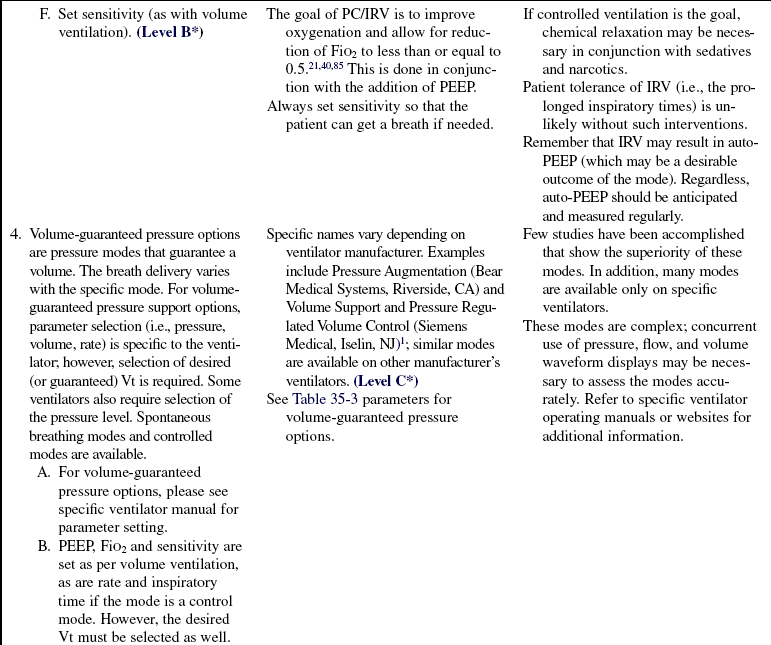
 Increasingly sophisticated ventilator technology has resulted in the development of volume-assured pressure modes of ventilation. Ventilator manufacturers have responded rapidly to the request of practitioners that pressure modes of ventilation be designed in such a way that volume be guaranteed on a breath-to-breath basis. The potential value of such modes is obvious. The more desirable decelerating flow pattern may be provided and plateau pressures controlled, with ensured Vt and MV.
Increasingly sophisticated ventilator technology has resulted in the development of volume-assured pressure modes of ventilation. Ventilator manufacturers have responded rapidly to the request of practitioners that pressure modes of ventilation be designed in such a way that volume be guaranteed on a breath-to-breath basis. The potential value of such modes is obvious. The more desirable decelerating flow pattern may be provided and plateau pressures controlled, with ensured Vt and MV.
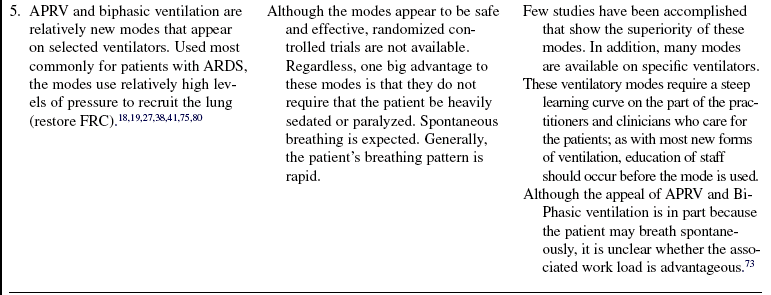
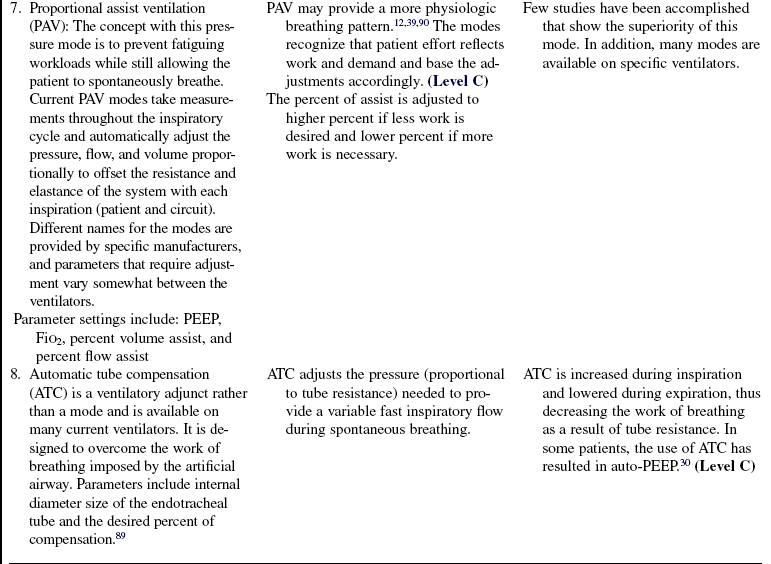
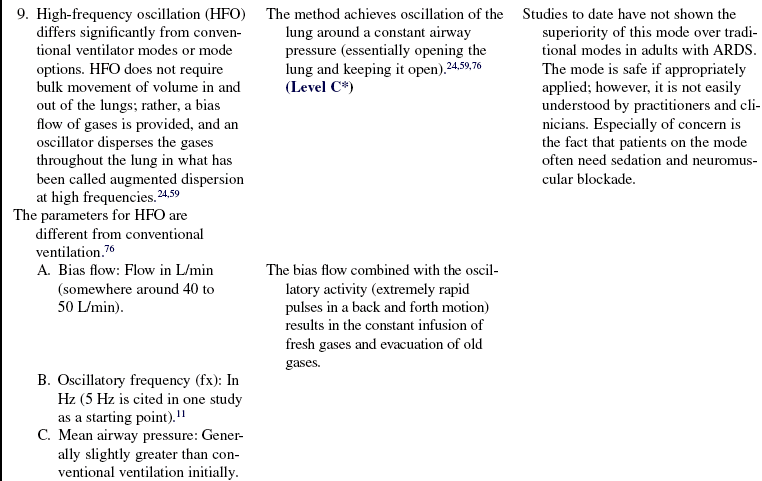
 Additional modes of ventilation have been promoted for use in patients with acute respiratory distress syndrome (ARDS), including high-frequency oscillation, pressure-release ventilation, and other ventilator-specific modes, such as biphasic, adaptive support and proportional assist ventilation. Although some data exist that suggest the modes may be beneficial in patients with ARDS, to date no change in mortality rate has been noted, although positive trends have been demonstrated in some variables of interest such as oxygenation.12,18,19,24,27,38,39,41,59,66,73,75,79–82,84,90
Additional modes of ventilation have been promoted for use in patients with acute respiratory distress syndrome (ARDS), including high-frequency oscillation, pressure-release ventilation, and other ventilator-specific modes, such as biphasic, adaptive support and proportional assist ventilation. Although some data exist that suggest the modes may be beneficial in patients with ARDS, to date no change in mortality rate has been noted, although positive trends have been demonstrated in some variables of interest such as oxygenation.12,18,19,24,27,38,39,41,59,66,73,75,79–82,84,90
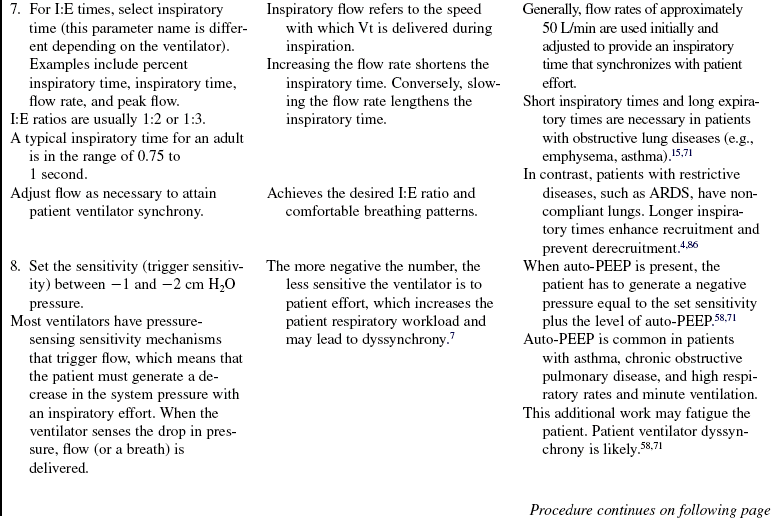
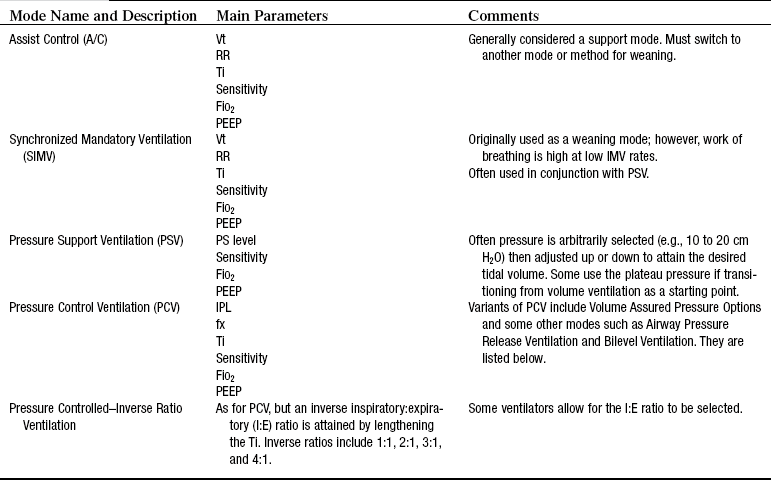
• Summary descriptions of modes, mode parameters, and ventilator alarms are provided within this procedure and in Tables 35-1, 35-2, and 35-3.
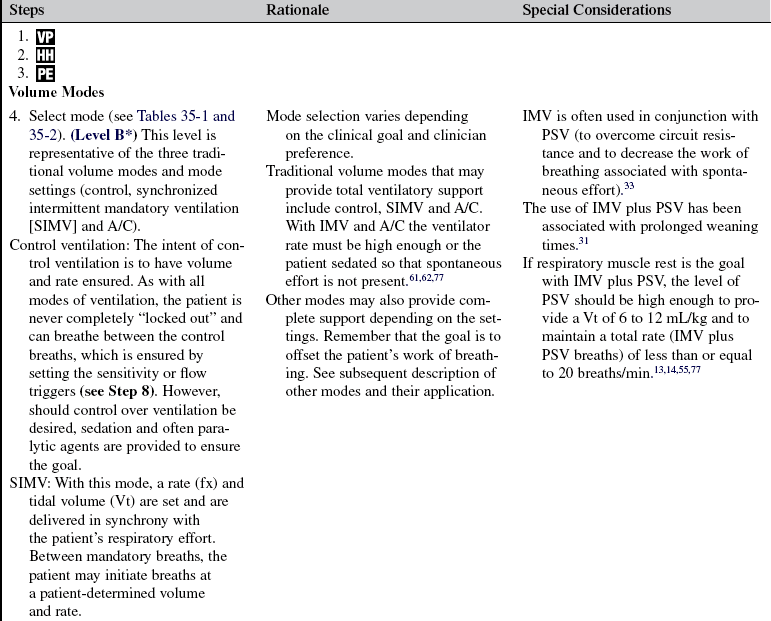
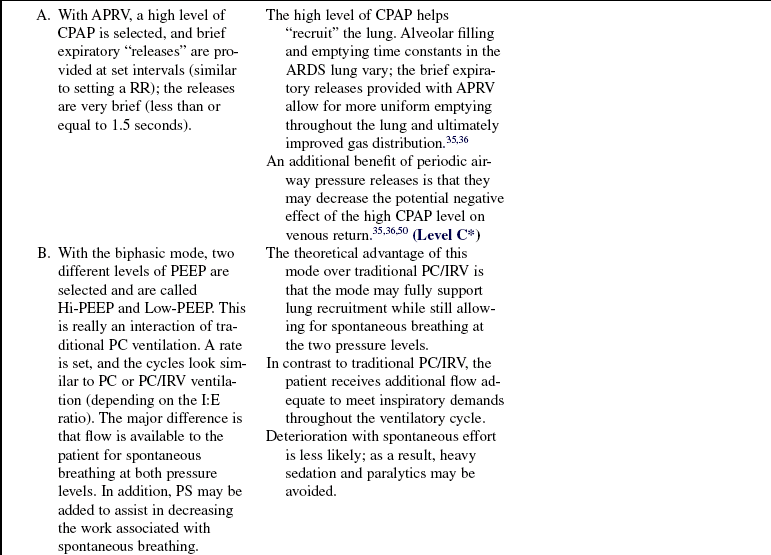
Table 35-1
Traditional Modes of Mechanical Ventilation (on All Ventilators)
Volume Modes
Control Ventilation (CV) or Controlled Mandatory Ventilation (CMV)
Description: With this mode, the ventilator provides all of the patient’s minute ventilation. The clinician sets the rate, Vt, inspiratory time, and PEEP. Generally, this term is used to describe situations in which the patient is chemically relaxed or is paralyzed from a spinal cord or neuromuscular disease and is unable to initiate spontaneous breaths. The ventilator mode setting may be set on CMV, assist/control (A/C), or synchronized intermittent mandatory ventilation (SIMV) because all these options provide volume breaths at the clinician-selected rate.
Assist/Control (A/C) or Assisted Mandatory Ventilation (AMV)
Description: This option requires that a rate, Vt, inspiratory time, and PEEP be set for the patient. The ventilator sensitivity also is set, and when the patient initiates a spontaneous breath, a full-volume breath is delivered.
Synchronized Intermittent Mandatory Ventilation (SIMV)
Description: This mode requires that rate, Vt, inspiratory time, sensitivity, and PEEP are set by the clinician. In between mandatory breaths, patients can spontaneously breathe at their own rates and Vt. With SIMV, the ventilator synchronizes the mandatory breaths with the patient’s own inspirations.
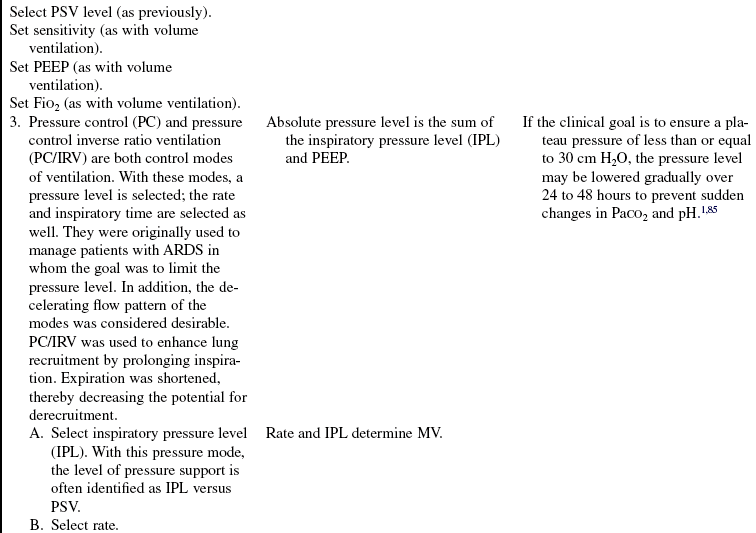
Pressure Modes
Pressure Support Ventilation (PSV)
Description: This mode provides an augmented inspiration to a patient who is spontaneously breathing. With PS, the clinician selects an inspiratory pressure level, PEEP, and sensitivity. When the patient initiates a breath, a high flow of gas is delivered to the preselected pressure level, and pressure is maintained throughout inspiration. The patient determines the parameters of Vt, rate, and inspiratory time.
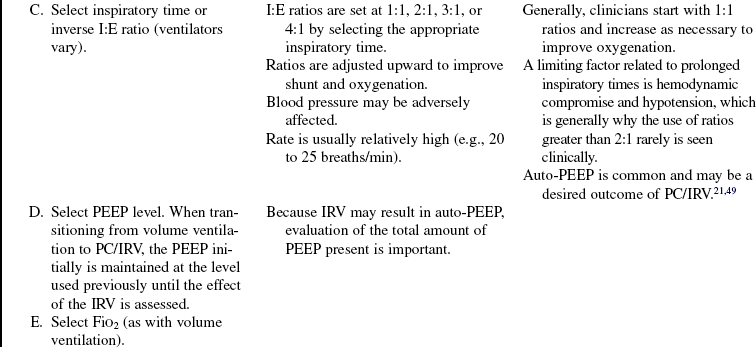
Pressure-Controlled/Inverse Ratio Ventilation (PC/IRV)
Description: This mode combines pressure-limited ventilation with an inverse ratio of inspiration to expiration. The clinician selects the pressure level, rate, inspiratory time (1:1, 2:1, 3:1, 4:1), and PEEP level. With prolonged inspiratory times, auto-PEEP may result. The auto-PEEP may be a desirable outcome of the inverse ratios. Some clinicians use PC without IRV. Conventional inspiratory times are used, and rate, pressure level, and PEEP are selected.
Positive End-Expiratory Pressure (PEEP) and Continuous Positive Airway Pressure (CPAP)
Description: This ventilatory option creates positive pressure at end exhalation. PEEP restores FRC. The term PEEP is used when end-expiratory pressure is provided during ventilator positive pressure breaths.
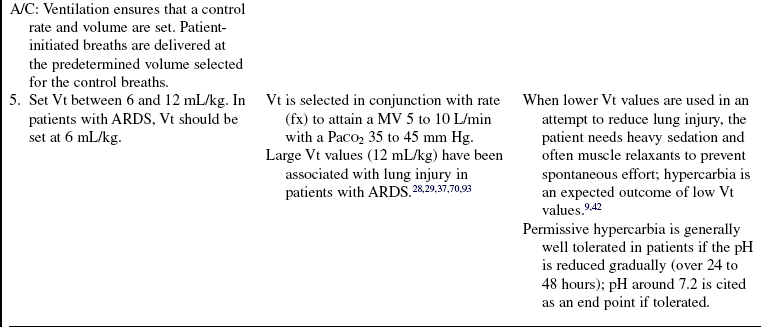
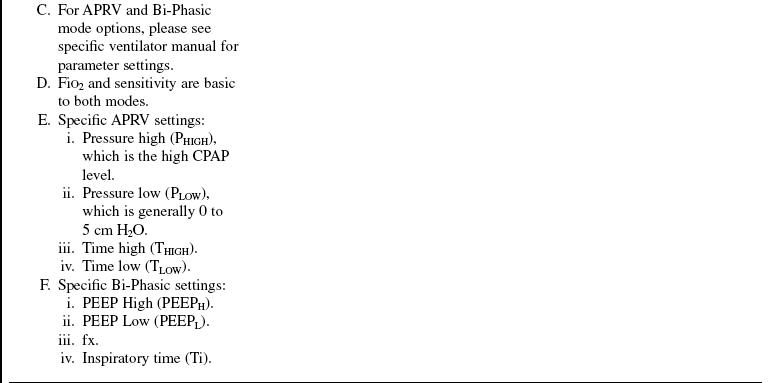
Table 35-2
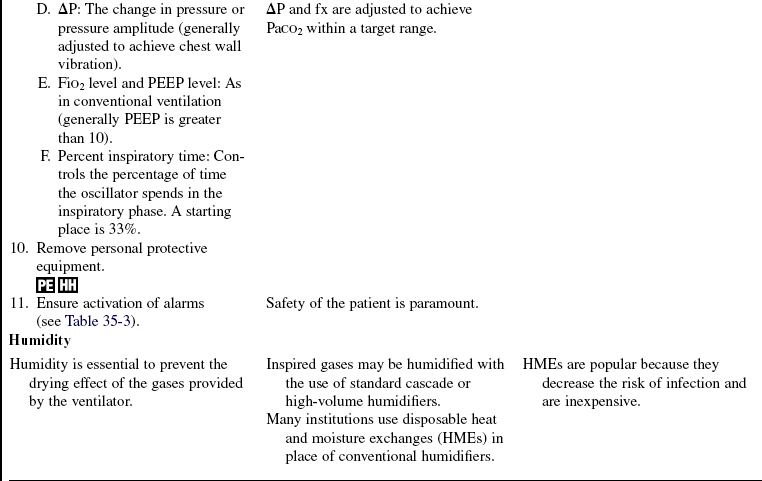
Volume and Pressure Modes and Corresponding Ventilator Parameters
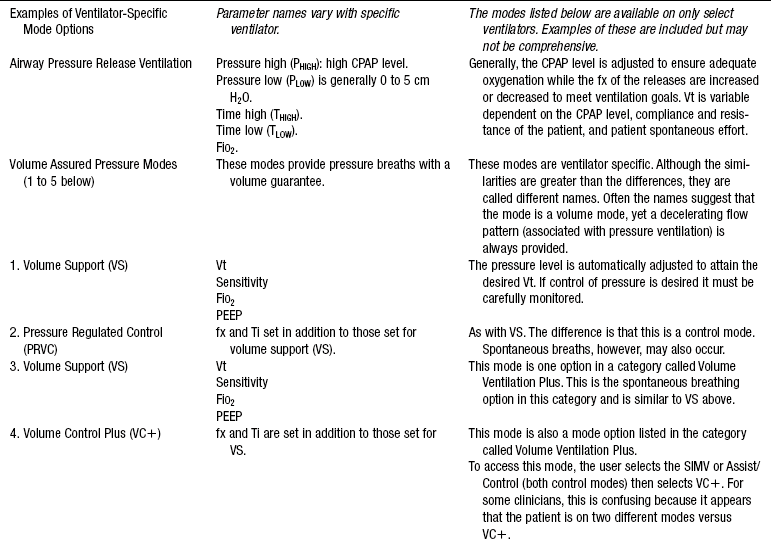
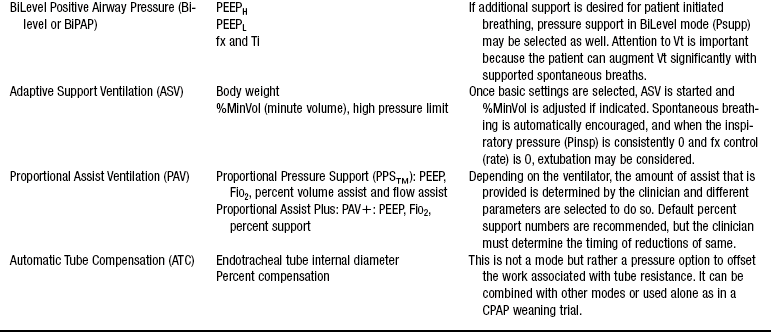
Adapted with permission from Burns S: Pressure modes of mechanical ventilation: the good, bad and the ugly, AACN Adv Crit Care 19:399-411, 2008.
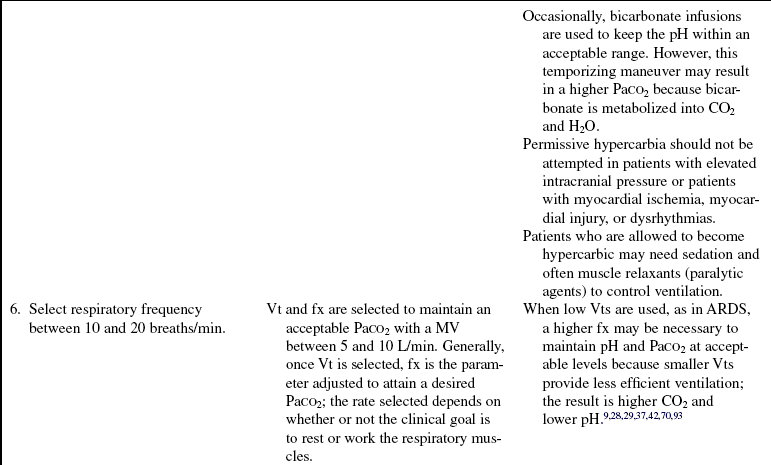
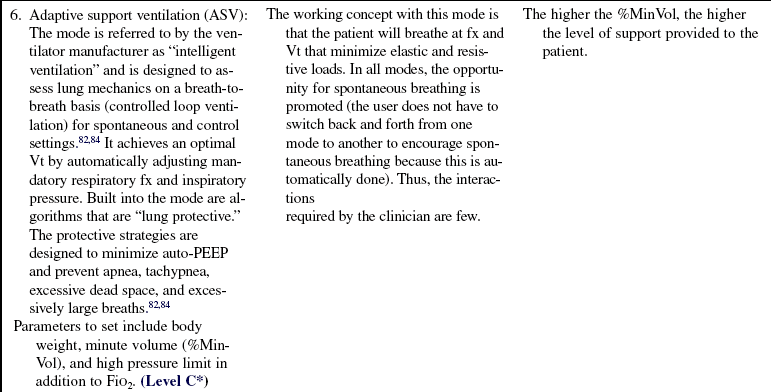
Table 35-3
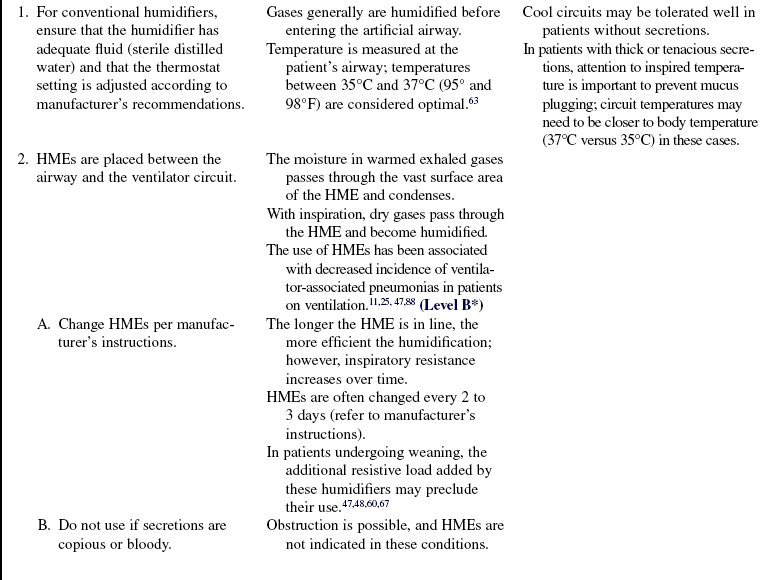
Disconnect Alarms (Low-Pressure or Low-Volume Alarms)
When disconnection occurs, the clinician must be immediately notified. Generally, this alarm is a continuous one and is triggered when a preselected inspiratory pressure level or minute ventilation is not sensed. With circuit leaks, this same alarm may be activated even though the patient may still be receiving a portion of the preset breath. Physical assessment, digital displays, and manometers are helpful in troubleshooting the cause of the alarms.
Pressure Alarms
High-pressure alarms are set with volume modes of ventilation to ensure notification of pressures that exceed the selected threshold. These alarms are usually set 10 to 15 cm H2O above the usual peak inspiratory pressure (PIP). Some causes for alarm activation (generally an intermittent alarm) include secretions, condensate in the tubing, biting on the endotracheal tubing, increased resistance (i.e., bronchospasm), decreased compliance (e.g., pulmonary edema, pneumothorax), and tubing compression.
Low-pressure alarms are used to sense disconnection, circuit leaks, and changing compliance and resistance. They are generally set 5 to 10 cm H2O below the usual PIP or 1 to 2 cm H2O below the PEEP level or both.
Minute ventilation alarms may be used to sense disconnection or changes in breathing pattern (rate and volume). Generally, low–minute ventilation and high–minute ventilation alarms are set (usually 5 to 10 L/min above and below usual minute ventilation). When stand-alone pressure support ventilation (PSV) is in use, this alarm may be the only audible alarm available on some ventilators.
FiO2 alarms are provided on most new ventilators and are set 5 to 10 mm Hg above and below the selected FiO2 level.
Alarm silence or pause options are built in by ventilator manufacturers so that clinicians can temporarily silence alarms for short periods (i.e., 20 seconds) because alarms must stay activated at all times. The ventilators reset the alarms automatically.
Alarms provide important protection for patients on ventilation. However, inappropriate threshold settings decrease usefulness. When threshold gradients are set too narrowly, alarms occur needlessly and frequently. Conversely, alarms that are set too loosely (wide gradients) do not allow for accurate and timely assessments.
From Burns SM: Mechanical ventilation and weaning. In Kinney MR, et al, editors: AACN clinical reference for critical care nursing, ed 4, St Louis, 1998, Mosby.
• Complications of PPV include volume-pressure trauma, hemodynamic changes, and pulmonary barotrauma.
 Volume-pressure trauma, in contrast to barotrauma (or air leak disease), was first described in animals with stiff noncompliant lungs who were ventilated with traditional lung volumes (range, 10 to 12 mL/kg). The investigators noted that the large volumes translated into high plateau pressures (also known as static, distending, or alveolar pressure) and subsequent acute lung injury. The lung injury was described as a loss of alveolar integrity (i.e., alveolar fractures) and movement of fluids and proteins into the alveolar space (sometimes called non-ARDS-ARDS).28,29,37,70,93 Plateau pressures of 30 cm H2O or more for greater than 48 to 72 hours were associated with the injury.28
Volume-pressure trauma, in contrast to barotrauma (or air leak disease), was first described in animals with stiff noncompliant lungs who were ventilated with traditional lung volumes (range, 10 to 12 mL/kg). The investigators noted that the large volumes translated into high plateau pressures (also known as static, distending, or alveolar pressure) and subsequent acute lung injury. The lung injury was described as a loss of alveolar integrity (i.e., alveolar fractures) and movement of fluids and proteins into the alveolar space (sometimes called non-ARDS-ARDS).28,29,37,70,93 Plateau pressures of 30 cm H2O or more for greater than 48 to 72 hours were associated with the injury.28
 Studies in humans followed the recognition that large Vts may be associated with lung injury.42,86 The ARDS Network conducted randomized controlled trial (RCTs) of adult patients with ARDS that compared low lung volume ventilation (6 mL/kg) with more traditional volumes (i.e., 12 mL/kg). The results showed that the lower volume ventilation resulted in a lower mortality rate.86 As a result, current recommendations are to limit volumes (and lower pressures) in patients with stiff lungs. With pressure ventilation, pressure is limited by definition; however, until additional evidence emerges on the efficacy of controlling pressures versus volumes in ARDS, a goal should be to ensure a Vt in the 6 mL/kg range. Another lung protective strategy is that of is that of “recruitment” and the prevention of “derecruitment.” Investigators showed that stiff noncompliant lungs were at risk of trauma from the repetitive opening associated with tidal breaths. The application of higher levels of positive end-expiratory pressure (PEEP) was associated with better recruitment and resulted in improved mortality rates.3,4,73
Studies in humans followed the recognition that large Vts may be associated with lung injury.42,86 The ARDS Network conducted randomized controlled trial (RCTs) of adult patients with ARDS that compared low lung volume ventilation (6 mL/kg) with more traditional volumes (i.e., 12 mL/kg). The results showed that the lower volume ventilation resulted in a lower mortality rate.86 As a result, current recommendations are to limit volumes (and lower pressures) in patients with stiff lungs. With pressure ventilation, pressure is limited by definition; however, until additional evidence emerges on the efficacy of controlling pressures versus volumes in ARDS, a goal should be to ensure a Vt in the 6 mL/kg range. Another lung protective strategy is that of is that of “recruitment” and the prevention of “derecruitment.” Investigators showed that stiff noncompliant lungs were at risk of trauma from the repetitive opening associated with tidal breaths. The application of higher levels of positive end-expiratory pressure (PEEP) was associated with better recruitment and resulted in improved mortality rates.3,4,73
 The extent of hemodynamic changes associated with PPV depends on the level of applied positive pressure, the duration of positive pressure during different phases of the breathing cycle, the amount of pressure transmitted to the vascular structures, the patient’s intravascular volume, and the adequacy of hemodynamic compensatory mechanisms. PPV can reduce venous return, shift the intraventricular septum to the left, and increase right ventricular afterload as a result of increased pulmonary vascular resistance.1,50 The hemodynamic effects of PPV may be prevented or corrected by optimizing filling pressures to accommodate the PPV-induced changes in intrathoracic pressures; by minimizing the peak pressure, plateau pressure, and PEEP; and by optimizing the inspiratory-to-expiratory (I:E) ratio.
The extent of hemodynamic changes associated with PPV depends on the level of applied positive pressure, the duration of positive pressure during different phases of the breathing cycle, the amount of pressure transmitted to the vascular structures, the patient’s intravascular volume, and the adequacy of hemodynamic compensatory mechanisms. PPV can reduce venous return, shift the intraventricular septum to the left, and increase right ventricular afterload as a result of increased pulmonary vascular resistance.1,50 The hemodynamic effects of PPV may be prevented or corrected by optimizing filling pressures to accommodate the PPV-induced changes in intrathoracic pressures; by minimizing the peak pressure, plateau pressure, and PEEP; and by optimizing the inspiratory-to-expiratory (I:E) ratio.
 Pulmonary barotrauma (i.e., air leak disease) is damage to the lung from extrapulmonary air that may result from changes in intrathoracic pressures during PPV. Barotrauma is manifested by pneumothorax, pneumomediastinum, pneumopericardium, pneumoperitoneum, and subcutaneous emphysema. The risk of barotrauma in a patient receiving PPV is increased with preexisting lung lesions (e.g., localized infections, blebs), high inflation pressures (i.e., large Vt, PEEP, main-stem bronchus intubation, patient-ventilator asynchrony), and invasive thoracic procedures (e.g., subclavian catheter insertion, bronchoscopy, thoracentesis). Barotrauma from PPV may be prevented by controlling peak and plateau pressures, optimizing PEEP, preventing auto-PEEP, ensuring patient-ventilator synchrony, and ensuring proper artificial airway position.
Pulmonary barotrauma (i.e., air leak disease) is damage to the lung from extrapulmonary air that may result from changes in intrathoracic pressures during PPV. Barotrauma is manifested by pneumothorax, pneumomediastinum, pneumopericardium, pneumoperitoneum, and subcutaneous emphysema. The risk of barotrauma in a patient receiving PPV is increased with preexisting lung lesions (e.g., localized infections, blebs), high inflation pressures (i.e., large Vt, PEEP, main-stem bronchus intubation, patient-ventilator asynchrony), and invasive thoracic procedures (e.g., subclavian catheter insertion, bronchoscopy, thoracentesis). Barotrauma from PPV may be prevented by controlling peak and plateau pressures, optimizing PEEP, preventing auto-PEEP, ensuring patient-ventilator synchrony, and ensuring proper artificial airway position.
 Auto-PEEP is a common complication of mechanical ventilation and can result in hemodynamic compromise and even death. Because increased intrathoracic pressures are transmitted to the adjacent capillaries, venous return is decreased and the effect can be profound. Auto-PEEP and dynamic hyperinflation should be assumed in the patient on ventilation with acute severe asthma whose condition is hemodynamically compromised, and a brief cessation of mechanical ventilation or decrease in rate and shortening of inspiratory time should be accomplished.54,71 Auto-PEEP is caused by inadequate expiratory time relative to the patient’s lung condition. Auto-PEEP is associated with prolonged inspiratory times, short expiratory times, high minute ventilation requirements, bronchospasm, low elastic recoil, mucus hypersecretion, increased wall thickness, airway closure or collapse, and mechanical factors (e.g., water in the ventilator circuit, pinched ventilator tubing).54,71 Correcting these factors reduces auto-PEEP. In some cases, adding set PEEP results in reduction of the inspiratory trigger threshold and thus improvement of patient triggering.15,58
Auto-PEEP is a common complication of mechanical ventilation and can result in hemodynamic compromise and even death. Because increased intrathoracic pressures are transmitted to the adjacent capillaries, venous return is decreased and the effect can be profound. Auto-PEEP and dynamic hyperinflation should be assumed in the patient on ventilation with acute severe asthma whose condition is hemodynamically compromised, and a brief cessation of mechanical ventilation or decrease in rate and shortening of inspiratory time should be accomplished.54,71 Auto-PEEP is caused by inadequate expiratory time relative to the patient’s lung condition. Auto-PEEP is associated with prolonged inspiratory times, short expiratory times, high minute ventilation requirements, bronchospasm, low elastic recoil, mucus hypersecretion, increased wall thickness, airway closure or collapse, and mechanical factors (e.g., water in the ventilator circuit, pinched ventilator tubing).54,71 Correcting these factors reduces auto-PEEP. In some cases, adding set PEEP results in reduction of the inspiratory trigger threshold and thus improvement of patient triggering.15,58
• Associated complications of PPV include ventilator-associated pneumonia (VAP)6, deep vein thrombosis (and subsequent pulmonary embolus), and gastrointestinal bleeding. Although all the associated complications are important and require that appropriate evidence-based prophylaxis regimens are initiated, only VAP is discussed. Please refer to other system-specific chapters in this manual for information on the others.
 VAP occurs after 3 to 5 days of mechanical ventilation and accounts for one third of all healthcare-associated infections and between 50% and 83% of infections in the patient with MV.6,26,52,78,91
VAP occurs after 3 to 5 days of mechanical ventilation and accounts for one third of all healthcare-associated infections and between 50% and 83% of infections in the patient with MV.6,26,52,78,91
 Modifiable risk factors to the aspiration of colonized organisms in the patient on ventilation include interventions such as proper endotracheal tube cuff inflation (secretions that collect above the cuff of the endotracheal or tracheostomy tube and leak past the cuff into the lungs), use of continuous aspiration subglottic suctioning (CASS) tubes, decreased ventilator tubing changes, use of heat and moisture exchangers (HMEs), stringent hand washing, backrest elevation (BRE) of greater than 30 degrees, and when possible, the use of noninvasive ventila- tion (especially in patients with immunocompromise).5,6,10,16,22,26,32,43,45,51,64,72,83
Modifiable risk factors to the aspiration of colonized organisms in the patient on ventilation include interventions such as proper endotracheal tube cuff inflation (secretions that collect above the cuff of the endotracheal or tracheostomy tube and leak past the cuff into the lungs), use of continuous aspiration subglottic suctioning (CASS) tubes, decreased ventilator tubing changes, use of heat and moisture exchangers (HMEs), stringent hand washing, backrest elevation (BRE) of greater than 30 degrees, and when possible, the use of noninvasive ventila- tion (especially in patients with immunocompromise).5,6,10,16,22,26,32,43,45,51,64,72,83
 Other interventions with a lower level of evidence supporting their use include oral care techniques such as mouth care and oral decontamination with agents such as chlorhexidine or oral antibiotics.45 Of interest, gastric residual volumes have not been found to be consistently associated with VAP.46,65 Table 35-4 lists the top recommendations of authoritative professional organizations for the prevention of VAP.
Other interventions with a lower level of evidence supporting their use include oral care techniques such as mouth care and oral decontamination with agents such as chlorhexidine or oral antibiotics.45 Of interest, gastric residual volumes have not been found to be consistently associated with VAP.46,65 Table 35-4 lists the top recommendations of authoritative professional organizations for the prevention of VAP.
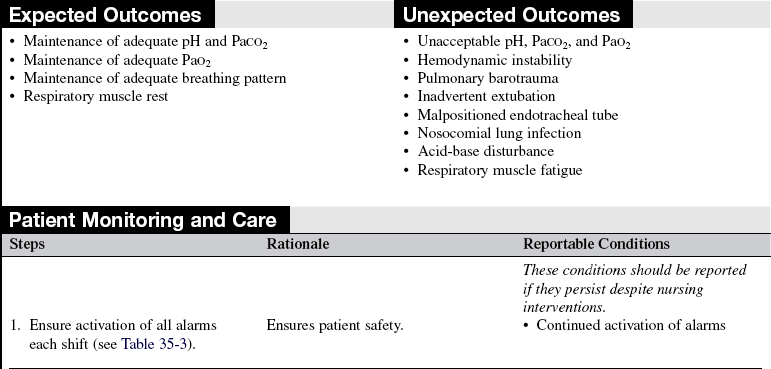
Table 35-4
Top Modifiable VAP Prevention Interventions: Guidelines by Authoritative Professional Organizations.
Top Guideline Recommendations by Professional Associations*
BRE (>30 to 45 degrees)
CASS tubes
Cuff inflation
Hand washing and aseptic technique
HMEs
No routine ventilator circuit change
Noninvasive ventilation when possible
*Professional Associations: American Thoracic Society (ATS), American Association of Critical-Care Nurses (AACN), Centers for Disease Control and Prevention (CDC), and Canadian Critical Care Trials Group and the Canadian Critical Care Society (CCCT/CCCS).
EQUIPMENT
• Endotracheal or tracheostomy tube (see Procedures 2 and 14)
• Electrocardiogram and pulse oximetry
• Manual self-inflating resuscitation bag-valve device (with PEEP adjusted to patient baseline level or with a PEEP valve)
• Appropriately sized resuscitation face mask
• End-tidal carbon dioxide detector, with a colorimetric CO2 detector or continuous monitor: The colorimetric detectors are used to ensure proper endotracheal tube placement and are a standard of care for intubation in many institutions. The continuous monitors are used in assessment of patients on ventilation on an ongoing basis.
PATIENT AND FAMILY EDUCATION
• Explain the procedure and the reasons for PPV to the patient and family.6  Rationale: Communication and explanations for therapy are cited as important needs of patients and families.
Rationale: Communication and explanations for therapy are cited as important needs of patients and families.
• Discuss the potential sensations the patient will experience, such as relief of dyspnea, lung inflations, noise of ventilator operation, and alarm sounds.  Rationale: Knowledge of anticipated sensory experiences reduces anxiety and distress.
Rationale: Knowledge of anticipated sensory experiences reduces anxiety and distress.
• Encourage the patient to relax.  Rationale: This encouragement promotes general relaxation, oxygenation, and ventilation.
Rationale: This encouragement promotes general relaxation, oxygenation, and ventilation.
• Explain that the patient will be unable to speak. Establish a method of communication in conjunction with the patient and family before initiating mechanical ventilation, if necessary.  Rationale: Ensuring the patient’s ability to communicate is important to alleviate anxiety.
Rationale: Ensuring the patient’s ability to communicate is important to alleviate anxiety.
• Teach the family how to perform desired and appropriate activities of direct patient care, such as pharyngeal suction with the tonsil-tip suction device, range-of-motion exercises, and reconnection to ventilator if inadvertent disconnection occurs. Demonstrate use of call bell.  Rationale: Family members have identified the need and desire to help in the patient’s care.
Rationale: Family members have identified the need and desire to help in the patient’s care.
• Provide the patient and family with information on the critical nature of the patient’s dependence on PPV.  Rationale: Knowledge of the prognosis, probable outcome, or chance for recovery is cited as an important need of patients and families.
Rationale: Knowledge of the prognosis, probable outcome, or chance for recovery is cited as an important need of patients and families.
• Offer the opportunity for the patient and family to ask questions about PPV.  Rationale: Asking questions and having questions answered honestly are cited consistently as the most important need of patients and families.
Rationale: Asking questions and having questions answered honestly are cited consistently as the most important need of patients and families.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess for signs and symptoms of acute ventilatory failure and fatigue:
 Rising arterial carbon dioxide tension
Rising arterial carbon dioxide tension
 Shallow or irregular respirations
Shallow or irregular respirations
 Tachypnea, bradypnea, or dyspnea
Tachypnea, bradypnea, or dyspnea
 Restlessness, confusion, or lethargy
Restlessness, confusion, or lethargy
 Rationale: Ventilatory failure indicates the need for initiation of PPV. While PPV is being considered and assembled, support ventilation via a self-inflating manual resuscitation bag-valve-mask, if necessary.
Rationale: Ventilatory failure indicates the need for initiation of PPV. While PPV is being considered and assembled, support ventilation via a self-inflating manual resuscitation bag-valve-mask, if necessary.
• Determine arterial pH and carbon dioxide tension.  Rationale: Acute ventilatory failure is confirmed by an uncompensated respiratory acidosis. Ventilatory failure is an indication for PPV.
Rationale: Acute ventilatory failure is confirmed by an uncompensated respiratory acidosis. Ventilatory failure is an indication for PPV.
• Assess for signs and symptoms of inadequate oxygenation:
 Decreasing arterial oxygen tension
Decreasing arterial oxygen tension
 Alterations in level of consciousness
Alterations in level of consciousness
 Intercostal and suprasternal retractions
Intercostal and suprasternal retractions
 Rationale: Hypoxemia may indicate the need for PPV. While PPV is being considered and assembled, provide 100% oxygen via manual resuscitation bag and mask or via an oxygen delivery device, such as a nonrebreather mask.
Rationale: Hypoxemia may indicate the need for PPV. While PPV is being considered and assembled, provide 100% oxygen via manual resuscitation bag and mask or via an oxygen delivery device, such as a nonrebreather mask.
• Determine PaO2 or arterial oxygen saturation (SaO2).  Rationale: Hypoxemia is confirmed by PaO2 of less than 60 mm Hg or SaO2 of less than 90% on supplemental oxygen. Hypoxemia may indicate the need for PPV.
Rationale: Hypoxemia is confirmed by PaO2 of less than 60 mm Hg or SaO2 of less than 90% on supplemental oxygen. Hypoxemia may indicate the need for PPV.
• Assess for signs and symptoms of inadequate breathing patterns:
 Rationale: Respiratory distress is an indication for PPV. A comfortable breathing pattern is a goal of PPV. An inadequate breathing pattern on ventilatory support can be corrected by determining and treating the underlying acute cause such as pulmonary edema or by fixing a mechanical problem such as a malpositioned endotracheal tube. Adjustment of the ventilator parameters in these cases may be necessary.
Rationale: Respiratory distress is an indication for PPV. A comfortable breathing pattern is a goal of PPV. An inadequate breathing pattern on ventilatory support can be corrected by determining and treating the underlying acute cause such as pulmonary edema or by fixing a mechanical problem such as a malpositioned endotracheal tube. Adjustment of the ventilator parameters in these cases may be necessary.
• Assess for signs of atelectasis:
 Localized changes in auscultation (increased or bronchial breath sounds)
Localized changes in auscultation (increased or bronchial breath sounds)
 Localized dullness to percussion
Localized dullness to percussion
 Tracheal deviation toward the side of abnormal findings
Tracheal deviation toward the side of abnormal findings
 Increased peak and plateau pressures
Increased peak and plateau pressures
 Decreased PaO2 or SaO2 (with constant ventilator parameters)
Decreased PaO2 or SaO2 (with constant ventilator parameters)
 Localized consolidation (“whiteout,” opacity) on chest radiograph
Localized consolidation (“whiteout,” opacity) on chest radiograph
 Rationale: Early detection of atelectasis indicates the need for alteration of interventions to promote resolution (e.g., hyperinflation techniques, PEEP adjustments).
Rationale: Early detection of atelectasis indicates the need for alteration of interventions to promote resolution (e.g., hyperinflation techniques, PEEP adjustments).
• Assess for signs and symptoms of pulmonary barotrauma (i.e., pneumothorax):
 Acute, increasing, or severe dyspnea
Acute, increasing, or severe dyspnea
 Localized changes in auscultation (decreased or absent breath sounds) on the affected side
Localized changes in auscultation (decreased or absent breath sounds) on the affected side
 Localized hyperresonance or tympany to percussion on the affected side
Localized hyperresonance or tympany to percussion on the affected side
 Elevated chest on the affected side
Elevated chest on the affected side
 Tracheal deviation away from the side of abnormal findings
Tracheal deviation away from the side of abnormal findings
 Increased peak and plateau pressures
Increased peak and plateau pressures
 Localized increased lucency with absent lung markings on chest radiograph
Localized increased lucency with absent lung markings on chest radiograph
 Rationale: Early detection of pneumothorax is essential to minimize progression to cardiac tamponade and death. Tension pneumothorax requires immediate emergency decompression with a large-bore needle (i.e., 14-gauge) into the second intercostal space, midclavicular line on the affected side, or immediate chest tube placement (see Procedure 20).
Rationale: Early detection of pneumothorax is essential to minimize progression to cardiac tamponade and death. Tension pneumothorax requires immediate emergency decompression with a large-bore needle (i.e., 14-gauge) into the second intercostal space, midclavicular line on the affected side, or immediate chest tube placement (see Procedure 20).
• Assess for signs of volume-pressure trauma that are consistent with ARDS:
 Acute, increasing, or severe dyspnea
Acute, increasing, or severe dyspnea
 Generalized crackles, especially in the dependent portions of the lung
Generalized crackles, especially in the dependent portions of the lung
 Increased peak and plateau pressures
Increased peak and plateau pressures
 Bilateral diffuse whiteout with chest radiograph
Bilateral diffuse whiteout with chest radiograph
 PaO2:fraction of inspired oxygen (FiO2) [P:F ratio] of less than 200
PaO2:fraction of inspired oxygen (FiO2) [P:F ratio] of less than 200
 Rationale: Volume-pressure trauma is assumed if the patient has the last three criteria noted. Ventilatory management should focus on ensuring that lung protective strategies are in place so that additional injury does not ensue. Some examples include Vt of 6 mL/kg and lung recruitment with PEEP. In general, these strategies result in hypercarbia because ventilation is not efficient.
Rationale: Volume-pressure trauma is assumed if the patient has the last three criteria noted. Ventilatory management should focus on ensuring that lung protective strategies are in place so that additional injury does not ensue. Some examples include Vt of 6 mL/kg and lung recruitment with PEEP. In general, these strategies result in hypercarbia because ventilation is not efficient.
• Assess for signs of cardiovascular depression (particularly after an increase in Vt, PEEP, or continuous positive airway pressure [CPAP] or with other hyperinflation maneuvers):
 Acute or gradual decrease in arterial blood pressure
Acute or gradual decrease in arterial blood pressure
 Tachycardia, bradycardia, or dysrhythmias
Tachycardia, bradycardia, or dysrhythmias
 Weak peripheral pulses, pulsus paradoxus, or decreased pulse pressure
Weak peripheral pulses, pulsus paradoxus, or decreased pulse pressure
 Acute or gradual increase in pulmonary capillary wedge pressure
Acute or gradual increase in pulmonary capillary wedge pressure
 Rationale: PPV can cause decreased venous return and afterload because of the increase in intrathoracic pressure. This mechanism often manifests immediately after initiation of mechanical ventilation and with large Vt, increases in PEEP or CPAP levels, and manual hyperinflation techniques. Cardiovascular depression associated with manual or periodic ventilator hyperinflation is immediately reversible with cessation of hyperinflation. Decreases in blood pressure with PPV also may be seen with hypovolemia.
Rationale: PPV can cause decreased venous return and afterload because of the increase in intrathoracic pressure. This mechanism often manifests immediately after initiation of mechanical ventilation and with large Vt, increases in PEEP or CPAP levels, and manual hyperinflation techniques. Cardiovascular depression associated with manual or periodic ventilator hyperinflation is immediately reversible with cessation of hyperinflation. Decreases in blood pressure with PPV also may be seen with hypovolemia.
• Assess for signs and symptoms of inadvertent extubation:
 Inability to deliver preset pressure
Inability to deliver preset pressure
 Decreased or absent breath sounds
Decreased or absent breath sounds
 Changes in endotracheal tube (ETT) depth
Changes in endotracheal tube (ETT) depth
 Signs and symptoms of inadequate ventilation, oxygenation, and breathing pattern
Signs and symptoms of inadequate ventilation, oxygenation, and breathing pattern
 Rationale: Inadvertent extubation is sometimes obvious (e.g., the endotracheal tube is in the patient’s hand). Often, the tip of the endotracheal tube is in the hypopharynx or in the esophagus, however, and inadvertent extubation may not be immediately apparent. Reintubation may be necessary, although some patients may not need reintubation. If reintubation is necessary, ventilation and oxygenation are assisted with a manual self-inflating resuscitation bag-valve device and face mask.
Rationale: Inadvertent extubation is sometimes obvious (e.g., the endotracheal tube is in the patient’s hand). Often, the tip of the endotracheal tube is in the hypopharynx or in the esophagus, however, and inadvertent extubation may not be immediately apparent. Reintubation may be necessary, although some patients may not need reintubation. If reintubation is necessary, ventilation and oxygenation are assisted with a manual self-inflating resuscitation bag-valve device and face mask.
• Assess for signs and symptoms of a malpositioned endotracheal tube:
 Unilateral decreased or absent breath sounds
Unilateral decreased or absent breath sounds
 Unilateral dullness to percussion
Unilateral dullness to percussion
 Rationale: Early detection and correction of a malpositioned endotracheal tube can prevent inadvertent extubation, atelectasis, barotrauma, and problems with gas exchange.
Rationale: Early detection and correction of a malpositioned endotracheal tube can prevent inadvertent extubation, atelectasis, barotrauma, and problems with gas exchange.
• Evaluate the patient’s need for long-term mechanical ventilation.  Rationale: This evaluation allows the nurse to anticipate patient and family needs for the patient’s discharge to an extended care facility, rehabilitation center, or home on PPV.
Rationale: This evaluation allows the nurse to anticipate patient and family needs for the patient’s discharge to an extended care facility, rehabilitation center, or home on PPV.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Perform a pre-procedure verification and time out, if non-emergent.  Rationale: Ensures patient safety.
Rationale: Ensures patient safety.
• Ensure that the patient understands preprocedural teachings. Answer questions as they arise, and reinforce information as needed.  Rationale: This communication evaluates and reinforces understanding of previously taught information.
Rationale: This communication evaluates and reinforces understanding of previously taught information.
• Premedicate as needed.  Rationale: Administration of sedatives, narcotics, or muscle relaxants may be necessary to provide adequate oxygenation and ventilation in some patients.
Rationale: Administration of sedatives, narcotics, or muscle relaxants may be necessary to provide adequate oxygenation and ventilation in some patients.
• Ensure patient is positioned properly for optimum ventilation.  Rationale: Placement of the patient in a head of bed elevation of at least 30 degrees enhances diaphragmatic excursion, decreases intrathoracic pressure and helps prevent aspiration and VAP.
Rationale: Placement of the patient in a head of bed elevation of at least 30 degrees enhances diaphragmatic excursion, decreases intrathoracic pressure and helps prevent aspiration and VAP.
References
![]() 1. Abraham, E, Yoshira, G. Cardiorespiratory effects of pressure controlled ventilation in severe respiratory failure. Chest. 1990; 98:1445–1449.
1. Abraham, E, Yoshira, G. Cardiorespiratory effects of pressure controlled ventilation in severe respiratory failure. Chest. 1990; 98:1445–1449.
![]() 2. Amato, MBP, et al, Volume-assured, pressure support ventilation (VAPSV). a new approach for reducing muscle workload during acute respiratory failure. Chest 1992; 102:1225–1234.
2. Amato, MBP, et al, Volume-assured, pressure support ventilation (VAPSV). a new approach for reducing muscle workload during acute respiratory failure. Chest 1992; 102:1225–1234.
![]() 3. Amato, MBP, et al. Beneficial effects of the “open lung approach” with low distending pressures in acute respiratory distress syndrome. Am J Respir Crit Care Med. 1995; 152:1835–1846.
3. Amato, MBP, et al. Beneficial effects of the “open lung approach” with low distending pressures in acute respiratory distress syndrome. Am J Respir Crit Care Med. 1995; 152:1835–1846.
![]() 4. Amato, MBP, Barbas, CSV, Medeiros, DM, et al, Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med 1998; 338 :347–354.
4. Amato, MBP, Barbas, CSV, Medeiros, DM, et al, Effect of a protective-ventilation strategy on mortality in the acute respiratory distress syndrome. N Engl J Med 1998; 338 :347–354.
5. American Association of Critical-Care Nurses, AACN practice alert. ventilator-associated pneumonia. www.aacn.org/WD/Practice/Docs/Ventilator_Associated_Pneumonia_1-2008.pdf, 2004 [retrieved from accessed 9/15/09].
6. American Thoracic Society and the Infectious Diseases Society of America. Guidelines for the management of adults with hospital acquired, ventilator-associated and healthcare associated pneumonia. Am Rev Respir Crit Care Med. 2005; 171:388–416.
![]() 7. Banner, MJ, Blanch, PB, Kirby, RR. Imposed work of breathing and methods of triggering a demand-flow continuous positive airway system. Crit Care Med. 1993; 21:183–190.
7. Banner, MJ, Blanch, PB, Kirby, RR. Imposed work of breathing and methods of triggering a demand-flow continuous positive airway system. Crit Care Med. 1993; 21:183–190.
![]() 8. Bellemare, F, Grassino, A. Evaluation of human diaphragm fatigue. J Appl Physiol. 1982; 53:1196–1206.
8. Bellemare, F, Grassino, A. Evaluation of human diaphragm fatigue. J Appl Physiol. 1982; 53:1196–1206.
![]() 9. Bidani, A, et al. Permissive hypercapnia in acute respiratory failure. JAMA. 1994; 272:957–962.
9. Bidani, A, et al. Permissive hypercapnia in acute respiratory failure. JAMA. 1994; 272:957–962.
![]() 10. Bonten, MJ, Kollef, MH, Hall, JB, Risk factors for ventilator-associated pneumonia. from epidemiology to patient management. Clin Infect Dis 2004; 38:1141–1149.
10. Bonten, MJ, Kollef, MH, Hall, JB, Risk factors for ventilator-associated pneumonia. from epidemiology to patient management. Clin Infect Dis 2004; 38:1141–1149.
![]() 11. Boots, RJ, et al. Clinical utility of hygroscopic heat and moisture exchanges in intensive care patients. Crit Care Med. 1997; 25:1707–1712.
11. Boots, RJ, et al. Clinical utility of hygroscopic heat and moisture exchanges in intensive care patients. Crit Care Med. 1997; 25:1707–1712.
12. Bosma, K, Ferreyra, G, Ambrogio, C, et al, Patient-ventilator interaction and sleep in mechanicalliy ventilated patients. pressure support versus proportional assist ventilation. Crit Care Med 2007; 35:1048–1054.
![]() 13. Brochard, L, et al. Inspiratory pressure support prevents diaphragmatic fatigue during weaning from mechanical ventilation. Am Rev Respir Dis. 1989; 139:513–521.
13. Brochard, L, et al. Inspiratory pressure support prevents diaphragmatic fatigue during weaning from mechanical ventilation. Am Rev Respir Dis. 1989; 139:513–521.
![]() 14. Brochard, L, Pluskwa, F, Lemaire, R. Improved efficacy of spontaneous breathing with inspiratory pressure support. Am Rev Respir Dis. 1987; 136:411–415.
14. Brochard, L, Pluskwa, F, Lemaire, R. Improved efficacy of spontaneous breathing with inspiratory pressure support. Am Rev Respir Dis. 1987; 136:411–415.
15. Burns, SM, Ventilating patients with acute severe asthma. what do we really know. AACN Adv Crit Care 2006; 17:188–193.
16. Burns, SM, Prevention of aspiration pneumonia in the enterally fed critically ill ventilated patient. keeping the head up takes a village. Pract Gastroenterol 2007; 31:63–72.
17. Burns, SM, Pressure modes of mechanical ventilation . the good, the bad and the ugly. AACN Adv Crit Care 2008; 19:399–411.
![]() 18. Calzia, E, Lindner, KH, Witt, S, et al. Pressure time product and work of breathing during biphasic continuous positive airway pressure and assisted spontaneous breathing. Am J Respir Crit Care Med. 1994; 150:904–910.
18. Calzia, E, Lindner, KH, Witt, S, et al. Pressure time product and work of breathing during biphasic continuous positive airway pressure and assisted spontaneous breathing. Am J Respir Crit Care Med. 1994; 150:904–910.
![]() 19. Cane, RD, Peruzzi, WT, Shapiro, BA. Airway pressure release ventilation in severe acute respiratory failure. Chest. 1991; 100:460–463.
19. Cane, RD, Peruzzi, WT, Shapiro, BA. Airway pressure release ventilation in severe acute respiratory failure. Chest. 1991; 100:460–463.
![]() 20. Cohen, CA, et al. Clinical manifestations of inspiratory muscle fatigue. Am J Med. 1982; 73:308–316.
20. Cohen, CA, et al. Clinical manifestations of inspiratory muscle fatigue. Am J Med. 1982; 73:308–316.
![]() 21. Cole, AGH, Weller, SF, Sykes, MK. Inverse ratio ventilation compared with PEEP in adult respiratory failure. Intensive Care Med. 1984; 10:227–232.
21. Cole, AGH, Weller, SF, Sykes, MK. Inverse ratio ventilation compared with PEEP in adult respiratory failure. Intensive Care Med. 1984; 10:227–232.
![]() 22. Craven, DE, Kunches, LM, Kilinsky, V, et al. Risk factors for pneumonia and fatality in patients receiving continuous mechanical ventilation. Am Rev Respir Dis. 1986; 133:792–796.
22. Craven, DE, Kunches, LM, Kilinsky, V, et al. Risk factors for pneumonia and fatality in patients receiving continuous mechanical ventilation. Am Rev Respir Dis. 1986; 133:792–796.
![]() 23. Davis, WB, et al, Pulmonary oxygen toxicity. early reversible changes in human alveolar structures induced by hyperoxia. N Engl J Med 1983; 309:878–883.
23. Davis, WB, et al, Pulmonary oxygen toxicity. early reversible changes in human alveolar structures induced by hyperoxia. N Engl J Med 1983; 309:878–883.
![]() 24. Derak, S, et al, and the Multicenter Oscillatory Ventilation for Acute Respiratory Distress Syndrome Trial (MOAT) Study Investigators. High-frequency oscillatory ventilation for acute respiratory distress syndrome in adultsa randomized controlled trial. Am J Respir Crit Care Med 2002; 166:801–808.
24. Derak, S, et al, and the Multicenter Oscillatory Ventilation for Acute Respiratory Distress Syndrome Trial (MOAT) Study Investigators. High-frequency oscillatory ventilation for acute respiratory distress syndrome in adultsa randomized controlled trial. Am J Respir Crit Care Med 2002; 166:801–808.
![]() 25. Djedaini, K, et al. Changing heat and moisture exchanges every 48 hours rather than 24 hours does not alter their efficacy and the incidence of nosocomial pneumonia. Am J Respir Crit Care Med. 1995; 152:1562–1569.
25. Djedaini, K, et al. Changing heat and moisture exchanges every 48 hours rather than 24 hours does not alter their efficacy and the incidence of nosocomial pneumonia. Am J Respir Crit Care Med. 1995; 152:1562–1569.
![]() 26. Dodek, P, Keenan, S, Cook, D, et al, for the Canadian Critical Care Trials Group and the Canadian Critical Care Society. Evidence-Based Clinical Practice Guidelines for the Prevention of Ventilator-Associated Pneumonia. Ann Intern Med 2004; 141:305–313.
26. Dodek, P, Keenan, S, Cook, D, et al, for the Canadian Critical Care Trials Group and the Canadian Critical Care Society. Evidence-Based Clinical Practice Guidelines for the Prevention of Ventilator-Associated Pneumonia. Ann Intern Med 2004; 141:305–313.
![]() 27. Downs, JB, Stock, MC, Airway pressure release ventilation. a new concept of ventilatory support. Crit Care Med 1987; 15:459–461.
27. Downs, JB, Stock, MC, Airway pressure release ventilation. a new concept of ventilatory support. Crit Care Med 1987; 15:459–461.
![]() 28. Dreyfuss, D, et al, High inflation pressure pulmonary edema. respective effects of high airway pressure, high Vt, and positive end-expiratory pressure. Am Rev Respir Dis 1988; 137:1159–1164.
28. Dreyfuss, D, et al, High inflation pressure pulmonary edema. respective effects of high airway pressure, high Vt, and positive end-expiratory pressure. Am Rev Respir Dis 1988; 137:1159–1164.
![]() 29. Dreyfuss, D, Saumon, G. The role of Vt, FRC, and end-inspiratory volume in the development of pulmonary edema following mechanical ventilation. Am Rev Respir Dis. 1993; 148:1194–1203.
29. Dreyfuss, D, Saumon, G. The role of Vt, FRC, and end-inspiratory volume in the development of pulmonary edema following mechanical ventilation. Am Rev Respir Dis. 1993; 148:1194–1203.
![]() 30. Elsasser, S, Guttmann, J, Stocker, R, et al. Accuracy of automatic tube compensation in new-generation mechanical ventilators. Crit Care Med. 2003; 31:2619–2626.
30. Elsasser, S, Guttmann, J, Stocker, R, et al. Accuracy of automatic tube compensation in new-generation mechanical ventilators. Crit Care Med. 2003; 31:2619–2626.
![]() 31. Esteban, A, Alia, I, Ibanez, J, et al. Modes of mechanical ventilation and weaning a national survey of Spanish hospital. Chest. 1994; 106:1188–1193.
31. Esteban, A, Alia, I, Ibanez, J, et al. Modes of mechanical ventilation and weaning a national survey of Spanish hospital. Chest. 1994; 106:1188–1193.
![]() 32. Fagon, J, Chastre, J, Vuagnat, A, et al. Nosocomial pneumonia and mortality among patients in intensive care units. JAMA. 1996; 275:866–869.
32. Fagon, J, Chastre, J, Vuagnat, A, et al. Nosocomial pneumonia and mortality among patients in intensive care units. JAMA. 1996; 275:866–869.
![]() 33. Fiastro, JF, Habib, MP, Quan, SF. Pressure support compensation for respiratory work due to endotracheal tubes and demand continuous positive airway pressure. Chest. 1998; 93:499–505.
33. Fiastro, JF, Habib, MP, Quan, SF. Pressure support compensation for respiratory work due to endotracheal tubes and demand continuous positive airway pressure. Chest. 1998; 93:499–505.
![]() 34. Fisher, AB, Oxygen therapy. side effects and toxicity. Am Rev Respir Dis 1980; 122:61–69.
34. Fisher, AB, Oxygen therapy. side effects and toxicity. Am Rev Respir Dis 1980; 122:61–69.
![]() 35. Frawley, PM, Habashi, N, Airway pressure release ventilation. theory and practice. AACN Clin Issues 2001; 12:234–246.
35. Frawley, PM, Habashi, N, Airway pressure release ventilation. theory and practice. AACN Clin Issues 2001; 12:234–246.
![]() 36. Frawley, PM, Habashi, NM, Airway pressure release ventilation and pediatrics. theory and practice. Crit Care Nurs Clin North Am 2004; 16:337–348.
36. Frawley, PM, Habashi, NM, Airway pressure release ventilation and pediatrics. theory and practice. Crit Care Nurs Clin North Am 2004; 16:337–348.
![]() 37. Fu, Z, et al. High lung volume increases stress failure in pulmonary capillaries. J Appl Physiol. 1992; 73:123–133.
37. Fu, Z, et al. High lung volume increases stress failure in pulmonary capillaries. J Appl Physiol. 1992; 73:123–133.
![]() 38. Garner, W, Downs, JB, Stock, MC, et al, Airway pressure release ventilation (APRV). a human trial. Chest 1998; 94:779–781.
38. Garner, W, Downs, JB, Stock, MC, et al, Airway pressure release ventilation (APRV). a human trial. Chest 1998; 94:779–781.
![]() 39. Giannouli, E, Webster, K, Roberts, D, et al. Response of ventilator-dependent patients to different levels of pressure support and proportional assist. Am J Respir Crit Care Med. 1999; 159:1716–1725.
39. Giannouli, E, Webster, K, Roberts, D, et al. Response of ventilator-dependent patients to different levels of pressure support and proportional assist. Am J Respir Crit Care Med. 1999; 159:1716–1725.
![]() 40. Gurevich, MJ, Van Dyke J, Young, ES, et al, Improved oxygenation and lower peak airway pressure in serve adult respiratory distress syndrome. treatment with inverse ratio ventilation. Chest 1986; 89:211–213.
40. Gurevich, MJ, Van Dyke J, Young, ES, et al, Improved oxygenation and lower peak airway pressure in serve adult respiratory distress syndrome. treatment with inverse ratio ventilation. Chest 1986; 89:211–213.
41. Habashi, NM, Other approaches to open-lung ventilation. airway pressure release ventilation. Crit Care Med 2005; 33:S228–S240.
![]() 42. Hickling, KG, et al, Low mortality rate in acute respiratory distress syndrome using low volume, pressure limited ventilation with permissive hypercapnia. a prospective study. Crit Care Med 1994; 22:1568–1578.
42. Hickling, KG, et al, Low mortality rate in acute respiratory distress syndrome using low volume, pressure limited ventilation with permissive hypercapnia. a prospective study. Crit Care Med 1994; 22:1568–1578.
![]() 43. Hilbert, G, et al. Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever and acute respiratory failure. N Engl J Med. 2001; 344:481–487.
43. Hilbert, G, et al. Noninvasive ventilation in immunosuppressed patients with pulmonary infiltrates, fever and acute respiratory failure. N Engl J Med. 2001; 344:481–487.
![]() 44. Holm, BA, et al. Pulmonary physiological and surfactant changes during injury and recovery from hyperoxia. J Appl Physiol. 1985; 59:1402–1409.
44. Holm, BA, et al. Pulmonary physiological and surfactant changes during injury and recovery from hyperoxia. J Appl Physiol. 1985; 59:1402–1409.
![]() 45. Hospital Infections Program, National Center for Infectious Diseases, CDC, Public health focus. surveillance, prevention and control of nosocomial pneumonia. MMWR 1992; 41:783–787.
45. Hospital Infections Program, National Center for Infectious Diseases, CDC, Public health focus. surveillance, prevention and control of nosocomial pneumonia. MMWR 1992; 41:783–787.
![]() 46. Ibanez, J, Penafiel, A, Raurich, JM, et al, Gastroesophageal reflux in intubated patients receiving enteral nutrition . effect of supine and semi-recumbent positions. J Parenter Enteral Nutr 1992; 16:419–422.
46. Ibanez, J, Penafiel, A, Raurich, JM, et al, Gastroesophageal reflux in intubated patients receiving enteral nutrition . effect of supine and semi-recumbent positions. J Parenter Enteral Nutr 1992; 16:419–422.
![]() 47. Iotti, GA, et al. Unfavorable mechanical effects of heat and moisture exchangers in ventilated patients. Intensive Care Med. 1997; 23:399–405.
47. Iotti, GA, et al. Unfavorable mechanical effects of heat and moisture exchangers in ventilated patients. Intensive Care Med. 1997; 23:399–405.
![]() 48. Johnson, PA, Raper, RF, Fisher, M. The impact of heat and moisture exchanging humidifiers on work of breathing. Anaesth Intensive Care. 1995; 23:697–701.
48. Johnson, PA, Raper, RF, Fisher, M. The impact of heat and moisture exchanging humidifiers on work of breathing. Anaesth Intensive Care. 1995; 23:697–701.
![]() 49. Kacmarek, RM, Hess, D, pressure-controlled inverse-ratio ventilation. panacea or auto-PEEP. Respiratory Care 1990; 35:945–948. [Editorial].
49. Kacmarek, RM, Hess, D, pressure-controlled inverse-ratio ventilation. panacea or auto-PEEP. Respiratory Care 1990; 35:945–948. [Editorial].
![]() 50. Kaplan, LJ, Bailey, H, Formosa, V. Airway pressure release ventilation increases cardiac performance in patients with acute lung injury/adult respiratory distress syndrome. Crit Care. 2001; 5:221–226.
50. Kaplan, LJ, Bailey, H, Formosa, V. Airway pressure release ventilation increases cardiac performance in patients with acute lung injury/adult respiratory distress syndrome. Crit Care. 2001; 5:221–226.
![]() 51. Kollef, M, Ventilator–associated pneumonia. a multivariate analysis. JAMA 1993; 270:1965–1970.
51. Kollef, M, Ventilator–associated pneumonia. a multivariate analysis. JAMA 1993; 270:1965–1970.
52. Kollef, MH, Shorr, A, Tabak, YP, et al, Epidemiology and outcomes of health-care-associated pneumonia. results from a large US database of a culture-positive pneumonia. Chest 2005; 128:3854–3862.
![]() 53. Lachman, B. Open up the lung and keep the lung open. Intensive Care Med. 1992; 18:319–321.
53. Lachman, B. Open up the lung and keep the lung open. Intensive Care Med. 1992; 18:319–321.
![]() 54. Leatherman, J, Ravenscraft, SA, Low measured auto-positive end expiratory pressure during mechanical ventilation of patients with severe asthma. hidden auto-positive end-expiratory pressure. Crit Care Med 1996; 24:541–546.
54. Leatherman, J, Ravenscraft, SA, Low measured auto-positive end expiratory pressure during mechanical ventilation of patients with severe asthma. hidden auto-positive end-expiratory pressure. Crit Care Med 1996; 24:541–546.
![]() 55. MacIntyre, NR. Respiratory function during pressure support ventilation. Chest. 1986; 89:677–683.
55. MacIntyre, NR. Respiratory function during pressure support ventilation. Chest. 1986; 89:677–683.
![]() 56. MacIntyre, NR. Effects of initial flow rate and breath termination criteria on pressure support ventilation. Chest. 1991; 99:134–138.
56. MacIntyre, NR. Effects of initial flow rate and breath termination criteria on pressure support ventilation. Chest. 1991; 99:134–138.
![]() 57. MacIntyre, NR. Ventilatory muscles and mechanical ventilatory support. Crit Care Med. 1997; 25:1106–1107.
57. MacIntyre, NR. Ventilatory muscles and mechanical ventilatory support. Crit Care Med. 1997; 25:1106–1107.
![]() 58. MacIntyre, NR, K-CG, Cheng, McConnell, R. Applied PEEP during pressure support reduces the inspiratory threshold load of intrinsic PEEP. Chest. 1997; 111:188–193.
58. MacIntyre, NR, K-CG, Cheng, McConnell, R. Applied PEEP during pressure support reduces the inspiratory threshold load of intrinsic PEEP. Chest. 1997; 111:188–193.
![]() 59. MacIntyre, NR. High-frequency ventilation. Crit Care Med. 1998; 26:1955–1956. [[editorial]].
59. MacIntyre, NR. High-frequency ventilation. Crit Care Med. 1998; 26:1955–1956. [[editorial]].
![]() 60. Manthous, CA, Schmidt, GA. Resistive pressure of a condenser humidifier in mechanically ventilated patients. Crit Care Med. 1994; 22:1792–1795.
60. Manthous, CA, Schmidt, GA. Resistive pressure of a condenser humidifier in mechanically ventilated patients. Crit Care Med. 1994; 22:1792–1795.
![]() 61. Marini, JJ, Rodriguez, M, Lamb, V. The inspiratory workload of patient-initiated mechanical ventilation. Am Rev Respir Dis. 1986; 134:902–909.
61. Marini, JJ, Rodriguez, M, Lamb, V. The inspiratory workload of patient-initiated mechanical ventilation. Am Rev Respir Dis. 1986; 134:902–909.
![]() 62. Marini, JJ, Smith, TC, Lamb, VJ, External work output and force generation during synchronized intermittent mechanical ventilation. effect of machine assistance on breath effort. Am Rev Respir Dis 1998; 138:1169–1179.
62. Marini, JJ, Smith, TC, Lamb, VJ, External work output and force generation during synchronized intermittent mechanical ventilation. effect of machine assistance on breath effort. Am Rev Respir Dis 1998; 138:1169–1179.
![]() 63. McEvoy, MT, Carey, TJ, Shivering and rewarming after cardiac surgery. comparison of ventilator circuits with humidifier and heated wires to heat and moisture exchangers. Am J Crit Care 1995; 4:293–299.
63. McEvoy, MT, Carey, TJ, Shivering and rewarming after cardiac surgery. comparison of ventilator circuits with humidifier and heated wires to heat and moisture exchangers. Am J Crit Care 1995; 4:293–299.
![]() 64. Mehta, S, Hill, NS, State of the art. non-invasive ventilation. Am J Respir Crit Care Med 2001; 163:540–577.
64. Mehta, S, Hill, NS, State of the art. non-invasive ventilation. Am J Respir Crit Care Med 2001; 163:540–577.
65. Metheny, NA, Schallom, L, Oliver, DA, et al. Gastric residual volume and aspiration in crucially ill patens receiving gastric feedings. Am J Crit Care. 2008; 17:512–520.
![]() 66. Mols, G, von Ungern-Sternberg B, Rohr, E, et al, Respiratory comfort and breathing pattern during volume proportional assist ventilation and pressure support ventilation. a study on volunteers with artificially reduced compliance. Crit Care Med 2000; 28:1940–1946.
66. Mols, G, von Ungern-Sternberg B, Rohr, E, et al, Respiratory comfort and breathing pattern during volume proportional assist ventilation and pressure support ventilation. a study on volunteers with artificially reduced compliance. Crit Care Med 2000; 28:1940–1946.
![]() 67. Nishimara, M, et al. Comparison of flow-resistive work load due to humidifying devices. Chest. 1990; 97:600–604.
67. Nishimara, M, et al. Comparison of flow-resistive work load due to humidifying devices. Chest. 1990; 97:600–604.
![]() 68. O’Kroy, JA, Coast, JR. Effects of flow and resistive training on respiratory muscle endurance and strength. Respiration. 1993; 60:279–283.
68. O’Kroy, JA, Coast, JR. Effects of flow and resistive training on respiratory muscle endurance and strength. Respiration. 1993; 60:279–283.
![]() 69. Orlando, R, ventilators. how clever, how complex. Crit Care Med 2003; 2704–2705. [Editorial].
69. Orlando, R, ventilators. how clever, how complex. Crit Care Med 2003; 2704–2705. [Editorial].
![]() 70. Parker, JC, Hernandez, LA, Peevy, KJ. Mechanisms of ventilator-induced lung injury. Crit Care Med. 1993; 21:131–143.
70. Parker, JC, Hernandez, LA, Peevy, KJ. Mechanisms of ventilator-induced lung injury. Crit Care Med. 1993; 21:131–143.
![]() 71. Pepe, PE, Marini, JJ. Occult positive end-expiratory pressure in mechanically ventilated patients with airflow obstruction. Am Rev Respir Dis. 1994; 126:166–173.
71. Pepe, PE, Marini, JJ. Occult positive end-expiratory pressure in mechanically ventilated patients with airflow obstruction. Am Rev Respir Dis. 1994; 126:166–173.
![]() 72. Peter, JV, et al, Noninvasive ventilation in acute respiratory failure. a meta analysis update. Crit Care Med 2002; 30:555–562.
72. Peter, JV, et al, Noninvasive ventilation in acute respiratory failure. a meta analysis update. Crit Care Med 2002; 30:555–562.
![]() 73. Putensen, C, et al. Long-term effects of spontaneous breathing during ventilatory support in patients with acute lung injury. Am J Respir Crit Care Med. 2001; 164:43–49.
73. Putensen, C, et al. Long-term effects of spontaneous breathing during ventilatory support in patients with acute lung injury. Am J Respir Crit Care Med. 2001; 164:43–49.
![]() 74. Ranieri, VM, et al. Effects of positive end-expiratory pressure on alveolar recruitment and gas exchange in patients with the adult respiratory distress syndrome. Am Rev Respir Dis. 1991; 144:544–551.
74. Ranieri, VM, et al. Effects of positive end-expiratory pressure on alveolar recruitment and gas exchange in patients with the adult respiratory distress syndrome. Am Rev Respir Dis. 1991; 144:544–551.
![]() 75. Rathgeber, J, Schorn, B, Falk, V, et al, The influence of controlled mandatory ventilation (CMV), intermittent mandatory ventilation (IMV) and biphasic intermittent positive airway pressure (BIPAP) on duration of intubation and consumption of analgesics and sedatives. a prospective analysis in 596 patients following adult cardiac surgery. Eur J Anaesth 1997; 14:576–582.
75. Rathgeber, J, Schorn, B, Falk, V, et al, The influence of controlled mandatory ventilation (CMV), intermittent mandatory ventilation (IMV) and biphasic intermittent positive airway pressure (BIPAP) on duration of intubation and consumption of analgesics and sedatives. a prospective analysis in 596 patients following adult cardiac surgery. Eur J Anaesth 1997; 14:576–582.
76. Rose, L, High-frequency oscillatory ventilation in adults. clinical considerations and management priorities. AACN Adv Crit Care 2008; 19:412–420.
![]() 77. Sassoon, CSH, et al. Inspiratory muscle work of breathing during flow-by, demand-flow and continuous-flow systems in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis. 1993; 143:860–866.
77. Sassoon, CSH, et al. Inspiratory muscle work of breathing during flow-by, demand-flow and continuous-flow systems in patients with chronic obstructive pulmonary disease. Am Rev Respir Dis. 1993; 143:860–866.
78. Shorr, AF, Kollef, MH, Ventilator-associated pneumonia . insights from recent clinical trials. Chest 2005; 128:583–591.
![]() 79. Slutsky, AS, Consensus Conference on Mechanical Ventilation, January 28-30, 1993. at Northbrook, IL, USA. parts 1 and 2. Intensive Care Med 1994; 20:64–79. [150-62].
79. Slutsky, AS, Consensus Conference on Mechanical Ventilation, January 28-30, 1993. at Northbrook, IL, USA. parts 1 and 2. Intensive Care Med 1994; 20:64–79. [150-62].
![]() 80. Staudinger, T, Kordova, H, Roggla, M, et al. Comparison of oxygen cost of breathing with pressure support ventilation and biphasic intermittent positive airway pressure ventilation. Crit Care Med. 1998; 26:1518–1522.
80. Staudinger, T, Kordova, H, Roggla, M, et al. Comparison of oxygen cost of breathing with pressure support ventilation and biphasic intermittent positive airway pressure ventilation. Crit Care Med. 1998; 26:1518–1522.
![]() 81. Stock, M, Downs, JB, Airway pressure release ventilation. a new approach to ventilatory support during acute lung injury. Respir Care 1987; 32:517–524.
81. Stock, M, Downs, JB, Airway pressure release ventilation. a new approach to ventilatory support during acute lung injury. Respir Care 1987; 32:517–524.
![]() 82. Sulzer, CF, Chiolero, R, Chassot, PG, et al, Adaptive support ventilation for fast tracheal extubation after cardiac surgery. a randomized controlled study. Anesthesiology 2001; 95:1339–1345.
82. Sulzer, CF, Chiolero, R, Chassot, PG, et al, Adaptive support ventilation for fast tracheal extubation after cardiac surgery. a randomized controlled study. Anesthesiology 2001; 95:1339–1345.
![]() 83. Tablan, OC, Anderson, LJ, Besser, R, et al, Guidelines for preventing health-care–associated pneumonia, recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee March 26, 2004. www.cdc.gov/mmwr/preview/mmwrhtml/rr5303a1.htm . MMWR. 2004; 53(RR03):1–36. [Available at].
83. Tablan, OC, Anderson, LJ, Besser, R, et al, Guidelines for preventing health-care–associated pneumonia, recommendations of CDC and the Healthcare Infection Control Practices Advisory Committee March 26, 2004. www.cdc.gov/mmwr/preview/mmwrhtml/rr5303a1.htm . MMWR. 2004; 53(RR03):1–36. [Available at].
![]() 84. Tassaux, D, Dalmas, E, Gratadour, P, et al, Patient-ventilator interactions during partial ventilatory support. a preliminary study comparing the effects of adaptive support ventilation with synchronized intermittent mandatory ventilation plus inspiratory pressure support. Crit Care Med 2002; 30:801–807.
84. Tassaux, D, Dalmas, E, Gratadour, P, et al, Patient-ventilator interactions during partial ventilatory support. a preliminary study comparing the effects of adaptive support ventilation with synchronized intermittent mandatory ventilation plus inspiratory pressure support. Crit Care Med 2002; 30:801–807.
![]() 85. Tharratt, RS, Allen, RP, Albertson, TE. Pressure controlled inverse ratio ventilation in severe adult respiratory failure. Chest. 1998; 94:755–762.
85. Tharratt, RS, Allen, RP, Albertson, TE. Pressure controlled inverse ratio ventilation in severe adult respiratory failure. Chest. 1998; 94:755–762.
![]() 86. The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000; 342:1301–1307.
86. The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000; 342:1301–1307.
![]() 87. Tobin, MJ, et al. Konno-Mead analysis of ribcage-abdominal motion during successful and unsuccessful trials of weaning from mechanical ventilation. Am Rev Respir Dis. 1987; 135:1320–1328.
87. Tobin, MJ, et al. Konno-Mead analysis of ribcage-abdominal motion during successful and unsuccessful trials of weaning from mechanical ventilation. Am Rev Respir Dis. 1987; 135:1320–1328.
![]() 88. Unal, N, et al. A novel method of evaluation of three heat-moisture exchangers in six different ventilator settings. Intensive Care Med. 1998; 24:138–146.
88. Unal, N, et al. A novel method of evaluation of three heat-moisture exchangers in six different ventilator settings. Intensive Care Med. 1998; 24:138–146.
89. Unoki, T, Serita, A, Grap, MJ. Automatic tube compensation during weaning form mechanical ventilation; evidence and clinical implications. Crit Care Nurse. 2008; 28:34–42.
90. Varelmann, D, Wrigge, H, Zinserling, J, et al, Proportional assist versus pressure support ventilation in patients with acute respiratory failure. cardiorespiratory responses to artificially increased ventilatory demand. Crit Care Med 2005; 33:1968–1975.
![]() 91. Vincent, JL, Bihari DJ. Suter PM, et al. The prevalence of nosocomial pneumonia in intensive care units in Europe (EPIC). JAMA. 1995; 274:639–644.
91. Vincent, JL, Bihari DJ. Suter PM, et al. The prevalence of nosocomial pneumonia in intensive care units in Europe (EPIC). JAMA. 1995; 274:639–644.
![]() 92. Vittacca, M, Bianchi, L, Zanotti, E, et al. Assessment of physiologic variables and subjective comfort under different levels of pressure support ventilation. Chest. 2004; 126:851–859.
92. Vittacca, M, Bianchi, L, Zanotti, E, et al. Assessment of physiologic variables and subjective comfort under different levels of pressure support ventilation. Chest. 2004; 126:851–859.
![]() 93. West, JB, et al. Stress fracture in pulmonary capillaries. J Appl Physiol. 1991; 70:1731–1742.
93. West, JB, et al. Stress fracture in pulmonary capillaries. J Appl Physiol. 1991; 70:1731–1742.
Burns, S. Mechanical ventilation and weaning. In: Carlson KK, ed. AACN advanced critical care nursing. St Louis: Elsevier, 2009.
Pierce, LNB. Invasive and noninvasive modes and methods of mechanical ventilation. In Burns S, ed. : AACN protocols for practice: care of mechanically ventilated patients, ed 2, Boston: Jones and Bartlett, 2007.
Pierce, LNB, Management of the mechanically ventilated patient. ed 2. Elsevier, St Louis, 2007.
Tobin, MJ. Principles and practice of mechanical ventilation, ed 2. New York: McGraw-Hill, 2006.
West, JB Respiratory physiology. the essentials. ed 8. Lippincott Williams & Wilkins, Baltimore, 2008.
West, JB Pulmonary pathophysiology. the essentials. Lippincott Williams & Wilkins, Baltimore, 2008.
Selected Manufacturers’ Websites
Avea. www.viasyshealthcare.com/prod_serv/downloads/284_Avea_Comp_Spec_Sheet.pdf, September 15, 2009 [retrieved, from].
Drager. www.draeger.com/MT/internet/pdf/CareAreas/CriticalCare/-cc_evita_atcpps_br_en.pdf, September 15, 2009. www.draeger.com/MT/internet/pdf/CareAreas/-CriticalCare/cc_bipap_book_en.pdf [retrieved from].
Hamilton, Medical. www.hamilton-medical.com/GALILEO-ventilators.37.0.html, November 17, 2008 retrieved from. www.med1online.com/documents/Hamilton_Products_Galileo_Classic_Specs.pdf, January 2, 2008 [retrieved from].
Maquet. www.maquet.com/productPage.aspx?m1=112599774495&m2=112808545902&m3=105584076919&productGroupID=112808545902&productConfigID=105584076919&languageID=1&titleCountryID=224, November 16, 2008 [retrieved from].
Puritan, Bennett. www.puritanbennett.com/prod/Product.aspx?S1=VEN&S2=&id=289., November 16, 2008 [retrieved from].