CHAPTER 34 Trauma and Posttraumatic Stress Disorder
DIAGNOSIS
Etiology
The diagnosis of PTSD is unique among psychiatric disorders in that the diagnostic criteria contain the presence of a presumptive etiology (i.e., a traumatic event), in addition to the more typical symptom constellation (Table 34-1). The current DSM-IV criteria require that the traumatic event (criterion A) be defined by two elements: the individual must have experienced, witnessed, or learned about an event that involved actual or threatened death or serious injury (A1); and the individual’s response to this experience must involve intense fear, helplessness, or horror (A2).
Table 34-1 DSM-IV Diagnostic Criteria for Posttraumatic Stress Disorder (309.81)
As previously noted, the DSM-IV stressor criterion significantly broadens the concept of a traumatic stressor from earlier versions of the DSM (that had conceptualized trauma as involving an event that is “outside the range of usual human experience”) (DSM-III-R). Thus, more common experiences (such as learning about an unexpected death or injury of a friend or family member) can be conceptualized as trauma by DSM-IV standards. The DSM-IV change in stressor definition (i.e., A1) may have increased the number of stressors that qualify for inclusion by nearly 60%.1 The addition of the A2 subjective element of the stressor (e.g., the presence of intense fear, helplessness, or horror) has likely had only a modest impact, given that more than three-quarters of individuals exposed to trauma endorse this response (90% of those who fully meet PTSD symptom criteria B, C, and D report also experiencing the A2 subjective element at the time of traumatic exposure).1,2 The net effect of combining the more inclusive nature of the DSM-IV A1 criterion with the modestly limiting A2 criterion has been to produce an increase of over 20% in the total number of qualifying traumatic events compared to earlier versions of the DSM.
Clinical Features
The symptomatology of PTSD is conceptualized within the framework of three symptom clusters (see Table 34-1): reexperiencing (criterion B; one of a list of five symptoms is required), avoidance (criterion C; three of a list of seven symptoms are required), and arousal (criterion D; two of a list of five symptoms are required). Factor analytic studies have supported this symptom structure for PTSD. However, most studies have suggested that the avoidance cluster represents two independent factors: avoidance (criteria C1 to C3) and numbing (criteria C4 to C7), the latter being associated with a more pervasive disturbance.3,4 The most common symptoms reported by individuals in the aftermath of trauma include sleep disturbance, intrusive memories/nightmares, and avoidance of reminders. For trauma-exposed people, the re-experiencing criterion B is most frequently met (reported in 60% to 80% of trauma survivors), followed by the arousal criterion D (seen in 30% to 60% of people).5,6 The avoidance/numbing criterion C is the least frequently observed (10% to 50%) among trauma-exposed individuals.5,6 Thus, it is a critical determinant of PTSD. In a study of survivors of the Oklahoma City bombing, only one-third of exposed individuals met the avoidance/numbing criterion (compared with more than 80% who met re-experiencing and arousal criteria).7 Of those who endorsed avoidance/numbing, there was a 94% probability of eventually meeting the criteria for PTSD. Trauma-exposed men are generally less likely than are women to meet the avoidance/numbing criterion. Even among victims of assault, only 20% of men meet criterion C compared with 50% of women.5
Many individuals fail to meet criteria for PTSD due to a failure to meet criterion C (avoidance/numbing). The prevalence of “subthreshold” or “partial” PTSD (often defined as meeting two of the three symptom clusters and having at least one symptom from the third) is believed to be two to four times more common than is full PTSD.8 Moreover, individuals with subthreshold PTSD demonstrate considerable occupational and social impairment relative to trauma-exposed controls; in some cases they demonstrate impairment comparable to those with PTSD.9 Furthermore, subthreshold PTSD is more closely linked with suicidal ideation (comparable to full PTSD) even after controlling for the presence of depression.10
Acute Stress Disorder
The DSM-IV introduced a new diagnostic category, acute stress disorder (ASD), to recognize brief stress reactions to traumatic events that are manifest in the first month following a trauma. Criteria for ASD appear in Table 34-2. In addition to a shorter duration (2 days to 4 weeks), ASD has a less restrictive set of PTSD symptoms in each of the three cluster types (re-experiencing, avoidance, and arousal) plus the requirement of meeting 3 out of 5 dissociative symptoms. Derived from theory, ASD represents one of the few disorders in the DSM-IV without prior empirical validation. As a result, controversy exists as to whether the diagnostic criteria for ASD constitute an optimal or meaningful clinical picture for those who experience acute stress in the aftermath of trauma. In particular, its emphasis on dissociative symptoms has been questioned.
Table 34-2 DSM-IV Diagnostic Criteria for Acute Stress Disorder (308.3)
Empirical studies have suggested that the ASD symptom cluster occurs in 10% to 30% of individuals exposed to trauma.11 Prospective studies suggest that 72% to 83% of those diagnosed with ASD go on to develop PTSD at 6 months after the trauma, and 63% to 80% have PTSD at 2 years after the trauma.11 Although dissociation in the acute posttrauma phase has led to significant predictive power for PTSD, its role within ASD may nonetheless be overemphasized. When the dissociation criterion is removed from the ASD diagnosis, comparable rates of subsequent PTSD are observed, that is, 60% of patients with ASD (minus dissociation) are reported to have PTSD 6 months after the trauma, and 70% report symptoms of PTSD 2 years after the trauma.12,13 In a similar vein, the application of the standard PTSD diagnostic criteria, without the 1-month duration, in the first month following trauma has been as effective as the ASD diagnosis in predicting subsequent and persistent PTSD.14,15 Regardless, the clinical utility of the ASD diagnosis has been supported by studies that have examined early treatment in such individuals. Preliminary research has suggested that the employment of specific treatment approaches (e.g., exposure therapy, cognitive therapy, stress management) for ASD leads to lower rates of later PTSD (approximately 15% to 25% at 6 months after the trauma) relative to ASD patients who are either untreated or who receive general supportive counseling (approximately 60% to 70% have PTSD at 6 months).11 Despite evidence regarding the prevalence and utility of the diagnosis of ASD, unresolved issues remain, not only with regard to its emphasis on dissociative symptoms, but also as to whether ASD and PTSD may in fact represent the same disorder, the latter merely differentiated by an arbitrary month-long duration criterion. In other words, ASD may simply exemplify “acute PTSD” as defined in the earlier DSM-III.15
EPIDEMIOLOGY
Prevalence
While the lifetime prevalence of PTSD in the general community is 8% to 9%, the 12-month prevalence of PTSD is nearly 4% (with more than two-thirds of cases manifest by moderate to severe functional impairment).16–18 Women show a higher lifetime prevalence (10% to 14%) than do men (5% to 6%).19 In primary care settings, as many as 12% of patients meet criteria for either partial or full PTSD.20 In mental health treatment–seeking populations, the prevalence of PTSD may be as high as 40% to 50%, even among individuals being treated for other conditions and not seeking specialized trauma care.21
Exposure to potentially traumatizing events in the general population is the rule rather than the exception. In the National Comorbidity Survey (NCS), the lifetime prevalence of exposure to any traumatic event (based on DSM-III-R criteria) was 60% for men and 50% for women.17 The lifetime prevalence of exposure to any trauma increases to nearly 90% when the broader DSM-IV exposure criteria are employed.22 More than half of individuals with trauma exposure report exposure to more than one event.17 The median number of distinct traumatic events among individuals exposed to any trauma is nearly five.22
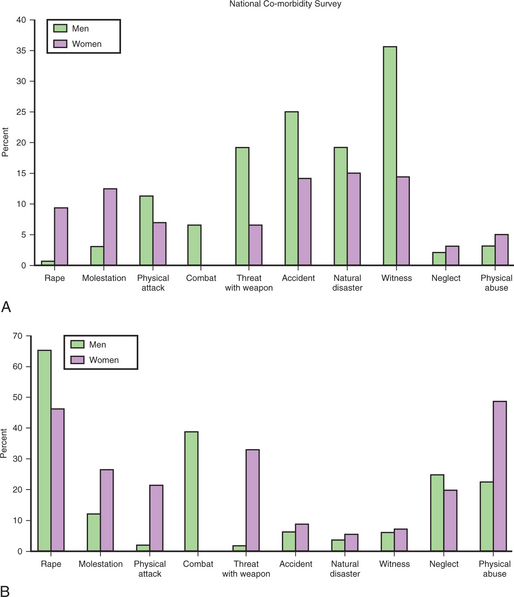
Events involving assaultive behavior (e.g., rape, military combat, kidnap/torture, physical assault, and molestation) are experienced by roughly 40% of the population, whereas other direct experiences of trauma (e.g., motor vehicle accidents, natural disasters, witnessing others being killed or injured, and being diagnosed with a life-threatening illness) have an estimated lifetime prevalence rate of 60%.22 Events that are only experienced indirectly (e.g., learning that a close friend or relative was assaulted or seriously injured) are reported by over 60% of the population. In fact, within this category, learning of the unexpected death of a close friend or relative is in itself associated with an exceedingly high lifetime prevalence (60%). The nature and type of trauma experienced by men and women differ considerably. NCS data for exposure to trauma are presented in Figure 34-1, A. Men more frequently report exposure to physical attacks, to combat, to being threatened with a weapon, to serious accidents, and to witnessing others being injured or killed.17 Men are twice as likely as women to be exposed to assaults, with nearly 35% being mugged or threatened with a weapon.22 Women more frequently report being raped, sexually molested, neglected as children, and physically abused. More than 40% of women have experienced interpersonal violence (including sexual violence and intimate partner violence).23 Exposure to all classes of trauma in both men and women peaks during late adolescence/early adulthood (ages 16 to 20).22 This is reflected in the median age of onset (23 years) for PTSD.24 Exposure to assaultive violence declines precipitously after this period, whereas all other classes of trauma exposure decline only modestly with advancing age, or not at all in the case of sudden unexpected death of a close friend or relative (an event that peaks in middle age). In general, the decline in all types of trauma following early adulthood appears to be steeper for women, suggesting that in women the risk of PTSD is especially pronounced during adolescence and early adulthood. The demographic variables of race, education, and income level do not appear to affect the risk of exposure to most types of trauma. The clear exception is assaultive violence, in which there is a twofold increase in exposure prevalence for nonwhites versus whites, for those with less education versus those with a college education, and for those with low incomes versus those with high incomes.22
Despite the high prevalence of traumatic exposure, the development of PTSD is the exception rather than the rule. The overall conditional probability of PTSD after a traumatic event is 9.2%.22 However, the risk of PTSD varies substantially with the type of trauma experienced. Assaultive violence in general demonstrates the highest probability (over 20%) of leading to PTSD whereas learning about traumatic events to others carries the lowest probability (2%).22 Figure 34-1, B, illustrates the conditional PTSD probabilities associated with specific types of trauma for both men and women based on results from the NCS. Specific traumatic events that carry the highest conditional probability for PTSD include rape (50% or greater), torture/kidnap (50%), combat (nearly 40%), and childhood physical abuse or sexual molestation (25% to 50%).17,22 Women exposed to trauma are in general more than twice as likely (13% to 20%) to develop PTSD than are men (6% to 8%).17,22 This general twofold increase in risk of PTSD in women is maintained after controlling for the distribution of trauma types. However, women’s increased vulnerability to PTSD does not appear to be equally generalizable to all types of trauma. Specifically, the increased risk of a woman developing PTSD occurs predominantly after an assault, in which women demonstrate a PTSD risk with a probability of 35% (versus 6% in men).5 A significant portion of this sex difference appears to be attributable to the greater likelihood that women relative to men will meet the avoidance/numbing symptoms (DSM-IV Criterion C) required for the diagnosis.
Nearly 40% of all cases of PTSD result from assaultive violence, which reflects the high conditional probability of PTSD associated with this type of trauma.22 For men, combat exposure alone accounts for a sizeable percentage, approximately 30%, of PTSD.25 For women, sexual violence accounts for nearly 25% of all PTSD cases, and being “badly beaten up” (including intimate partner violence) constitutes an additional 20% of all cases of PTSD reported by women.5 Surprisingly, learning of the sudden, unexpected death of a close relative or friend accounts for the second highest proportion of overall PTSD cases (greater than 30%), a finding that reflects the extremely high prevalence for this type of event (60%) despite only a moderate conditional probability for PTSD (14%).22 Only 7% of all PTSD cases are attributable to other events related to learning about trauma to others. Approximately 23% of all PTSD cases result from direct exposure to nonassaultive events (e.g., accidents, natural disasters, and witnessing death).
As a final note in considering the rates of PTSD described above, it is important to recognize the “fluid” nature of epidemiological data, that is, reported prevalence rates are estimates that are not written in stone. Epidemiological studies of PTSD have shown that multiple methodological factors can affect the reported prevalence and risk rates of PTSD. Different diagnostic instruments (e.g., the Diagnostic Interview Schedule [DIS] versus the Structured Clinical Interview for DSM [SCID]) and data-gathering procedures (e.g., telephone versus in-person interview) can produce widely disparate prevalence estimates in the same population. Revisions to the diagnostic criteria as the DSM evolves can substantially alter overall rates of estimated trauma exposure and PTSD. Methodological variations in the documentation of traumatic events or the validation of symptom status or functional impairment can also have a significant impact on estimates. A recent reexamination of the well-known National Vietnam Veterans Readjustment Study (NVVRS) illustrates this point.26 The NVVRS is often cited for its estimate of a lifetime PTSD prevalence of 30.9% in Vietnam veterans.27 Employing the same database, the re-examination study provided a more systematic military record documentation of trauma exposure, differentiated war-related from prewar symptom onset, and factored in distress levels and severity of social/occupational impairment. Based on such refinements, the overall lifetime prevalence of PTSD in Vietnam veterans was reduced to 18.7%, nearly a 40% change from the original estimate. It is not known to what degree other accepted epidemiological “facts” may be challenged by future refinements. Recognizing the mutable and evolving nature of prevalence and risk estimates for PTSD has important implications regarding the establishment of future public health policy, as well as our understanding of the significance of such constructs as resiliency and “normative” response to trauma.
Co-morbidity
Psychiatric co-morbidity is the rule rather than the exception in PTSD. The percentage of a lifetime history of other psychiatric disorders in individuals diagnosed with PTSD has been estimated by the NCS at nearly 90% in men and 80% in women. In fact, nearly 60% of men and 45% of women with PTSD report more than three co-morbid psychiatric conditions.17 Major depressive disorder (MDD) is among the most common of co-morbid conditions for both men and women (affecting nearly 50%). Alcohol abuse (in the majority) and conduct disorder (over 40%) are also highly co-morbid in men. Additionally, there is a threefold to sevenfold increased risk for both men and women with PTSD to be diagnosed with other anxiety disorders, including generalized anxiety disorder (GAD), panic disorder, and specific phobias. High levels of psychiatric co-morbidity in PTSD may result from the substantial symptom overlap between PTSD and disorders such as MDD (with a loss of interest, social withdrawal, insomnia, and poor concentration) and other anxiety disorders (manifest by hyperarousal and avoidance). NCS results suggest that more often than not, PTSD is primary with respect to co-morbid affective disorders and substance abuse disorders, but secondary with respect to co-morbid anxiety disorders (and for men, co-morbid conduct disorder).17 Most studies have failed to find an increased risk of MDD or drug abuse for trauma-exposed individuals who are not diagnosed with PTSD.19 The same has been found for alcohol abuse or dependence in males, but not females. This suggests that MDD and substance abuse (with the exception of alcohol abuse in women) are not likely to be psychiatric conditions that independently occur outside of PTSD in response to trauma; rather they appear more likely either to be the result of PTSD (i.e., an emotional response to impairment and “self-medication” through substance abuse) or to share antecedent genetic or environmental factors (i.e., with a shared liability for both PTSD and depression/substance abuse).
Risk Factors
An understanding of relevant risk factors for the development of PTSD is complicated by the fact that independent risks may exist for an increased exposure to traumatic events and to an increased susceptibility for the development of PTSD once exposed to traumatic events. Research into the genetics of PTSD illustrates this complexity. Combat and civilian twin studies have estimated the genetic heritability of exposure to trauma as between 20% and 50%.28,29 Furthermore, exposure to different types of trauma may be differentially mediated by genetic factors. The likelihood of exposure to traumatic events involving assaultive violence appears to be highly influenced by genetics, whereas event exposure involving nonassaultive trauma appears to be largely nongenetic.29 It has been proposed that one pathway underlying genetic predisposition to traumatic exposure may be mediated through heritable personality traits (e.g., neuroticism, antisocial behavior, extroversion, and sensation seeking) that increase the risk of experiencing a traumatic event. It has been reported, for example, that the likelihood of experiencing a violent assault is predicted by antisocial personality traits, as well as the more nonpathological personality style of “being open to new ideas and experiences,” with genetic factors accounting for upwards of 10% of the relationship between personality and trauma exposure.30
Once exposed to a traumatic event, the conditional risk of PTSD also appears to be substantially influenced by genetics. Both combat and civilian trauma twin studies estimate the genetic heritability of PTSD to be approximately 30% to 40% after controlling for trauma exposure.29,31 Genetic heritability appears to be comparable among the three symptom clusters (i.e., re-experiencing, avoidance/numbing, and arousal). It remains unclear as to whether genetic factors for risk of PTSD are different for men and women or for different trauma types. Some preliminary gene studies have identified specific dopamine- or serotonin-transporter linked polymorphic regions that may be linked to PTSD susceptibility.32,33 However, these findings have yet to be fully replicated.
Beyond genetics, factors that have been found to be predictive of a vulnerability to PTSD fall into two broad categories: pre-existing (characteristics present before trauma exposure) and peritraumatic (characteristics noted at the time of trauma or shortly thereafter). Many of the identified pre-event factors are not well understood (i.e., whether their impact is attributable to the likelihood of traumatic event exposure or to PTSD liability once exposed; in some cases they are implicated in both). Meta-analytic studies have identified several pretrauma factors (female gender, previous trauma exposure, a history of MDD or an anxiety disorder, a history of mental disorder in the family, an earlier age of traumatic exposure, and a social/educational/intellectual disadvantage) for an increased risk of PTSD.34,35
Previous trauma exposure (not resulting in PTSD) has been well established as a risk factor for PTSD after subsequent traumas. The impact of previous trauma is particularly significant when prior exposure involves assaultive violence or more than one previous traumatic event (assaultive or nonassaultive). A history of two or more traumatic events of assaultive violence in childhood has been shown to increase the risk of PTSD to an adulthood traumatic event by a factor of five.36 Combat veterans who develop PTSD are more likely to have histories of childhood abuse (estimated at between 25% and 45%).37,38 The impact of previous assaultive trauma on increasing the rate of PTSD with subsequent trauma appears to persist without decrement across time. In contrast, the sensitizing impact of previous nonassaultive trauma does appear to weaken over time (estimated at an 8% attenuation rate per year).36
Pre-existing psychiatric symptomatology, especially of MDD, anxiety disorders, neuroticism, and conduct/antisocial personality disorder, is relevant both to the increased risk of traumatic event exposure and to an increased susceptibility to PTSD once exposed. A history of affective disorder may be more prominent as a risk factor in women, whereas a history of anxiety disorder or parental psychiatric history may be of greater relevance as a risk factor in men.39 An earlier age of trauma exposure has not been consistently found to be predictive of PTSD; however, an earlier age of onset may constitute a risk for a more chronic course PTSD. The impact of lower educational and socioeconomic status on heightened PTSD risk has been previously described. In addition, a number of studies (primarily in combat veterans) have identified pre-existing cognitive/intellectual capacity as a risk factor that accounts for 10% to 20% of the variance associated with PTSD severity.40,41 The majority of studies that examined intellectual capacity in PTSD have failed to identify clear deficits in individuals diagnosed with PTSD. Rather, above-average cognitive capacity appears to confer a relative protective effect for those trauma survivors who do not develop PTSD. Such findings are consistent with research that suggests that higher order cognitive reasoning and verbal encoding of traumatic events may reduce the more persistent negative effects of traumatic exposure.
The most frequently cited peritraumatic risk factors for PTSD include severity of the trauma, dissociative reactions, excessively heightened arousal, feelings of anger/shame, and reduced social support. Meta-analytic studies of these factors tend to reveal effect sizes in the small to moderate range (.10 to .40 d).34,35 A significant dose-response relationship is routinely observed between the severity or duration of a traumatic event and the likelihood of developing PTSD. A recent examination of combat veterans employing objective measures of traumatic event severity found the lifetime prevalence rates of PTSD to be threefold to fourfold greater among high-combat-stress veterans versus low-combat-stress veterans, and nearly thirtyfold greater when examining the prevalence of PTSD more than 10 years after combat.26 Findings regarding the significance of traumatic event severity are also reported among most noncombat trauma studies. Likewise, peritraumatic dissociation (acute feelings of depersonalization, derealization, or amnesia at the time of the traumatic event) has frequently been cited as a significant risk factor for chronic PTSD. A comprehensive meta-analysis has recently reported an average effect size in the moderate range (.35 d) for studies that examined the risk of PTSD associated with peritraumatic dissociation.35 However, some studies have failed to replicate this association and have criticized current estimates on the basis of a failure to control for moderating variables (e.g., dissociation effect is attenuated when controlling for more general personality variables, such as neuroticism) and failure to account for time parameters (e.g., persistent dissociation and emotional disengage-ment well beyond the traumatic event has been found to be a stronger predictor of PTSD than peritraumatic dissociation).42,43
A number of recent studies have suggested that physiological indices of excessive autonomic arousal (e.g., increased heart rate following trauma exposure) are associated with increased probability of PTSD at 4 months and 2 years.44,45 The significant presence of anger or guilt has also been found to be predictive of the development and maintenance of PTSD, particularly among crime victims, child abuse survivors, and combat veterans. Nearly two-thirds of sexual abuse survivors report high levels of shame at the time of abuse discovery. Those who report persistent feelings of shame are significantly more likely to report a greater presence and severity of all three PTSD symptom clusters both 1 and 6 years following abuse discovery.46 Finally, meta-analytic studies have identified average effect sizes in the moderate range (.40 d) regarding the protective effect of social support. Some studies have suggested that the presence of a negative social environment (e.g., blaming and disbelief) has a stronger impact on risk for chronic PTSD than mere absence of perceived positive support. Furthermore, recent research involving victims of violent crime has found that although men and women were equally likely to report having received positive support, women were significantly more likely to report the presence of negative responses from family and friends.47 In turn, negative responses were found to be predictive of PTSD at 6 months, with this relationship being stronger among women than men.
PROGNOSIS
Recovery and Course of Illness
Recovery from PTSD appears to be most pronounced within the first year following trauma exposure. Large-scale epidemiological studies suggest a remission rate of approximately 25% at 6 months and 40% at 1 year.22 The rate of recovery following the first year slows, with the median time to remission estimated at between 2 and 3 years.17,22 The NCS has estimated that the median time to remission for treated individuals is approximately 36 months whereas the median time to remission in untreated individuals increases to 64 months. Regardless of treatment, more than 30% of individuals diagnosed with PTSD appear never to remit. If PTSD remission has not occurred within 6 to 7 years after the trauma, the chance for significant recovery thereafter appears to be quite small.17 An estimated 10% to 15% of all Vietnam combat veterans, and nearly 30% of those with high or very high combat exposure, were found to have PTSD 12 years following the cessation of combat.26,27 Twenty-eight percent of adult survivors of the Buffalo Creek flood failed to show remission from PTSD after 14 years.48 In a longitudinal prospective study of Israeli veterans from the 1982 Lebanon War, 20% of individuals who experienced combat stress reactions maintained a diagnosis of chronic PTSD for 20 years following the war.49 Many of the risk factors for the development of PTSD also appear to be relevant to increased risk for a chronic course (e.g., co-morbidity, multiple trauma exposures, negative social support, and trauma severity). In addition, the presence and intensity of avoidance and numbing symptoms (DSM-IV criterion C) may specifically predispose toward a chronic, rather than a remitting, course of illness in PTSD.50
In the majority of cases, the appearance of PTSD occurs shortly following traumatic exposure. Approximately 94% of rape victims meet the full PTSD symptom criteria 1 week following the traumatic event.51 Following the Oklahoma City bombing, symptoms of PTSD began within 1 day of the bombing in 76% of cases, in 94% within the first week, and in 98% within the first month.7 Recent longitudinal studies of remote traumatic events have suggested a symptom pattern characterized by immediate onset with gradual decline in subsequent years, followed by increasing PTSD symptom levels in midlife and beyond. Thus, not all cases of PTSD appear to fall into clear patterns of either remitting or chronic PTSD. In prisoners of war from World War II and the Korean War, increased rates of PTSD have been observed in older veterans as they age, with over 10% reporting an increase in PTSD symptoms some 40 years following discharge from the war despite having experienced relative remission during the preceding 25 to 30 years.52
Delayed-Onset PTSD
Numerous studies have estimated the prevalence of delayed-onset PTSD (with first symptoms occurring more than 6 months following a traumatic event) to range between 5% and 25%.49,53,54 Combat trauma has often been associated with higher rates of delayed-onset PTSD, as well as initial patterns of gradually worsening symptomatology over the first 6 months to 2 years after the trauma (in contrast to previously described rapid onset in other trauma types). Nearly 25% of Israeli combat veterans who demonstrated no combat stress reactions and no evidence of PTSD 3 years after the war were found to be diagnosed with PTSD 20 years later.49 In some cases, it has been suggested that delayed-onset PTSD may represent “reactivated” PTSD, in which previous subthreshold levels of symptomatology are triggered to threshold levels as a result of the aging process (e.g., transition to retirement) or external environment (e.g., stressful events that serve as reminders of the original trauma).
Suicide Attempts
A number of studies have identified PTSD as a robust risk factor for suicide ideation and attempts. A diagnosis of PTSD has been associated with a threefold to fivefold increase in suicide ideation and a threefold to sixfold increase in suicide attempts.55,56 In a multivariate prediction model based on NCS suicide data, the diagnosis of PTSD represents one of a limited number of factors identified as most parsimoniously predictive of suicide attempts. At least two additional risk factors (MDD and substance abuse/dependence) have been identified as common co-morbid conditions in PTSD. Based on risk analysis data from the NCS, the probability of a suicide attempt in PTSD patients would be markedly increased by the presence of either MDD or substance abuse (odds ratio = 21) or both (odds ratio = 125).55 This translates into a lifetime conditional probability of making a suicide attempt equal to 17% (per annum probability = 0.1%) for PTSD alone, with a 26% lifetime probability (per annum probability = 0.2%) for PTSD plus co-morbid MDD or substance abuse, and a 32% lifetime probability (per annum probability = 1%) for PTSD plus both co-morbid MDD and substance abuse. The lethality of suicide attempts or the percentage of successful suicide attempts in individuals diagnosed with PTSD has not been empirically established.
Impairment
Occupational and social impairment secondary to PTSD appears to be substantial. Individuals diagnosed with PTSD report an average increase of nearly 1 lost workday per month, as well as nearly 3 days per month in reduced productivity, due to psychiatric symptomatology.57 These figures are higher than almost all other psychiatric diagnoses examined (including MDD, dysthymia, and substance abuse disorders), with only GAD and panic disorder demonstrating higher workday losses. In an examination of the worst 30-day period in the past year, PTSD patients reported a total work loss of nearly 14 days within that period due to distress about their traumatic experiences.8 Studies of PTSD in primary care settings report significantly increased numbers of hospitalizations for medical/physical problems, significantly more emergency department visits, and higher utilization of medical care.20 Significant social impairments in the areas of marital/family function and general quality of life have frequently been reported for patients with chronic PTSD. During the worst 30-day period (when most upset about traumatic experiences) over the past year, individuals diagnosed with PTSD report nearly 17 of those days in which they spent less time with people and experienced more problems with tension and disagreements.8
PATHOGENESIS
Freud characterized traumatic anxiety as the affect that develops when it becomes no longer possible to avoid, or do anything about, a threatening situation, and the ego becomes overwhelmed. A prominent feature of the traumatized response is hyperarousal. A large epidemiological study performed by the Rand Corporation documented that posttraumatic hyperarousal strongly influences, but is not generally influenced by, other PTSD symptom clusters. The investigators concluded that hyperarousal plays a prominent role in the natural course of posttraumatic psychological distress.58
Several studies have shown that increased heart rate (a physical manifestation of hyperarousal) in the aftermath of a traumatic event predicts the subsequent development of PTSD.59 Although part of this effect may reflect diminished parasympathetic activity, the bulk is likely to reflect sympathetic overactivity, including the release of the emergency hormone epinephrine (adrenaline). Increased heart rate is likely to persist even after chronic PTSD has developed.60 Cerebrospinal norepinephrine levels are also elevated in chronic PTSD.61
How sympathetic arousal contributes to PTSD remains to be elucidated, but it is likely to involve both conditioning and nonconditioning (e.g., sensitization) mechanisms. In support of the latter, results of an identical twin study support the conclusion that increased heart rate response to loud tones, an unconditioned measure of arousal, is acquired as a result of the traumatic event in combat veterans who develop PTSD.62 It is likely that peripheral sympathetic arousal is secondary to central nervous system changes (e.g., amygdala hyper-reactivity), which are primary in mediating PTSD’s pathogenesis (see discussion of neuroimaging findings in PTSD elsewhere in this chapter).
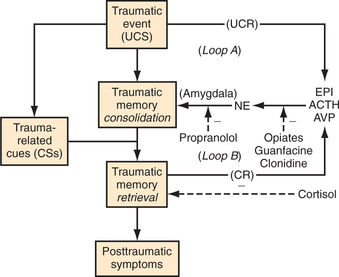
A current translational model of PTSD’s pathogenesis posits the following. A traumatic event (unconditioned stimulus [UCS]) overstimulates endogenous stress hormones such as epinephrine (unconditioned response [UCR]); these mediate an overconsolidation of the event’s memory traces. Then, recall of the event in response to reminders (conditioned stimulus [CS]) releases further stress hormones (conditioned response [CR]); these cause further overconsolidation, and the overconsolidated memory generates PTSD symptoms.63 This model is schematically displayed in Figure 34-2. Also shown are points for possible pharmacological intervention. An important paradox that needs to be clarified in future research is that, although adrenergic mechanisms appear to be critically involved in PTSD’s pathogenesis, antidepressant drugs that are thought to act primarily through serotonergic mechanisms represent the pharmacological treatment of choice for this disorder.
Psychophysiology
Over the past 25 years, findings from psychophysiological research have played an important role in characterizing the psychobiology of PTSD and in assessing key features of the disorder as specified in the DSM-IV. The symptom “physiological reactivity on exposure to internal or external cues that symbolize or resemble an aspect of the traumatic event” (DSM-IV Criterion B.5) has received considerable attention. A consistent picture has emerged demonstrating greater peripheral (e.g., electrodermal, heart rate, and facial electromyogram) reactivity to stimuli that represent, or are related to, the traumatic events of individuals who developed, compared to those who did not develop, PTSD.64,65 This heightened reactivity has been observed across individuals with PTSD resulting from a wide range of traumatic events (such as combat, sexual assault, motor vehicle accidents, cancer diagnosis, or witnessing horrific events). Approximately two-thirds of individuals who meet diagnostic criteria for PTSD show heightened psychophysiological reactivity when ex-posed to cues related to their particular traumatic event. Few individuals who do not meet diagnostic criteria for PTSD show this heightened reactivity.66 The diagnosis of PTSD is solely based, as has been the case for most psychiatric disorders, on self-reported phenomenology. The fact that some individuals can meet diagnostic criteria for PTSD, yet show little or no psychophysiological reactivity when confronted with trauma-related cues, raises interesting questions regarding whether it is reasonable to assume that self-reported experiences provide an adequate basis on which to establish the PTSD diagnosis.
Another PTSD symptom that has been the focus of considerable psychophysiological investigation is exaggerated startle (DSM-IV Criterion D.5). Exaggerated startle has long been recognized as a central feature of posttrauma reactions and may be one of the most reliably reported symptoms of the disorder. However, research support for exaggerated startle, which typically is measured from the eye-blink response to a sudden, loud burst of white noise, has been equivocal and only observed in about half of the studies that have examined it.64 Context is an important moderator of the startle response and may help to explain the equivocal findings. Specifically, individuals with PTSD have been found to reliably show increased startle in the presence of contextual anxiety cues (e.g., anticipation of a threatened shock or needle stick).64 This suggests that PTSD is associated with a heightened sensitivity to threatening cues or contexts.
One of the most reliable psychophysiological markers for PTSD is increased heart rate response to repeated presentations of loud pure tones.65 Converging data suggest that the increased heart rate response to loud tones reflects reduced parasympathetic, rather than increased sympathetic, activity in PTSD, in contrast to heart rate increases following trauma exposure or in response to traumatic reminders, which appear to primarily reflect increased sympathetic activity.62,67 Importantly, this elevated heart rate reactivity appears to represent an acquired, rather than a pre-existing, feature of PTSD. Because this is an acquired response, change in the magnitude of heart rate responses to loud tones may provide a useful biological measure of clinical improvement. It is not yet clear whether this increased heart rate reactivity is specific to PTSD or is a feature of anxiety disorders in general. Heart rate activity has also been used to measure the level of adrenergic activity at the time of the traumatic event. Increased adrenergic activity is believed to contribute to the development of PTSD, as suggested by findings that demonstrate that elevated heart rate measured soon after a traumatic event predicts those individuals who will go on to develop chronic PTSD.44
In addition to the insights provided by peripheral psychophysiological measures, electrophysiology has been used to address the alteration of central processes in PTSD.68 For example, PTSD is associated with reduced cortical responses, that is, event-related potentials, during tasks requiring the identification of particular (“target”) novel stimuli. This suggests impaired attention in individuals with PTSD, providing support for the symptom of disturbed concentration (DSM-IV Criterion D.3). It is worth noting that this reduced cortical response appears to be mitigated by psychoactive medications, as it has not been found in samples of medicated individuals with PTSD.69 As has also been observed for MDD, individuals with PTSD demonstrate a different pattern of electrophysiological cortical responses to increasingly loud auditory stimuli.70,71 The intensity dependence of these cortical responses has been linked to serotonergic activity and may be a useful predictor of the clinical response to selective serotonin reuptake inhibitor (SSRI) treatment.72
Neuroimaging and Neurocircuitry
Two principal lines of evidence have influenced neuro-circuitry models of PTSD.73 First, animal research has delineated the brain regions that mediate conditioned fear acquisition, expression, and extinction. Second, informed by animal research, human neuroimaging studies have tested specific hypotheses regarding brain structure and function in PTSD. To elaborate, the amygdala has been implicated as the key structure mediating conditioned fear acquisition and expression across species.74 Interestingly, specific cortical regions have been shown to provide top-down governance over the amygdala response. Ventromedial prefrontal territories have been shown to suppress amygdala responses in the service of extinction recall, whereas the hippocampus appears to play a critical role in processing relevant contextual information.75,76 This has led to hypotheses that suggest that anxiety disorders in general, and PTSD in particular, may be characterized by exaggerated amygdala responsivity, and/or deficient top-down governance over the amygdala referable to diminished medial frontal and/or hippocampal function.
A growing human neuroimaging literature has accrued in support of the aforementioned model.73 Using various functional imaging techniques, exaggerated amygdala responses have been observed in PTSD versus control subjects during exposure to reminders of traumatic events, as well as in response to general threat-related stimuli. Conversely, diminished prefrontal cortical and hippocampal functions have been observed in PTSD during exposure to reminders of traumatic events, as well as during specially designed cognitive-behavioral activation paradigms. Furthermore, morphometric imaging studies have indicated that individuals with PTSD exhibit smaller medial frontal and hippocampal volumes than do comparison subjects without PTSD. Taken together, these data support a model of amygdala hyper-responsivity in PTSD that may explain formation of enduring conditioned fear associations, as well as exaggerated conditioned fear responses. In addition, the attenuated capacity of key cortical regions may mediate deficiencies in extinction capacity and failures to appreciate safe contexts, which are in accord with the clinical phenomenology of this disorder.
It remains unclear whether these differences represent pre-existing vulnerability factors for PTSD or fundamental pathogenic factors that emerge as a consequence of the traumatic exposure. However, at least with respect to the hippocampus, findings from a twin study suggest that smaller hippocampal volumes may represent a pre-existing risk factor for developing PTSD, rather than a property emerging from traumatic exposure.77 This line of translational research has the potential to offer objective diagnostic tests and early identification of individuals at risk in the future. Moreover, as the neurocircuitry underlying PTSD becomes better understood, this work promises new targets for innovative therapies.
TREATMENT
Utilization
Limited and delayed treatment-seeking significantly contribute to morbidity in PTSD. These factors likely reflect, in part, the avoidance symptoms inherent in the disorder. NCS data suggest that only 7% of individuals make treatment contact within the first year of PTSD onset.78 This figure compares unfavorably with most other psychiatric disorders, including GAD (33%), panic disorder (34%), MDD (37%), dysthymia (42%), bipolar disorder (39%), and alcohol dependence (21%). The median duration of delay in seeking treatment for PTSD is 12 years. In any given year, only an estimated 38% of individuals with PTSD will seek or use any treatment service, and only 22% of PTSD patients will seek treatment from mental health professionals.79 Those who do seek treatment from mental health professionals are seen for an average of 22 visits per year (highest among all psychiatric diagnoses with the exception of nonaffective psychosis). The projected lifetime proportion of PTSD cases that will make it to treatment is 65% (compared with approximately 90% for MDD and bipolar disorder).78
Psychotherapy
A variety of psychological interventions have been advocated for the treatment of PTSD (including prolonged exposure therapy, cognitive therapy, stress management, psychodynamic therapy, and eye movement desensitization and reprocessing [EMDR]). Some degree of empirical evidence for efficacy exists for all of these approaches.80 However, the PTSD psychotherapy outcome literature has focused primarily on cognitive-behavioral approaches (prolonged exposure and cognitive restructuring) that are based on contemporary learning theory. More recently there has been an increased interest in EMDR. In part, this focus reflects the fact that these approaches lend themselves readily to randomized-controlled trial (RCT) designs due to their brief duration (generally 6 to 14 sessions) and highly structured nature (easily “manualized” into a standardized treatment package). However, recent studies investigating specific psychodynamic approaches, which have likewise been operationalized into a standardized brief treatment package (e.g., interpersonal therapy), have provided preliminary results that suggest efficacy that may be comparable to the more empirically established cognitive-behavioral approaches.81
The research outcome literature has consistently demonstrated the efficacy of cognitive-behavioral approaches in the treatment of PTSD, which is regarded in many practice guidelines (including those published by the International Society for Traumatic Stress Studies) as a first-line treatment.80 Exposure therapy (sometimes known as flooding, implosive therapy, or direct therapeutic exposure) involves confronting traumatic memories and asking the patient to imaginally “relive” the experience in a safe therapeutic setting. Modes of therapeutic action are thought to involve extinction of anxiety/fear responses, blocking of negative reinforcement associated with avoidance, incorporation of safety information into the traumatic memory, and differentiation of the traumatic event from the current context. Cognitive restructuring therapy typically involves efforts to confront and challenge erroneous or overgeneralized beliefs that are developed in the context of trauma and often involve themes of safety, trust, control, and self-esteem (e.g., “The world is unsafe,” and “I am incompetent to take care of myself”). Exposure and cognitive therapy approaches often overlap in practice, and some approaches (such as cognitive processing therapy [CPT]) formally incorporate both exposure and cognitive restructuring elements.82 A recent meta-analysis of cognitive-behavioral approaches has found an average short-term improvement rate of 53% for those completing exposure treatment (42% for individuals who enter treatment, including noncompleters, i.e., intent-to-treat sample) and 48% for cognitive therapy completers (38% of intent-to-treat sample).83 More impressively, 68% of exposure treatment completers on average no longer meet criteria for PTSD at the end of treatment (53% of intent-to-treat sample), and an average of 56% of cognitive therapy completers no longer meet PTSD criteria (46% of intent-to-treat sample).
EMDR is a more recent development, originating from observations posited by Dr. Francine Shapiro in 1987. This approach involves asking patients to develop a mental image of their traumatic event while tracking an alternating bilateral stimulus (most commonly the therapist’s fingers being moved back and forth across the patient’s visual field). Unlike the cognitive-behavioral approaches, the development of EMDR was not theory driven and to date no clear mode of therapeutic action has been established. As a result, EMDR has generated controversy within the PTSD-treatment community. Furthermore, questions have been raised regarding the necessity of the visual tracking component, and whether EMDR may actually represent a different application of exposure and cognitive-behavior treatment elements.84 At any rate, RCTs have demonstrated the efficacy of EMDR as a treatment modality. The same meta-analysis applied to cognitive-behavioral approaches found a mean improvement rate of 60% in EMDR treatment completers (52% of intent-to-treat sample).83 Furthermore, 65% of EMDR completers no longer meet PTSD criteria at the end of treatment (60% of intent-to-treat sample). These figures are comparable to those reported for cognitive-behavioral approaches, although the number of EMDR studies on which this is based is fewer.
The majority of meta-analytic studies and “head-to-head” comparison studies have failed to find differential efficacy among the empirically studied psychotherapies described previously.83–86 That is, no substantial differences in treatment efficacy have been established between exposure therapy, cognitive therapy, and EMDR. Nor have combination treatments (e.g., exposure therapy plus cognitive restructuring, exposure therapy plus stress management) been found to be more effective than individual approaches alone.87,88 Thus, there are few empirical data to support the superiority of any of the major treatment approaches over the others. Furthermore, the treatment literature to date does not provide any systematic data with which to guide decisions regarding differential effectiveness of various treatments for different types of trauma. Meta-analytic reviews have suggested that some populations may be less responsive to treatment in general (e.g., combat veterans) whereas other populations may be relatively more responsive to treatment (e.g., women). However, specific treatment approaches have not been empirically established as more or less effective for specific trauma populations.
A number of important caveats should be offered in understanding the applicability and efficacy of the empirically supported treatments in a clinical setting. Although brief cognitive-behavioral and EMDR approaches have produced substantial posttreatment improvements for individuals diagnosed with PTSD, these approaches have yet to establish long-term efficacy, not to mention effectiveness. The majority of studies have failed to examine outcome at or beyond 6 months (a recent meta-analysis was only able to identify two studies with follow-up as long as 1 year).83 Given the highly chronic nature of PTSD (as described elsewhere) this poses a serious issue regarding clinical utility. Of those studies examining follow-up data at 6 months to 1 year, it is estimated that on average nearly two-thirds of treatment participants failed to meet criteria for clinical improvement.83
Outcome studies in PTSD often report percentages of treated patients who no longer “meet criteria for PTSD diagnosis” at the end of treatment. Although these percentages can be impressive, they should not be interpreted as “cure” rates. Far from suggesting a “cure” or even substantial improvement, a change in a single symptom can move a treatment participant from a diagnosis of PTSD to non-PTSD. As reviewed previously, partial or subthreshold PTSD is often associated with considerable levels of dysfunction and symptomatology. The fact that a recent meta-analysis has found average percentages of patients who “lost their PTSD diagnosis” to actually be higher than the average percentage of patients who met investigator-defined “improvement” criteria (a situation not typically found in treatment outcome studies of other psychiatric disorders) is consistent with this observation.83 Significant pathology can still exist even for those defined as treatment “successes.”
As opposed to “efficacy,” which has largely been demonstrated in the ivory tower, psychotherapies for PTSD have not yet been clearly shown to be “effective,” that is, helpful in ordinary clinical settings. Dropout rates even in efficacy RCTs of PTSD treatments may in some cases run as high as 40%, with the average dropout rate estimated at nearly 25%.83,88 In some cases, clinical trials do not account for “dropouts” that occur before treatment randomization, thus underestimating the true rates of treatment implementation failures that would be relevant to a practicing clinician. Furthermore, treatment dropout rates in clinical settings may run even higher. A recent study of completion rates of cognitive-behavioral treatment for PTSD in a clinical setting (employing few exclusion criteria) found only 28% of patients to complete treatment.89 Over 40% of those who started exposure therapy did not complete it; 76% of patients who dropped out did so even before starting treatment. Treatment dropout was found to be related to PTSD symptom severity; co-morbid borderline personality disorder; higher depression, avoidance, and arousal levels; and social impairment. Thus, in clinical settings, the potential effectiveness of empirically supported PTSD therapies must be judged against the backdrop of significant proportions of patients who will fail to engage in or complete such treatments.
Also relevant to effectiveness, it is unclear to what degree the study populations employed in the majority of laboratory-setting RCTs of cognitive-behavioral therapy (CBT) and EMDR are representative of general clinical populations encountered by clinicians. Nearly one-third of patients referred for treatment for PTSD in RCTs are excluded based on conditions that a typical clinician in practice would not have the option to exclude (e.g., suicide ideation, substance abuse, co-morbid Axis I or II conditions).83 Little has been empirically established regarding the differential effectiveness of these treatments with more complex case presentations and the co-morbid presence of serious Axis I or Axis II conditions. For reasons of maintaining internal validity, clinical trials of PTSD treatments are frequently and understandably focused on creating homogeneous populations of relatively “pure” PTSD cases. Given the extremely high rates of co-morbidity in PTSD (as reviewed previously), these limitations do not provide clinicians with easy guidelines for applying the empirically supported therapies to complex, polysymptomatic patients who may frequently be encountered in ordinary clinical practice.
The majority of RCTs to date have employed wait-list or “minimal attention” controls (a small number of studies have included simple “relaxation therapy” or vaguely defined “supportive therapy”). The reliance on relatively inert comparison conditions fails to rule out “common” or “nonspecific” factors applicable to any psychotherapy (e.g., a trusting relationship, accurate empathy, a positive working alliance, an opportunity for ventilating of concerns, and expectation for change), which may play a significant role in positive outcome when a treatment is well structured, is credible, and involves a committed therapist. The failure to clearly demonstrate differential efficacy among the major treatment approaches is consistent with this hypothesis. A recent well-controlled study of women with PTSD secondary to childhood sexual abuse found that a “present-centered therapy” (which focused on current problem solving and specifically excluded processing of traumatic memories) was found to be as effective as CBT (including both exposure and cognitive restructuring).90 The present-centered therapy had been intended as a control condition. Thus, caution should be exercised in concluding the efficacy of “specific” treatment approaches. A parsimonious interpretation of the current psychotherapy research literature in PTSD might suggest that most well-designed and credible treatments (e.g., exposure therapy, cognitive therapy, EMDR, psychodynamic interpersonal therapy, and present-centered therapy) will be more effective than doing little or nothing. Furthermore, because RCTs generally test a standardized treatment package, it is premature based on available data to know what specific elements of treatment (e.g., nature and duration of prolonged exposure and particular techniques for restructuring of cognitions), if any at all, are essential or critical to outcome. Nor has it been empirically established that the typical course of 6 to 14 sessions is optimal for treatment of chronic PTSD.
Few clinicians actually employ many of the empirically supported therapies described. In a recent large-scale survey of psychologists, only 17% used exposure therapy to treat PTSD.91 Moreover, even among psychologists fully trained in, and familiar with, exposure therapy, one-third did not use exposure therapy at all with their PTSD patients, and a majority of the clinicians used the intervention with less than half of their PTSD patients.
Pharmacotherapy
In the treatment of PTSD, pharmacotherapy has advantages and disadvantages compared to psychotherapy. Its major advantage is availability. Drug treatment may be obtained from any psychiatrist, or nonpsychiatric physician, with a license to prescribe. In contrast, as noted previously, the major forms of psychotherapy with empirically demonstrated efficacy for PTSD, such as CBT, with few exceptions, still remain available only in academic centers. EMDR therapy may have been more widely disseminated. However, the number of CBT or EMDR practitioners with sufficient skill in treating PTSD remains small. A related advantage of pharmacotherapy is its ease of administration, given the shorter duration of medication management compared to psychotherapy sessions, and the lesser effort on the part of both the physician and the patient. Another advantage of pharmacotherapy for PTSD is that it has been demonstrated in large-scale studies to be beneficial in settings approaching ordinary clinical settings. In other words, it has been found to be effective.
For readers wishing to acquaint themselves further with the pharmacotherapy of PTSD, a number of useful recent reviews are available.92–94
CURRENT CONTROVERSIES AND FUTURE DIRECTIONS
1 Breslau N, Kessler RC. The stressor criterion in DSM-IV posttraumatic stress disorder: an empirical investigation. Biol Psychiatry. 2001;50:699-704.
2 Brewin CR, Andrews B, Rose S. Fear, helplessness, and horror in posttraumatic stress disorder: investigating DSM-IV criterion A2 in victims of violent crime. J Traumatic Stress. 2000;13:499-509.
3 Asmundson GJ, Stapleton JA, Taylor S. Are avoidance and numbing distinct PTSD symptom clusters? J Traumatic Stress. 2004;17:467-475.
4 Breslau N, Reboussin BA, Anthony JC, et al. The structure of posttraumatic stress disorder: latent class analysis in 2 community samples. Arch Gen Psychiatry. 2005;62:1343-1351.
5 Breslau N, Chilcoat HD, Kessler RC, et al. Vulnerability to assaultive violence: further specification of the sex difference in post-traumatic stress disorder. Psychol Med. 1999;29:813-821.
6 Green BL. Disasters and posttraumatic stress disorder. In: Davidson JRT, Foa EB, editors. Posttraumatic stress disorder: DSM-IV and beyond. Washington, DC: American Psychiatric Press, 1993.
7 North CS, Nixon SJ, Shariat S, et al. Psychiatric disorders among survivors of the Oklahoma City bombing. JAMA. 1999;282:755-762.
8 Breslau N, Lucia VC, Davis GC. Partial PTSD versus full PTSD: an empirical examination of associated impairment. Psychol Med. 2004;34:1205-1214.
9 Stein MB, Walker JR, Hazen AL, et al. Full and partial posttraumatic stress disorder: findings from a community survey. Am J Psychiatry. 1997;154:1114-1119.
10 Marshall RD, Olfson M, Hellman F, et al. Comorbidity, impairment, and suicidality in subthreshold PTSD. Am J Psychiatry. 2001;158:1467-1473.
11 Harvey AG, Bryant RA. Acute stress disorder: a synthesis and critique. Psychol Bull. 2002;128:886-902.
12 Harvey AG, Bryant RA. The relationship between acute stress disorder and posttraumatic stress disorder: a prospective evaluation of motor vehicle accident survivors. J Consult Clin Psychol. 1998;66:507-512.
13 Harvey AG, Bryant RA. The relationship between acute stress disorder and posttraumatic stress disorder: a two-year prospective evaluation. J Consult Clin Psychol. 1999;67:985-988.
14 Koren D, Arnon I, Klein E. Acute stress response and posttraumatic stress disorder in traffic accident victims: a one-year prospective, follow-up study. Am J Psychiatry. 1999;156:367-373.
15 Marshall RD, Spitzer R, Liebowitz MR. Review and critique of the new DSM-IV diagnosis of acute stress disorder. Am J Psychiatry. 1999;156:1677-1685.
16 Breslau N, Davis GC, Andreski P, et al. Traumatic events and posttraumatic stress disorder in an urban population of young adults. Arch Gen Psychiatry. 1991;48:216-222.
17 Kessler RC, Sonnega A, Bromet E, et al. Posttraumatic stress disorder in the National Comorbidity Survey. Arch Gen Psychiatry. 1995;52:1048-1060.
18 Kessler RC, Chiu WT, Demler O, et al. Prevalence, severity, and comorbidity of 12-month DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:617-627.
19 Breslau N. Epidemiologic studies of trauma, posttraumatic stress disorder, and other psychiatric disorders. Can J Psychiatry. 2002;47:923-929.
20 Stein MB, McQuaid JR, Pedrelli P, et al. Posttraumatic stress disorder in the primary care medical setting. Gen Hosp Psychiatry. 2000;22:261-269.
21 Mueser KT, Goodman LB, Trumbetta SL, et al. Trauma and posttraumatic stress disorder in severe mental illness. J Consult Clin Psychol. 1998;66:493-499.
22 Breslau N, Kessler RC, Chilcoat HD, et al. Trauma and posttraumatic stress disorder in the community: the 1996 Detroit Area Survey of Trauma. Arch Gen Psychiatry. 1998;55:626-632.
23 Plichta SB, Falik M. Prevalence of violence and its implications for women’s health. Women’s Health Issues. 2001;11:244-258.
24 Kessler RC, Berglund P, Demler O, et al. Lifetime prevalence and age-of-onset distributions of DSM-IV disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:593-602.
25 Prigerson HG, Maciejewski PK, Rosenheck RA. Population attributable fractions of psychiatric disorders and behavioral outcomes associated with combat exposure among US men. Am J Public Health. 2002;92:59-63.
26 Dohrenwend BP, Turner JB, Turse NA, et al. The psychological risks of Vietnam for US veterans: a revisit with new data and methods. Science. 2006;313:979-982.
27 Kulka RA, Schlenger WE, Fairbank JA, et al. Trauma and the Vietnam War generation: report of findings from the National Vietnam Veterans Readjustment Survey. New York: Brunner/Mazel, 1990.
28 Lyons MJ, Goldberg J, Eisen SA, et al. Do genes influence exposure to trauma? A twin study of combat. Am J Med Genet. 1993;48:22-27.
29 Stein MB, Jang KL, Taylor S, et al. Genetic and environmental influences on trauma exposure and posttraumatic stress disorder symptoms: a twin study. Am J Psychiatry. 2002;159:1675-1681.
30 Jang KL, Stein MB, Taylor S, et al. Exposure to traumatic events and experiences: aetiological relationships with personality function. Psychiatry Res. 2003;120:61-69.
31 True WR, Rice J, Eisen SA, et al. A twin study of genetic and environmental contributions to liability for posttraumatic stress symptoms. Arch Gen Psychiatry. 1993;50:257-264.
32 Segman RH, Cooper-Kazaz R, Macciardi F, et al. Association between the dopamine transporter gene and posttraumatic stress disorder. Mol Psychiatry. 2002;7:903-907.
33 Lee HJ, Lee MS, Kang RH, et al. Influence of the serotonin transporter promoter gene polymorphism on susceptibility to posttraumatic stress disorder. Depress Anxiety. 2005;21:135-139.
34 Brewin CR, Andrews B, Valentine JD. Meta-analysis of risk factors for posttraumatic stress disorder in trauma-exposed adults. J Consult Clin Psychol. 2000;68:748-766.
35 Ozer EJ, Best SR, Lipsey TL, et al. Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol Bull. 2003;129:52-73.
36 Breslau N, Chilcoat HD, Kessler RC, et al. Previous exposure to trauma and PTSD effects of subsequent trauma: results from the Detroit Area Survey of Trauma. Am J Psychiatry. 1999;156:902-907.
37 Bremner JD, Southwick SM, Johnson DR, et al. Childhood physical abuse and combat-related posttraumatic stress disorder in Vietnam veterans. Am J Psychiatry. 1993;150:235-239.
38 Zaidi LY, Foy DW. Childhood abuse experiences and combat-related PTSD. J Traumatic Stress. 1994;7:33-42.
39 Bromet E, Sonnega A, Kessler RC. Risk factors for DSM-III-R posttraumatic stress disorder: findings from the National Comorbidity Survey. Am J Epidemiol. 1998;147:353-361.
40 Macklin ML, Metzger LJ, Litz BT, et al. Lower precombat intelligence is a risk factor for posttraumatic stress disorder. J Consult Clin Psychol. 1998;66:323-326.
41 Gilbertson MW, Paulus LA, Williston SK, et al. Neurocognitive function in monozygotic twins discordant for combat exposure: relationship to posttraumatic stress disorder. J Abnorm Psychol. 2006;115:484-495.
42 Holeva V, Tarrier N. Personality and peritraumatic dissociation in the prediction of PTSD in victims of road traffic accidents. J Psychosom Res. 2001;51:687-692.
43 Briere J, Scott C, Weathers F. Peritraumatic and persistent dissociation in the presumed etiology of PTSD. Am J Psychiatry. 2005;162:2295-2301.
44 Shalev AY, Sahar T, Freedman S, et al. A prospective study of heart rate response following trauma and the subsequent development of posttraumatic stress disorder. Arch Gen Psychiatry. 1998;55:553-559.
45 Bryant RA, Harvey AG, Guthrie RM, et al. Acute psychophysiological arousal and posttraumatic stress disorder: a two-year prospective study. J Traumatic Stress. 2003;16:439-443.
46 Feiring C, Taska LS. The persistence of shame following sexual abuse: a longitudinal look at risk and recovery. Child Maltreat. 2005;10:337-349.
47 Andrews B, Brewin C, Rose S. Gender, social support, and PTSD in victims of violent crime. J Traumatic Stress. 2003;16:421-427.
48 Green BL, Lindy JD, Grace MC, et al. Buffalo Creek survivors in the second decade: stability of stress symptoms. Am J Orthopsychiatry. 1990;60:43-54.
49 Solomon Z, Mikulincer M. Trajectories of PTSD: a 20-year longitudinal study. Am J Psychiatry. 2006;163:659-666.
50 Marshall RD, Turner JB, Lewis-Fernandez R, et al. Symptom patterns associated with chronic PTSD in male veterans: new findings from the National Vietnam Veterans Readjustment Study. J Nerv Ment Dis. 2006;194:275-278.
51 Foa EB, Rothbaum BO, Riggs D, et al. Treatment of posttraumatic stress disorder in rape victims: a comparison between cognitive behavioral procedures and counseling. J Consult Clin Psychol. 1991;59:715-723.
52 Port CL, Engdahl B, Frazier P. A longitudinal and retrospective study of PTSD among older prisoners of war. Am J Psychiatry. 2001;158:1474-1479.
53 Wolfe J, Erickson DJ, Sharkansky EJ, et al. Course and predictors of posttraumatic stress disorder among Gulf War veterans: a prospective analysis. J Consult Clin Psychol. 1999;67:520-528.
54 Gray MJ, Bolton EE, Litz BT. A longitudinal analysis of PTSD symptom course: delayed-onset PTSD in Somalia peacekeepers. J Consult Clin Psychol. 2004;72:909-913.
55 Kessler RC, Borges G, Walter E. Prevalence of and risk factors for lifetime suicide attempts in the National Comorbidity Survey. Arch Gen Psychiatry. 1999;56:617-626.
56 Sareen J, Cox BJ, Afifi TO, et al. Anxiety disorders and risk for suicidal ideation and suicide attempts: a population-based longitudinal study of adults. Arch Gen Psychiatry. 2005;62:1249-1257.
57 Kessler RC, Frank RG. The impact of psychiatric disorders on work loss days. Psychol Med. 1997;27:861-873.
58 Schell TL, Marshall GN, Jaycox LH. All symptoms are not created equal: the prominent role of hyperarousal in the natural course of posttraumatic psychological distress. J Abnorm Psychol. 2004;113:189-197.
59 Bryant RA. Longitudinal psychophysiological studies of heart rate: mediating effects and implications for treatment. Ann N Y Acad Sci. 2006;1071:19-26.
60 Buckley TC, Kaloupek DG. A meta-analytic examination of basal cardiovascular activity in posttraumatic stress disorder. Psychosom Med. 2001;63:585-594.
61 Geracioti TDJr, Baker DG, Ekhator NN, et al. CSF norepinephrine concentrations in posttraumatic stress disorder. Am J Psychiatry. 2001;158:1227-1230.
62 Pitman RK, Delahanty DL. Conceptually driven pharmacologic approaches to acute trauma. CNS Spectr. 2005;10:99-106.
63 Orr SP, Metzger LJ, Miller MW, et al. Psychophysiological assessment of PTSD. In Wilson JP, Keane TM, editors: Assessing psychological trauma and PTSD: a handbook for practitioners, ed 2, New York: Guilford Publications, 2004.
64 Orr SP, Metzger LJ, Pitman RK. Psychophysiology of posttraumatic stress disorder. Psychiatr Clin North Am. 2002;25:271-293.
65 Orr SP, McNally RJ, Rosen GM, et al. Psychophysiological reactivity: implications for conceptualizing PTSD. In: Rosen GM, editor. Posttraumatic stress disorder: issues and controversies. United Kingdom: John Wiley & Sons, 2004.
66 Orr SP, Metzger LJ, Lasko NB, et al. Psychophysiologic responses to sudden, loud tones in monozygotic twins discordant for combat exposure: relationship to posttraumatic stress disorder. Arch Gen Psychiatry. 2003;60:283-288.
67 Shalev AY, Peri T, Brandes D, et al. Auditory startle responses in trauma survivors with PTSD: a prospective study. Am J Psychiatry. 2000;157:255-261.
68 Metzger LJ, Gilbertson MW, Orr SP. Electrophysiology of PTSD. In: Vasterling J, Brewin C, editors. Neuropsychology of PTSD: biological, clinical, and cognitive perspectives. New York: Guilford Publications, 2005.
69 Metzger LJ, Orr SP, Lasko NB, et al. Auditory event-related potentials to tone stimuli in combat-related posttraumatic stress disorder. Biol Psychiatry. 1997;42:1006-1015.
70 Metzger LJ, Carson MA, Paulus LA, et al. Event-related potentials to auditory stimuli in female Vietnam nurse veterans with posttraumatic stress disorder. Psychophysiology. 2002;39:49-63.
71 Paige SR, Reid GM, Allen MG, et al. Psychophysiological correlates of posttraumatic stress disorder in Vietnam veterans. Biol Psychiatry. 1990;27:419-430.
72 Paige SR, Hendricks SE, Fitzpatrick DF, et al. Amplitude/intensity functions of auditory event-related potentials predict responsiveness to bupropion in major depressive disorder. Psychopharmacol Bull. 1995;31:243-248.
73 Rauch SL, Shin LM, Phelps EA. Neurocircuitry models of posttraumatic stress disorder and extinction: human neuroimaging research past, present and future. Biol Psychiatry. 2006;60:376-382.
74 LeDoux JE. The emotional brain. New York: Simon & Schuster, 1996.
75 Milad MR, Quirk GJ. Neurons in medial prefrontal cortex signal memory for fear extinction. Nature. 2002;420:70-74.
76 Corcoran KA, Maren S. Factors regulating the effects of hippocampal inactivation on renewal of conditional fear after extinction. Learn Mem. 2004;11:598-603.
77 Gilbertson MW, Shenton ME, Ciszewski A, et al. Smaller hippocampal volume predicts pathologic vulnerability to psychological trauma. Nat Neurosci. 2002;5:1242-1247.
78 Wang PS, Berglund P, Olfson M, et al. Failure and delay in initial treatment contact after first onset of mental disorders in the National Comorbidity Survey Replication. Arch Gen Psychiatry. 2005;62:603-613.
79 Kessler RC, Zhao S, Katz SJ, et al. Past-year use of outpatient services for psychiatric problems in the National Comorbidity Survey. Am J Psychiatry. 1999;156:115-123.
80 Foa EB, Keane TM, Friedman MJ, editors. Effective treatments for PTSD. New York: Guilford Press, 2000.
81 Bleiberg KL, Markowitz LC. A pilot study of interpersonal psychotherapy for posttraumatic stress disorder. Am J Psychiatry. 2005;162:181-183.
82 Resick PA, Schnicke MK. Cognitive processing therapy for sexual assault victims. J Consult Clin Psychol. 1992;60:748-756.
83 Bradley R, Greene J, Russ E, et al. A multidimensional meta-analysis of psychotherapy for PTSD. Am J Psychiatry. 2005;162:214-227.
84 Seidler GH, Wagner FE. Comparing the efficacy of EMDR and trauma-focused cognitive-behavioral therapy in the treatment of PTSD: a meta-analytic study. Psychol Med. 2006;2:1-8.
85 Resick PA, Nishith P, Weaver TL, et al. A comparison of cognitive-processing therapy with prolonged exposure and a waiting condition for the treatment of chronic posttraumatic stress disorder in female rape victims. J Consult Clin Psychol. 2002;70:867-879.
86 Rothbaum BO, Astin MC, Marsteller F. Prolonged exposure versus eye movement desensitization and reprocessing (EMDR) for PTSD rape victims. J Traumatic Stress. 2005;18:607-616.
87 Foa EB, Dancu CV, Hembree EA, et al. A comparison of exposure therapy, stress inoculation training, and their combination for reducing posttraumatic stress disorder in female assault victims. J Consult Clin Psychol. 1999;67:194-200.
88 Foa EB, Hembree EA, Cahill SP, et al. Randomized trial of prolonged exposure for posttraumatic stress disorder with and without cognitive restructuring: outcome at academic and community clinics. J Consult Clin Psychol. 2005;73:953-964.
89 Zayfert C, DeViva JC, Becker CB, et al. Exposure utilization and completion of cognitive behavioral therapy for PTSD in a “real world” clinical practice. J Traumatic Stress. 2005;18:637-645.
90 McDonagh A, Friedman M, McHugo G, et al. Randomized trial of cognitive-behavioral therapy for chronic posttraumatic stress disorder in adult female survivors of childhood sexual abuse. J Consult Clin Psychol. 2005;73:515-524.
91 Becker CB, Zayfert C, Anderson E. A survey of psychologists’ attitudes towards and utilization of exposure therapy for PTSD. Behav Res Ther. 2004;42:277-292.
92 Davidson JR. Pharmacologic treatment of acute and chronic stress following trauma. J Clin Psychiatry. 2006;67:34-39.
93 Davis LL, Frazier EC, Williford RB, et al. Long-term pharmacotherapy for post-traumatic stress disorder. CNS Drugs. 2006;20:465-476.
94 Stein MB. Pharmacological interventions for posttraumatic stress disorder. In: Kato N, Kawata M, Pitman RK, editors. Brain mechanisms and clinical implications. Tokyo: Springer-Verlag, 2006.