Shunt Calculation
PREREQUISITE NURSING KNOWLEDGE
• Right-to-left intrapulmonary shunting (also referred to as physiologic shunting, wasted blood flow, and venous admixture) is the pathologic phenomenon whereby venous blood is shunted past the alveoli without taking up oxygen. This blood then returns to the left side of the heart as venous blood with a low oxygen tension.1,2
• Right-to-left intrapulmonary shunting is expressed as a fraction or percentage of shunted blood flow (Qs) to total blood flow (Qt) as expressed by the equation (Qs/Qt). The normal physiologic shunt is less than 5% and is caused by venous blood from the bronchial and coronary veins returning to the left side of the heart as desaturated blood.1,2
• Shunting of blood past the alveoli means that a certain percentage of the blood flows through an area of lung that receives no ventilation. Examples of conditions in which shunt is present include acute respiratory distress syndrome, acute lung injury, atelectasis, pneumonia, and pulmonary edema with fluid-filled alveoli.
• As the percentage of the shunted cardiac output increases, the mixture of venous shunted blood with arterial blood increases with a concomitant decrease in the arterial oxygen tension. The extent of the hypoxemia depends on the amount of the lung parenchyma that is not ventilated.
• The hallmark of right-to-left intrapulmonary shunting is persistent hypoxemia despite high concentrations of inspired oxygen (called refractory hypoxemia).1,2
• For evaluation of shunt, heparinized* arterial and mixed venous blood samples are analyzed with a cooximeter to determine saturation. Use of the calculated saturation obtained in conjunction with blood gas analysis or with pulse oximetry is not as accurate.1,2
EQUIPMENT
• Mixed venous and arterial blood gas and saturation measurements
• Pulmonary artery catheter, for drawing mixed venous blood samples, or venous oxygen saturation (SVO2) catheter. If an SVO2 catheter is used, the mixed venous saturation recorded on the monitor can be used for the calculation (as long as in vitro and in vivo calibrations have been done according to manufacturer’s recommendations)
PATIENT AND FAMILY EDUCATION
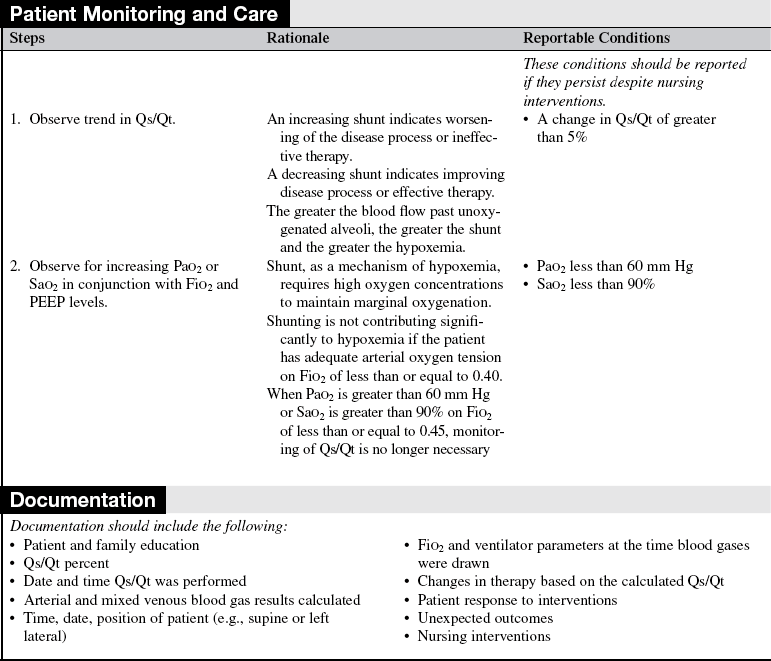
• Keep the patient and family informed about the patient’s oxygenation status. Inform them of changes in therapy and how to interpret the changes. If the patient or a family member requests specific information about intrapulmonary shunting, explain the general relationship between Qs/Qt and hypoxemia.  Rationale: Most patients and families are less concerned with the diagnostic and therapeutic details and more concerned with how the patient’s condition is progressing overall or in relation to a specific physiologic function.
Rationale: Most patients and families are less concerned with the diagnostic and therapeutic details and more concerned with how the patient’s condition is progressing overall or in relation to a specific physiologic function.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Signs and symptoms of inadequate oxygenation include the following:
 Decreasing arterial oxygen tension and saturation
Decreasing arterial oxygen tension and saturation
 Intercostal and suprasternal retractions
Intercostal and suprasternal retractions
 Rationale: Calculation of Qs/Qt is indicated to help differentiate between the mechanisms of hypoxemia, to determine the degree of shunt for trending, and to evaluate the effectiveness of therapies.
Rationale: Calculation of Qs/Qt is indicated to help differentiate between the mechanisms of hypoxemia, to determine the degree of shunt for trending, and to evaluate the effectiveness of therapies.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Determine arterial oxygen tension or saturation.  Rationale: Hypoxemia is confirmed by a decreasing arterial partial pressure of oxygen (PaO2), decreasing arterial oxygen saturation (SaO2), an absolute Pao2 of less than 60 mm Hg, or an absolute SaO2 of less than 90%. A low PaO2 and a low Sao2 with increasing supplemental oxygen confirm hypoxemia caused by right-to-left intrapulmonary shunting.
Rationale: Hypoxemia is confirmed by a decreasing arterial partial pressure of oxygen (PaO2), decreasing arterial oxygen saturation (SaO2), an absolute Pao2 of less than 60 mm Hg, or an absolute SaO2 of less than 90%. A low PaO2 and a low Sao2 with increasing supplemental oxygen confirm hypoxemia caused by right-to-left intrapulmonary shunting.
• Determine Qs/Qt trends with therapies and interventions.  Rationale: Calculation of Qs/Qt is indicated to help differentiate mechanisms of hypoxemia and to provide appropriate interventions. The effect of therapies such as positive end-expiratory pressure (PEEP), selected ventilator modes (e.g., pressure release ventilation, inverse ratio), and prone positioning on shunting and oxygenation can be quantified.
Rationale: Calculation of Qs/Qt is indicated to help differentiate mechanisms of hypoxemia and to provide appropriate interventions. The effect of therapies such as positive end-expiratory pressure (PEEP), selected ventilator modes (e.g., pressure release ventilation, inverse ratio), and prone positioning on shunting and oxygenation can be quantified.
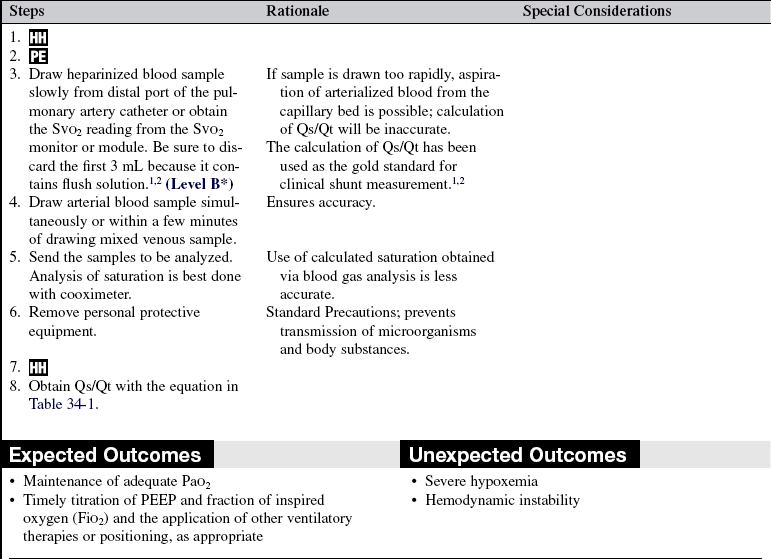
Table 34-1
Qs/Qt = (Cco2 – Cao2)/(Cco2 – Cvo2)
Cco2 = (Hgb × 1.39* × Sat† [1.0] + (Pao2‡ × 0.003)
Cao2 = (Hgb × 1.39* × Sao2) + (Pao2 × 0.003)
Cvo2 = (Hgb × 1.39* × Svo2) + (Pvo2 × 0.003)
*Depending on institutional policy, standards between 1.39 and 1.34 are used.
†In the equation for calculation of Cc-o2, saturation is assumed to be 100% as in an “ideal” capillary with no shunt.