Compliance and Resistance Measurement
PREREQUISITE NURSING KNOWLEDGE
• Compliance is a measure of lung (and chest wall) distensibility. Conditions that decrease compliance include acute lung injury (ALI), acute respiratory distress syndrome (ARDS), pulmonary edema, atelectasis, pneumonia, obesity, pulmonary fibrosis, and kyphoscoliosis. Compliance increases with emphysema.2,5
• Resistance is a measure of how easily gases move down the airways. Conditions that adversely affect resistance include bronchospasm, secretions, and endotracheal tube size.2,5
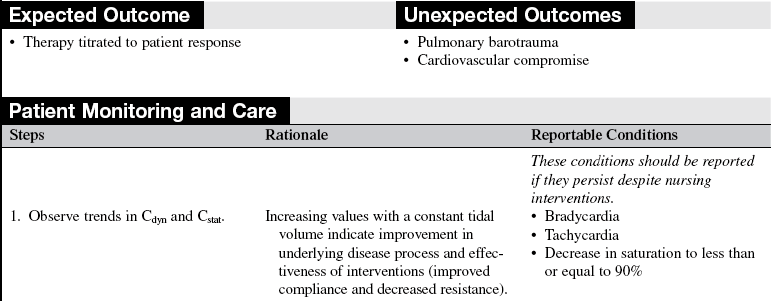
• Compliance and resistance are reflected in the patient on mechanical ventilation by changes in peak inspiratory and plateau pressures (i.e., volume modes) and by changes in volume (i.e., pressure modes). With monitoring of changes in volume per unit change in pressure (mL/cm H2O), trends can be measured and therapies adjusted.2.5
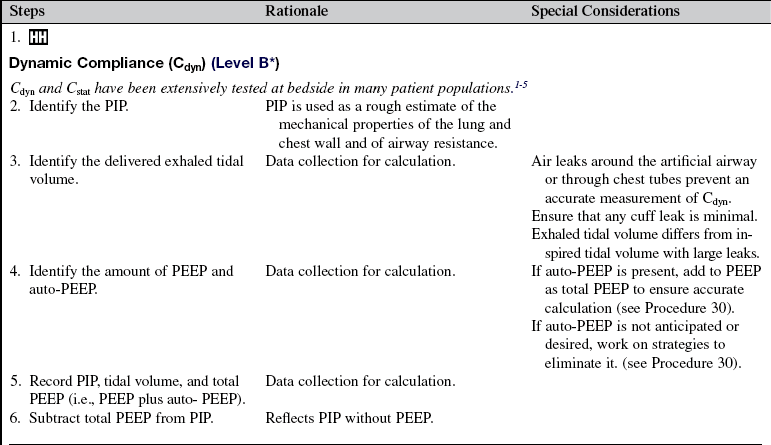
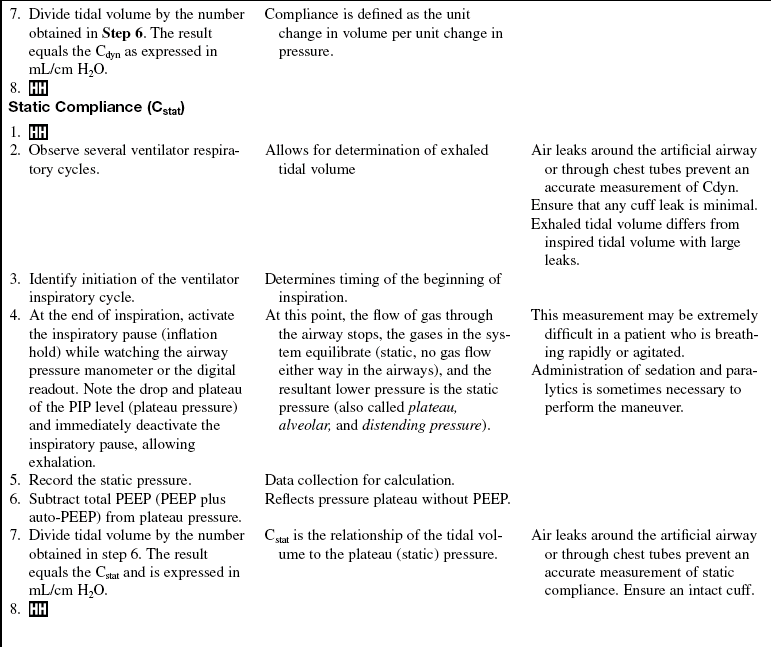
• Although spirometry or plethysmography are required for the exact measurement of airway flow resistance and lung compliance, two clinical measurements are frequently used to estimate the contributions of each in a patient on mechanical ventilation: dynamic compliance (Cdyn), which is more accurately called dynamic characteristic, and static compliance (Cstat).
 The measurements of Cdyn and Cstat are obtained while the patient is on a volume mode of ventilation. Cdyn requires that the delivered volume be divided by the peak inspiratory pressure (PIP) minus positive end-expiratory pressure (PEEP). PIP reflects both the contribution of airway resistance (how easily gases flow down the airways) and lung compliance (dispensability of the lung). Thus the measurement of Cdyn, which does not separate resistance and compliance is a measure of the overall state of the lung (inclusive of compliance and resistance). For this reason, dynamic characteristic is a more accurate term for this measurement than is dynamic compliance.2,3,5
The measurements of Cdyn and Cstat are obtained while the patient is on a volume mode of ventilation. Cdyn requires that the delivered volume be divided by the peak inspiratory pressure (PIP) minus positive end-expiratory pressure (PEEP). PIP reflects both the contribution of airway resistance (how easily gases flow down the airways) and lung compliance (dispensability of the lung). Thus the measurement of Cdyn, which does not separate resistance and compliance is a measure of the overall state of the lung (inclusive of compliance and resistance). For this reason, dynamic characteristic is a more accurate term for this measurement than is dynamic compliance.2,3,5
 Cstat is measured during a breath-hold maneuver (i.e., end inspiration). By stopping gas flow, the pressure in the system equilibrates, and the resultant pressure reflects the pressure required to distend the lungs separate from the pressure needed to move gases down the airways. The pressure measured during the breath hold is called static pressure (also called plateau, alveolar, or distending pressure). By also subtracting PEEP, this number becomes the denominator for the calculation of Cstat (i.e., tidal volume ÷ [plateau pressure − PEEP]). The normal gradient between PIP and plateau pressure is 10 to 15 cm H2O. In comparison of the difference between the two, the contribution of airway resistance is easily noted. Although PIP and plateau pressure are helpful in monitoring clinical trends, calculation of Cdyn and Cstat is most useful for quantifying the degree of improvement or compromise over time.2,5
Cstat is measured during a breath-hold maneuver (i.e., end inspiration). By stopping gas flow, the pressure in the system equilibrates, and the resultant pressure reflects the pressure required to distend the lungs separate from the pressure needed to move gases down the airways. The pressure measured during the breath hold is called static pressure (also called plateau, alveolar, or distending pressure). By also subtracting PEEP, this number becomes the denominator for the calculation of Cstat (i.e., tidal volume ÷ [plateau pressure − PEEP]). The normal gradient between PIP and plateau pressure is 10 to 15 cm H2O. In comparison of the difference between the two, the contribution of airway resistance is easily noted. Although PIP and plateau pressure are helpful in monitoring clinical trends, calculation of Cdyn and Cstat is most useful for quantifying the degree of improvement or compromise over time.2,5
• Static pressure is especially helpful to monitor when the lung is stiff (e.g., ALI or ARDS) and when great potential exists for barotrauma (e.g., pneumothorax) or volutrauma (e.g., alveolar injury).1,2,4 In a randomized controlled trial by the ARDS Network, patients ventilated with low-volume ventilation (i.e., 6 mL/kg) had a lower mortality rate than patients ventilated at larger “traditional” volumes (i.e., 12 mL/kg).4 The plateau pressures associated with the low-volume ventilation were less than 30 cm H2O. The clinical goal for patients with ARDS is to ensure a tidal volume (Vt) of 6 mL/kg and, with both volume and pressure ventilation; plateau pressure should be less than 30 cm H2O (see Procedure 35).4
• Measuring static pressure may increase the risk of barotrauma or cardiovascular compromise; this risk is low, however, because the measurement should take only a few seconds to accomplish.
EQUIPMENT
• Ventilator measurements: Vt, PIP, static pressure, PEEP, (see Procedure 35) and auto-PEEP, if present (see Procedure 30)
PATIENT AND FAMILY EDUCATION
• Inform the patent and family about the patient’s respiratory status, changes in therapy, and how to interpret the changes. If the patient or a family member requests specific information about Cdyn or Cstat, explain the relationship between the measurements and the ability to get air into the lungs and down the airway.  Rationale: Most patients and families are less concerned with diagnostic and therapeutic details and more concerned with how the patient’s condition is progressing overall.
Rationale: Most patients and families are less concerned with diagnostic and therapeutic details and more concerned with how the patient’s condition is progressing overall.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• If the patient is on a volume mode, monitor PIP for gradual or acute airway or compliance changes.  Rationale: Given a constant tidal volume, a change in PIP indicates a change in airway resistance or lung compliance.
Rationale: Given a constant tidal volume, a change in PIP indicates a change in airway resistance or lung compliance.
• If the patient is on a pressure mode, monitor tidal volume for gradual or acute airway or compliance changes.  Rationale: With pressure modes of ventilation, the pressure is stable. Thus, a change in tidal volume (or rate if the patient is breathing spontaneously) is indicative of a change in compliance or resistance.
Rationale: With pressure modes of ventilation, the pressure is stable. Thus, a change in tidal volume (or rate if the patient is breathing spontaneously) is indicative of a change in compliance or resistance.
Patient Preparation
• Ensure that the patient understands pre-procedural teachings. Answer questions as they arise, and reinforce information as needed.  Rationale: This communication evaluates and reinforces understanding of previously taught information.
Rationale: This communication evaluates and reinforces understanding of previously taught information.
• Premedicate as needed.  Rationale: This measurement may be extremely difficult in a patient who is breathing rapidly or is agitated. Sedation and paralytics are sometimes necessary.
Rationale: This measurement may be extremely difficult in a patient who is breathing rapidly or is agitated. Sedation and paralytics are sometimes necessary.
References
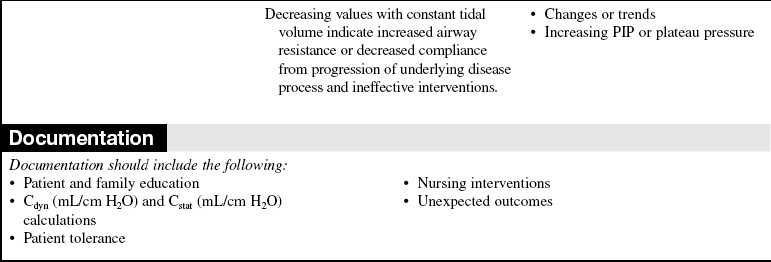
![]() 1. Dreyfuss, D, et al, High inflation pressure pulmonary edema. respective effects of high airway pressure, high tidal volume, and positive end-expiratory pressure. Am Rev Respir Dis 1988; 137:1159–1164.
1. Dreyfuss, D, et al, High inflation pressure pulmonary edema. respective effects of high airway pressure, high tidal volume, and positive end-expiratory pressure. Am Rev Respir Dis 1988; 137:1159–1164.
![]() 2. Marini, JJ, Lung mechanics determinations at the bedside. instrumentation and clinical applications. Respir Care 1990; 35:669.
2. Marini, JJ, Lung mechanics determinations at the bedside. instrumentation and clinical applications. Respir Care 1990; 35:669.
![]() 3. Pepe, PE, Marini, JJ. Occult positive end-expiratory -pressure in mechanically ventilated patients with airflow obstruction. Am Rev Respir Dis. 1982; 126:166–170.
3. Pepe, PE, Marini, JJ. Occult positive end-expiratory -pressure in mechanically ventilated patients with airflow obstruction. Am Rev Respir Dis. 1982; 126:166–170.
![]() 4. The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000; 342:1301–1307.
4. The Acute Respiratory Distress Syndrome Network. Ventilation with lower tidal volumes as compared with traditional tidal volumes for acute lung injury and the acute respiratory distress syndrome. N Engl J Med. 2000; 342:1301–1307.
5. West, JB, Respiratory physiology. the essentials. ed 8. Lippincott Williams & Wilkins, Baltimore, 2008.
Burns, S. Mechanical ventilation and weaning. In: Carlson KK, ed. AACN advanced critical care nursing. St Louis: Elsevier, 2009.
Pierce, LNB. Practical physiology of the pulmonary system. In Pierce LNB, ed. : Management of the mechanically ventilated patient, ed 2, St Louis: Elsevier, 2007.
West, JB Pulmonary pathophysiology. the essentials. Lippincott Williams & Wilkins, Baltimore, 2008.