Auto–Positive End-Expiratory Pressure (Auto-PEEP) Calculation
PREREQUISITE NURSING KNOWLEDGE
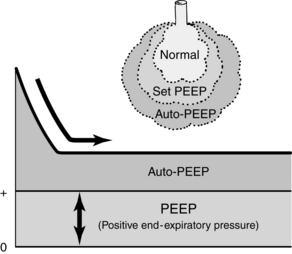
• Auto–positive end-expiratory pressure (Auto-PEEP) is often called occult because it is not set on the ventilator; instead, it is a result of inadequate exhalation time (Fig. 30-1).2–11
• Auto-PEEP is associated with high minute ventilation requirements, small-diameter endotracheal tubes, bronchospasm, long inspiratory times, high respiratory rates, and mechanical factors, such as water accumulation in the ventilator tubing.2–11
• Auto-PEEP may result in an increased work of breathing. The set sensitivity of the ventilator is referenced to the amount of set-PEEP selected by the clinician. Because auto-PEEP is not sensed by the ventilator, the patient has to generate a pressure equal to the set sensitivity plus auto-PEEP to “trigger” inspiratory flow or a breath from the ventilator.2,9
• Auto-PEEP may elevate static pressure (i.e., plateau pressure). High plateau pressures can result in barotrauma and hemodynamic compromise.9
• Auto-PEEP may be a desirable outcome of select ventilator settings (e.g., pressure-controlled inverse ratio ventilation). In these cases, the goal of auto-PEEP is to restore functional residual capacity and reduce shunt.
• Interventions to offset auto-PEEP include the use of large-diameter endotracheal tubes, bronchodilators, short inspiratory times, long expiratory times, lower respiratory rates, frequent emptying of ventilator circuit water accumulation (heated circuits may eliminate this complication), and the use of sedatives and narcotics (if the patient’s breathing pattern is such that it increases the minute ventilation). Occasionally the addition of set-PEEP is used to offset auto-PEEP. The addition of set-PEEP serves as a splint by keeping the airway open throughout exhalation, decreasing auto-PEEP.2–7,11 An example of this technique is the patient with chronic obstructive pulmonary disease in whom early airway closure during exhalation results in gas trapping.
PATIENT AND FAMILY EDUCATION
• Inform the patient and family about the patient’s respiratory status, changes in therapy, and how to interpret the changes. If the patient or family requests specific information about auto-PEEP measurements, explain the general relationship between auto-PEEP, the work of breathing, and complication risks.  Rationale: Most patients and families are less concerned with the diagnostic and therapeutic details and more concerned with how the patient’s condition is progressing overall or in relation to a specific physiologic function.
Rationale: Most patients and families are less concerned with the diagnostic and therapeutic details and more concerned with how the patient’s condition is progressing overall or in relation to a specific physiologic function.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess for the presence of auto-PEEP; have a high index of suspicion if any of the following is noted:
 Minute ventilation requirements are greater than 10 L/min.
Minute ventilation requirements are greater than 10 L/min.
 The patient has chronic obstructive pulmonary disease.
The patient has chronic obstructive pulmonary disease.
 The respiratory rate is rapid (i.e., ≥20/min).
The respiratory rate is rapid (i.e., ≥20/min).
 The inspiratory time is long (i.e., >1 second).
The inspiratory time is long (i.e., >1 second).
 Dyssynchrony exists between patient and ventilator, especially when the ventilator does not cycle with patient inspiration.
Dyssynchrony exists between patient and ventilator, especially when the ventilator does not cycle with patient inspiration.  Rationale: Auto-PEEP increases the work of breathing by increasing the threshold load to trigger inspiration. The increased work of breathing may cause fatigue.
Rationale: Auto-PEEP increases the work of breathing by increasing the threshold load to trigger inspiration. The increased work of breathing may cause fatigue.
 Auto-PEEP is present (when any of the previously listed criteria is present) and the patient is hypotensive or shows signs of barotrauma.
Auto-PEEP is present (when any of the previously listed criteria is present) and the patient is hypotensive or shows signs of barotrauma.
 Patients in status asthmaticus are at high risk for auto-PEEP. Consider the presence of auto-PEEP as the result of vigorous bagging, high ventilator rates, or large tidal volumes, especially if hypotension is present.
Patients in status asthmaticus are at high risk for auto-PEEP. Consider the presence of auto-PEEP as the result of vigorous bagging, high ventilator rates, or large tidal volumes, especially if hypotension is present.  Rationale: Auto-PEEP, similar to intentional PEEP, puts the patient at risk for barotrauma from increased intra-alveolar pressures. In patients with asthma, lung compliance is good, but airway resistance is high, which encourages dynamic hyperinflation (alveolar overdistention) and potential barotrauma. Hemodynamic compromise occurs when the increased alveolar pressure results in compression of the corresponding capillaries; decreased venous return and hypotension result.
Rationale: Auto-PEEP, similar to intentional PEEP, puts the patient at risk for barotrauma from increased intra-alveolar pressures. In patients with asthma, lung compliance is good, but airway resistance is high, which encourages dynamic hyperinflation (alveolar overdistention) and potential barotrauma. Hemodynamic compromise occurs when the increased alveolar pressure results in compression of the corresponding capillaries; decreased venous return and hypotension result.
• Auto-PEEP may not be detected in some patients with severe asthma despite its presence. This situation may occur if the end-expiratory hold maneuver is too short to allow complete equilibration of pressures and with airway obstruction. In addition, if airways are noncommunicating, as in the case of obstruction from mucus or severe bronchospasm, auto-PEEP is not able to be measured. Assume auto-PEEP in these cases. Monitoring of plateau pressure may be a better method of assessment of hyperinflation (see Procedure 31).5–7
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient understands preprocedural teachings. Answer questions as they arise, and reinforce information as needed.  Rationale: This communication evaluates and reinforces understanding of previously taught information.
Rationale: This communication evaluates and reinforces understanding of previously taught information.
References
![]() 1. Bidani, A, Tzouanakis, AE, Carenas, VJ, et al. Permissive hypercapnia in acute respiratory failure. JAMA. 1994; 272:957–962.
1. Bidani, A, Tzouanakis, AE, Carenas, VJ, et al. Permissive hypercapnia in acute respiratory failure. JAMA. 1994; 272:957–962.
2. Burns, SM, Ventilating patients with acute severe asthma. what do we really know. AACN Advanced Crit Care 2006; 17:188–193.
![]() 3. Coussa, ML, Guerin, C, Eissa, NT, et al. Partitioning of work of breathing in mechanically ventilated COPD -patients. J Appl Physiol. 1993; 75(4):1711–1719.
3. Coussa, ML, Guerin, C, Eissa, NT, et al. Partitioning of work of breathing in mechanically ventilated COPD -patients. J Appl Physiol. 1993; 75(4):1711–1719.
![]() 4. Georgopoulos, D, Giannouli, E, Patakas, D. Effects of -extrinsic positive end-expiratory pressure on mechanically ventilated patients with chronic obstructive pulmonary disease and dynamic hyperinflation. Intensive Care Med. 1993; 19:197–203.
4. Georgopoulos, D, Giannouli, E, Patakas, D. Effects of -extrinsic positive end-expiratory pressure on mechanically ventilated patients with chronic obstructive pulmonary disease and dynamic hyperinflation. Intensive Care Med. 1993; 19:197–203.
![]() 5. Leatherman, JW, McArthur, C, Shapiro, RS. Effect of -prolongation of expiratory time on dynamic hyperinflation in mechanically ventilated patients with severe asthma. Crit Care Med. 2004; 32:1542–1545.
5. Leatherman, JW, McArthur, C, Shapiro, RS. Effect of -prolongation of expiratory time on dynamic hyperinflation in mechanically ventilated patients with severe asthma. Crit Care Med. 2004; 32:1542–1545.
![]() 6. Leatherman, JW, Ravenscraft, SA, Low-measured auto-positive end-expiratory pressure during mechanical ventilation of patients with severe asthma. hidden auto-positive end expiratory pressure. Crit Care Med 1996; 24:541–546.
6. Leatherman, JW, Ravenscraft, SA, Low-measured auto-positive end-expiratory pressure during mechanical ventilation of patients with severe asthma. hidden auto-positive end expiratory pressure. Crit Care Med 1996; 24:541–546.
![]() 7. MacIntyre, NR, Cheng, KC, McConnell, R. Applied PEEP during pressure support reduces inspiratory threshold of intrinsic PEEP. Chest. 1997; 111:188–193.
7. MacIntyre, NR, Cheng, KC, McConnell, R. Applied PEEP during pressure support reduces inspiratory threshold of intrinsic PEEP. Chest. 1997; 111:188–193.
![]() 8. Pepe, PE, Marini, JJ. Occult positive end-expiratory pressure in mechanically ventilated patients with airflow obstruction. Am Rev Respir Dis. 1994; 126:166–173.
8. Pepe, PE, Marini, JJ. Occult positive end-expiratory pressure in mechanically ventilated patients with airflow obstruction. Am Rev Respir Dis. 1994; 126:166–173.
![]() 9. Rossi, A, Gottfried, SB, Zocchi, L, et al, Measurement of static compliance of the total respiratory system in patients with acute respiratory failure during mechanical ventilation. the effect of intrinsic positive end-expiratory pressure. Am Rev Respir Dis. 1985; 131(5):672–677.
9. Rossi, A, Gottfried, SB, Zocchi, L, et al, Measurement of static compliance of the total respiratory system in patients with acute respiratory failure during mechanical ventilation. the effect of intrinsic positive end-expiratory pressure. Am Rev Respir Dis. 1985; 131(5):672–677.
![]() 10. Smith, TC, Marini, JJ. Impact of PEEP on lung mechanics and work of breathing in severe airflow obstruction. J Appl Physiol. 1988; 65:1488–1499.
10. Smith, TC, Marini, JJ. Impact of PEEP on lung mechanics and work of breathing in severe airflow obstruction. J Appl Physiol. 1988; 65:1488–1499.
11. Tobin, MJ, Alex, CA, Fahey, PJ. Fighting the ventilator. In: Tobin MJ, ed. Principles and practice of mechanical ventilation. New York: McGraw-Hill, 2006.
Burns, S. Mechanical ventilation and weaning. In: Carlson KK, ed. AACN advanced critical care nursing. St Louis: Elsevier, 2009.
Pierce, LNB, Invasive and noninvasive modes and methods of mechanical ventilationBurns SM, ed.. AACN protocols for practice. care of mechanically ventilated patients. ed 2. Jones and Bartlett, Boston, 2007.
Pierce, LNB, Mechanical ventilation. indications, ventilator performance of the respiratory cycle, and inititationPierce LNB, ed. Management of the mechanically -ventilated patient, ed 2, St Louis: Elsevier, 2007.