Trauma
Edited by Peter Cameron
3.1 Trauma overview
Peter Cameron and Gerard O’Reilly
Epidemiology
Trauma is the leading cause of death from 1 to 44 years of age in developed countries. The burden of injury is especially high in developing countries, where systems of trauma care are generally non-existent [1,2]. Globally, road traffic crashes are the number one killer of young people [3]. Deaths from unintentional injury are much more common than suicide or homicide, even in the USA [1]. However, in the USA, homicide causes more deaths than suicide in the 15–24-year age group [1]; this differs from other developed countries. Suicide now causes more deaths than motor vehicle accidents (MVAs) in regions such as Australasia and the UK [4,5].
Morbidity due to injury affects a much larger group. The 2010 Global Burden of Disease Study showed that injuries cost the global population some 300 million years of health every year, causing 11% of disability-adjusted life years (DALYs) worldwide [3]. The economic and social costs are great as most victims are young and are major contributors to society through their work, family and organizational involvement.
The trauma system – background
In most developed countries, there have been significant reductions in mortality and morbidity due to injury as a result of a systematic approach to trauma care [6,7]. The majority of these reductions have resulted from prevention strategies, including seatbelt legislation, drink–driving legislation, improved road engineering, motor cycle and cycle helmet use and road safety and workplace injury awareness campaigns. Changes in both trauma system configuration and individual patient management have brought about improvements in the survival rate of those who are seriously injured, although the impact has not been as great as that of injury prevention.
Civilian interest in injury morbidity and mortality was initially most evident in the USA because of the high incidence of urban violence and road trauma and because of lessons learnt from the wars of the 20th century. Research into systems of trauma care began with epidemiological work by Trunkey and others examining trauma deaths [8]. These researchers developed the concept of a trimodal distribution of trauma deaths. Trunkey proposed that about 50% of deaths occurred within the first hour as a result of major blood vessel disruption or massive CNS/spinal cord injury. This could only be improved by prevention strategies. A second more important group (from the therapy perspective) accounted for about 30% of deaths and included patients with major truncal injury causing respiratory and circulatory compromise. The remaining 20% of patients were said to die much later from adult respiratory distress syndrome, multiple organ failure, sepsis and diffuse brain injury. Trunkey initially identified the second group as most likely to benefit from improvements in trauma system organization and it is a tribute to the effectiveness of such schemes that the number of patients dying from avoidable factors within the first few hours of injury has generally declined. In some systems, it is reported to be as low as 3% but, generally, is probably nearer to 10–15% [9,10]. Improvements in trauma system provision have resulted in a redistribution of the three groups proposed by Trunkey and it is now generally accepted that far fewer than 30% are included in the second group. In fact, more recent studies have shown that complications, such as multiple organ failure (MOF) and acute respiratory distress syndrome (ARDS), have decreased to such an extent, with improved initial management, that, in mature trauma systems, even the third peak is now minimal, with the vast majority of deaths occurring in the first 1–2 hours from major head injury and massive organ disruption [11].
Trauma care systems have been developed to ensure a multidisciplinary approach and a continuum of care from the roadside through hospital care to rehabilitation. Identifying weakness in such a system is always difficult because of the delay between cause and effect. Inappropriate management does not usually lead to immediate death: for example, a period of hypoxia may result in organ failure many hours later. Another difficulty is the relatively low incidence of death. Although this is of course to be welcomed, it does make statistical analysis more difficult when the ‘adverse event’ occurs uncommonly. Careful audit of the entire trauma process and accurate measurement of ‘input’ (i.e. injury severity) and ‘output’ (i.e. death or quality of survival) is essential if the process of trauma care is to be reviewed.
The trauma system – pre-hospital
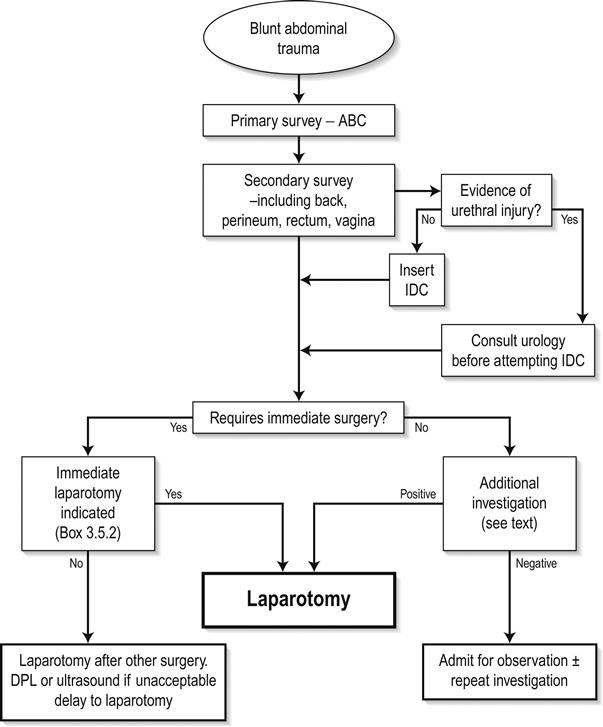
Whereas the initial work on trauma system development focused on the need for centres of expertise and trauma management, it is now accepted that the pre-hospital phase is of critical importance. The linchpin of a mature trauma system is a highly skilled and resourced pre-hospital service following the key principle of ‘the right patient to the right hospital in the shortest time’ [12]. Timely triage of the injured patient to the closest most appropriate facility is essential. Specifically, high-risk patients should be taken to a hospital capable of managing critically ill trauma patients [12]. A diagrammatic representation of one integrated trauma system, at its inception in 1999, is provided in Figure 3.1.1[13].
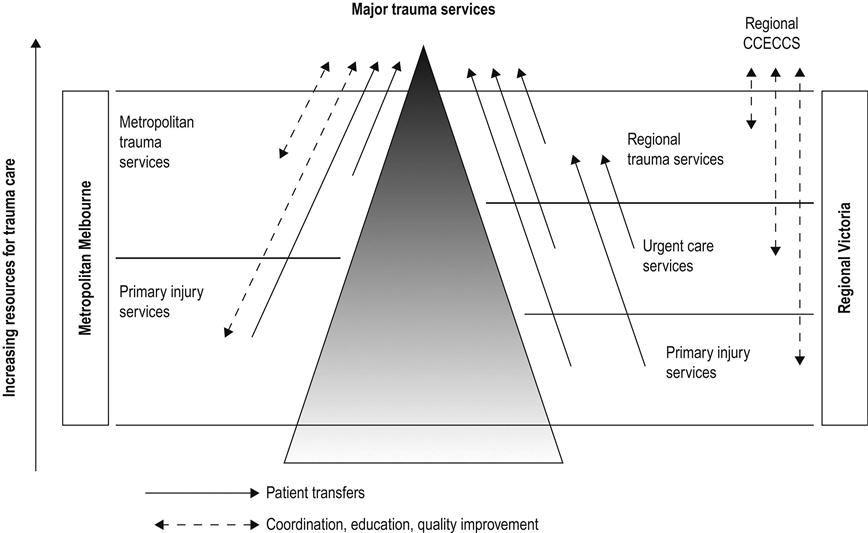
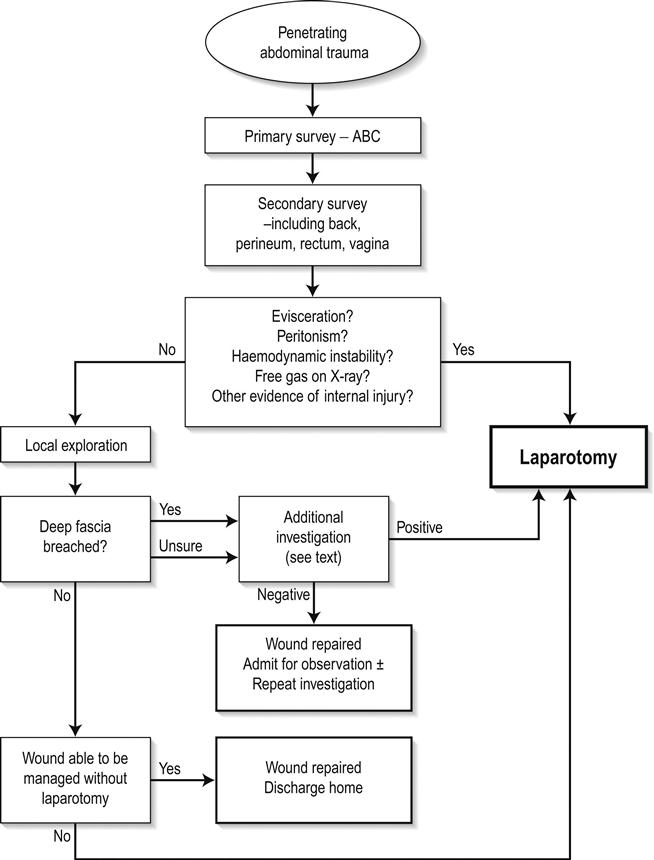
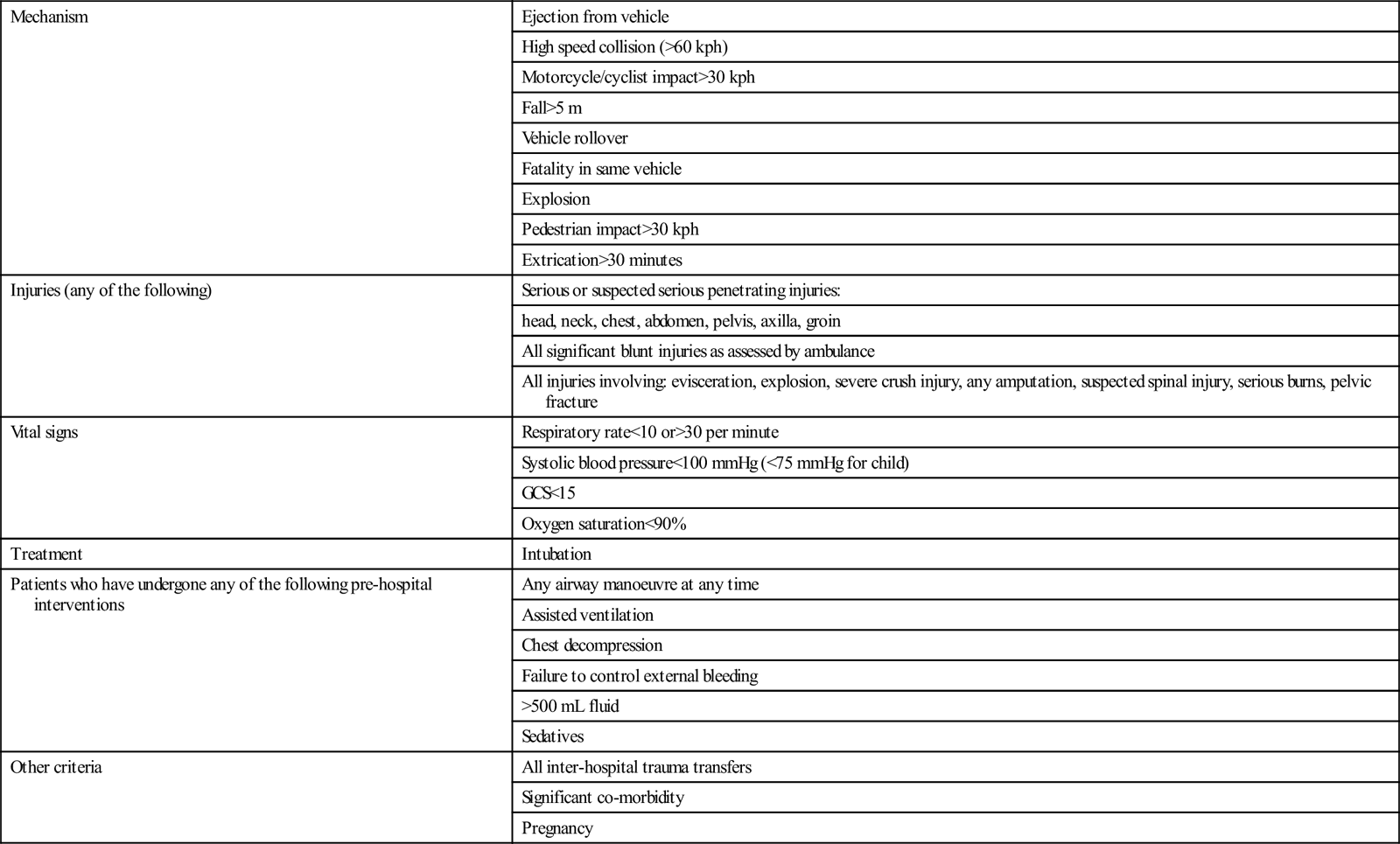
Criteria for identifying those patients who may require resuscitation at a tertiary level Trauma Centre or ‘Major Trauma Service (MTS)’ will depend on resources. In the most developed trauma systems, ‘mechanism of injury’ criteria are usually included in the pre-hospital triage tool. This ensures high sensitivity of the tool, but leads to considerable overtriage. In less-resourced settings, it may be appropriate to identify high-risk patients on the basis of abnormal vital signs and obvious major injury. The elements of a trauma system’s triage tool may include most or all of the predictors of life-threatening injury listed in Table 3.1.1.
Table 3.1.1
Predictors of life-threatening injury appropriate for use in pre-hospital trauma triage
| Mechanism | Ejection from vehicle |
| High speed collision (>60 kph) | |
| Motorcycle/cyclist impact>30 kph | |
| Fall>5 m | |
| Vehicle rollover | |
| Fatality in same vehicle | |
| Explosion | |
| Pedestrian impact>30 kph | |
| Extrication>30 minutes | |
| Injuries (any of the following) | Serious or suspected serious penetrating injuries: |
| head, neck, chest, abdomen, pelvis, axilla, groin | |
| All significant blunt injuries as assessed by ambulance | |
| All injuries involving: evisceration, explosion, severe crush injury, any amputation, suspected spinal injury, serious burns, pelvic fracture | |
| Vital signs | Respiratory rate<10 or>30 per minute |
| Systolic blood pressure<100 mmHg (<75 mmHg for child) | |
| GCS<15 | |
| Oxygen saturation<90% | |
| Treatment | Intubation |
| Patients who have undergone any of the following pre-hospital interventions | Any airway manoeuvre at any time |
| Assisted ventilation | |
| Chest decompression | |
| Failure to control external bleeding | |
| >500 mL fluid | |
| Sedatives | |
| Other criteria | All inter-hospital trauma transfers |
| Significant co-morbidity | |
| Pregnancy |
The appropriate application of pre-hospital triage guidelines relies upon adequate resourcing. In regions with developed trauma systems, pre-hospital staff are expected to provide a range of advanced life support interventions including patient intubation and chest decompression, thereby ensuring that further organ injury is limited during the pre-hospital phase. The pre-hospital care providers armed with these skills may be doctors (as in many European countries) or highly trained paramedics (as in the USA, Australia and the UK).
The trauma system – intrahospital
Preparation
Effective pre-hospital communication, usually by phone and/or radio, allows timely preparation for the arrival of a trauma patient. Proper communication includes trauma team notification, staff and trauma bay identification and the adoption of universal precautions (gloves, gowns, etc.).
Trauma team notification might occur by phone or paging system and ensures the gathering of the trauma team prior to the patient’s arrival. Members of the trauma team may vary. An example of trauma team composition and roles in a Level 1 Trauma Centre is provided in Box 3.1.1. Variations to this list may occur in different settings depending upon the availability of skilled staff and the nature of specific injuries or physiological status prior to the patient’s arrival
Trauma team call-out criteria reflect the pre-hospital trauma triage criteria (see Table 3.1.1) and should be applied rigorously. Trauma team skill, functioning and leadership are essential to achieve the best patient outcome. The appropriate skill mix is reflected by the team membership listed in Box 3.1.1. Trauma team performance, including leadership and communication, will have an impact on patient outcome.
Initial management
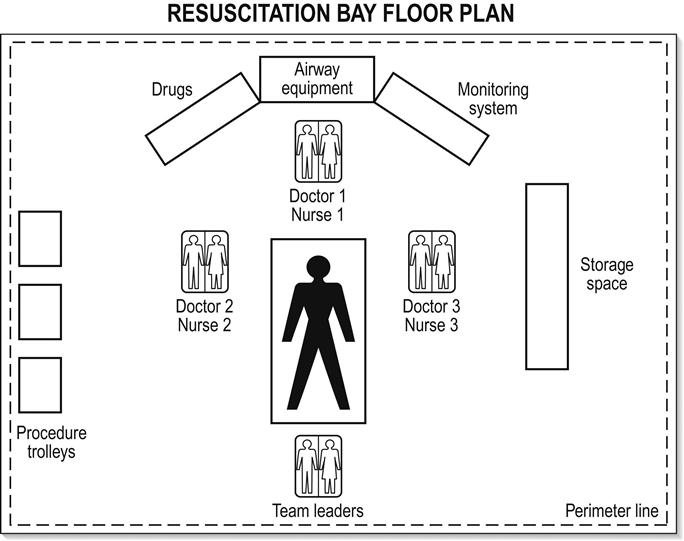
The application of a consistent systematic approach to trauma resuscitation has been widely promulgated by training programmes, such as the Advanced Trauma Life Support (ATLS) [14]. The patient is brought directly to a prepared bay, the layout of which is illustrated in Figure 3.1.2. The principles of the initial identification and management of immediately life-threatening injuries, with prioritization accorded to airway (including protection of cervical spine), breathing, circulation, (neurological) disability and exposure are applied to all injured patients. This is followed by a secondary survey involving a head-to-toe examination. In most departments, parallel processing of the patient will occur simultaneously with management of ABCDE problems.
Airway
It should be assumed that hypoxia is present in all patients who have sustained multiple injuries. Early expert airway intervention is essential. Every patient should receive initial supplemental oxygen via a well-fitting face-mask. If the airway is clear and protected, the neck should be immobilized with a semi-rigid collar but, if airway manoeuvres are necessary, it is often better to use manual inline immobilization without a collar, ensuring minimal neck movement with constant vigilance. The management of an obstructed airway in a trauma patient should be undertaken by an experienced senior clinician with significant anaesthetic experience. The first priority is to clear the upper airway by direct visualization, suction and removal of any foreign bodies. Insertion of an oropharyngeal or nasopharyngeal airway and the jaw-thrust manoeuvre are usually successful in clearing an upper airway obstruction. Insertion of a nasopharyngeal airway can be hazardous in patients with a fracture of the cribriform plate. The direction of insertion (backwards not upwards) is important. Chin lift is not recommended because it may cause additional movement of the cervical spine.
Early endotracheal intubation should be undertaken if the patient is apnoeic, has an unrelieved upper airway obstruction, has persistent internal bleeding from facial injuries, has respiratory insufficiency due to chest or head injuries or the potential for airway compromise (airway burns, facial instability, coma or seizures). Intubation may also be necessary for procedures such as computed tomography (CT) scanning or for the management of confused or disturbed patients. Any operator undertaking emergency intubation of major trauma victims should be skilled in rapid sequence induction and prepared for a difficult intubation. He/she must also be equipped with the skills for dealing with a ‘failed’ intubation (see Chapter 2.1) with a variety of interventions, including surgical cricothyroidotomy.
Breathing
Once the airway is secure, the patient’s breathing needs to be assessed. Particular attention is paid to optimizing oxygenation and maintaining normocapnia. During the primary survey, immediately life-threatening risks to breathing must be identified and dealt with. These injuries include tension pneumothorax, open pneumothorax, massive haemothorax, flail and pulmonary contusion. The specific features and management of these injuries is covered in Chapter 3.6.
Circulation
Shock is a clinical syndrome in which the perfusion of vital organs is inadequate to maintain function. Blood loss is the major cause of shock in the major trauma patient. Other less common causes of shock also need to be considered:
 Tension pneumothorax. This will cause rapid and severe disruption to the circulation.
Tension pneumothorax. This will cause rapid and severe disruption to the circulation.
 Anaphylactic shock and septic shock may coexist with hypovolaemic shock.
Anaphylactic shock and septic shock may coexist with hypovolaemic shock.
The initial stages of hypovolaemia can be difficult to detect. Reliance on systolic blood pressure to identify shock is dangerous. All patients who have sustained an injury that could be associated with significant blood loss, however remote the possibility, must be carefully monitored. In the initial phase, measurement of the clinical parameters will give some information about vital organ perfusion. However, more invasive monitoring will be required if hypovolaemia is severe or sustained.
It is essential to gain good venous access at the earliest phase in resuscitation. This is usually via two large-bore peripheral cannulae. In the absence of accessible arm veins, central venous access may be indicated. The recommended site (subclavian, jugular or femoral) depends on a number of factors. The subclavian vein is reliable in terms of patency, while the ease of access to the femoral vein is offset by its potential futility in major truncal haemorrhage. The internal jugular veins can be difficult to access in the immobilized trauma patient. Cut-downs of the saphenous veins and cubital fossa may also be used.
At the initial stages, where the blood pressure is unchanged, patients with potential blood loss can usually be managed without blood transfusion, namely crystalloid. There has been no benefit demonstrated in using non-blood colloids over crystalloids in traumatic haemorrhage [15–17]. Similarly, for hypertonic crystalloid the available data are inconclusive [18].
Where there is hypotension and tachycardia, blood transfusion should commence immediately, initially using O-negative blood and changing to group-specific or cross-matched blood as it becomes available. Chapter 3.12 covers the role and details of massive transfusion therapy in the trauma patient. Conversely, until the source of haemorrhage has been identified and haemostasis achieved, vigorous over resuscitation with fluid may actually result in a worse outcome [19,20].
The essential point is that after securing the airway and optimizing oxygenation and ventilation, the most important determinant of outcome in the major trauma patient with haemorrhagic shock is the time to definitive haemostasis. There is certainly no point in delaying surgery ‘to normalize the intravascular volume’. The major source of haemorrhage in the trauma patient must be identified early. The usual suspects are chest, abdomen, pelvis, long bone and/or external (e.g. scalp, major limb artery).
Disability
As the purpose of the primary survey is to identify immediate threats to life, the assessment for a head injury and its severity entails an examination of conscious state (Glasgow Coma Score) and neurological signs (pupils, limb weakness). If there is any risk of intracranial injury, a CT brain scan will be indicated immediately upon completion of the primary survey. Chapter 3.2 deals with the assessment and management of traumatic brain injury.
Exposure
Hypothermia is associated with worse outcomes in the major trauma patient [21]. Temperature control is now considered to be of critical importance in reducing the sequelae of major trauma (metabolic derangement, coagulopathy). The role of therapeutic hypothermia in isolated head injury remains controversial and is a subject of ongoing research. While maintaining normothermia, it is important to have fully exposed the patient, including a log roll with spinal immobilization, to enable a complete examination.
Next steps
By this stage, the trauma patient will have been received into a well-organized resuscitation area and the first life-saving procedures will have been initiated by an integrated and skilled team of doctors and nurses. Any immediately life-threatening conditions can be expected to have been identified and dealt with. Constant vigilance and reassessment are essential. Other occult injuries may be present in those patients identified with serious injuries.
While the trauma team leader continues to review the situation in the light of a constantly changing clinical scenario and, hopefully, the provision of more biomechanical data from the site of the incident, he or she should also be beginning to consider the next steps. The first of these is the calling in of other experts. Whereas it will have been clear that an airway doctor will be an essential part of the initial resuscitation team, it may be some minutes before it is known which other skills are required. Usually orthopaedic surgeons and neurosurgeons are near the top of the list. General surgery is not required as often as is commonly supposed [22], although general surgeons are often useful in coordinating ongoing care. Whichever specialty is required, the patient’s emergency problems demand experience, therefore, ‘if in doubt, refer’.
Radiographs are required at this stage. The initial films should be limited to those that will have a direct bearing on immediate management, including a chest AP view and a pelvis AP view.
Lateral X-ray of the cervical spine is no longer mandatory at this stage of assessment. Cervical immobilization is routine and it is not possible to exclude cervical injury with a lateral cervical spine X-ray. Therefore, a cervical X-ray does not alter initial management. Its utility at this stage would be to confirm an irretrievable injury, i.e. craniocervical dislocation.
Ideally, the resuscitation room should have an integrated X-ray facility but, if this is not available, portable films should be obtained. It is not appropriate to transfer a multiply injured unstable patient to a separate X-ray facility.
Other forms of imaging have become popular in localizing the source of haemorrhagic shock. The increasing availability of the focused assessment with sonography in trauma (FAST) has superseded diagnostic peritoneal lavage (DPL) as the bedside adjunct for detecting intraperitoneal haemorrhage.
Following the primary survey and investigations deemed necessary, the patient requires a secondary survey, the full head-to-toe examination for injuries not classified as immediately life-threatening.
Subsequent chapters deal with individual trauma problems, but it is essential that throughout the patient’s stay in hospital a single clinician has overriding responsibility for his or her care. In the resuscitation area, this is the ‘team leader’, who may be from any trauma-related discipline. Handover to the clinician responsible for ongoing care must be comprehensive, timed and well documented.
Trauma audit
Trauma kills people in a variety of ways; hence no one department in a hospital will see a large number of deaths. Many trauma victims die before they reach hospital, some in the ED and others scattered through the inpatient specialties and in intensive care. Hence from any one clinician’s perspective, trauma is not an outstanding problem. However, when looked at from a public health perspective, it is clearly a major issue, not least because some of the deaths are avoidable. Identifying these and the much more difficult-to-define group of patients who survive but whose outcome is not as good as expected is a major problem.
The most important variables to measure are the extent of the anatomical injury, the degree of physiological derangement that results, age and the previous well-being of the patient. All these have a direct effect on outcome and must therefore be measured before any comment can be made about the process of care. Outcome itself must also of course be measured. This is relatively easy in terms of mortality. However, disability is a much more difficult issue and, currently, there are no universally accepted measurement tools. The Glasgow Outcome Scale (GOSE) [23, 24], and the Short Form–36 (SF36) questions [25] are available tools that have been used. As 90% of major trauma patients survive their injury in a mature trauma system, it is important to measure disability and quality of life following major trauma when comparing outcomes [26].
Trauma audit was first formalized by Champion at the Washington Hospital Centre in the 1970s, using the Trauma Injury Severity Score (TRISS) methodology [27,28]. Most current trauma systems are now audited using some approach to examining risk-adjusted mortality. Injury severity adjustment, allowing intra- and intersystem comparison, usually requires measures of anatomical injury (e.g. Injury Severity Score), physiological effects (e.g. Revised Trauma Score) and age.
Trauma in developing countries
Globally, national governments are beginning to recognize the burgeoning human and economic cost of trauma, particularly road trauma. The public health achievements of the developed countries (seatbelts, helmets, alcohol and speed restrictions) are being implemented and, similarly, governments of developing countries are looking to implement trauma systems [29,30].
Research in developing countries reinforces the benefits of trauma systems previously described in countries with established emergency medical systems. For example, evidence indicates that people with life-threatening but potentially treatable injuries are up to six times more likely to die in a country with no organized trauma system than in one with an organized, resourced trauma system [31]. Trauma system development requires trauma outcome measurement [32,33]. As such, developing countries are likely to adopt trauma registries over the next several decades in an attempt to track the burden of trauma and the impact of system-wide interventions.
As developing countries embark upon trauma system development, it is becoming increasingly important to access standardized trauma care education through intensive short-courses. Advanced Trauma Life Support (ATLS) has been widely used. Other courses (such as Primary Trauma Care (PTC)) have also become popular in the developing world. Such courses are often less expensive and more flexible than ATLS.
3.2 Neurotrauma
Gerard O‘Reilly, Lee Wallis and Peter Cameron
Introduction
Neurotrauma is a common feature in the presentation of multisystem trauma, particularly when associated with motor vehicle accidents and falls. Over 50% of trauma deaths are associated with head injury. The implications for the health system are enormous, with an annual rate of admission to hospital wards associated with head trauma approaching 300 per 100 000 population [1] and twice this in the elderly [2]. The long-term sequelae of moderate and severe neurotrauma are a major health resource drain and the morbidities associated with mild brain injury are becoming clearer.
Advances in preventative strategies, trauma systems, resuscitative therapies and rehabilitation management have improved outcomes. However, neurotrauma remains a serious health issue, predominantly affecting the productive youth of society.
Pathogenesis
Primary brain injury occurs as a result of the forces and disruptive mechanics of the original incident: this can only be avoided through preventative measures, such as the use of bicycle helmets.
Secondary brain injury is due to a complex interaction of factors and typically occurs within 2–24 hours of injury [3]. A principal mechanism of secondary injury is cerebral hypoxia due to impaired oxygenation or impaired cerebral blood flow. Cerebral blood flow is dependent on cerebral perfusion pressure (CPP), mean arterial systemic blood pressure (MAP) and intracranial pressure (ICP).
< ?xml:namespace prefix = "mml" />
Intracranial pressure may be raised as a result of the mass effect of the haemorrhage or by generalized cerebral oedema. Cerebral vasospasm further reduces cerebral blood flow in patients in whom significant subarachnoid haemorrhage has occurred.
Cellular dysfunction is a result of both primary and secondary mechanisms and involves sodium, calcium, magnesium and potassium shifts across the cell membrane, the development of oxygen free radicals, lipid peroxidation and glutamate hyperactivity. Excessive release of excitatory neurotransmitters and magnesium depletion also occur [4].
Classification of primary injury in neurotrauma
Skull fracture
The significance of skull fracture is not related to the specific bony injury but rather the associated neurotrauma. Fractures in the region of the middle meningeal artery in particular may be associated with acute extradural haemorrhage. Fractures involving the skull base and cribriform plate may be associated with CSF leak and the risk of secondary infection. Depressed skull fractures may compress underlying structures, cause secondary brain injury and require surgical elevation. Injury to underlying structures may result in secondary epilepsy.
Concussion
Concussion is a transient alteration in cerebral function, usually associated with loss of consciousness and often followed by a rapid recovery. The proposed mechanism is a disturbance in the function of the reticular activating system. Post-concussive syndromes, including headache and mild cognitive disturbance, are common [5,6]. Symptoms, particularly headache, are usually short-lived but may persist. ‘Second-impact syndrome’ describes a greater risk of significant re-injury following an initial injury causing a simple concussion. It is likely to be due to diffuse cerebral swelling [7]. In animal models, concussion may be associated with modest short-term increases in intracranial pressure and disturbances in cerebral cellular function [8].
Contusion
Cerebral contusion is bruising of the brain substance associated with head trauma. The most common mechanism is blunt trauma. Forces involved are less than those required to cause major shearing injuries and often occur in the absence of skull fracture. Morbidity is related to the size and site of the contusion and coexistent injury. Larger contusions may be associated with haematoma formation, secondary oedema or seizure activity. The most common sites for contusions are the frontal and temporal lobes [9].
Intracranial haematoma
Extradural
Extradural haematoma (EDH) is uncommon but classically associated with fracture of the temporal bone and injury to the underlying middle meningeal artery. Haemorrhage subsequently occurs, stripping the dura from the skull and expanding to cause a rise in intracranial pressure and eventually uncal herniation and death. Haemorrhage may be from vessels other than the middle meningeal artery (e.g. brisk arteriolar or venous bleeding). Signs will depend on the site of the haematoma.
Subdural
Subdural haematomata (SDH) may have an acute, subacute or chronic course. It generally follows moderate head trauma with loss of consciousness. In the elderly, SDH may be associated with trivial injury and, in children, with shaking (abuse) injury. Haemorrhage occurs into the subdural space, slowly enlarging to cause a space-occupying collection whose functional implications will vary according to location. Acute subdural haemorrhage carries a high mortality (>50%), similar to acute EDH. Subacute and chronic SDH is associated with a degree of cerebral dysfunction, headache or other symptomatology and is associated with a significantly lower mortality (up to 20%) [10].
Intracerebral
As with cerebral contusion, the most common sites of intracerebral haemorrhage associated with trauma are the temporal and posterior frontal lobes. Effects on function are variable, depending on the site. Intracerebral haemorrhage may progress from an initial contusion or be secondary to altered vascular characteristics. Symptom development and complications may be delayed as the size of the haemorrhage increases over time.
Subarachnoid and intraventricular haemorrhage
Subarachnoid blood is relatively common after major head injury. Intraventricular haemorrhage may also be evident. As in non-traumatic settings, the presence of subarachnoid blood may lead to cerebral vasospasm and secondary ischaemic brain injury.
Diffuse axonal injury
Diffuse axonal injury (DAI) is the predominant mechanism of injury in neurotrauma, occurring in up to 50% of patients [11]. Shearing and rotational forces on the axonal network may result in major structural and functional disturbance at a microscopic level. Disturbance to important communicative pathways sometimes results in significant long-term morbidity, despite non-specific or minimal changes on computed tomography (CT) scanning. The exact pathogenesis of diffuse axonal injury is incompletely understood. Specific injury in the regions of the corpus callosum and midbrain has been proposed; however, DAI is believed to be the mechanism for persistent neurological deficits seen in head-traumatized individuals with normal CT scans [12].
Penetrating injury
Penetrating neurotrauma is characterized by high levels of morbidity and mortality. This is especially true of gunshot wounds. Exposure of cerebral tissue through large compound wounds or through basilar skull structures is associated with a dismal outlook. Penetrating injury in the periorbital and perinasal regions is associated with high risk of infection.
Epidemiology
Neurotrauma is surprisingly common. In some settings, more than 30% of the population have suffered from a trauma brain injury. In addition to being a major cause of death in trauma, neurotrauma leads to significant morbidity. More than 40% of those who have sustained a traumatic brain injury will have residual disability one year later [13].
Common causes include motor vehicle accidents (including vehicle versus pedestrian and bicycle collisions), falls, assault and firearms. In young males, alcohol is often involved.
Prevention
Primary prevention of neurotrauma depends on the cause. Most preventative strategies are directed at vehicular traffic and include speed-calming measures, in-car safety devices and bicycle helmets. Improving roadside lighting and enhancing pedestrian visibility contribute to reduction of injury in this group.
Prevention of secondary injury involves maintenance of cerebral perfusion and oxygenation and is addressed under clinical management.
Clinical features
Definition
Neurotrauma may be classified according to severity as minimal, mild, moderate or severe (Box 3.2.1) [14]. Such a classification allows for directed investigation and management, but there is clearly a continuum of injury within the spectrum of neurotrauma.
History
A detailed history of the mechanics of the trauma is essential. This should be followed by consideration of time courses, pre-hospital care, pre-sedative and pre-relaxant neuromuscular function and episodes and duration of hypotension or other decompensation. A history of previous health problems, allergies, medications and social setting is desirable.
Primary survey
As with all trauma patients, the initial assessment and therapy must be directed at maintenance of airway, ventilation and circulatory adequacy along standard Advanced Trauma Life Support (ATLS) principles. Early assessment of neurological disturbance using the Glasgow coma score (GCS) or AVPU scale (Alert: GCS 14–15; response to Verbal stimuli: GCS 9–13; response to Painful stimuli: GCS 6–8; or Unresponsive: GCS 3–5) is important. Simultaneous protection of the cervical spine by immobilization is fundamental. This management should commence in the pre-hospital setting and the level of care be maintained.
The greatest risks to the patient with a moderate to severe head injury are hypoxic injury and deficient cerebral perfusion due to systemic hypotension.
Secondary survey
A full secondary survey, including log-roll, should follow.
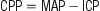
Clinical assessment of the neurological status of head-injured patients commences with formal documentation of the GCS (Table 3.2.1). The maximum score is 15 and the minimum 3. Coma may be defined in terms of the GCS, in which patients have a total score of 8 or less:
 Fail to show eye opening in response to pain (eye-opening response=1)
Fail to show eye opening in response to pain (eye-opening response=1)
 Fail to obey commands (best motor response=5)
Fail to obey commands (best motor response=5)
 Make at best only incomprehensible sounds (best verbal response=2).
Make at best only incomprehensible sounds (best verbal response=2).
Table 3.2.1
| Best motor response | |
| Obeys command | 6 |
| Localizes to pain | 5 |
| Withdraw to pain | 4 |
| Abnormal flexion to pain | 3 |
| Abnormal extension to pain | 2 |
| Nil | 1 |
| Best verbal response | |
| Orientated | 5 |
| Confused | 4 |
| Uses inappropriate words | 3 |
| Incomprehensible sounds | 2 |
| Nil | 1 |
| Eye opening | |
| Spontaneously | 4 |
| To verbal command | 3 |
| To pain | 2 |
| Nil | 1 |
Examination of pupillary responses, particularly in the unconscious patient, is important as an indicator of increasing intracranial pressure; a non-responsive dilated pupil indicating ipsilateral herniation. However, a more common cause of abnormal pupil reactions in head injury is the presence of direct ocular trauma.
A general neurological examination, including reflexes, should be performed; the degree to which cooperation is possible and lateralization of signs being particularly important to document. Consideration of the pre-injury mental state is important, particularly where drug or alcohol intoxication is possible.
Clinical investigations
Minimal–mild head injury
In head injury associated with loss of consciousness or amnesia and a GCS of 14–15, CT scanning will demonstrate a relevant positive scan (i.e. cerebral contusion, haematoma, oedema, pneumocephalus) in 7–12% and a subsequent craniotomy rate of 1–3% [15–18].
On the weight of research evidence, current ED investigation of mild head injury should include CT scanning in all patients in this group [14,19–22]. Certain high-risk groups (such as the intoxicated, the elderly (>65 years), anticoagulated or demented patients) warrant CT scanning even after minimal presumed or possible head injury.
Despite considerable research within the minimal–mild head injury group, reliable risk stratification has not been achieved. The Canadian Head Rules detail five high-risk criteria for neurosurgical intervention in patients with GCS 13–15 and mild head injury [23]. The NICE head injury rules were based in part on the Canadian rules [24]; the NEXUS II [25] investigators showed that development of a simple head injury CT rule that is both sensitive and specific is extremely difficult. There have been conflicting results as to which has the best predictive power in adults and children, however, each has its critics for over-scanning [26,27].
Cervical spine imaging is indicated if the patient has neck pain, neurological abnormality, altered conscious state, intoxication or significant distracting injury.
Moderate–severe head injury
Urgent CT scanning is the investigation of choice in moderate-to-severe neurotrauma (GCS of 3–13); however, other investigations and therapy may take priority in the patient with multisystem trauma, particularly in the presence of unresponsive haemorrhagic shock.
In the absence of a CT scan, consultation with a neurosurgeon or early transfer to an appropriate facility is essential.
Imaging of the cervical spine is indicated in all patients with moderate to severe neurotrauma. A significant proportion of patients with severe head injury will have cervical spine fractures.
Treatment
Minimal–mild head injury
All patients with mild head injury must be counselled appropriately and discharged with written advice in the care of a responsible adult. Specific advice must be provided regarding expected duration of symptoms, possible risks or delayed complications and reasons for re-presentation to the ED (Box 3.2.2). Information should also be given about the second-impact syndrome and exclusions from sporting activity.
Follow up by a local medical officer should be arranged and neuropsychological assessment may be warranted for high-risk groups. Patients should be cautioned about making major life, occupational and financial decisions until they are free of post-concussive symptoms.
In minimal and mild head injury, a normal CT scan and the absence of neurological abnormality are reasonable criteria for patient discharge [3]. It is essential to assess for ongoing post-traumatic amnesia (PTA), as this is frequently overlooked in the ED. A simple screen to use is the modified Westmead PTA scale [6]. In the presence of these criteria, the persistence of mild symptoms (e.g. mild headache, nausea, occasional vomiting) is common and patients should be advised accordingly. In adults, such symptoms may be treated with mild analgesics (paracetamol, aspirin) and antiemetics (metoclopramide, prochlorperazine) and the patient discharged when comfortable. Advising patients that there will be problems with post-concussive symptoms (including short-term memory and information processing) and providing them with written material has been shown to improve outcomes at 3 months [6,28].
Currently there is no drug to treat the primary pathology in mild and minor head injury [29].
Moderate–severe head injury
Priority in the management of moderate to severe neurotrauma is given to maintenance of the airway and an adequate cerebral perfusion pressure. Hypotension (SBP<90) and hypoxia (PaO2<60 [8 kPa]) should be corrected immediately [30]. Control or modification of intracranial pressure has a place in the emergency management of neurotrauma. Avoidance of secondary brain injury and associated cerebral swelling is the mainstay of such therapy.
Intracranial pressure monitoring is generally indicated in patients with severe head injury (GCS<8) who remain comatose. Institutional variability exists in methods for measurement, as do specific indications for monitoring. Elevation of the head of the bed to 30° will reduce ICP modestly without altering CPP.
Mannitol (0.5–1.0 g/kg IV) may produce a short-term reduction in ICP. Mannitol causes an osmotic dehydration which is non-selective. Complications of mannitol therapy include fluid overload, hyperosmolality, hypovolaemia and rebound cerebral oedema. Mannitol may be used as a temporizing measure to enable a patient with a surgically remediable lesion to get to theatre.
Routine use of hyperventilation in head injury is contraindicated. Hypocarbia reduces cerebral blood flow (and ICP) through vasoconstriction which, if extreme, may reduce CPP to the point of exacerbation of secondary brain injury [31].
Anticonvulsant prophylaxis (phenytoin 15–18 mg/kg IV over 30–60 minutes) is indicated for the prevention of seizures within the first week after injury [32]. Seizures are managed acutely using standard therapies and guidelines (including benzodiazepines and phenytoin). The use of barbiturates, endotracheal intubation and mechanical ventilation may be indicated for status epilepticus or seizures that are refractory to therapy.
Antibiotic prophylaxis is indicated for compound fractures. Tetanus immunoprophylaxis is given as part of routine wound care. Steroid therapy has had varied support but is not recommended [33]; in 2005, the CRASH collaborators reported conclusively that intravenous corticosteroids should not be used in the treatment of head injury [34].
There has been considerable interest and experimental endeavour with regard to cerebral protection and salvage therapies. To date, no benefit has been demonstrated in the administration of aminosteroids, amino acids or monoamine antagonists in patients with head injury [35–37] and the role of calcium channel blockers remains unclear [38]. More recent research demonstrated worse outcomes for patients with diffuse traumatic brain injury who had a decompressive craniectomy [39]. The role of hypothermia is controversial; while animal studies have shown a benefit, prospective studies have shown either harm or no harm [40,41]. In summary, general supportive therapy, including the maintenance of thermoregulation, hydration, pressure care and nutrition are the mainstays of therapy.
Resuscitation in neurotrauma
There are two features of prime importance to resuscitation in patients suffering neurotrauma:
With elevation of intracranial pressure and loss of autoregulation of cerebral circulation, relatively higher systemic blood pressures are required. The practice of minimal-volume resuscitation has no place in the patient with serious neurotrauma. Standard approaches to the management of hypovolaemia in head- injured patients should be adopted. The use of hypertonic solutions in resuscitation (including hypertonic saline) has been studied with variable conclusions [42]. But the only randomized controlled trial performed with hypertonic saline showed no improvement in outcome [43]. Albumin has also been shown to have detrimental effects in severe traumatic brain injury [44].
Indications for intubation and ventilation of the neurotrauma patient are inadequate ventilation or gas exchange (hypercarbia, hypoxia, apnoea); inability to maintain airway integrity (protective reflexes); a combative or agitated patient; and the need for transport where the status of the airway is potentially unstable (between hospitals, to CT, to angiography, etc.).
Disposition
In patients with minimal–mild head injury, recommendations with regard to a ‘safe’ period of observation, need for hospital admission or predictive value of injury mechanism are not consistent. Rural and isolated settings present logistic difficulties in the management of this group. Careful observation for a prolonged period is a reasonable alternative and early neurosurgical consultation, together with a low threshold to transfer to a neurosurgical centre, is prudent.
Patients with moderate to severe neurotrauma require hospital admission, preferably under the care of a neurosurgeon in a specialized neurosurgical unit or ICU. Rehabilitation and social readjustment is a focus of therapy from early in the clinical course.
Inter-hospital transfer of patients with significant neurotrauma requires the attendance of skilled transfer staff and the maintenance of level of care during transfer. Airway management must anticipate the potential for the patient to deteriorate en route. The presence of pneumocephalus precludes unpressurized (high) altitude flight. The use of teleradiology and neurosurgical consultation will be of value in the management of the remote head-injured patient.
Prognosis
The level of residual neurological impairment is a function of the severity of the degree of trauma and quality of care. A poor outcome is associated with prolonged pre-hospital time, delay of transfer to the appropriate facility, admission to an inappropriate facility and delay in definitive surgical treatment.
Overall mortality in severe head injury is of the order of 35%. A lower GCS at presentation is associated with a worse outcome. Approximately half the patients who remain comatose with GCS<9 for longer than 6 hours will die [12]. Acute subdural haematoma and diffuse axonal injury producing persistent coma are associated with the vast majority of neurotrauma deaths. Early neurological abnormalities are, however, not reliable prognostic factors and an initial period of maximally aggressive therapy is indicated in patients with closed neurotrauma.
Acknowledgements
The chapter’s authors for this edition would like to acknowledge the important contribution of authors for previous editions, including Dr Marcus Kennedy.
3.3 Spinal trauma
Pieter van Driel
Introduction
Spinal cord injury is one of the most disabling traumas, causing major and irreversible physical and psychological disability to the patient and permanently affecting their lifestyle. The emotional, social and economic consequences affect the individual, family, friends and society in general.
Approximately 2% of adult victims of blunt trauma suffer a spinal injury and this risk is tripled in patients with craniofacial injury [1].
Motor vehicle collisions, falls and sporting injuries – notably diving and water sports – are the major causes of acute spinal cord injury in Australia [2]. Road traffic accidents account for about half of all spinal injuries. Despite the work to minimize spinal injuries in contact sports, such as rugby, serious spinal cord injuries still occur [2]. Spinal injuries occur mostly in young people, but minor falls in the elderly or low-impact injuries in people with pre-existing bony pathology can also cause spinal cord damage. Spinal cord injury due to pathological vertebral fractures may be the first presentation of malignancy.
Observations from two studies [3,4] suggest that possibly preventable neurological deterioration may be due to one or more of the following:
Pathophysiology
Level of vertebral injury
The level of neurological injury in patients who sustain spinal injuries is variously reported. In studies from Victoria and New South Wales [4,5], the distribution of the level of injuries was cervical 60%, thoracic 30%, lumbar 4% and sacral 2%.
Spinal cord injuries occur most commonly at the level of the 5th, 6th and 7th cervical vertebrae, largely because of the greater mobility of these regions. The C5–6 and C6–7 levels account for almost 50% of all subluxation injury patterns in blunt cervical spinal trauma [6].
Associated injuries
There are three noteworthy observations [3,5] from associated injuries in patients with spinal injury:
 Owing to the mechanism of injury, many patients with spinal injuries often have other associated injuries, including head, intrathoracic or intra-abdominal injuries, which may modify management priorities [5].
Owing to the mechanism of injury, many patients with spinal injuries often have other associated injuries, including head, intrathoracic or intra-abdominal injuries, which may modify management priorities [5].
Spinal trauma might result in several injuries directly related to the spinal cord. Specific injuries, such as vertebral injuries, spinal shock, spinal cord injuries and their neurological symptoms, are described later in this chapter.
Autonomic nervous system effects of spinal cord damage
Autonomic nervous system effects are mentioned here as important pathophysiological mechanisms must be understood to deliver optimum care and treatment to patients with spinal cord injuries.
The whole of the sympathetic nervous system and the pelvic parasympathetic outflow is transmitted in the spinal cord. In an injury higher than the upper thoracic vertebrae, there is significant impairment of total body sympathetic and pelvic parasympathetic functions. The extent and severity of autonomic dysfunction is dependent on the segmental level(s) and the extent or completeness of the neurological insult.
Direct effects
Direct effects include manifestations related to the cardiovascular, gastrointestinal, urogenital and thermoregulatory systems.
Cardiovascular effects
In complete quadriplegia, sympathetic denervation causes relaxation of resting vasomotor tone, resulting in generalized systemic vasodilatation. It is recognized by dry extremities with variable warmth and colour during initial assessment. In males, there may be penile engorgement or priapism. Owing to the peripheral vasodilatation, there is a drop in total peripheral resistance, with consequent hypotension (neurogenic shock). Under normal circumstances, this would result in a baroreceptor response in order to achieve compensation. However, as the effector arm of the sympathetic nervous system is paralysed, the normal compensatory effects of tachycardia and vasoconstriction do not occur. The vagus nerve carrying parasympathetic supply to the heart is unopposed, with resultant bradycardia. The higher and more complete the spinal cord injury, the more extensive the autonomic dysfunction.
The usual symptoms and signs of the shock process in response to hypovolaemia cannot occur, as tachycardia and vasoconstriction are mediated by the sympathetic nervous system, which has been interrupted by the high spinal cord lesion.
Gastrointestinal effects
Following spinal cord injury, a paralytic ileus develops. This is usually self-limiting and recovers over 3–10 days. Paralysis of sphincters occurs at the lower end of the oesophagus and at the pylorus; as a consequence, passive aspiration of the stomach contents, especially of fluid, is a potential problem. Furthermore, owing to thoracic and abdominal wall muscle paralysis, the capacity to cough and hence clear the airway is diminished. In quadriplegia and high paraplegia, occult fluid aspiration due to passive regurgitation of retained gastric content may not be recognized. The airway therefore requires close observation and active protection. A nasogastric tube must be inserted and gastric contents drained.
Urinary effects
Urinary retention is partly the consequence of acute bladder denervation and, in the early post-injury phase, due to spinal shock. Catheter insertion is required to prevent overdistension of the bladder in order to optimize recovery. It also permits measurement of urinary output.
Thermoregulatory effects
Following cervical or upper thoracic spinal cord injury, the spinal patient effectively becomes poikilothermic. In a cold environment, they are unable to vasoconstrict to conserve heat or shiver to generate heat. The patient is already peripherally vasodilated which promotes loss of heat and lowering of body temperature. In the warm environment, although the patient is already peripherally vasodilated, the capacity to sweat is sympathetically controlled and therefore lost.
Pre-hospital issues
Extrication and immobilization
Emergency medical services (EMS) personnel are sent to see trauma patients in difficult circumstances. Patients, for instance, could be stuck in vehicles, (partially) submersed in water or found in small and inconvenient places. These circumstances often make it hard initially to immobilize fully the (cervical) spine. Several devices have been developed to extricate a trauma patient from a crashed vehicle with maximum in-line protection of the spinal column.
Restlessness in patients, due to hypotension, hypoxia, drug abuse, anxiety or other causes, makes it even harder to immobilize fully the spine. Depending on local protocols, training and skills, EMS personnel should either be able to treat the cause of the restlessness or sedate these patients in order to immobilize the (cervical) spine.
Next to resuscitation interventions following the ABCDE approach, focus should be given to in-line immobilization of the total spine. Trauma patients should remain in immobilization devices until spinal trauma has been excluded and splinting of specific injuries can be effected. However, they do not need to be left in the devices applied by pre-hospital care providers: these are structured to provide rigid immobilization for initial stabilization and transport. Nor should they be left tied to spine boards or wrapped in extrication devices, as these are uncomfortable and can cause unwanted cutaneous pressure injuries. Tight webbing and wraps can interfere with respiratory excursion. In general, the pre-hospital devices are removed and replaced with more appropriate ones for the emergency department environment.
Immobilization of the spine
Immobilization of the spine continues to be a standard of care. However, the effectiveness of common techniques is largely unproven and there are side effects from unnecessary immobilization. The Cochrane Collaboration failed to infer a potential for good, in spite of the fact that splinting any suspected bony injury is universally considered standard management [7].
Although failure to detect and immobilize cervical spine injury in hospitalized patients is associated with a 7–10-fold risk of secondary neurological injury, it is unclear whether the secondary injuries occur in the out-of-hospital setting and can be prevented by spinal immobilization devices. Despite this, there is evidence that not immobilizing the cervical spine is not associated with an increase in neurological injury [8]. A benefit of applying a cervical collar can be to alert the medical team to the potential presence of spinal injury. The weight of opinion is in favour of splinting devices until spinal injury can be eliminated. Therefore, immobilization and the use of splinting devices remains commonplace in clinical practice.
Several types of devices exist and are used either alone or in combination. The common combination in out-of-hospital spine care comprises a cervical collar, spine board and associated padding to ensure a normal curvature of the spine. Other devices, such as extrication devices, not primarily designed as spinal immobilizers, have been used to splint the spine in special circumstances.
The various devices and techniques are variably effective and do not completely immobilize. However, they have generally been tested on uninjured subjects with normal muscular tone and posture.
As mentioned before, spinal immobilization can be harmful. Standard spinal immobilization applied to otherwise healthy subjects resulted in significant spinal pain in 100% of subjects [9]. Spinal immobilization can mask life-threatening injuries. Cervical collars have been shown to increase intracranial pressure. Spinal immobilization restricts pulmonary function in healthy adults and children. Prolonged immobilization of the cervical spine with rigid pre-hospital rescue collars and other immobilization devices may unnecessarily add to patient discomfort and the need for ongoing spinal nursing. Tissue perfusion in the sacral area is adversely affected within 30 minutes on a rigid spinal board [10]. This predisposes to pressure area problems and problematic decubitus ulceration. Therefore, upon arrival of the patient in the Emergency Department (ED), the pre-hospital devices should be removed as soon as possible (usually immediately after the primary survey) and replaced with more appropriate ones for the emergency department environment.
First treatment options
Primary survey
Patients presenting with a potential spinal cord injury are managed in keeping with the approach for any major trauma patient. Therefore, a standard approach of primary survey, resuscitation, secondary survey and definitive management is adopted.
Specific attention should be paid to the following issues important in the assessment and treatment of patients with (potential) spinal injury.
Airway
Assessment of the airway is vital in the management of suspected spinal cord injury, especially when the cervical spine is involved. Passive regurgitation and aspiration of fluid stomach contents may occur as a result of blunting or absence of cough, gag and vomiting responses. This is especially the case with higher cervical injuries. Therefore, the insertion of a nasogastric tube is of vital importance in minimizing the likelihood of aspiration. In quadriplegia and high paraplegia, unopposed vagal action owing to functional total or near-complete sympathectomy predisposes the patient to bradycardia on vagal stimulation of the pharynx. It is important that such patients have ECG monitoring and that atropine be immediately available to block these effects. Pretreatment with atropine prior to manipulation of the upper airway is a consideration.
Advanced airway management
Early endotracheal intubation and assisted ventilation should be considered in patients with quadriplegia and high paraplegia. Regular assessment of respiratory status is undertaken and includes continuous pulse oximetry and frequent vital capacity measurement, in order to detect fatigue.
Blind nasal or endoscopic-assisted intubation under local anaesthetic is the preferred mode of non-emergency intubation. Additionally, every manipulation to the head and neck of the patient should be done with extreme caution to minimize further damage to the vulnerable spine.
The literature suggests that video- laryngoscopy results in less overall movement during intubation and it does not seem to have an impact on cord injury.
Since the rocuronium antagonist sugammadex has become widely available, rocuronium has become the muscle relaxant of first choice in many settings because of the beneficial side-effect profile. Suxamethonium is therefore used less often, but still acceptable for a rapid-sequence intubation in the emergency setting. The hyperkalaemia associated with denervation is a concern in injuries more than 10–12 hours old (see Chapter 2.1).
Breathing
Ventilation in patients with spinal cord injury may be affected by the level of cord injury, aspiration and primary lung injury. In the absence of major airway obstruction and flail chest, the presence of paradoxical breathing is considered highly suggestive of cervical spine injury. Paradoxical breathing occurs because of loss of motor tone and paralysis of thoracic muscles innervated by thoracic spinal segments. Diaphragmatic action results in a negative intrapleural pressure. As a consequence of chest wall paralysis, the tendency is for the soft tissues of the thorax to ‘cave in’, producing paradoxical chest wall movement. The diaphragm needs to undertake the full work of breathing, including overcoming added resistance to ventilation caused by paradoxical chest wall movement. In addition to standard respiratory status assessment, continuous pulse oximetry and assessment of vital capacity is necessary. Early intubation should be considered if vital capacity is inadequate or falling.
Circulation
Volume resuscitation in the resuscitative phase of the primary survey is undertaken in keeping with usual practices. With the exception of perhaps diving injuries, hypotensive trauma victims should be considered as intravascular volume depleted and bleeding until proved otherwise. Standard initial volumes of resuscitation fluid will not adversely affect the haemodynamic welfare. Owing to peripheral vasodilatation, spinal cord trauma patients are relatively intravascular volume depleted and, therefore, volume preloading is appropriate. However, unnecessary volume overloading in an attempt to raise systolic blood pressure substantially will lead to acute pulmonary oedema.
After resuscitation fluids have been administered, haemorrhage controlled, ongoing losses replaced and fluid required for oedema responses to injury considered, routine maintenance fluids are all that is needed.
Paralysis of the sympathetic nervous system and, hence, the compensatory mechanisms for intravascular volume depletion, necessitates a heightened suspicion of ongoing bleeding, the signs of which may be dramatic or subtle. Progressive hypotension is a key sign. Paradoxically, the heart rate may rise progressively from a bradycardia of 50–60 beats per minute to more normally acceptable rates. It is uncertain by which mechanism this pseudo or relative tachycardia of quadriplegia occurs. One thought is that with progressive hypotension and brainstem hypoperfusion, the vagal effects are switched off by the brainstem, thus allowing the heart rate to rise towards a more normal or denervated range. The skin may develop patchy or blotchy cyanosis. This is due to a sluggish peripheral circulation and hence locally elevated levels of deoxygenated or desaturated haemoglobin.
In cases of spinal cord injury, the impact of functional sympathectomy will depend upon the level and completeness of the neurological injury. Complete injuries above T1, and perhaps T4, can be expected to have clinically significant manifestations of neurogenic shock. The clinical signs are bradycardia due to unopposed vagal action, peripheral vasodilatation and cessation of sweating. Peripheral vasodilatation is responsible for variable cutaneous manifestations. Initially, flushing can be expected, however, the skin may be pale or cyanosed and its temperature elevated, reduced or within normal limits. The state of the above signs is dependent on perfusion pressure, adequacy of oxygenation and the ambient temperature.
Priapism in a trauma patient is due to penile vasodilatation and is regarded as a highly suggestive sign of spinal cord injury.
Circulatory status is best assessed by conscious state, urine output and venous pressure monitoring. In the early phases of management, close urine output monitoring is of major importance. Early insertion of the urinary catheter allows measurement of urine output, may assist in identifying occult renal tract injury and also prevents undesirable bladder overdistension.
Inotropic support is often unnecessary [5]. However, satisfactory cerebral perfusion is essential. In order to maintain cerebral perfusion, a mean arterial pressure (MAP) of at least 60 mmHg is recommended. In the patient with a previously normal Mini Mental State examination, deterioration may suggest intracranial hypoperfusion due to either intracranial trauma or the neurogenic shock process. Chronotropic and vasoconstrictor agents are occasionally required. These are more likely to be necessary in older patients or those suffering from hypertension who are now relatively hypotensive despite volume loading. Chronotropic agents are occasionally required for patients prescribed β-blocker, peripheral and central vasodilator drugs. Likewise, patients with established cerebrovascular disease may require higher perfusion pressures than the resting pressure of the quadriplegic.
The degree of the physiological effects on the circulation will depend on the site and completeness of the injury. Spinal cord injury below the sympathetic outflow will have little effect on the circulation; complete spinal cord injury above the thoracic outflow will produce a total body sympathectomy. A complete spinal-cord injury in the mid-thoracic segments should result in preserved vasomotor function in the head, neck and upper limbs. Cardiac reflexes should also be relatively well preserved. Vasomotor tone to the abdominal cavity, pelvis and lower limbs will be paralysed. Likewise, incomplete lesions will have a varying affect depending on the site and completeness of the injury. Careful establishment of the segmental level and degree of spinal cord injury on secondary survey will assist in anticipating the likely extent of autonomic dysfunction.
The denervated lung is intolerant of volume overloading. Therefore, careful monitoring of fluid balance, including urine output and, in circumstances of low urine flow, central venous pressure, is required.
Disability
Spinal cord injury has an association with significant head trauma. In patients with altered conscious state due to head trauma, the early brief assessment of mental state and pupillary reflexes is important. All trauma victims with altered conscious state require spinal immobilization until spinal cord or unstable vertebral injury is excluded on physical examination and investigation.
In patients with injuries at or above T4, bilateral Horner’s syndrome may be present, with relative pupillary constriction.
Exposure
As a spinal cord injury may be one of several injuries, the patient should be fully exposed and then kept in a warming blanket in keeping with a routine approach to patients with multisystem trauma.
General management issues
The general management is in keeping with the approach to any victim of major trauma.
Analgesia and medications
Owing to the variable physiology of the peripheral circulation due to vascular tone denervation and sympathetic efferent interruption, the absorption of subcutaneous and intramuscular medications is unreliable. It is recommended that analgesia be provided by continuous intravenous infusion, with careful monitoring of vital signs. For similar reasons and where possible, all other medications are administered by the intravenous route.
Temperature
In complete quadriplegia, the patient has been rendered poikilothermic by the interruption of efferent sympathetic activity. Attention is directed to ensuring that the core temperature remains within the normal range. Such patients will demonstrate a core body temperature in keeping with changes in ambient temperature.
Clearing the spine
Clearing the cervical spine
Prolonged immobilization of the spine with rigid pre-hospital rescue collars and other rigid immobilization devices may unnecessarily add to patient discomfort, complications of the immobilization devices and the need for ongoing spinal nursing.
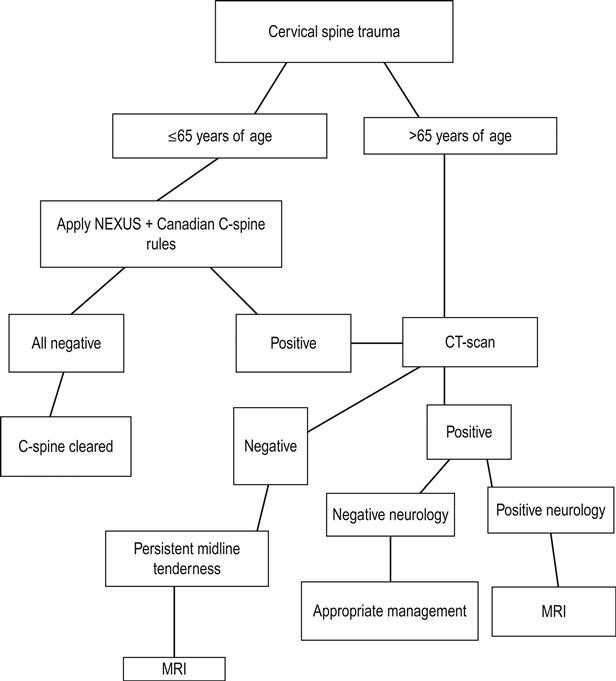
Although various algorithms exist for clearing the spine of significant injures and compliance with such clearing algorithms is high, none have been validated for clinical effectiveness. Most incorporate the elements of either the United States National Emergency X-Radiography Utilization Study (NEXUS) or the Canadian Cervical Spine Rules (Canadian C-Spine Rules [CCR]) thus restricting evidence-based decision rules to the cervical spine [11] (see Tables 3.8.7 and 3.8.8)).
It still is the emergency physician’s responsibility to minimize exposure to radiation. The need for imaging of the cervical spine can be safely determined by applying both the criteria of NEXUS and the CCR. The application of both of these two clinical tests essentially clears the c-spine in a number of patients.
The fundamental differences between the two tests are that the CCR incorporates the mechanism of injury, circumstances and examination findings of active movement of the cervical spine [12–14].
Following the (radiological) algorithm in Figure 3.3.1 is a safe way to approach the patient for cervical spine trauma.
Thoracic, lumbar and sacral spine clearance
There is little information available to provide evidence-based guidelines for clearing the thoracic, lumbar and sacral spine. The investigation and injury exclusion strategy is based on appropriate clinical reasoning (read the mechanism!) and an understanding of the effectiveness and limitations of medical imaging options, in both logistics and effectiveness. All patients with significant mechanisms of injury and pain or tenderness along the thoracic, lumbar and sacral spine should be imaged. Additionally, patients with multiple injuries and high-risk mechanisms should be routinely imaged.
Secondary survey, referral-disposition and definitive treatment
The secondary survey of spinal cord damage
The definitive diagnosis of a spinal cord injury is made from the findings on secondary survey. Two specific injury entities need to be considered: skeletal and neurological.
A head-to-toe clinical examination is conducted in keeping with the standard conventions used in examining any victim of major trauma. The following outlines the specific points of clinical examination pertinent to spinal injury.
Head and neck
An examination of the cervical spine is conducted maintaining immobilization. Palpation of the spine posteriorly may demonstrate generalized tenderness owing to diffuse muscular spasm. However, the point of maximal tenderness should be determined. In hyperextension injuries, the prevertebral and paravertebral muscles are often contused. This is a helpful sign when evaluating hyperextension–hyperflexion injuries in patients who were in stationary vehicles hit from behind. Longitudinal pressure to the head increases cervical pain. Such patients should be considered to have a higher likelihood of a significant vertebral injury.
The neck should be examined for swelling and bruising. Deformity will be noted if there is a dislocation with significant displacement. It should be remembered that significant bony and soft tissue injury frequently occurs without any major findings on external examination.
As prolonged immobilization of the cervical spine with rigid pre-hospital rescue collars and other rigid immobilization devices may unnecessarily add to patient discomfort, complications from the application of splinting devices and the need for ongoing spinal nursing, it is important to determine whether immobilization devices can be removed early during the assessment and treatment phases of management. Reasons for lengthy periods of immobilization include times to definitive radiological assessment and waiting for windows of opportunity to ensure vertebral stability (see also Immobilization of the spine and Clearing the spine).
A re-examination of the upper airway is required. A prevertebral haematoma can cause obstruction; the gag reflex may be blunted; airway protection may be embarrassed owing to paralysis of muscles below the neck, resulting in inefficient gag and cough. The patient will have gastric stasis and is at considerable risk of fluid aspiration.
The torso
The patient should either be lifted or rolled on to the side using a formal spinal-lifting technique, so that the back can be examined. The spine is examined for alignment, swelling, bruising and abrasion. Deformity is generally not a feature, except in the presence of major dislocation or disruption.
The rise and fall of the chest is noted. Paradoxical movement is a sign of thoracic cage muscular paralysis and will be more pronounced the higher the segmental level of injury. Careful examination of the thorax, abdomen and pelvis is required. In both quadriplegia and high paraplegia, serious injury may be masked by the use of analgesia and anaesthesia. Significant vertebral injury to the thoracic and lumbar spines is associated with major injuries to the thoracic, abdominal and pelvic organs.
The abdomen is specifically assessed for an evolving paralytic ileus.
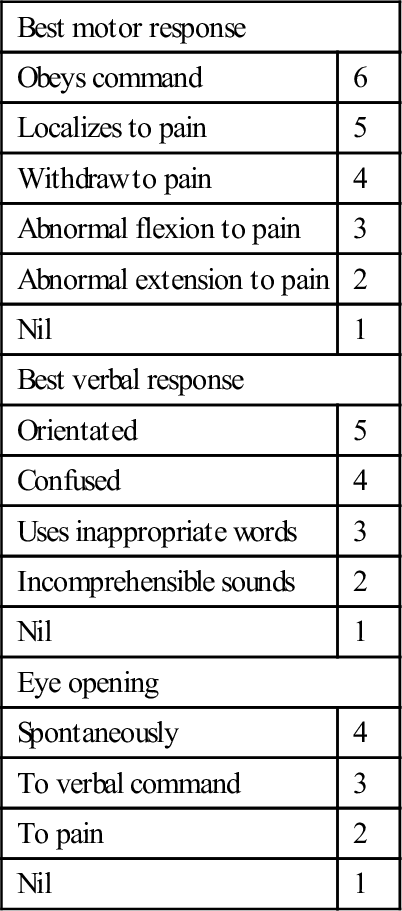
Neurological assessment
A thorough examination of the peripheral nervous system is required. It is strongly recommended that both motor and sensory examinations be undertaken in accordance with the following convention. Examine motor, sensory and reflex components independently. Examination begins at the head and then progresses across the shoulders. The upper limbs are then examined. The torso evaluation begins from just below the clavicles, extending inferiorly to the groin; each lower limb is then assessed. Finally, the saddle area and pelvic floor are assessed.
This approach reduces the likelihood of an incorrect diagnosis of paraplegia by finding a ‘pseudo’ neurological level of injury just below the clavicles when upper limbs have not been examined. It is therefore important that the upper limbs be assessed before examining the torso.
Motor function
Muscle power is assessed in terms of neurological segments and not muscle groups. Muscle power in each segment is graded from 0 to 5 as shown in Table 3.3.1.
Table 3.3.1
| Power grade | Clinical finding |
| Grade 0/5 | No movement |
| Grade 1/5 | Flicker |
| Grade 2/5 | Movement present, but not a full range against gravity |
| Grade 3/5 | Full range of movement against gravity with no added resistance |
| Grade 4/5 | Full range of movement against gravity with added resistance but with reduced power |
| Grade 5/5 | Normal power |
It is often impossible to assess power grades in certain segments owing to the patient’s injuries. The upper limbs are the most easily examined. The strength of a cough provides some information as to the state of thoracic and abdominal musculature.
In the emergency setting, the state of the pelvic muscles is determined through a rectal examination by assessing rectal tone and requesting the patient to tighten the sphincter on the examiner’s gloved finger.
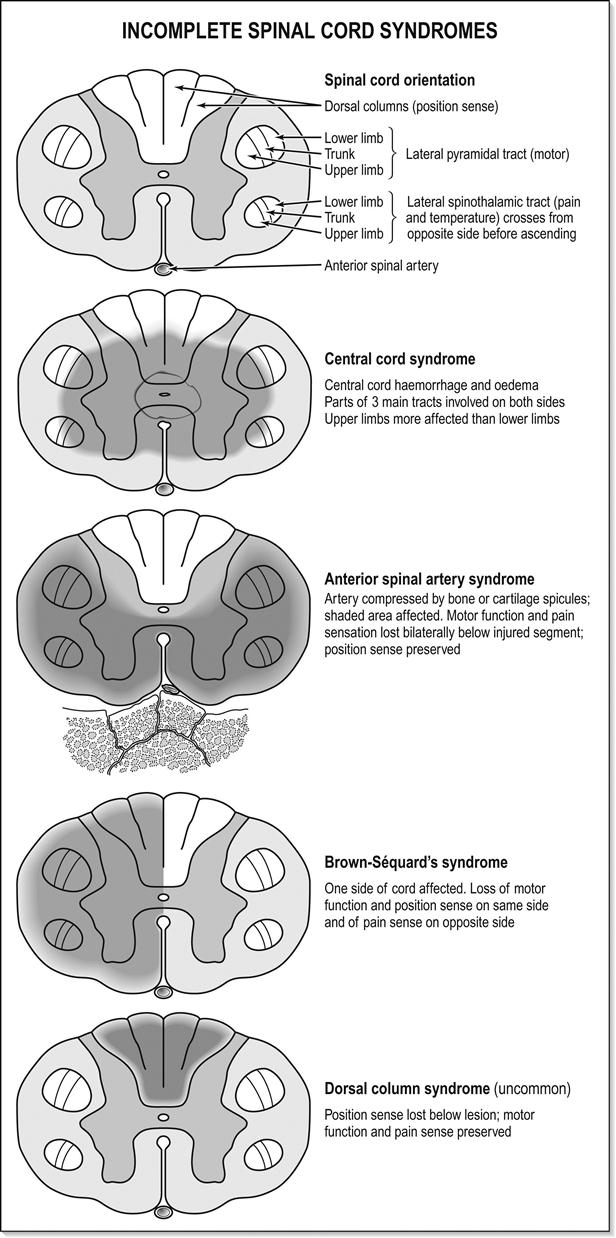
Sensory function
Dorsal column sensation is assessed using a piece of cotton wool and testing for light touch. Spinothalamic sensation is assessed using a pin or sharp object. Although proprioception, vibration and temperature can be assessed, these are not essential and add little to the emergency examination. When testing with a sharp object, a hypodermic injection needle or a trocar stylet must not be used: these are engineered to stab the skin as painlessly as possible, therefore they cause trauma and are unreliable.
The general convention described below should be followed. Sensory examination begins on the face which, as it is supplied by the trigeminal nerve and bypasses the spinal cord, acts as a reference point. It is an important axiom based on anatomy that ‘in the absence of head injury or local facial injury, sensation to the face is always normal in pure spinal cord injury’ (the trigeminal nerve comes from above the spinal cord). It is recommended that examination of the head, neck and upper torso is performed as follows. Start by examining the C2 dermatome laterally on the neck behind the mandible and beneath the ear. Extend examination onto the top of the shoulder, thus assessing the C3, C4 and C5 dermatomes. In the upper limbs, examine the dermatomes in segmental order. This should include T2 on the upper medial aspect of the arm. Then carry on examining the torso in the mid-clavicular plane or at the outer border of the surface marking of the rectus sheath.
Reflexes
Reflexes are examined in keeping with usual examination practices. Superficial abdominal reflexes should be noted. The anal and bulbocavernosus reflexes are important in assessing sacral segments.
Corticosteroids–methylprednisolone
A Cochrane review from 2012 found that administration of methylprednisolone within 8 hours after injury gave a significant recovery of motor function [15].
Administration for an additional 24 hours (totalling 48 hours) may give an additional improvement of motor neurological function and functional outcome. On the other hand, the use of methylprednisolone is not without complications. It is contraindicated in patients with heavily contaminated open injuries, other heavily contaminated situations, such as perforated bowel and established sepsis. It has the risk of developing acute adrenal insufficiency in these patients, which needs recognition and prompt treatment to prevent further complications. It is relatively contraindicated in diabetes mellitus. Prophylactic measures, such as for acute peptic ulceration and monitoring of blood glucose, should be instituted.
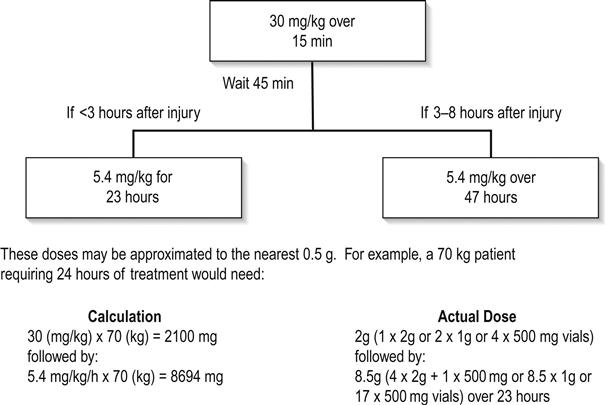
The benefit of steroids in spinal cord injury is therefore considered questionable. Despite this, their use remains a treatment option and several centres prefer to use high-dose methylprednisolone in the early management of patients with neurological injury. In Australia, spinal cord injury is not listed as an indication for high-dose methylprednisolone. Therefore, the decision to use high-dose corticosteroids should be made in conjunction with the specialist services, either the major trauma service or spinal injuries service that will be managing continuing care. If used, treatment must be commenced within 8 hours from the time of injury. The total treatment period should be for 24 hours if treatment is commenced within 3 hours of injury and 48 hours if commenced between 3 and 8 hours.
A guideline for the use of methylprednisolone in acute spinal cord injury is presented in Figure 3.3.2.
Referral-disposition
Patients with a spinal cord injury should be referred to a centre with facilities for optimal management as soon as practicable. Specific treatments such as immobilization, specific therapy and transport considerations should be discussed with the continuing care provider or spinal injuries unit prior to transfer. If transport is delayed, it is appropriate that the spinal injuries unit be involved and contribute to the patient’s initial management, especially in areas of specific management, as soon as possible, even if transfer is to be delayed by several days.
Specific conditions
Vertebral injury [2]
Cervical spine fractures
Cervical spine injuries may result from one or more combinations of the following mechanisms:
Hyperflexion
Hyperflexion produces the following injuries:
Flexion injuries can cause a vertebral body fracture with an anteroinferior extrusion teardrop fracture. This is often associated with retropulsion of a vertebral body fracture fragment or fragments into the spinal canal.
The clay shoveller’s fracture is a particular spinous process fracture produced by a sudden load on a flexed spine, with resulting avulsion of the C6, C7 or T1 spinous processes.
Hyperextension
Anterior widening of disc spaces, prevertebral swelling, avulsion of a vertebral body by the anterior longitudinal ligament, subluxation and crowding of the spinous processes are features of the hyperextension injury. Encroachment on the canal by an extruded disc or a posterior osteophyte may occur in patients with osteoarthritis of the cervical spine.
Flexion–rotation
This is responsible for unilateral facet dislocation or forward subluxation of the cervical spine.
Vertebral compression
This is the mechanism responsible for burst fractures. The intervertebral disc is disrupted and driven into the vertebral body below. In addition, disc material may be extruded anteriorly into prevertebral tissues and posteriorly into the spinal canal. The vertebral body may be comminuted to varying degrees, with fragments being extruded anteriorly and posteriorly into the spinal canal.
Lateral flexion
This may produce uncinate fractures, isolated pillar fractures, transverse process injuries and lateral vertebral compression.
Distraction
These injuries may result in gross ligamentous and intervertebral disc disruption. The hangman’s fracture may also occur by combined distraction and hyperextension mechanisms.
C1 – the atlas
Fractures of the atlas comprise 4% of cervical spine injuries. Mechanisms of injury generally involve hyperextension or compression. Around 15–20% of fractures may be associated with a C2 injury and 25% may be associated with a lower cervical injury. The Jefferson fracture is a blowout fracture of the ring. Other fractures include isolated injuries of the posterior arch, the anterior arch and the lateral mass.
C2 – the axis
Axis fractures comprise 6% of cervical spine injuries, with an association with concurrent C1 injury in the majority of cases.
Computed tomography (CT) scan images are examined for odontoid subluxation. Three types of odontoid fracture are described:
Other fractures of the odontoid include avulsion fractures of the lower anterior margin of the body due to a hyperextension injury. A hangman’s fracture is a bilateral neural arch fracture of C2. It is a hyperextension injury and is associated with prevertebral soft tissue swelling, anterior subluxation of C2 on C3 and avulsion of the anteroinferior corner of C2.
C3–C7
Fractures in this segment of the cervical spine are clearly picked up with CT scanning. Fractures are defined as unstable when:
Fractures of the thoracic spine
Hyperflexion is the principal mechanism of injury to the thoracic spine, with resultant wedging of vertebral bodies. Owing to the rigidity of the thoracic cage and the associated costovertebral articulations, most thoracic spine injuries are stable. However, internal stabilization may be necessary where kyphosis is pronounced.
Thoracolumbar spine
Fractures of the thoracolumbar spine comprise 40% of all vertebral fractures responsible for neurological deficit. Most are flexion or hyperflexion-rotation injuries. Plain films may demonstrate facet joint disruption, evidence of interspinal ligament disruption, posterior bony fragments protruding into the spinal canal and burst fragments at the superior surface of the vertebral body. These fractures are generally unstable.
Lumbar spine
Injuries similar to those previously described do occur in the lumbar spine. Three specific injuries of the lumbar spine merit further discussion and are broadly considered posterior distraction injuries of the vertebral arch. They constitute a group known as seatbelt injuries, produced when a hyperflexion force is applied to a person wearing a lap-only type seatbelt. In unrestrained persons, a flexion injury generally flexes the spine around a point through the anterior spinal column, typically causing a wedge compression fracture of the body. In the restrained person, the point of flexion is moved forward to the anterior abdominal wall. This change in momentum forces converts the hyperflexion mechanism to one of distraction. These injuries are caused by deceleration from high speed, as seen in head-on road traffic accidents or aircraft crashes.
Plain film radiology remains the first-line imaging study. Suggestive findings include:
 a vacant or empty appearance of the vertebral body on the AP film
a vacant or empty appearance of the vertebral body on the AP film
 discontinuity in the cortex of the pedicles or spinous processes on the AP view
discontinuity in the cortex of the pedicles or spinous processes on the AP view
 fracture, with or without dislocation in the lateral view, which may be subtle.
fracture, with or without dislocation in the lateral view, which may be subtle.
CT or magnetic resonance imaging (MRI) are of value in further delineating architectural disruption. However, the exact nature of the fracture complex may be difficult to delineate on axial images, as the fractures are often orientated parallel to the scanning plane. Three-dimensional reconstruction of multislice CT images has greatly improved spinal injury imaging.
These injuries are often associated with concurrent intra-abdominal visceral injuries.
Chance fractures
These are characterized by an oblique or horizontal splitting of the spinous process and neural arch, extending the superior posterior aspect of the vertebral body into and damaging the intervertebral disc.
Horizontal fissure fracture
This fracture is very similar to the chance fracture, with the exception of the fracture line, which extends horizontally through the vertebral body to its anterior aspect.
Smith fracture
This spares the posterior spinous process. The fracture line involves the superior articular processes, the arch and a small posterior fragment of the superior posterior aspect of the vertebral body. Although the spinous process is intact, the posterior ligaments are disrupted.
Spinal shock
Spinal shock is often confused with the neurogenic shock of sympathetic interruption. They are different entities. Complete separation of the spinal cord from the brain abolishes voluntary movement and sensory perception and causes changes in cord physiology and reflex activity. Acute cord confusion is a simple explanation of the resulting pathophysiology. Spinal shock is manifested by the transient cessation of cord activity in the normal cord below the injury. The cord distal to the injury is unable to function as one would expect from a newly created upper motor neuron lesion. Spinal shock may last for a few hours to several weeks, depending on the segmental level and extent of the cord injury. During this period, both somatic and autonomic reflexes below the injured segments disappear. Spinal shock has been attributed to the sudden loss of descending facilitatory impulses from higher centres. Recovery from spinal shock is heralded by the return of the Babinski response, followed by the perineal reflexes. In quadriplegia and high paraplegia, as the cord recovers from spinal shock, either recovery of function (depending on the degree of injury resolution at the injury site) occurs or, more commonly, spasticity develops. If the cord injury is at the conus medullaris or the cauda equina, unless recovery occurs, a lower motor neuron pattern with areflexia remains.
Spinal cord injuries
Spinal cord injuries should be divided into primary and secondary injuries, as the causes affect the choice of treatment. Primary spinal cord injuries refer to the injuries directly caused by the trauma mechanism and its damaging energy onto the spinal cord. Secondary spinal cord injuries are caused by other mechanisms often related to the initial trauma, i.e. hypotension, hypoxia, etc.
Primary spinal cord damage (Fig. 3.3.3)
Transverse spinal cord syndrome
The spinal cord is completely damaged transversely across one or more adjacent spinal segments. No motor or autonomic information can be transmitted below the damaged area and ascending sensory stimuli from below the damaged spinal segments are blocked. The manifestations are: total flaccid paralysis, total anaesthesia, total analgesia and, usually, areflexia below the injured segment.
The transverse cord syndrome can be incomplete, with partial paralysis, reduced sensation and pain sensibility below the injured part.
The term ‘sacral sparing’ implies that some sensibility with or without motor activity in the areas supplied by the sacral segments is preserved in an otherwise complete transverse cord syndrome. The presence of sacral sparing implies an incomplete injury, as some neurological transmission through the injured segments is preserved. It will be recalled that spinothalamic and corticospinal transmission to and from sacral segments are located in the outermost parts of the spinal cord and are, therefore, immediately adjacent to the origin of the spinal cord’s blood supply.
Acute central cervical cord syndrome
The central part or grey matter of the spinal cord is injured. Transmission in the outer rim of the spinal cord is essentially intact but impaired. The signs of this injury are:
This is frequently caused by a hyperextension injury and is typically seen in older patients with cervical spondylosis. In this situation, the cord is compressed between posterior osteophytes and the intervertebral disc in front and the ligamentum flavum behind.
Acute anterior cervical cord syndrome
The anterior half of the spinal cord – the region supplied by the anterior spinal artery – is damaged (see Figs 3.3.3 and 3.3.5). There is motor loss or paralysis below the level of the injured segment(s). Spinothalamic transmission is impaired and thus there is analgesia with loss of temperature sensation and coarse touch. As the dorsal columns are relatively intact, there is some preservation of joint position, vibration sense and fine touch. In the context of an acute cord injury, the patient may not interpret dorsal column preservation in terms of joint position sense or light touch. Dorsal column function may be manifested as preservation of vague and poorly localized sensation in the extremities.
These injuries are frequently the result of flexion–rotation or vertical compression injuries.
Brown-Séquard’s syndrome
This syndrome is a functional cord hemisection with dissociated sensory loss. One half of the cord is damaged. In a pure Brown-Séquard lesion, ipsilateral motor function is impaired, as are light touch, joint position sense and vibration. Contralateral spinothalamic sensation – that is, pain and temperature – is impaired, whereas ipsilateral sensation is relatively preserved. Reflexes are variable.
Posterior cord syndrome
This is an uncommon injury that causes contusion or disruption to the dorsal columns, leading to impaired or disrupted proprioception, vibration and fine touch sensation.
This syndrome is usually the result of penetrating trauma to the back or a hyperextension injury in association with fractures of the vertebral arch.
Spinal cord concussion
This diagnosis implies a temporary cessation of spinal cord neurological function. In this instance, there is a near full recovery of cord function within 48 hours. The patient will be first assessed as suffering from either a complete or an incomplete spinal cord injury and will then recover within the above period. The patient has suffered an injury to the spinal cord that has been enough temporarily to cease electrical activity in the injured spinal segment, with no, or very little, mechanical or anatomical injury to the cord, such as haemorrhage or contusion. It is the pattern of recovery over a day or two that allows the diagnosis to be made. Unfortunately, this constitutes less than 1% of all spinal cord injuries.
In all the incomplete spinal cord syndromes, the location of cord pressure or damage varies in terms of incompleteness and segmental level(s) of cord injury and so will the range of symptoms and signs.
Secondary spinal cord damage
It is often believed that most spinal cord damage occurs at the time of injury, but it may occur subsequent to the initial injury [6]. This secondary damage may be caused by:
 Inappropriate manual handling [4,5]. Subsequent mishandling causes significant movement at the site of the primary vertebral injury, leading to spinal cord damage. This can be prevented by careful handling of the patient. It is important to be aware of the possibility of a spinal cord injury and protect the spine until the diagnosis has been excluded. This involves standard cervical in-line immobilization, whole-spine immobilization using a spine board or a Jordan frame and ‘log roll’ for moving the patient.
Inappropriate manual handling [4,5]. Subsequent mishandling causes significant movement at the site of the primary vertebral injury, leading to spinal cord damage. This can be prevented by careful handling of the patient. It is important to be aware of the possibility of a spinal cord injury and protect the spine until the diagnosis has been excluded. This involves standard cervical in-line immobilization, whole-spine immobilization using a spine board or a Jordan frame and ‘log roll’ for moving the patient.
Unconscious patients
As previously mentioned, the definitive diagnosis of spinal cord injury is a secondary survey consideration and hence identified primarily from symptoms and physical findings. There is no pathognomonic sign of a spinal cord injury in an unconscious patient. The following should alert the examiner to the possibility of a coexisting spinal cord injury in an unconscious trauma victim:
 priapism in the unconscious trauma victim suggests quadriplegia or high to mid-thoracic paraplegia
priapism in the unconscious trauma victim suggests quadriplegia or high to mid-thoracic paraplegia
 preserved facial grimace in the absence of a response to painful stimuli in the limbs
preserved facial grimace in the absence of a response to painful stimuli in the limbs
 lower limb flaccidity in the presence of normal upper limb tone suggests paraplegia
lower limb flaccidity in the presence of normal upper limb tone suggests paraplegia
 observed upper limb movement in the absence of lower limb movement suggests paraplegia
observed upper limb movement in the absence of lower limb movement suggests paraplegia
 the combination of the persistent bradycardia and hypotension despite volume challenge
the combination of the persistent bradycardia and hypotension despite volume challenge
Special attention, again, should go to protection of the C-spine in this category of patients. As the golden standard of imaging, the cervical spine CT is highly sensitive and may reliably exclude unstable injuries in patients with obtunded or intubated blunt trauma [17].
Documentation conventions
Two of the pitfalls in the management of any neurological injury are terminology and documentation. The following convention is recommended.
Motor function is recorded either using segmental terminology in written format or on a muscle chart (Fig. 3.3.4). It will be impossible to chart every segment accurately, but motor power in the upper and lower limbs should be able to be confidently recorded. Power should be graded using the 0–5/5 system.
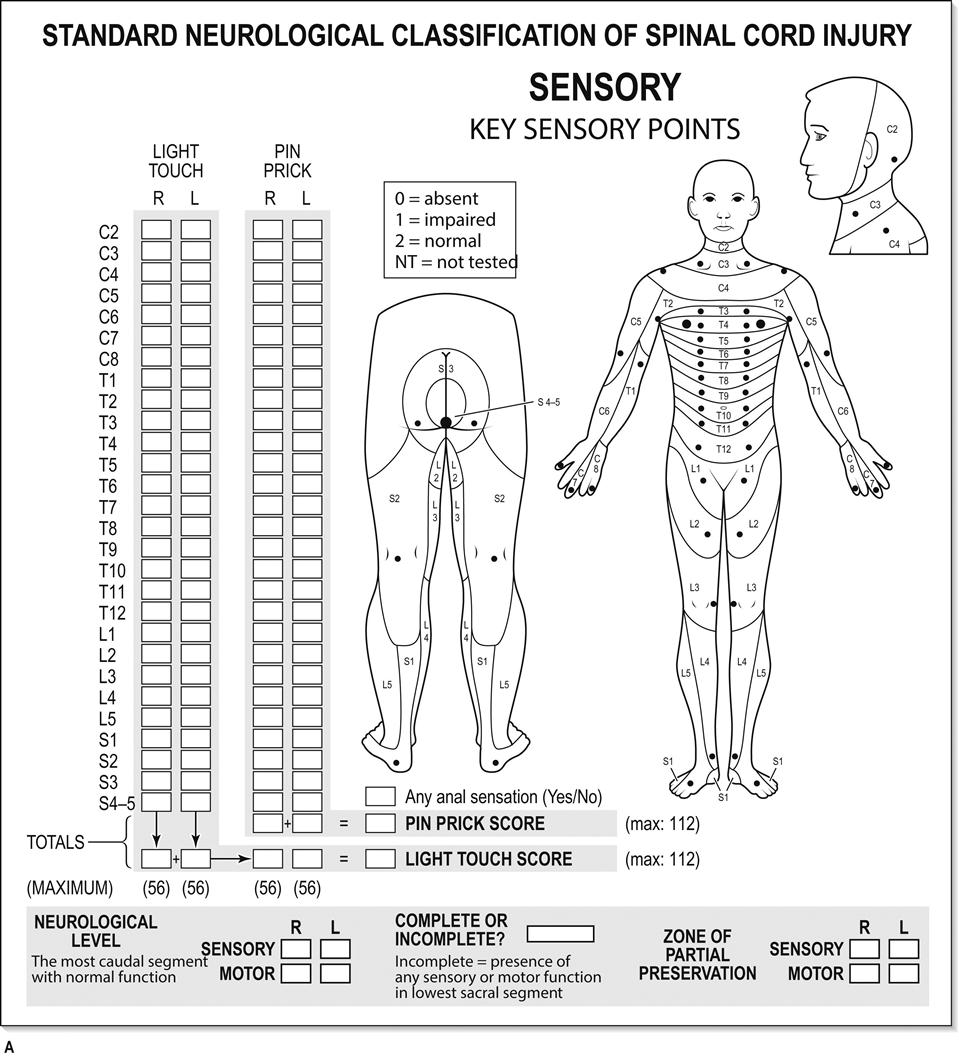
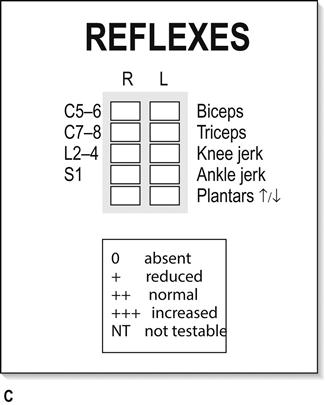

Sensation is recorded more descriptively. Normaesthesia, hyperaesthesia, hypoaesthesia and anaesthesia are the descriptors for dorsal column function and testing for light touch. Normalgesia, hyperalgesia, hypoalgesia and analgesia are used in describing pain perception. These are recorded on sensory charts or described according to the following two examples.
In a patient with a transverse spinal cord syndrome, incomplete below C6 and complete below T1, the sensation is described as:
In a patient with an acute central cervical cord syndrome below C6, with total segmental paralysis in the C6–C8 segments and with some involvement of C5, the sensation might be described as:
 normaesthesia and normalgesia to C4
normaesthesia and normalgesia to C4
 hypoalgesia and hypoaesthesia below C4
hypoalgesia and hypoaesthesia below C4
Acknowledgement
The author of this chapter in the previous edition of this textbook was Jeff Wassertheil. The text in this new edition is based on the original chapter for which Jeff Wassertheil must be acknowledged.
3.4 Facial trauma
Lewis Macken
Introduction
Facial trauma is defined as injury to the facial soft tissues (including the ear) and bony skeleton. This covers a wide spectrum of injuries [1]. Patients with facial trauma are usually male, between the ages of 20 and 25 years and have usually sustained their injuries as a result of blunt trauma. Isolated facial injury after an assault accounts for most injuries, with motor vehicle injuries, contact sports and falls accounting for most of the remainder [2]. Up to 20% of patients with facial injuries as part of multisystem injury will have associated life-threatening injuries [3,4].
Management of blunt and penetrating trauma to the face can be challenging. Life-threatening facial injuries are those that result in airway compromise or ongoing haemorrhage. At the same time, attention must be given to preserving long-term cosmesis and the normal functions of sight, speech and mastication. After immediate resuscitation and stabilization, management of facial injuries requires a knowledge of anatomy, the injuries commonly associated with facial injury and an awareness of treatment methods for the differing injuries to the face [5,6]. Consultation should be sought when the injury threatens the restoration of normal function or appearance. Non-accidental injury should always be considered, as some studies report that over 20% of head, neck and facial injuries in women are the result of domestic violence [7].
History
The evaluation should commence with the history, with emphasis given to the mechanism of injury. The velocity of force directed to the face determines the degree of facial fracture [8]. Respiratory and haemodynamic observations and quantification of pre-hospital blood loss are important components of the history.
Examination
The physical examination involves evaluation of all facial areas by inspection, palpation and assessment of function. Inspection of the face may reveal deformity, loss of normal symmetry, changes in contour and localized areas of swelling. Skull-base fractures may be suggested by periorbital or postauricular bruising and the ears must be inspected to exclude haemotympanum or cerebrospinal fluid (CSF) otorrhoea. Gentle systematic palpation of the facial skeleton should follow, assessing for tenderness and feeling for asymmetry, bony margin irregularities, abnormal motion or crepitus. Specific attention should be given to the supraorbital and infraorbital margins, the zygomas, nasal bones, maxilla and mandible. Mobility associated with midfacial maxillary fractures is assessed by grasping the anterior maxilla with the thumb and index finger of one hand, while stabilizing the forehead at the nasal bridge with the other. Ophthalmological evaluation includes inspection for enophthalmos or exophthalmos and globe injury and assessment of pupillary responses, visual acuity, visual fields, extraocular movements and inquiry for diplopia. Although eye injury is an infrequent complication of blunt trauma, subjective impairment in visual acuity remains the most sensitive single predictor of eye injury [9] and examination that reveals the presence of an afferent pupillary defect or a non-reactive pupil is the most important factor in predicting the severity of eye injury [10]. The nose should be inspected for the presence of any septal deviation, haematoma (more common in children) or CSF rhinorrhoea. Oral examination is necessary to look for loose, broken or missing teeth, malocclusion of dentition, soft tissue lacerations and contusions. Examination of the mandible includes assessment of the temporomandibular joint in the open and closed positions.
Assessment of the function of facial structures is the final component of the examination of the face. Malocclusion, often identified by the presence of a new gap between the occlusal surfaces of the teeth when the patient closes his/her jaws, is a good indicator of maxillary or mandibular fracture. Similarly, pain on biting on a tongue depressor, loss of bite strength and limitation of jaw movement are strongly suggestive of a fracture; the patient should be asked if the bite has subjectively changed [11,12]. Motor function of the facial nerve should be assessed and all three branches of the trigeminal nerve should be evaluated. Commonly encountered symptoms and signs are hypoaesthesia or paraesthesia of the upper lip or upper alveolar margin, suggesting fracture of the maxilla causing injury to the alveolar branches of the infraorbital nerve. Sensory changes in the lower lip and lower alveolar margin suggest fracture through the mandibular canal, causing inferior alveolar nerve injury (a branch of the mandibular nerve) [11].
Radiographic examination
Computed tomography (CT) is the initial imaging modality of choice in evaluating patients with facial trauma. Although an orthopantomogram (OPG) view is very helpful in investigating a suspected fracture of the mandible, CT will be required for patients with clinically obvious complex facial injuries, especially of the upper and middle thirds of the face and for patients with multisystem injuries. CT and derived image reconstructions display soft tissue relations to the bony skeleton and the degree of skeletal distortion, displacement and comminution. CT assists with surgical planning and evidently allows other injured areas to be imaged at the same time for multitrauma patients.
Immediate management in the emergency department
It is important to prioritize injuries in the management of the patient with facial trauma because facial injuries that do not threaten the airway or risk life-threatening haemorrhage can usually be assessed and managed as part of the secondary survey. Proper attention should be given to potentially more significant head, chest and abdominal injuries before a non-life-threatening facial injury is thoroughly evaluated, no matter how impressive and disfiguring the facial injury appears. The association of facial injury with cervical spine or cord injury is questionable, especially if vehicular trauma was not the cause [13]. After blunt assault, the incidence of associated cervical spine injury is low, but is more likely if there is a fall after the assault [14]. Patients with clinically significant head injuries (especially Glasgow Coma Score [GCS]<9) are at greater risk of having cervical spine injuries than those with evidence of facial trauma [15–18]; intracranial injuries are more frequently associated with facial fractures than are cervical spine injuries [19].
Airway management
Asphyxia due to upper airway obstruction is the major cause of death from facial trauma. The airway must be rapidly assessed, respiratory obstruction relieved and an adequate airway established. Managing these patients in the supine position is often risky and early semi-elective intubation may be required. Signs of partial airway obstruction include tachycardia, tachypnoea, restlessness, fighting to sit up, noisy respirations, stridor and supraclavicular and intercostal retractions. This may lead to complete obstruction. An unobstructed airway in the presence of facial trauma should be closely monitored because increasing oedema and persistent bleeding may later compromise airway patency.
Fractures of the mandible and maxilla with posterior or inferior displacement, together with displaced soft tissues, blood, secretions or other foreign material, may lead to airway embarrassment. Simple airway measures, such as chin lift and jaw thrust should be performed and the mouth immediately examined. Any loose foreign material, such as food, broken dentures or teeth or bone fragments, should be removed and blood clots suctioned. If anterior traction on the fractured mandible or on the mobile segment of the maxilla (performed by inserting two fingers behind the soft palate and lifting the middle third of the face forwards and upwards) fails to relieve posterior pharyngeal obstruction and does not establish unobstructed ventilation, a definitive airway must be placed. Distorted facial anatomy may make bag and mask ventilation difficult. Rapid-sequence orotracheal intubation can usually be performed. Awake fibreoptic intubation is an option, but the presence of persistent bleeding makes the procedure technically difficult. Standard drills for anticipated intubation difficulties should be at hand and equipment for performing a cricothyroidotomy and transtracheal jet ventilation should be available. A surgical airway may be life saving when anatomical disruption makes intubation difficult. A tracheostomy performed under local anaesthesia in the operating theatre is often the safest option in a stable patient with significant midfacial injuries in whom airway difficulties are expected [20].
Control of haemorrhage
Traumatic facial haemorrhage can be massive, difficult to manage and potentially life threatening in approximately 5% of patients with midfacial fractures [21]. Bleeding from midface trauma mainly originates from branches of the external carotid artery (with branches of the internal carotid artery also supplying the nose). Most haemorrhage can be controlled with direct pressure, anterior nasal packs and double balloon catheters providing anterior and posterior nasopharyngeal tamponade (the placement of 12–14 G Foley catheters with 10 mL balloons inflated and taped under tension to the side of the face is an alternative) [22]. Care must be taken with nasal instrumentation: the incidence of associated skull-base fractures is more common with orbital wall or rim fractures than with more inferiorly located facial fractures. Also, a skull-base fracture is more likely in the presence of multiple facial fractures (the presence of three or more facial fractures is associated with an incidence of skull-base fracture of up to 33%) [23]. Attempts to clamp bleeding vessels in the emergency department (ED) should be avoided because of the associated risks of damaging important structures, such as the facial nerve, parotid duct or lacrimal apparatus. If simple measures fail to arrest the bleeding, operative reduction of the fractures, especially of the maxilla, and possible ligation of bleeding vessels should be undertaken, with angiography and selective embolization considered if other measures fail.
Disposition
After initial stabilization, immediate treatment of most facial injuries is mainly supportive. Fractures requiring operative management are often dealt with on a delayed basis, when soft tissue swelling is resolving. The need for antibiotics for patients with facial trauma depends on the mechanism of injury, the extent of the injury and the immune status of the patient. Systemic antibiotics are not required for most facial wounds. However, antibiotics should be given for bites and grossly contaminated wounds; wounds that extend into the oral cavity, nose and paranasal sinuses; wounds with exposed nasal or ear cartilage; crush wounds and wounds with considerable oedema; and for immunologically compromised patients. Specific antibiotic choices include amoxicillin–clavulanate or cephalexin. However, the evidence to support or refute the use of prophylactic antibiotics in facial trauma is weak. Tetanus immunity should be assessed.
Thorough documentation of injuries is important for medicolegal reasons, as facial injuries are frequently due to personal assault and so later litigation is often likely.
Specific injuries
Soft-tissue injuries
Soft-tissue injuries include abrasions, contusions, lacerations, avulsions and burns. The aim of treatment is to preserve appearance and function. The management of soft-tissue facial injuries involves consideration of how the wound should be repaired and whether it should be repaired in the ED. Possible reasons for delayed wound closure are more urgent coexisting injuries, severe crush injuries, the presence of a foreign body, severely contaminated wounds and an underlying fracture. In these cases, the wound should be irrigated, haemostasis achieved, covered with normal saline-soaked gauze and the patient referred to the appropriate specialty team.
Soft-tissue injuries that usually require repair in the operating theatre include ocular or significant eyelid injury; parotid gland or duct injury; facial nerve injury (injuries to the cheek between the tragus of the ear and a line drawn vertically through the pupil may be associated with damage to the facial nerve, parotid gland or duct); nasolacrimal apparatus injury; alveolar process wounds and significant tooth injuries; lacerations with significant tissue loss or contamination or requiring exact anatomical closure; or where difficulties with patient cooperation are expected. Careful consideration is required before areas of special concern are repaired in the ED, e.g. the lips and perioral area; tongue and oral cavity; nose; ears; periorbital structures; and eyebrows. The eyebrow should not be shaved. Subperichondrial haematomas of the ear require drainage within 7–10 days to avoid permanent cartilage injury (cauliflower ear) and to achieve best cosmetic results. For all wounds closed in the ED, careful attention must be given to thorough cleansing. This can be effectively achieved with pulsatile wound irrigation with normal saline and abrasions containing dirt or other foreign bodies must be scrubbed to prevent traumatic tattooing of the dermis. If the wound is gaping or if structures deeper than the skin and the subcutaneous layer are involved, then multiple-layer repair is usually advisable. This helps to prevent deep tissue space collections and may produce a better cosmetic result, with less scar depression or widening.
Visual assessment after facial trauma can be difficult, especially in the unconscious patient. Loss of vision after blunt facial trauma may be due to: direct injury to the globe; direct injury to the optic nerve (usually bony impingement); indirect injury to the optic nerve (deceleration injury); or due to raised local intraocular pressure (orbital compartment syndrome [OCS]) [24]. OCS is an uncommon ophthalmic emergency, but the diagnosis is clinical. Relief of the intraocular hypertension is time critical and usually requires a lateral canthotomy and inferior cantholysis [25].
Facial fractures
The facial skeleton is constructed to allow applied force to be dispersed via a series of small bone fractures, thereby protecting the skull and intracranial contents. The maxilla and mandible require three times the amount of applied force to cause a fracture as do the nasal bones [26]. Diagnosis of a facial fracture involves a combination of inspection, palpation and radiographic examination. Fractures other than undisplaced fractures of the nose, zygomatic arch or maxilla will usually require acute maxillofacial surgical review. All fractures should be managed initially with elevation of the patient’s head, if associated injuries allow this, and the application of ice.
Mandible
The horseshoe shape of the mandible disperses applied force, which leads to fractures occurring at vulnerable sites regardless of the point of impact and a high incidence of multiple fractures. Common sites of fracture are the condylar neck and angle and the body at the level of the first or second molar [27]. Fractures of the mandibular body usually demonstrate point tenderness, malocclusion and abnormal range of motion and interference with normal mastication. The integrity of the dental arch must be assessed. The application of a soft cervical collar may offer symptomatic relief by providing mandibular support.
Antibiotics should be given when there is the suggestion of a compound fracture with extension into the oral cavity. Most fractures will require some form of internal fixation. Complications of mandibular fractures include chin paraesthesia or hypoaesthesia, delayed union, non-union, infection and malocclusion [28].
Zygomatic arch
Isolated fractures of the zygomatic arch are uncommon and are more commonly part of a more extensive zygomatic complex fracture. An isolated fracture may be evidenced by a depression over the arch, point tenderness and limited or painful mouth opening owing to impingement on the coronoid process of the mandible by the fractured arch. Surgical reduction is required for cosmetic reasons or to correct restricted mandibular range of motion.
Zygomatic complex
Blunt trauma to the zygoma more commonly results in fractures at the articulations of the zygomatic bones with the frontal bone, maxilla and zygomatic process of the temporal bone. Separation at the zygomaticofrontal suture, the zygomaticotemporal suture and at the zygomaticomaxillary suture or infraorbital rim produces the tripod or tripartite fracture. Frequently, the lateral wall of the maxillary sinus and the lateral and central portions of the orbital floor (not to be confused with the orbital blowout fracture) will also fracture as part of the zygomaticomaxillary complex fracture.
Clinical signs of a tripod fracture include flattening of the cheek initially (owing to depression of the fracture segment); this is best seen by standing behind and above the patient, but it is soon replaced by significant swelling. Other signs are hypo-/hyperaesthesia or paraesthesia in the distribution of the infraorbital nerve; asymmetry of the ocular levels; a palpable step defect of the inferior orbital margin; and circumorbital and subconjunctival ecchymoses [11]. Diplopia is often also present and 10–20% of these fractures are accompanied by an ocular injury [29].
Orbital fractures
Fracture of the orbital floor may occur as part of a zygomaticomaxillary fracture or as an isolated injury – the less common orbital blowout fracture. This is a fracture of the orbital floor without fracture of the orbital margin. An increase in intraorbital pressure, as delivered by a fist or a small ball, is transmitted to within the orbit and the relatively weak orbital floor is disrupted, with possible herniation of the contents into the maxillary sinus. Very rarely, a supraorbital rim fracture may be part of a frontal sinus fracture, or lateral orbital wall fracture may be associated with a fracture of the zygoma or a medial orbital wall fracture may occur with a nasoethmoidal fracture. Clinical examination in cases of fracture of the orbital floor may reveal enophthalmos, a difference in pupillary levels, diplopia and impairment of upward gaze and infraorbital hypo-/hyperaesthesia or paraesthesia [6]. An irregular edge to the orbital rim may be evident on palpation. The integrity and function of the eye should be documented to exclude associated injury. CT scanning is necessary to define these fractures fully. Orbital apex fractures are uncommon, but clinical or radiological signs of optic nerve compression (e.g. retro-bulbar haematoma or bone fragment impingement) necessitate urgent surgical referral [30]. All patients with orbital margin or floor fractures require referral. Complications of surgical treatment of orbital floor fractures include persistent diplopia, hypo-/hyperaesthesia or paraesthesia, ectropion and epiphora [31].
Maxillary fractures
Fractures of the maxilla include fractures of the alveolar ridge of the maxilla, fracture of the anterolateral wall of the maxillary sinus and the Le Fort fractures. Isolated maxillary fractures are rare.
In Paris in 1901, Le Fort described a classification of patterns of midface fractures, following cadaveric experiments [32]: Le Fort I (horizontal maxillary fracture) involves only the maxilla at the level of the nasal fossae; Le Fort II (pyramidal fracture) is the most common midface fracture and involves the maxilla, nasal bones and medial aspect of the orbit; Le Fort III (craniofacial dysjunction) separates the midfacial skeleton from the base of the cranium, with the fracture extending through the base of the nose and ethmoid region and across the orbits and zygomatic arches bilaterally.
Most midface fractures are combination injuries, with different Le Fort patterns on each side of the face. Le Fort II and III fractures may require urgent reduction in the ED to improve airway compromise and to arrest ongoing haemorrhage. Patients with such injuries may demonstrate mid-face mobility, and these fractures are associated with skull-base fractures, leading to CSF rhinorrhoea. All patients require a complete eye examination and these injuries necessitate referral.
Nasal fractures
These are common facial fractures. Diagnosis is largely clinical, plain X-rays are unreliable and usually unnecessary and the major concerns for the emergency physician are control of epistaxis and exclusion of a septal haematoma. Displaced fractures should be reduced within 7–10 days.
Nasoethmoidal fractures are more complicated and are caused by trauma to the bridge of the nose. Disruption of the medial canthal ligaments may produce rounding of the palpebral fissures or widening of the intercanthal distance (telecanthus) [11]. Persistent epistaxis and CSF rhinorrhoea may also be evident. Referral is necessary for these patients.
Temporomandibular joint dislocation
Dislocation of the temporomandibular joint may follow trauma to the face or may occur as a result of simply opening the mouth widely. Patients complain of inability to close the mouth and moderate discomfort. X-rays should be performed to confirm that no fracture is present and dislocation will be evidenced by the appearance of the condyle anterior to the articular eminence of the fossa. A directed history will exclude extrapyramidal dystonia mimicking a dislocation. Reassurance, sedation and firm downward pressure of the physician’s thumbs on the patient’s posterior teeth, with upward tilting of the symphysis, is usually successful in relocating the mandibular condyles. Post-reduction X-rays are not always necessary. Analgesia and a soft diet should be prescribed and the patient warned to avoid wide opening of the mouth in the short term [33].
Penetrating injuries to the face
Penetrating trauma to the face from gunshot, stab wounds and impaling foreign bodies is often dramatic at the time of presentation. Such isolated injury is rarely fatal, but may result in significant morbidity due to the combination of soft-tissue and bone defects. The wounding capability of penetrating projectiles (bullets and pellets) is proportional to the energy imparted to the tissue; therefore, the mass of the slug, its velocity and design and the density of the body tissue penetrated determine the amount of tissue destruction [34].
Early aggressive airway management is necessary in patients with gunshot wounds to the face, as respiratory decompensation may be rapid: approximately one-third of patients will require emergency airway intervention [35]. Shotgun and stab wounds are less likely to require an emergency airway, although the presence of a significant vascular injury or oedema remains a universal indication for airway intervention and patients with mandibular entry sites are more likely to require an emergency airway than those with midfacial entry sites. Orotracheal intubation can usually be achieved, with cricothyroidotomy the preferred alternative if necessary. Central nervous system injuries are common after gunshot injuries and CT scans of the head and cervical spine will be required [36].
Arterial injury is suggested by evidence of active bleeding and an expanding haematoma; angiography (carotid and vertebral arteries), which is required in approximately 35–40% of cases [35,36], should be performed when the bullet trajectory suggests proximity to major vessels or the skull base or where the knife or foreign body is in close proximity to a major vascular structure [36–38].
Peripheral nerve injuries, especially of the facial nerve and the mandibular branch of the trigeminal nerve, are also frequently present [36]. Careful eye examination is necessary because ocular trauma is the most common overall complication of penetrating facial trauma [39].
Antibiotics and tetanus prophylaxis are indicated and wounds are managed with conservative debridement, closed reduction of facial fractures and early repair of palatal injuries. Open facial fracture reduction is usually delayed [35].
Conclusion
Facial trauma is common in the ED, encompasses many types of injury and, after rapid exclusion of life-threatening complications, requires thorough patient evaluation to exclude other more urgent injuries. The aim of management of isolated facial injuries is the maintenance of normal function and appearance.
3.5 Abdominal trauma
Garry J Wilkes
Introduction
One in 10 deaths from trauma is due to abdominal injuries. These may be difficult to detect initially, as the abdominal cavity cannot be viewed with the naked eye, plain radiography is insensitive to intra-abdominal bleeding and solid organ injury and signs and symptoms of blood loss may be attributed to more obvious injuries. It is therefore not surprising that missed abdominal injuries are a major cause of preventable death in trauma patients. A high index of suspicion should be maintained for this important cause of morbidity and mortality.
A stepwise approach to the management of the multiply injured patient will address the possibility of significant intra-abdominal injury. The principles of initial management are to identify the presence or otherwise of such injury, the need for surgery and most appropriate timing of interventions. This process requires the presence of an experienced clinician at the earliest possible stage to direct and coordinate the trauma team. Ideally, the trauma surgeon should be present at the initial resuscitation.
The initial resuscitation, history, examination and specific investigations will be reviewed in turn.
Primary and secondary surveys
The abdomen does not normally form part of the primary survey. The unstable patient requiring continued fluid resuscitation without other sources of haemorrhage must be considered to have ongoing intra-abdominal bleeding. Specific points to remember are to expose the patient fully, including an examination of the back as well as the rectum and vagina.
History
The history and knowledge of the mechanism of injury will provide vital clues to the increased likelihood of significant intra-abdominal trauma (Box 3.5.1). Ambulance personnel will be able to provide valuable details of the incident. It is important to remember that trauma does not skip body regions and that significant intra-abdominal injuries frequently occur in the absence of external signs of abdominal trauma. Other important aspects of focused history are summarized by the acronym AMPLE: Allergies; Medications; Past medical history; Last ate and drank; Events associated with the trauma incident.
Abdominal examination
Penetrating injuries are overt and dramatic. Blunt trauma is more common and more difficult to assess on clinical grounds. Bruising and abrasions are associated with intra- abdominal pathology. The spleen and liver are the most commonly injured organs, with different patterns of injury seen in blunt and penetrating injuries (Table 3.5.1) [1]. Marks from lap-type seatbelts carry a high association with chance fractures (T12/L1), small bowel injury and pancreatic injury. Palpation of the abdomen may reveal local/generalized tenderness and evidence of peritonism, but is less reliable in detecting retroperitoneal injury and in the presence of altered sensorium. Auscultation is rarely useful; however, the absence of bowel sounds should increase the suspicion of intra-abdominal injury.
Table 3.5.1
Organ injuries associated with blunt and penetrating trauma [1]
| Blunt trauma (%) | Stabbing (%) | Gunshot (%) | |
| Spleen | 40–55 | – | – |
| Liver | 35–45 | 40 | 30 |
| Retroperitoneal haematoma | 15 | – | – |
| Small bowel | 5–10 | 30 | 50 |
| Diaphragm | – | 20 | – |
| Colon | – | 15 | 40 |
| Abdominal vascular structures | – | – | 25 |
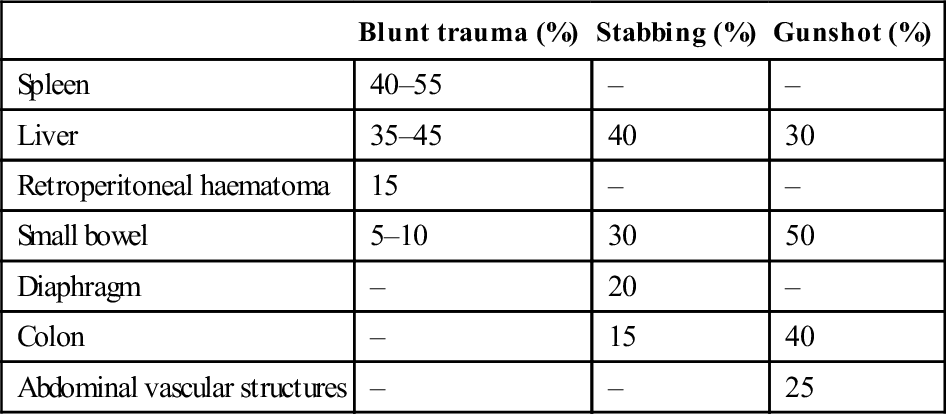
Rectal examination may demonstrate frank blood from injured bowel, a high-riding or mobile prostate from urethral rupture and may allow direct palpation of fractures or breaches of bowel wall integrity. Vaginal examination is important for similar reasons and may detect an unrecognized gravid uterus. The examination of the abdomen is not complete until the back, buttocks and perineum have been fully exposed.
Although unexplained hypotension suggests intra-abdominal haemorrhage, not all patients with significant blood loss will display the typical pattern of hypotension and tachycardia [2]. This is especially true of the younger patient. Less than one-third of patients with significant blood loss will have both hypotension and tachycardia [3]. More important are trends in pulse and blood pressure with time and in response to fluid resuscitation. Continuing falls in blood pressure and rises in pulse rate indicate ongoing haemorrhage which, if no other source is identified, must be assumed to be intra-abdominal. Abdominal distension does not occur until several litres of blood have been sequestered and can initially be confused with obesity.
Once the patient has been examined, a urinary catheter should be inserted, unless there is suspicion of a urethral injury. Blood at the urethral meatus, scrotal haematoma and a high-riding or mobile prostate are suggestive of urethral injury and a urological opinion should be sought before attempting to insert a catheter. In these circumstances, a suprapubic catheter may be preferable. Patients with a suspicion of abdominal injury also require a gastric catheter. Nasogastric catheterization is more comfortable for the patient than the oral route, but is contraindicated by evidence of basilar skull fracture. Gastric decompression may be both diagnostic and therapeutic. Penetration of the stomach or proximal small bowel will produce a bloodied aspiration. Aspiration of air will relieve gastric tamponade, which is occasionally an unrecognized cause of hypotension from impaired venous return. Urinary and gastric catheterization is mandatory prior to diagnostic peritoneal lavage (DPL).
A penetrating object, such as a knife protruding from the abdomen, should be left in situ unless it is an immediate threat to life. While tempting to remove such objects from stable patients in order to examine the patient and the wound tract, following this impulse can lead to disastrous consequences if the object is adjacent to or penetrates vascular structures. The sudden release of a tamponade may be rapidly fatal. The only place to remove a penetrating object is in an operating theatre, with staff on hand capable of dealing with all possible complications.
Investigations
The initial resuscitation of all trauma patients includes blood drawn for full blood count, urea and electrolytes, blood sugar determination, cross-matching, blood gases (if available) and a trauma radiology series. There is little place for plain radiology of the abdomen.
Gunshot wounds are unpredictable in their path, can produce secondary missiles and cavitation effects and all require laparotomy. Stab wounds that have penetrated the peritoneum may also require laparotomy and need immediate assessment by an experienced trauma surgeon. In cases where immediate laparotomy is indicated, the patient should be escorted to theatre with no further investigations (Box 3.5.2). Further investigations, such as trauma ultrasound or DPL, may assist in determining the need for or timing of laparotomy if other urgent procedures are also required. The final order is determined by the trauma team leader.
Unstable patients require surgical intervention as soon as possible. Stable patients can be investigated further, allowing better planning of further management. The difficulty arises in the common situation where there are multiple injuries and only a suspicion – not confirmation – of significant intra-abdominal pathology. Some patients are at risk of abdominal injury but cannot be assessed on clinical grounds. These include those with head, chest and spinal injuries, intoxicated or sedated patients and those who will be inaccessible while undergoing lengthy operations on other body regions. For these patients, it is important to make a further assessment of the presence or otherwise of intra-abdominal injury. Additional investigations of benefit are ultrasound, DPL and computed tomography (CT). Each has advantages and disadvantages (Table 3.5.2). They may also be consecutive and complementary, thereby minimizing the disadvantages of each individually. Areas poorly imaged by all modalities are hollow organ injuries, such as small bowel rupture and vascular compromise. Serial clinical examination is essential to detect these injuries, even if investigation results are normal.
Table 3.5.2
Comparison of abdominal CT, DPL and ultrasound for investigation of abdominal trauma
| Abdominal CT | DPL | Ultrasound |
| Advantages | ||
| Anatomical information | Rapid, cheap, sensitive | Rapid, portable, repeatable |
| Non-invasive | Minimal training | Non-invasive |
| Visualizes retroperitoneum | Ideal in unstable patients | Ideal in unstable patients |
| Also views chest, pelvis | Can be done in resus. room | Can be done in resus. room |
| Also views chest, pelvis | ||
| Disadvantages | ||
| Not suitable for unstable patients | Not organ specific | Requires specific training |
| Requires transport from resus. room | False negative | Operator dependent |
| Patient safety | Retroperitoneal injuries | False negative |
| Inaccessible while scanning | Hollow viscus injury | Retroperitoneal injuries |
| Time | Diaphragm injury | Hollow viscus injury |
| Cost | Iatrogenic injury | Diaphragm injury |
| False negative | Fluid and gas introduced during the procedure interfere with subsequent imaging | False positive |
| Hollow viscus injuries | Ascites | |
| IV contrast reactions | ||
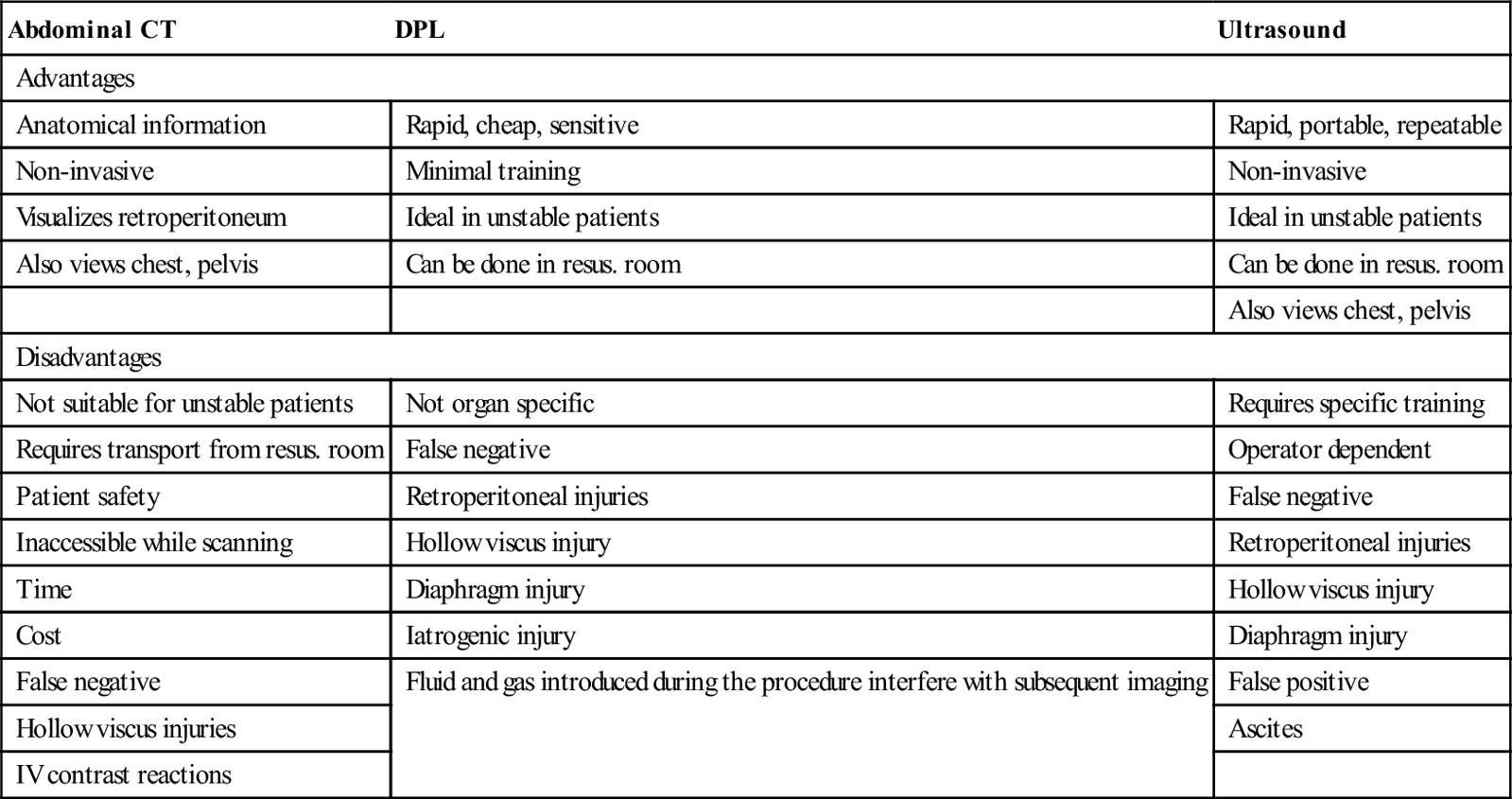
DPL was first described in 1965 and can be completed in less than 4 minutes by experienced operators [4,5]. However, DPL is of limited value when CT or FAST are available and the increasing availability of these modalities has largely resulted in this procedure no longer being used in trauma resususcitation.
Abdominal CT
Abdominal CT is non-invasive and provides precise anatomical details of intra-abdominal pathology. The major disadvantages are associated with the use of IV contrast and the need for the patient to be transported from the resuscitation area to the CT scanner, where they are not accessible during the procedure. Intravenous contrast may rarely produce allergic reactions and can precipitate or exacerbate renal impairment, particularly in higher doses and in the presence of renal hypoperfusion and hypofunction. Although modern machines complete scans in a single breath-hold, time is still required to load and unload the patient. Transport and transfer are times of maximum patient risk and minimum monitoring. Therefore, only stable patients are suitable for transfer for CT scanning. Unstable patients require further resuscitation or operative intervention if this is unsuccessful. The definition of stable is not agreed. The final decision can only be made by the most experienced physician available, although a systolic pressure of at least 90 mmHg and no requirement for additional fluids after correction of estimated losses would be minimum requirements.
Focused assessment sonography in trauma
Focused ultrasound is a skill practised by many clinicians involved in acute trauma management. Abdominal ultrasound is non-invasive, may be done at the bedside and can be repeated as needed. The technique can be easily learnt by clinicians and completed in less than 5 min without interfering with the function of a trauma resuscitation team [6]. Ultrasound combines the advantages of being rapid, accurate and non-invasive and can be performed at the bedside. It is at least as accurate as DPL and, in experienced hands, has similar results to CT in determining the presence of intraperitoneal injury. As a decision-making tool for identifying the need for laparotomy in hypotensive patients (systolic BP<90), FAST has a sensitivity of 100%, specificity of 96% and negative predictive value (NPV) of 100% [7,8]. It is the bedside investigation of choice if an experienced operator is available.
Laparoscopy
Laparoscopy has been investigated in some centres, but the skills required and the time needed for a thorough examination limit the widespread usefulness of this modality in acute blunt trauma. However, it is useful in excluding peritoneal penetration in abdominal stab wounds.
Penetrating injuries
Penetrating injuries produce a different pattern of injury (see Table 3.5.1) and are managed in a different manner from blunt injuries (Figs 3.5.1 and 3.5.2). Cavitation effects and the potential for secondary missiles causing widespread injury mandate formal laparotomy in all cases. Stab wounds with haemodynamic compromise or other indications should also proceed to laparotomy without delay for other investigations. Local exploration of stab wounds by experienced surgeons in patients without evidence of internal injury may be useful, as up to one-third of wounds do not breach the peritoneum. Selected patients may then be managed conservatively.