Chapter 17 2ST/2Gr, 4ST, and 3ST/2Gr Techniques
Deciding Which Hamstring Configuration to Use
Introduction
Use of the four-strand hamstring (4HS) graft using the semitendinosus (ST) with or without the gracilis (Gr) has increased dramatically in the past 5 years. This graft has long been considered to have lower morbidity than bone–patellar tendon–bone (BPTB) grafts. After reports showed its clinical stability results to meet or exceed those of the BPTB,1–7 its use began to significantly increase. 2ST/2Gr is the most commonly used hamstring graft, followed by 4ST. However, a total of six different multistrand hamstring graft configurations have been reported and are in current use. This chapter will describe the advantages of each configuration according to the five parameters involved in decision making. Graft preparation techniques will also be described.
The Parameters for Choosing A Hamstring Graft Configuration
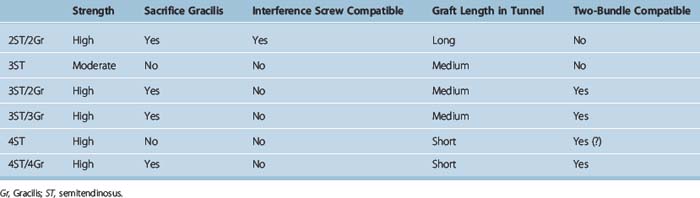
Five parameters (Table 17-1 and see later discussion) will drive decision making regarding which HS graft, or soft tissue graft in general, will be used. The first three parameters are available graft length in the tunnel, the type of fixation that can be used, and whether the gracilis must be sacrificed. These are generally themost important considerations to most orthopaedic surgeons. The last two parameters, relative graft strengths and whether it is double-bundle compatible, are important to some.
1 Is the Graft Long Enough to Allow Adequate Tunnel Healing?
In our experience, ST harvests range in length from 24 to 34 cm, with most being between 26 and 30 cm in usable length. Intraarticular anterior cruciate ligament (ACL) length is 3 to 3.5 cm.8 Roughly 1 cm of shortening occurs as a result of whipstitch implantation. Thus, for example, a 27-cm graft will be 26 cm after suturing. When quadrupled, this length is 6.5 cm. Subtracting 3 cm for the intraarticular portion leaves 3.5 cm of graft for both tunnels, or about 1.75 cm or 17.5 mm for each tunnel. If the ST is only doubled and not quadrupled, the resultant 12 cm or longer graft can provide 4 cm or more of graft length in each tunnel. Some surgeons9 will use 4ST if the ST is 30 cm or longer and 2ST/2Gr if the ST harvest is less than 30 cm.
The Argument for Greater Length Being Necessary
Many surgeons are not comfortable with graft lengths of less than 2 cm in each tunnel. The principal argument in favor of this is the study by Greis et al10 that shows greater pull-out strength as graft length increases.
The Argument for Less Length Being Sufficient
However, there is a significant body of data indicating that 15 mm or even less graft in a tunnel is acceptable. A recent study by Zantop et al in goats using Endobutton fixation showed no difference in load to failure between 15 mm and 25 mm of graft in the tunnel.11 A study by Yamazaki et al in dogs using whipstitch cortical screw post fixation showed no difference between 5 mm and 15 mm.12 Equally persuasive in favor of shorter lengths being acceptable is the clinical experience of a number of experienced surgeons such as Rosenberg and Cooley2 and Paulos13 who have had excellent results using 15-mm grafts. We have also used 15 mm as a minimum without a graft failure.
2 Is the Graft Long Enough to Allow Direct Tibial Fixation or Only Indirect?
Direct fixation includes all interference screw and interference screw–based techniques such as Intrafix and techniques that rely on direct friction with the graft, such as the WasherLoc. Indirect fixation uses a fabric interface with the graft such as the whipstitch post technique or Fastlok. As seen in Table 17-1, use of the Gr as well as the ST is necessary to be certain of a long-enough graft to ensure the use of direct fixation techniques.
3 Is the Gracilis Sacrificed?
The Gracilis Is not Really a Hamstring
One argument against the 2ST/2Gr graft is that it disables not one but two hamstring muscles because the Gr is also harvested in addition to the ST. However, the Gr is not really a hamstring. Gray’s Anatomy14 lists only three hamstring muscles: the biceps femoris, semimembranosus, and ST. All are innervated by the sciatic nerve; all flex the knee. The Gr is not listed as a hamstring. Rather, the Gr is listed with the adductors longus, brevis, and magnus as “medial femoral muscles.” All of these muscles, including the Gr, are innervated by the obturator nerve. The gracilis’ action is listed as “adducts the thigh.” Thus, the loss of the Gr is not the loss of a second hamstring. Rather, it is the loss of an accessory adductor, much as the loss of the ST is the loss of an accessory hamstring.
What Is Lost by Harvesting the Gracilis in Addition to the Semitendinosus?
Chapter 67 reviews strength after hamstring harvest. Hamstring strength can be restored in virtually 100% of patients in our experience. Specific testing has noted a small decrease in peak flexion torque at high flexion angles and decreased tibial internal rotation strength in flexion; however, no clinical deficit has ever been reported in function as a result of the addition of Gr harvest relative to ST alone. On theoretical grounds, some have avoided Gr harvest in sprinters and soccer players.15 However, performance deficits or subjective complaints have not been reported in this group. Anecdotally, we have performed bilateral 2ST/2Gr in a professional soccer player with excellent subsequent performance.
4 How Strong Is the Graft?
Using the data from the classic study of Noyes et al16 in which the ST was 70% of the strength of the native ACL and the Gr was 49% of the strength, extrapolated hamstring graft strengths can be estimated. The 4ST would be 280%, the 2ST/2Gr would be 238%, the 3ST would be 210%, and the 2ST would be 140%. The 4ST and 2ST/2Gr have produced very high stability rates in clinical series.2–7 The 2ST has been associated with low rates, although this may well be largely due to the outmoded fixation that was used when those studies were done.17–19 Regardless of whether this is true, few surgeons today are comfortable with only a 2ST graft. The 3ST graft has produced high stability in some20 but not all21 series. This mixed clinical performance and the lower strength of the graft coupled with the increased complexity of using an odd-stranded graft in the femur has resulted in this graft being seldom used.
5 Is the Graft Double-Bundle Compatible?
Yasuda et al22 have reported a six-strand, double-bundle technique with 3ST/3Gr, as described in Chapter 22. Christel uses a 2ST anteromedial (AM) bundle and either a 2Gr or 3Gr (if the Gr is small) posterolateral (PL) bundle, as described in Chapter 23. Zhao et al have reported a 4ST AM and 4Gr PL bundle eight-strand technique.23 Generally, excellent stability has been reported with these techniques. As with the later-described 5HS single-bundle technique, 6HS and 8HS techniques have not seemed to have the problems associated with the large size of these grafts, which are significantly larger than the native ACL. 2ST/2Gr has generally not been used in a double-bundle configuration. Single-bundle techniques use primarily AM bundle positioning. This has produced high success rates. The argument for double-bundle techniques supposes that the addition of a PL bundle can only help stability. However, PL bundle techniques are new and questionable to many. If the AM bundle is significantly weakened to provide a graft for the PL bundle, then the entire graft may be too weak if the PL technique is indeed not providing significant additional strength. Taking the Gr away from the AM bundle would leave only a 2ST graft, which alone has performed poorly in the literature in the past. It would seem safer to leave a stronger AM bundle, at least a 3ST graft, which would then be augmented by the PL bundle. Gobbi has reported excellent success with a 2ST AM bundle, but he has used the stronger 2ST graft rather than 2Gr for a PL bundle (see Chapter 24).
Graft Preparation Techniques
2ST/2Gr Graft Preparation Technique Using Endobutton Femoral and Whipstitch Posttibial Fixation
Cleaning and First Whipstitch Implantation
After harvest the tendons should be cleaned of muscle tissue. We place whipstitches (see Chapter 42) in the combined tibial attachment of #5 braided nonabsorbable or #2 braided high-strength nonabsorbable suture such as Fiberwire (Arthrex, Naples, FL) or ultra-braid (Smith & Nephew, Andover, MA). We do not cut the graft at this point and do not whipstitch the other end. It is better to determine length once tunnel lengths have been determined.
Troubleshooting
What if Either the ST or Gr Is Cut Too Short to Double?
We have not had this occur using the posterior mini-incision harvest technique (see Chapter 13). However, if graft length is questionable, the first step should be to precisely measure the intraarticular length. The minimum graft we have used is this length plus 15 mm for each of the tibial and femoral tunnels. Thus, a 30-mm intraarticular length would allow a 30 + 15 + 15 = 60 mm total graft. Six centimeters doubled is 12 cm. Adding 1 cm for shortening yields a 13-cm graft. Thus, all that should be necessary for most knees for a 4ST/Gr graft is a total length of 13 cm or 14 cm, allowing for measurement error. If the surgeon has this length, then he or she should be fine to proceed. If either the ST or Gr is shorter than this length, then the surgeon should plan to triple the other tendon to add to the single short limb of the short tendon. The two possibilities would thus be either 3ST/1Gr (stronger than 2ST/2Gr) or 1 ST/3Gr (not as strong as 2ST/2Gr but more than sufficiently strong). We would then implant whipstitches in the free ends. Whipstitch post fixation or Endobutton could then be used for femoral fixation. Cross-pin fixation would generally be difficult without the ability to loop each graft.
Five Strand Using 3ST/2Gr
Surgical Technique
The ST and Gr are harvested in the usual fashion. The ST is measured and, provided that it is at least 22.5 cm in length, the proximal one-third is sectioned from the distal two-thirds. For example, a 24-cm ST would be cut to leave 16 cm intact with its insertion, and the proximal 8 cm would be cut off to use as a single limb. This tissue would otherwise be discarded. In our experience the ST is always at least 24 cm in length, and no more than 15 cm is ever required for 2ST/2Gr. Thus, there is almost always a third (if not a fourth) limb of ST that would otherwise be discarded. Number 2 whipstitches are placed in each end of this extra graft limb. The whipstitches from one end are tied one to one around the fabric loop of the Endobutton loop (Fig. 17-1). The sutures from the other end are tied one to one around the tibial cortical screw.
Results
We recently presented an 8- to 9-year follow-up of a five-strand technique using whipstitch post fixation on both the tibia and femur24 in 20 consecutive patients. This was the first report of a greater than four-strand HS graft using a single-bundle technique. No graft failures were found, and 89% of the grafts were within 1 mm of the opposite knee. The mean side-to-side KT-1000 difference of 0.44 mm is the lowest reported for an ST/Gr graft. We compared this group with a previously reported high-stability 2ST/2Gr cohort and found significantly higher stability with the five-strand graft.
Uses
This technique is useful in patients with ligamentous laxity, small tendons, or other stability risk factors for which the strongest possible graft is required. It is also of use in double-bundle techniques. The 3ST part of the graft allows the AM bundle to approximate the strength of a 2ST/2Gr single bundle (210% versus 238% of the approximate strength of the native ACL by extrapolation from the data of Noyes25). Thus, the use of the Gr for the PL bundle does not need to significantly weaken the AM bundle, which closely corresponds to what most surgeons were using for a single bundle. This provides a measure of insurance in case the more difficult PL bundle is misplaced or inadequately tightened. Because double-bundle techniques are new to most surgeons, this should essentially eliminate any “learning curve” laxity as facility with the double-technique is gained and as further research shows the best ways to perform the double-bundle procedure.
Conclusions
1 Prodromos CC, Joyce BT, Shi K, et al. A meta-analysis of stability after anterior cruciate ligament reconstruction as a function of hamstring versus patellar-tendon graft and fixation type. Arthroscopy. 2005;21:1202-1208.
2 Cooley VJ, Deffner KT, Rosenberg TD. Quadrupled semitendinosus anterior cruciate ligament reconstruction: 5-year results in patients without meniscus loss. Arthroscopy. 2001;17:795-800.
3 Gobbi A, Tuy B, Mahajan S, et al. Quadrupled bone-semitendinosus anterior cruciate ligament reconstruction: a clinical investigation in a group of athletes. Arthroscopy. 2003;19:691-699.
4 Prodromos CC, Han YS, Keller BL, et al. Stability results of hamstring anterior cruciate ligament reconstruction at two- to eight-year follow-up. Arthroscopy. 2005;21:138-146.
5 Feller JA, Webster KE. A randomized comparison of patellar tendon and hamstring tendon anterior cruciate ligament reconstruction. Am J Sports Med. 2003;31:564-573.
6 Yasuda K, Kondo E, Ichiyama H, et al. Anatomic reconstruction of the anteromedial and posterolateral bundles of the anterior cruciate ligament using hamstring tendon grafts. Arthroscopy. 2004;20:1015-1025.
7 Gobbi A, Mahajan S, Zanazzo M, et al. Patellar tendon versus quadrupled bone-semitendinosus anterior cruciate ligament reconstruction: a prospective clinical investigation in athletes. Arthroscopy. 2003;19:592-601.
8 Duthon VB, Barea C, Abrassart S, et al. Anatomy of the anterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2006;14:204-213.
9 Prodromos CC, Fu F, Howell S, et al. Controversies in soft tissue anterior cruciate ligament reconstruction. Presented at the 2006 Symposium of the American Academy of Orthopaedic Surgeons, AAOS Symposium—Controversies in Soft Tissue Reconstruction, Chicago. March, 2006.
10 Greis PE, Burks RT, Bachus K, et al. The influence of tendon length and fit on the strength of a tendon-bone tunnel complex: a biomechanical and histologic study in the dog. Am J Sports Med. 2001;29:493-497.
11 Zantop T, Brucker P, Bell K, et al. The effect of tunnel-graft length on the primary and secondary stability in ACL reconstruction: a study in a goat model. Presented at the 2006 meeting of the European Society of Sports Traumatology, Knee Surgery, and Arthroscopy, Innsbruck, Australia. May, 2006.
12 Yamazaki S, Yasuda K, Tomita F, et al. The effect of intraosseous graft length on tendon-bone healing in anterior cruciate ligament reconstruction using flexor tendon. Knee Surg Sports Traumatol Arthrosc. 2006;14:1086-1093.
13 Paulos L. Personal communication. May 2006.
14 Goss CM. Muscles and Fasciae. In Gray’s anatomy, ed 29, Philadelphia: Lea and Febiger, Courage Books; 1973:495-503.
15 Gobbi A, Domzalski M, Pascual J, et al. Hamstring anterior cruciate ligament reconstruction: is it necessary to sacrifice the gracilis? Arthroscopy. 2005;21:275-280.
16 Noyes FR, Butler DL, Grood ES, et al. Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J Bone Joint Surg Am. 1984;66A:344-352.
17 Meyestre J, Vallotton J, Benvenuti J. Double semitendinosus anterior cruciate ligament reconstruction: 10-year results. Knee Surg Sports Traumatol Arthrosc. 1998;6:76-81.
18 Aglietti P, Buzzi R, Menchetti P, et al. Arthroscopically assisted semitendinosus and gracilis tendon graft in reconstruction for acute anterior cruciate ligament injuries in athletes. Am J Sports Med. 1996;24:726-731.
19 Anderson A, Snyder R, Lipscomb B. Anterior cruciate ligament reconstruction: a prospective randomized study of three surgical methods. Am J Sports Med. 2001;29:272-279.
20 Goradia VK, Grana WA. A comparison of outcomes at 2 to 6 years after acute and chronic anterior cruciate ligament reconstructions using hamstring tendon grafts. Arthroscopy. 2001;17:383-392.
21 Harilainen A, Sandelin J, Jansson KA. Cross-pin femoral fixation versus metal interference screw fixation in anterior cruciate ligament reconstruction with hamstring tendons: results of a controlled prospective randomized study with 2-year follow-up. Arthroscopy. 2005;21:25-33.
22 Yasuda K, Kondo E, Ichiyama H, et al. Clinical evaluation of anatomic double-bundle anterior cruciate ligament reconstruction procedure using hamstring tendon grafts: comparisons among three different procedures. Arthroscopy. 2006;22:240-251.
23 Zhao J, Peng X, He Y, et al. Two-bundle anterior cruciate ligament reconstruction with eight-stranded hamstring tendons: four-tunnel technique. Knee. 2006;13:36-41.
24 Prodromos CC, Joyce BT. Five-strand hamstring ACL reconstruction: a new technique with better long-term stability than four-strand. Presented at the 2006 meeting of the Arthroscopy Association of North America Hollywood, FL. May, 2006.
25 Noyes FR, Butler DL, Grood ES, Zernicke RF, Hefzy MS. Biomechanical analysis of human ligament grafts used in knee-ligament repairs and reconstructions. J Bone Joint Surg Am. 1984;66-A:344-352.