Administration
Edited by George Jelinek
27.1 Emergency department staffing
Sue Ieraci and Julie Considine
General principles
Patients requiring emergency care have the right to timely care by skilled staff. The aim of staffing an emergency department is ultimately to provide care in an acceptable time according to the patient’s clinical urgency (triage category). Staff working in the emergency department also have the right to safe and manageable working conditions and reasonable job satisfaction.
As the activity of an emergency department fluctuates in both volume and acuity, a threshold level of staffing and resources is required in order to be prepared for likely influxes of patients. In addition, the staffing number and mix needs to take account of the important teaching role of emergency departments.
The precise numbers and designation of medical, nursing, allied health and other staff employed will be determined by the local work practices (what tasks are carried out and by whom). This chapter discusses staffing requirements under the current Australasian model of emergency department work practices. This includes a major supervisory and teaching role for consultants and a significant proportion of specialist trainees and junior medical staff in the medical workforce, with a range of tasks, including venepuncture, test requisitioning and written documentation. In addition, roles are expanding into wider realms, such as toxicology, ultrasound and academic and observation medicine. Nursing roles range from bedside monitoring, physical care and treatment to advanced practice roles, including the initiation of tests and treatment.
Estimating medical workload
Emergency department (ED) case mix and costing studies have sought to measure the medical time commitment for various clinical conditions. Table 27.1.1 describes the approximate average medical time commitment for each of the Australasian Triage Scale categories [1]:
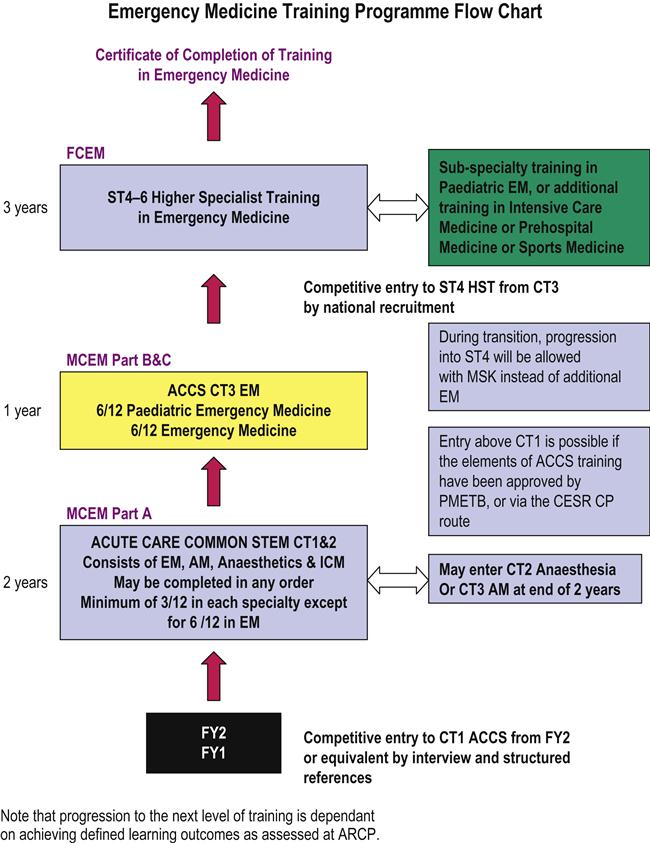
 The workforce should be resourced and organized so that patients are treated within the benchmark times for their clinical acuity (triage category). The Australasian College for Emergency Medicine (ACEM) has defined benchmarks for waiting time by triage category (Table 27.1.2) [2].
The workforce should be resourced and organized so that patients are treated within the benchmark times for their clinical acuity (triage category). The Australasian College for Emergency Medicine (ACEM) has defined benchmarks for waiting time by triage category (Table 27.1.2) [2].
Table 27.1.2
Benchmarks for waiting time by triage category
| Category 1 | Category 2 | Category 3 | Category 4 | Category 5 | |
| Treatment acuity | Immediate | Within 10 min | Within 30 min | Within 60 min | Within 120 min |
| Benchmark performance (%) | 98 | 95 | 90 | 90 | 85 |
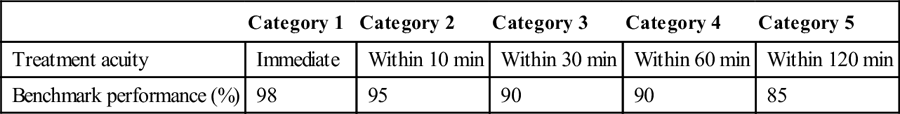
Table 27.1.1
Australasian Triage Scale categories
| NTS category | Medical time (min) |
| Category 1 | 160 |
| Category 2 | 80 |
| Category 3 | 60 |
| Category 4 | 40 |
| Category 5 | 20 |
Structure of medical staff
The medical workforce of Australasian emergency departments currently includes the following categories:
 consultants (specialist emergency physicians), including a medical director
consultants (specialist emergency physicians), including a medical director
 registrars (specialist trainees)
registrars (specialist trainees)
 senior non-specialist staff: experienced hospital medical officers
senior non-specialist staff: experienced hospital medical officers
The specialist practice of emergency medicine includes non-clinical roles (including departmental management and administration, planning, education, research and medicopolitical activities) as well as clinical roles. The non-clinical workload of an individual department varies with its size and role, the structure of its staffing and the other management systems within the institution. For senior staff, clinical work generally includes coordination of patient flow, bed management and supervision and bedside teaching of junior staff, in addition to direct patient care. Some emergency physicians may have other particular roles, such as retrieval and hyperbaric medicine or toxicology services. The increasing number of academic staff may have major research and teaching commitments.
To cover these roles, the ACEM recommends a minimum of 30% non-clinical time for consultants (more for directors of departments and directors of emergency medicine training) and 15% non-clinical time for registrars.
Throughout Australasia, EDs are experiencing increasing levels of activity. The calculation of medical staff numbers required for a particular department must include not only the extent of consultant cover required, but also the clinical workload and performance, local work practices and the nature of clinical and non-clinical roles. Because of variations in roles and work practices between sites, it is not possible to devise a staffing profile that is universally appropriate. Other recent changes in staffing patterns include employment across a network, increasing part-time work and sessional contract arrangements. Many emergency physicians are diversifying their practice profile to achieve a balanced and sustainable career, combining salaried and contract work, different types of hospitals and part-time work with a range of other interests.
Estimating nursing workload
Australian models for calculating ED nursing workload include the Emergency Care Workload Unit [3] (based on triage category and admission status) and the Victorian Nurse-to-Patient Ratio model [4] (using patient dependencies). Additionally, a minimum skill mix is required to manage the acute and complex workload. In addition to the bedside nursing workload, there are requirements to provide for education and training, patient flow and both clinical and departmental administrative roles. Larger departments require clinical managers on every shift.
Nurse staffing structure
In Australia, there are three levels of nurses registered with the Australian Health Professionals Regulation Agency (AHPRA):
Enrolled nurses work under the supervision of registered nurses and their scope of practice is generally limited to general adult or paediatric areas. One of the major changes to enrolled nurse scope of practice in recent years is their ability to administer medications and, depending on their level of education and registration notation, they may administer oral or parenteral (including intravenous) medications.
The majority of nurses working in emergency departments are registered nurses who have completed a 3-year bachelor degree typically followed by a 12-month graduate nurse programmme. In many states, 6–12 month transition programmes to specialty practice in emergency nursing are offered to novice nurses wishing to pursue a career in emergency nursing and are often a precursor to postgraduate studies in emergency nursing. Australian emergency nurses have one of the highest standards of education worldwide with the majority holding a graduate certificate or graduate diploma in emergency nursing. Postgraduate qualifications are considered by many as the industry standard for complex emergency nursing roles, such as resuscitation and triage. Triage assessment is a nursing role in Australia and emergency nurses are often responsible for advanced patient assessment, initiation of investigations and symptom relief care prior to medical assessment. Emergency nurses are also primarily responsible for ongoing surveillance and escalation of care in the event of deterioration. Advanced emergency nursing roles for postgraduate qualified emergency nurses are widespread in Australia and nurse initiated pathology, X-rays and analgesia are among common examples. There are also a number of Masters and PhD prepared emergency nurses in Australia working in various advanced clinical roles, joint clinical–academic appointments, nursing education and nursing management.
At the time of writing, there were over 700 endorsed nurse practitioners in Australia and emergency nursing has the largest cohort of nurse practitioners. In Australia, to be endorsed as a nurse practitioner, nurses must complete a clinically based master’s degree or a specific nurse practitioner master’s degree, demonstrate experience in advanced nursing practice in a clinical leadership role in emergency nursing and have undertaken an approved course of study for prescribing scheduled medicines as determined by the NMBA. Nurse practitioners form a key workforce strategy in managing demand for emergency care and are able independently to manage specific patient groups within their defined scope of practice, including prescribing medications, ordering diagnostic tests, referring to specialists and discharging patients home. Published research shows that emergency nurse practitioners can provide safe, efficient and timely care and are a valuable member of the emergency department team [5,6].
Allied health, clerical and other support staff
Allied health, clerical and other ancillary staff are essential to the efficient provision of emergency department services. They should be specifically trained and experienced for emergency department work. Clerical staff have a crucial role, encompassing reception, registration, data entry and communications within and outside the department, as well as maintenance of medical records. Dedicated paramedical staff, including therapists and social workers, are important in providing thorough assessment and management of patients, including participating in disposition decisions and discharge support. Other staff, such as porters and ward assistants, play an important role in releasing clinical staff from non-clinical roles as well as movement of patients within and beyond the emergency department.
Optimizing work practices
Traditional hospital work practices involve systems and tasks that are inefficient for the smooth running of modern, busy emergency departments. In a work environment with a rapid patient throughput and large numbers of staff, efficient work practices are crucial in optimizing clinical performance as well as job satisfaction. A review of staff numbers and seniority cannot provide maximum benefit without consideration of the way the work is done, what tasks are done and by whom.
A review of emergency department work practices can encompass the following principles:
As the emergency department workforce develops greater seniority and specialization and the demands of patient care increase, it is no longer possible to justify outdated work practices. Local research has shown that it is possible to improve clinical service provision by reorganizing roles and tasks in a sustainable way [7]. The opportunity exists to create a work environment that both delivers good clinical service and is rewarding and satisfying for staff.
27.2 Emergency department layout
Matthew WG Chu
Introduction
The emergency department (ED) is a core clinical unit within a hospital. The experience and satisfaction of patients attending the ED are significant contributors to the public image of the hospital. Its primary function is to receive, triage, stabilize and provide emergency care to patients who present with a wide range of undifferentiated conditions which may be critical to semi-urgent in nature. The ED may contribute between 15 and 75% of a hospital’s total number of admissions. It plays an important role in the hospital’s response to major incidents and trauma and in the reception and management of disaster victims. To optimize its core function, the department should be purpose-built, providing a safe environment for patients, their carers and staff. The physical environment includes an effective communication system, appropriate signposting, adequate ambulance access and clear observation of relevant areas from the triage area. There should be easy access to the resuscitation area and quiet and private areas should cater for patients and their relatives. Adequate staff facilities and tutorial areas should be available. Clean and dirty utilities and storage areas are also required.
Design considerations
The design of the department should promote rapid access to every area with the minimum of cross-traffic. There must be proximity between the resuscitation and the acute treatment areas for non-ambulant patients. Supporting areas, such as clean and dirty utilities, the pharmacy room and equipment stores, should be centrally located to prevent staff traversing long distances. The main aggregation of clinical staff will be at the staff station in the acute treatment area. This is the focus around which the other clinical areas should be grouped.
Lighting should conform to national standards and clinical care areas should have exposure to daylight whenever possible to minimize patient disorientation. Climate control is essential for the comfort of both patients and staff. Each clinical area needs to be serviced with medical gases, suction, scavenging units and power outlets. The minimum suggested configuration for each type of clinical area is outlined in Table 27.2.1.
Table 27.2.1
Configurations for clinical areas
| Resuscitation | Acute treatment | Specialty plaster/procedure | Consultation room | |
| Oxygen outlets | 3 | 2 | 2 | 1 |
| Medical air outlets | 2 | 1 | 1 | – |
| Suction outlets | 3 | 2 | 1 | 1 |
| Nitrous oxide | 1 | 1 | 1 | – |
| Scavenging unit | 1 | 1 | 1 | – |
| Power outlets | 16 | 8 | 8 | 4 |
Medical gases should be internally piped to all patient care areas and adequate cabling should ensure the availability of power outlets to all clinical and non-clinical areas. Although patient and emergency call facilities are often considered, there is often inadequate provision for telephone and information technology ports. The availability of wireless technology to support equipment, such as computer on wheels (COWS), is desirable. Emergency power must be available to all lighting and power outlets in the resuscitation and acute treatment areas. All computer terminals in the department should have access to emergency power and emergency lighting should be available in all other areas. The electricity supply should be surge protected to protect electronic and computer equipment, physiological monitoring areas should be cardiac protected and other patient care areas should be body protected.
Approximately 35–45% of the total area of the department is circulation space. An example of this would be the provision of corridors wide enough to allow the easy passage of two hospital beds with attached intravenous fluids. Although circulation space should be kept to a minimum, functionality, fire safety and occupational health and safety requirements also need to be considered. The floor covering in all patient care areas should be durable and non-slip, easy to clean, impermeable to water and body fluids and with properties that reduce sound transmission and absorb shocks. Areas accommodating the administrative functions, interview and counselling and support of distressed relatives should be carpeted.
Size and composition of the emergency department
The appropriate size of the ED depends on a number of factors: the census, patient mix and acuity, the admission rate, the defined performance levels manifested in waiting times, the length of stay of patients in the ED and the role delineation of the department. Departments of inadequate size are uncomfortable for patients, often function inefficiently and may significantly impair patient care. Overcrowding of patients increases mortality and morbidity with the risk of infectious disease transmission and increases harmful cognitive stimulation for patients with mental disturbance. For the average Australasian ED with an admission rate of approximately 25–35%, its total internal area (excluding departmental radiological imaging facilities and observation/holding ward) should be approximately 50 m2/1000 yearly attendances. The total number of patient treatment areas (excluding interview, plaster and procedure rooms) should be at least 1/1100 yearly attendances and the number of resuscitation areas should be at least one for every 15 000 yearly attendances. It is recommended that, for departments with average patient acuity, at least half the total number of treatment areas should have physiological monitoring available.
Clinical areas
Individual treatment areas
The design of individual treatment areas should be determined by their specific functions. Adequate space should be allowed around the bed for patient transfer, assessment, performance of procedures and storage of commonly used items. The use of modular storage bins or other materials employing a similar design concept should be considered.
To prevent transmission of confidential information, each area should be separated by solid partitions that extend from floor to ceiling. The entrance to each area should be able to be closed by a movable partition or curtain.
Each acute treatment bed should have access to a physiological monitor. Central monitoring is recommended and monitors should ideally be of the modular type, with recording and print capabilities. The minimum monitored physiological parameters should include oxygen saturation (SpO2), non-invasive blood pressure (NIBP), electrocardiogram (ECG) and temperature. Monitors may be mounted adjacent to the bed on an appropriate pivoting bracket or be movable.
All patient care areas, including toilets and bathrooms, require individual patient call facilities and emergency call facilities, so urgent assistance can be summoned when required. In addition, an examination light, a sphygmomanometer, ophthalmoscope and otoscope, waste disposal unit should all be immediately available. Hand washing facilities should be easily accessible.
Resuscitation area
This area is used for the resuscitation and treatment of critically ill or injured patients. It must be large enough to fit a standard resuscitation bed, allow access to all parts of the patient and allow movement of staff and equipment around the work area. As space must also be provided for equipment, monitors, storage, wash-up and disposal facilities, the minimum suitable size for such a room is usually 35 m2 (including storage area) or 25 m2 (excluding storage area) for each bed space in a multibedded room. The area should also have visual and auditory privacy for both the occupants of the room and for other patients, their carers and relatives. The resuscitation area should be easily accessible from the ambulance entrance and the staff station and be separate from the patient circulation areas. In addition to standard physiological monitoring, invasive pressure, capnography and temperature probe monitoring should be available. Other desirable features include a ceiling-mounted operating theatre light, a radiolucent resuscitation trolley with cassette trays, overhead X-ray and lead lining of walls and partitions between beds.
Acute treatment area
This area is used for the assessment, treatment and observation of patients with acute medical or surgical illnesses. Each bed space must be large enough to fit a standard mobile bed, with adequate storage and circulation space. The recommended minimum space between beds is 2.4 m and each treatment area should be at least 12 m2. All of these beds should be positioned to enable direct observation from the staff station and easy access to the clean and dirty utility rooms, procedure room, pharmacy room and patient shower and toilet.
Single rooms
These rooms should be used for the management of patients who require isolation, privacy or who are a source of visual, olfactory or auditory distress to others. Deceased patients may also be placed there for the convenience of grieving relatives. These rooms must be completely enclosed by floor-to-ceiling partitions but allow controlled visual access and have a solid door. Each department should have at least two such rooms. The isolation room is used to treat potentially infectious patients. The isolation room should be located in an area which does not allow cross infection to other patients in the emergency department. Each isolation room should have negative-pressure ventilation, an ante room with change and scrub facilities and be self-contained with en-suite facilities. A decontamination area should be available for patients contaminated with toxic substances. In addition to the design requirements of an isolation room, this room must have a floor drain and contaminated water trap. The decontamination area should be directly accessible from the ambulance bay and be located in an area which will prevent the ED from being contaminated in the event of a chemical or biological incident. Single rooms should otherwise have the same requirements as acute treatment area bed spaces.
Acute mental health area
This is a specialty area designed specifically for the assessment, protection and containment of patients with actual or potential behavioural disturbances. Ideally, each unit comprises two separate but adjacent rooms allowing for interview, behavioural assessment and treatment functions. Each room should have two doors large enough to allow a patient to be carried through and must be lockable only from the outside. One of the doors may be of the ‘barn door’ type, enabling the lower section to be closed while the upper section remains open. This allows direct observation of and communication with the patient without requiring staff to enter the room. Each room should be squarely configured and be at least 16 m2 in size to enable a restraint team of five members to contain a patient without the potential of injury to a staff member. The examination/treatment room will facilitate physical examination or chemical restraint when indicated. The unit should be shielded from external noise, located as far away as possible from external sources of stimulation (e.g. noise, traffic) and must be designed in such a way that direct observation of the patient by staff outside the room is possible at all times. Services, such as electricity, medical gases and air vents or hanging points, should not be accessible to the patient. It is preferable that furniture be made of material which would prevent it being used as a weapon or inflicting self-harm. A smoke detector should be fitted and closed-circuit television may be considered as an adjunct to direct visual monitoring. Psychiatric Emergency Care Centres (PECC) have been introduced in some hospitals. They are located within or adjacent to an ED and consist of 4–6 rooms with the configurations previously mentioned. Governance is dictated by the local operational policies.
Consultation area
Consultation rooms are provided for the examination and treatment of ambulant patients who are not suffering a major or serious illness. These rooms have similar space requirements to acute treatment area bed spaces. In addition, they are equipped with office furniture with a computer terminal, a radiological viewing panel and a basin for hand washing. Consultation rooms may be adapted and equipped to serve specific functions, such as ENT or ophthalmology treatment, or as part of a fast track area to treat patients with non-complex single system diseases. When the fast track model of care is adopted, the provision of an adjacent subwaiting area for patients waiting for the results of investigations will promote the efficient use of the available floor space.
Plaster room
The plaster room allows for the application of splints, plaster of Paris and for the closed reduction of displaced fractures or dislocations and should be at least 20 m2 in size. Physiological equipment to monitor the patient undergoing procedural sedation or regional anaesthesia is required. Specific features of such a room include a storage area for plaster, splints and bandages; X-ray viewing panel/digital imaging systems facility; provision of oxygen and suction; a nitrous oxide delivery system; a trolley with plaster supplies and equipment; and a sink and drainer with a plaster trap. Ideally, a splint and crutch store should be directly accessible in the plaster room.
Procedure room
A procedure room(s) may be required to undertake procedures, such as lumbar puncture, tube thoracostomy, thoracocentesis, peritoneal lavage, bladder catheterization or suturing. It requires noise insulation and should be at least 20 m2 in size excluding a storage area for minor equipment and supporting sterile supplies. Physiological equipment to monitor the patient undergoing procedures, a ceiling mounted operating theatre light, X-ray viewing panel/digital imaging systems facility, provision of oxygen and suction, a nitrous oxide delivery system, a waste disposal unit and hand washing facilities should all be available.
Staff station
A single central staff area is recommended for staff servicing the different treatment areas, as this enables better communication between, and coordination of, staff members. The staff station in the acute treatment area should be the major staff area within the department. The staff area should be of an ‘arena’ or ‘semi-arena’ design, whereby the main areas of clinical activity are directly observable. The station may be raised in order to give uninterrupted vision of patients and should be centrally located. In larger departments, interlocking pods each involving a centrally located staff station overseeing an acute treatment area may be arranged to ensure patient visibility is maximized. The staff station should be constructed to ensure that confidential information can be conveyed without breach of privacy. Sliding windows and adjustable blinds may be used to modulate external stimuli and a separate write-up area may be considered. Sufficient space should be available to house an adequate number of telephones, computer terminals, printers and data outlets and X-ray viewing panels/digital imaging systems, dangerous drug/medication cupboards, emergency and patient call displays, under-desk duress alarm, valuables storage area, police blood alcohol sample safe, photocopier and stationery store, and write-up areas and workbenches. Direct telephone lines, bypassing the hospital switchboard, should be available to allow staff to receive admitting requests from outside medical practitioners or to participate in internal or external emergencies when the need arises. A dedicated line to the ambulance and police service is essential, as is the provision of a facsimile line. A pneumatic tube system for the transport of specimens to pathology, drugs from pharmacy and the transfer of medical records and imaging requests may also be located in this area.
Short-stay unit
Many EDs possess a short-stay unit, i.e. emergency medical unit (EMU) which is managed under its governance and operates as an extension of the department. The purpose of these units is to manage patients who would benefit from extended observation and treatment but have an expected length of stay of less than 24 hours. It is considered that the minimum functional unit size is eight beds. It is configured along similar lines to a hospital ward with its own staff station. The capacity is calculated to be 1 bed per 4000 attendances per year and its size will be influenced by its function and case mix. As short-stay units are usually high volume users of mental health, social work, physiotherapy, drug and alcohol and community support services, appropriate space should be allocated to allow these services to operate effectively.
Medical assessment and planning unit
A medical assessment and planning unit (MAPU) or medical assessment unit (MAU) is an inpatient hospital unit which may either be co-located or built near an ED. It is managed by the inpatient medical service. The purpose is to facilitate the assessment and treatment of patients who require intensive coordinated multidisciplinary team interventions to minimize the length of stay and optimize health outcomes. The expected length of stay of patients utilizing this type of unit tends to be less than 72 hours. Its configuration and function is determined by case mix and local operational policies. It is usually configured up to 30 beds along similar lines to a hospital ward.
Clinical support areas
The clean utility area requires sufficient space for the storage of clean and sterile supplies and procedural equipment and bench tops to prepare procedure trays. The dirty utility should have sufficient space to house a stainless steel bench top with sink and drainer, pan and bottle rack, bowl and basin rack, utensil washer, pan/bowl washer/sanitizer and slop hopper and storage space for testing equipment (such as for urinalysis). A separate store room may be used for the storage of equipment and disposable medical supplies. A common design fault is to underestimate the amount of storage space required for a modern department. A pharmacy/medication room may be used for the storage of medications and vaccines used by the department and should be accessible to all clinical areas. Entry should be secure with a self-closing door and the area should have sufficient space to house a refrigerator for the storage of heat-sensitive drugs and vaccines. Other design features should include spaces for a linen trolley, mobile radiology equipment, patient trolleys and wheelchairs. Beverage-making facilities for patients and relatives, a blanket-warming cupboard, disaster equipment store, a cleaners’ room and shower and toilet facilities also need to be accommodated. An interview room allows for the interviewing or counselling of patients, carers and relatives in private. It should be acoustically treated and removed from the main clinical area of the department. A distressed relatives’ room should be provided for the relatives of seriously ill or deceased patients. Consideration for the provision of two rooms should be given in larger departments to allow the separation of relatives of patients who have been protagonists in violent incidents or clashes. They should be acoustically insulated and have access to beverage-making facilities, a toilet and telephones. A single-room treatment area should be in close proximity to these rooms to enable relatives to be with dying patients and should be of a size appropriate to local cultural practices.
Non-clinical areas
Waiting area
The waiting area should provide sufficient space for waiting patients as well as relatives or carers and should be open and easily observed from the triage and reception areas. Seating should be comfortable and adequate space should be allowed for wheelchairs, prams, walking aids and patients being assisted. There should be an area where children may play and support facilities, such as television, should be available. Easy access from the waiting room to the triage and reception area, toilets and baby change rooms and light refreshment should be possible. Public telephones should be accessible and dedicated telephones with direct lines to taxi firms should be encouraged. The area should be monitored to safeguard security and patient well-being and it is desirable to have a separate waiting area for children. The waiting area should be at least 5 m2/1000 yearly attendances and should contain at least one seat per 1000 yearly attendances.
Reception/triage area
The department should be accessed by two separate entrances: one for ambulance patients and the other for ambulant patients. It is recommended that each contain a separate foyer that can be sealed by the remote activation of security doors. Access to treatment areas should also be restricted by the use of security doors. Both entrances should direct the patient flow towards the reception/triage area, which should have clear vision to the waiting room and the ambulance entrance. The triage area should have access to a vital signs monitor, computer terminal, hand basin, examination light, telephones, chairs and desk and patient weighing scales. There should be adequate storage space nearby for bandages, minor medical equipment and stationery.
Reception/clerical office
Staff at the reception counter receive patients arriving for treatment and direct them to the triage area. After triage assessment, patients or relatives will generally be directed back to the reception/clerical area, where clerical staff will conduct registration interviews, collate the medical record and print identification labels. Clerks may interview patients or relatives at the bedside but return to the reception area to finalize the administrative details. The counter should provide seating and be partitioned for privacy for interviews. There should be the ability for direct communication between the reception/triage area and the staff station in the acute treatment area to occur. The design should take due consideration for staff safety. This area should have access to an adequate number of telephones, computer terminals, printers, facsimile machines and the photocopier. It should also have sufficient storage space for stationery and medical records.
Tutorial room
This room provides facilities for formal undergraduate and postgraduate education and meetings. It should be in a quiet, non-clinical area near the staff room and offices. Provision should be made to accommodate webcasting, webconferencing, simulation and procedural skills training as well as local lectures and small group teaching. Technological support systems integrating computer, screen projection facilities, broadband access to capitalize on advances in web technology, electronic picture archiving and communication systems are essential. Equipment to support traditional teaching methods utilizing whiteboard, tube X-ray viewer system and examination couch must also be available.
Telemedicine area
Telemedicine is becoming increasing important, particularly for EDs in hospitals which are either remotely located or have limited access to subspecialty support. In these EDs, the telemedicine equipment may be located in the resuscitation area or in a dedicated room where patient encounters, such as mental health assessments, may be undertaken or the transmission of images, such as burns or digital X-rays, expedited. A dedicated facility with appropriate power and communications cabling is necessary. For facilities that receive the telemedicine transmissions, the room should be of a suitable size to allow simultaneous interactions by members of the consulting service teams. It should be in close proximity to the staff station.
Offices
Offices provide space for the administrative, managerial, quality improvement activities, teaching and research roles of the ED. The number of offices required will be determined by the number and type of staff. In a large department, offices may be needed for the director, deputy director, nurse manager, academic staff, specialists, registrars, nurse consultants/practitioners, nurse educator, secretary, social worker/mental health crisis worker, information support officer, research and projects officers and clerical supervisor. Larger departments will require the incorporation of a meeting room into the office area.
Staff facilities
A room should be provided within the department to allow staff a break and to relax from the intensity of their clinical work. Food and drink should be able to be prepared and stored and appropriate table and seating arrangements should be provided in bright and attractive surroundings. It should be located away from patient care areas and have access to natural lighting and appropriate floor and wall coverings. A staff change area with lockers, toilets and shower facilities should also be provided.
Likely developments over the next 5–10 years
Over the last 20 years, EDs have been facing significant challenges. There has been a never-ending increase in demand. The work environment has become increasingly pressured. This has been compounded by resource constraints and the introduction of electronic information management technology. The provision of care has been increasingly complex. Changes in technology have enabled the management of greater numbers of patients in the community who would previously have required hospitalization. As financial pressures on hospitals have also increased, the importance of the ED has grown considerably and modern departments have significantly expanded facilities. Future design considerations are likely to centre on advances in the areas of information technology, telecommunications and newer non-invasive diagnostic modalities. In addition to these technologically driven changes, a greater emphasis will be placed on developing ED design configurations which will support redefined service delivery models to maximize efficient work practices aimed to minimize the number of patient moves, to ensure patients receive timely definitive care and to allow time-critical interventions to be delivered. Computerized patient tracking systems using electronic tags and built-in sensors will provide additional information that may further improve operational efficiency. The electronic medical record will make detailed medical information immediately available and will greatly facilitate the provision of timely care, quality improvement and research activities. Digital radiography, personal communication devices, voice recognition systems, wireless technology and portable computers and expanded telemedicine facilities will make the ED of the future as reliant on electricity and cabling as it is on oxygen and suction.
The increasing age of the population needs also to be considered when designing an ED. Older patients have multiple co-morbidities leading to impaired mobility, vision and balance as well as being at increased risk of delirium due to underlying disease or hospitalization. They are likely to require greater space for the use of mobility aids and require greater shielding from sources of cognitive overstimulation than other patients. Standard hospital trolleys may pose a falls risk and contribute to the development of pressure areas. Strategies, such as the use of alternative hospital beds with pressure relieving mattresses and more comfortable ‘reclining lounge chair’ style seating, should be adopted for this subset of patients. Adequate lighting, the availability of natural lighting and the maintenance of a normal diurnal ‘night–day’ light pattern should be considered in the design to cater for the elderly patients who may spend prolonged periods of time in the emergency department.
27.3 Quality assurance/quality improvement
Diane King
Introduction
A primary role of the emergency department (ED) is to deliver the best possible care to all presenting patients. In order to deliver optimal care, a system of quality management must be part of the culture for all staff and be applied to all functions of the department. A quality framework provides the structure for the wide-ranging aspects of practice that are involved. Quality management requires effective leadership and commitment to improving processes and systems through analysis of data, change of processes and practice, staff engagement accountability and communication. Quality management is a continuous cycle, with measurement and monitoring required to establish that improvement is required in a practice or process, planning of the change, implementation, with re-evaluation and monitoring to ensure the change has the desired effect. Consumer involvement is a fundamental part of quality management. In the emergency setting, consumers include patients, families and carers, staff and the other clinical and hospital staff who interface with the ED.
History
The traditional approach of quality assurance involves a number of retrospective attempts to police various activities of the ED. The types of tools used in this approach are pathology result checking, missed fractures, medical record reviews, death audits and patient complaints.
The role of quality improvement in healthcare has evolved from the 1990s as it became evident that healthcare is prone to significant error and that, despite medical advances and escalating costs, the delivery of safe, acceptable and effective care is frequently lacking. Most industries adopted the quality improvement model to improve safety, reliability and efficiency. The implementation in the healthcare environment is noteworthy for the complexity of its systems, difficulty measuring clinical outcomes and competing priorities [1]. A modern quality system provides a framework that includes monitoring, audit and improvement of the clinical aspects of care, processes and structure, competence of staff, including education and training, and has clear governance and accountability [2].
Definitions
 Quality–‘doing those things necessary to meet the needs and reasonable expectations of those we service and doing those things right every time’ [3].
Quality–‘doing those things necessary to meet the needs and reasonable expectations of those we service and doing those things right every time’ [3].
 Quality assurance (QA)–‘a system used to establish standards for patient care, to monitor how well standards of care are met, and to correct unwarranted deviations from the standards’ [4]. This implies intervention to correct deficiencies and is often externally driven.
Quality assurance (QA)–‘a system used to establish standards for patient care, to monitor how well standards of care are met, and to correct unwarranted deviations from the standards’ [4]. This implies intervention to correct deficiencies and is often externally driven.
 Quality improvement (QI)–raising quality performance to ever increasing levels.
Quality improvement (QI)–raising quality performance to ever increasing levels.
Continuous quality improvement
The Deming cycle (described by WE Deming) is a fundamental tool for the approach to quality in any system. The PDSA (plan, do, study, act) cycle should incorporate the important sequential steps of planning, staff engagement, implementation, measurement, re-measurement and re-evaluation, followed by an improved plan and so on.
A QI system covers a number of dimensions. These are variously described, but include:
 access and equity, e.g. waiting times and access to inpatient beds
access and equity, e.g. waiting times and access to inpatient beds
 acceptability or patient centredness, e.g. complaint rates, patient satisfaction surveys
acceptability or patient centredness, e.g. complaint rates, patient satisfaction surveys
 efficiency: cost-effectiveness and value, e.g. appropriate imaging, avoiding waste.
efficiency: cost-effectiveness and value, e.g. appropriate imaging, avoiding waste.
There are a number of vital characteristics of a CQI programme that are necessary for its successful operation. A CQI programme:
 requires leadership (management) commitment and strategic planning
requires leadership (management) commitment and strategic planning
 focuses around clear governance structures and accountability
focuses around clear governance structures and accountability
A more detailed outline of TQM is beyond the scope of this book, however, the recent literature abounds with discussion on the various tools used, pitfalls in introduction and so on [5–8].
National bodies
The quality agenda has been facilitated by various bodies, including The Australian Council on Healthcare Standards (ACHS), that, in 1997, introduced its Evaluation and Quality Improvement Programme (EQuIP) as a framework for hospitals to establish quality processes. This is a requirement for accreditation with the ACHS. In 2006, the Australian Commission for Safety and Quality of Health Care was established to oversee improvements in the Australian context (previously the Australian Council for Safety and Quality). In the USA, the Joint Commission on Accreditation of Healthcare Organizations (JCAHO) and the Institute for Healthcare Improvement have led the way in the move from QA to QI [9,10].
The Australasian College for Emergency Medicine, the American College of Emergency Physicians and the UK College of Emergency Medicine are facilitating the process of QI by their training role, introduction of clinical indicators, policy development and standards for EDs. In addition, the International Federation for Emergency Medicine (IFEM) has developed a consensus document outlining a framework for measuring quality in 2012 available on the IFEM website.
Quality in the ED
The ED is a complex environment, which involves close interaction with the rest of the hospital and the community. The inputs are uncontrollable and unregulated and the ‘customers’ are under a high level of stress because of the nature of their problems, the unfamiliarity of the environment and the lack of control they perceive at a time when they are feeling personally vulnerable.
The ED is dealing simultaneously with life-threatening illness and minor complaints. It is an area under a high level of scrutiny from all quarters: the patients, the families and friends, the other departments in the hospital and the wider community–both medical and non-medical. This in itself is error prone and is compounded by the fact that many of the staff working in the ED are rotating through the department for relatively short periods of time, are often relatively junior and are undergoing training themselves. This training role is of critical importance in most EDs and must not be forgotten in any process dealing with quality issues. All these aspects of an ED make the maintenance of quality difficult and all the more imperative. In order to establish a system where quality care can be delivered with any degree of reliability, it is important that all staff are committed to the process and that management provides appropriate leadership and resources. The delivery of quality involves a continuing process of data collection (performance measures), analysis, feedback and introduction of strategies to improve the system, followed by re-analysis of the performance measures (the quality cycle).
Common quality measures in ED
The following are not exhaustive but are commonly used measures:
 time to thrombolysis or percutaneous coronary intervention (PCI)
time to thrombolysis or percutaneous coronary intervention (PCI)
 waiting time by triage category
waiting time by triage category
 death audits–and morbidity or adverse event reviews
death audits–and morbidity or adverse event reviews
 flow measures: 4 hour total ED times, times to inpatient bed
flow measures: 4 hour total ED times, times to inpatient bed
 chart audits for specific complaints, e.g. management of headache, abdominal pain, etc.
chart audits for specific complaints, e.g. management of headache, abdominal pain, etc.
 time to analgesia: generally and for specific conditions, such as abdominal pain or fractures
time to analgesia: generally and for specific conditions, such as abdominal pain or fractures
 time to antibiotic for sentinel diagnoses, such as febrile neutropaenia or pneumonia
time to antibiotic for sentinel diagnoses, such as febrile neutropaenia or pneumonia
 trauma audits–missed cervical fractures, delay in craniotomy
trauma audits–missed cervical fractures, delay in craniotomy
 X-ray and pathology report follow up
X-ray and pathology report follow up
 equipment functioning and supply
equipment functioning and supply
 safety of the working environment including, for example, electrical safety or violent incidents
safety of the working environment including, for example, electrical safety or violent incidents
It is clear from the list that the measures are potentially innumerable, that local factors must dictate those areas of special interest and that this will vary from hospital to hospital. In deciding which areas should be measured, it is important to focus on areas critical for patient or staff safety, that are strategically aligned or have been targeted as requiring improvements with which staff engage.
All EDs have common areas where there is high potential for problems to develop and these areas should be routinely monitored. The mechanism for doing this will vary from institution to institution.
Another aspect of the measuring of performance is that the process is one in evolution.
Not only should the quality of the service improve as the measures are improved and re-assessed, but the areas for attention can change and develop with the whole system. Peeling off layers as problems are addressed, exposes new things to improve. Again, this process must be internally driven to be effective. There is little point in collecting an enormous amount of data, unless the process is useful to the improved functioning of the whole system. Those best able to make those improvements should be an integral part of the system.
Likely developments over the next 5–10 years
27.4 Business planning
Richard H Ashby
Introduction
Emergency departments (EDs) in public sector health services in Australasia are typically mid-sized clinical units within the organizational structures of hospitals. Staff numbers may range from 30 to over 200 and expenditure budgets from $3 m to over $30 m per annum. ED efficiency directly affects the global efficiency of the healthcare process in the hospital and purchasers are therefore increasingly interested in the value and performance of emergency medicine services. ED managers are being required to report on the dimensions of cost, output, quality and efficiency through a business planning process and other reporting mechanisms in order to justify their level of resourcing.
Types of plans
ED plans are relatively low in the hierarchy of planning instruments that begin with national and state health policy, health departments’ strategic and corporate plans, regional and hospital strategic and business plans and, finally, the business and project plans of individual clinical units and departments. Strategic plans describe how organizations propose to respond to changing technology, altered demographics, shifting paradigms of care and industrial and regulatory reform, as well as issues associated with the cost, quality and accessibility of healthcare. These plans typically look 5–10 years into the future and the ED should reasonably expect to have input at a variety of levels into the strategic planning process.
Project plans, on the other hand, are highly focused on a particular objective outcome to be achieved within a given time frame and with a specified level of resources. Project plans may need to be created by an ED for the implementation of a new and significant piece of technology, major refurbishment or redevelopment or some types of clinical process redesign. However, the most important planning instrument for an ED is its annual business plan.
The business plan
The business plan is an important multipurpose document that needs to be developed by the ED management group, in consultation with hospital management, on an annual basis. At one level, the business plan represents a management contract between the executive of the hospital and the ED. At another level, the business plan provides information to the staff of the department about the agreed targets for revenue and expenditure, activity, efficiency and quality of services to be provided in the next financial year.
Planning process
The plan should be developed by the medical director, business manager and nurse manager of the ED informed by consultation with the wider staff group. It is often useful to include a representative from the hospital’s financial services department early in the process, so that there is a clear understanding of the financial framework for the plan. It is vitally important that the process be informed with as many useful data as possible, including accurate and up-to-date financial and activity statistics and quality and efficiency indicators. The premises, or context, of the business plan needs to be established. Unless there are specific reasons for change, it can usually be assumed that hospital managers will require that the business plan be based on management of the same level of activity at a similar quality to the previous year. In some years, there may be a requirement for a productivity dividend where management expects the same output from a reduced budget or improved performance from the same budget. Other assumptions, relating to estimated wages growth, non-labour cost escalations, leave requirements and so on, should be stated.
The timing of business plan development depends on the government budget cycle for public sector EDs and the timing of the financial year for private sector EDs. In most jurisdictions, this process needs to commence in early January, with the draft business plan available for the hospital executive by the end of February. The process may need to begin much earlier if significant additional or special funding is being sought. Such requests are best handled as separate submissions, which will then need to pass through the various evaluation and approval steps. It is uncommon for special projects requiring substantial funds to be approved and funded within one budget cycle.
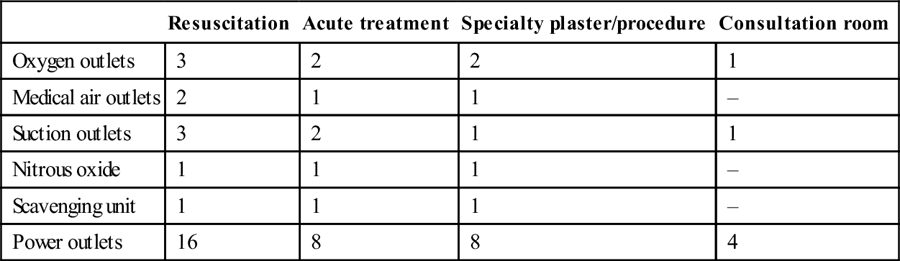
A typical business planning cycle is illustrated in Figure 27.4.1.
Business plan content
The ED business plan must address, as a minimum, each of the dimensions of performance, that is, revenue, expenditure, activity, quality and efficiency. A typical index is illustrated in Table 27.4.1. Some hospitals may require that their own format be used.
Table 27.4.1
| 1.0 | Introduction |
| Mission, role, objectives | |
| 2.0 | Executive summary |
| 3.0 | Projected outcomes 2012/2013 |
| 3.1 | Budget–revenue and expenditure |
| 3.2 | Budget variance analysis |
| 3.3 | Staffing profile |
| 3.4 | Activity |
| 3.5 | Quality and efficiency key performance indicators |
| Efficiency indicators | |
| Clinical indicators | |
| Consumer indicators | |
| 4.0 | Budget estimates 2013/2014 |
| 5.0 | SPECIAL ISSUES 2013/2014 |
| Equipment–clinical and non-clinical | |
| <$5000 | |
| >$5000 | |
| Facility maintenance | |
| Projects | |
| Information system replacement | |
| Short-stay unit expansion | |
| Head-injury research |
The introduction to the business plan should be brief. It is often useful to re-state the role and objectives of the ED and of any of its subunits. The executive summary should present an overview of the business plan, including a general perspective on the integrity of the budget and activity targets for the current year and outlining any premises used in the creation of the current plan. Special issues may be highlighted.
Budget
The projected financial outcomes for the current financial year should have been carefully estimated. This projected end-of-year position should be shown in a tabular format against the agreed targets from the previous year’s business plan, as well as the actual outcomes of the previous year. In government organizations, adherence to budget is the highest priority and, therefore, the budget details should be presented first. The management group should have a detailed understanding of every variance from the budget that has occurred in the current year and a note of explanation of variance on every line item should be provided. Because the high fixed costs associated with operating an ED are related to the labour intensity of the service, it is useful to include a section tracking paid full-time equivalent staff, by month, for the current year compared to the previous financial year. This is especially important if there has been an overrun in the labour budget, as the hospital executive will wish to be reassured that this is not due to the employment of excess staff or excessive overtime.
In some jurisdictions, hospitals are funded based on activity, including ED activity, and it is incumbent on the ED to gather accurately and completely all necessary information to optimize this revenue. Similarly, privately insured patients must be identified as well as individuals for whom special funding or revenue premiums apply. Such expectations should be discussed with the finance department.
Activity
The activity of the ED may be shown as total attendances and attendances by category of the Australasian Triage Scale. The admission rate by triage category should also be shown and all values should be tabulated against the previous year’s activity levels. Where an ED operates a short-stay ward or observation unit, the top 20 diagnosis-related groups by volume should be shown, together with the number of total separations, weighted separations and the case-mix index. This information should be available from the finance department. Again, the data should be benchmarked to the previous year. Additional relevant activity data, such as inter-hospital transfers, retrievals and so on, should be included.
Quality and efficiency
Waiting time by triage category is the key quality and efficiency indicator for an ED. The average waiting time per patient in each triage category should be shown, together with the percentage of patients in each triage category who are seen within the timeframe specified by the Australasian Triage Scale. In addition, the percentage of all ED patients seen and admitted, discharged or transferred within 4 hours (Australia-National Emergency Access Target) must be reported against target. These data should be benchmarked against the previous year’s performance and, ideally, also against benchmarking data from similar hospitals elsewhere. Performance against clinical indicators recommended or required by government and other central agencies should also be reported. Additional access indicators include the frequency and duration of ambulance bypass, patient off-stretcher time and admission access block (percentage of total admitted patients spending longer than 8 hours in the ED) should be provided. EDs need to have a complete understanding of the Key Performance Indicators (KPIs) that are applicable to their services and have clear plans to achieve these. Dashboard displays of KPI achievement should be regularly published to both managers and staff.
It is appropriate in the section on ‘quality’ that research and educational achievements and plans should be succinctly reported, together with any innovative projects.
Projections
Having summarized the current year’s performance, the remainder of the business plan should be used to present the ED’s projections and estimates for the next financial year. Again, the projected budget should be presented first. This is best done in a tabular format and compared to the previous year’s budget and projected actual expenditure. Any premises, assumptions or caveats related to the projected budget should be included as footnotes to the table. The most common premise relates to the volume and quality of services to be provided and the usual approach is iso-volume/iso-quality; this should not be varied in the business plan unless previously agreed by the hospital executive. Periodically, circumstances will dictate that a hospital vary the desired quality of services, perhaps as part of a strategic initiative to develop the ED or the volume of services in response to changing demographic projections. Apart from anticipated wages growth, it is important for the management group to make reasonable enquiries about predictable leave (such as sabbaticals or long-service leave) and these should be appropriately costed. In the non-labour budget, possible variations in the cost of overseas-sourced clinical supplies or pharmaceuticals due to revaluation of the currency should be considered although, in some jurisdictions, non-labour increments are specified, for budget purposes, across the whole of government. Particular attention should be paid to high-cost areas of pathology, radiology and pharmacy with evidence-based utilization being regularly assessed.
Realistically, most hospital executives will reject a budget proposal that exceeds the previous year’s expenditure, escalated by projected wages growth, unless there are special mitigating factors or a source of funds for the predicted additional expenditure has been identified. For this reason, it is often useful to have three additional sections in the business plan addressing equipment needs, facility maintenance needs and a projects summary.
Equipment
The ED management group should canvass widely among the staff about perceived equipment needs. It is important that the totality of clinical and non-clinical equipment needs is understood and equitably prioritized in order to optimize the efficiency of the whole department. Most hospitals require that equipment requests be stratified according to cost, with items less than $5000 typically being met from a global allocation to the department. Apart from tabulating the need for this lower-priced equipment, a few lines of narrative about each item often assists the executive in ensuring the reasonableness of the request. The table should indicate whether the equipment is new or replacement. New high-cost equipment (e.g. ultrasound machines, computed tomography scanners or arterial blood gas machines) or large-scale renovations or new builds usually require the presentation of a full business case in line with government procurement instructions. The replacement of old, high-cost equipment should be part of a pre-planned hospital programme.
Facility maintenance
All but the newest departments will require some expenditure on maintenance each year. Again, it is useful for the ED management group to undertake a focused tour of all areas of the department to establish an inventory of maintenance needs. Reasonably accurate costings can be obtained from hospital engineering services or external contractors.
Projects
This final section can be used to describe and cost small or large projects to enhance the ED facilities, infrastructure or services. For example, there may be a proposal to establish a 10-bed short-stay unit adjacent to the ED, involving facility redevelopment, the acquisition of clinical and non-clinical equipment (including information systems), staff resourcing and clinical process redesign. This is best presented in a project format, including a clear description of the business need (supported by all available, relevant data), a business case outlining all the costs and benefits and, if possible, additional material, such as architects’ sketches and a project implementation plan, including a project timetable. Professional advice in preparing this documentation is essential.
Private EDs
The overview of business planning presented above is equally relevant to EDs in private hospitals. However, private EDs also need to develop a more robust revenue budget and marketing plan appropriate to their circumstances. The marketing plan will usually be a part of the hospital’s overall arrangements, but the ED should be in a position to report on any changes in referral pattern or on any opportunities to expand the business.
Business plan implementation and monitoring
Soon after the hospital receives its global budget, activity targets and KPIs from government, a short process of negotiation between the hospital executive and the ED management group should take place. This will fine-tune the business plan and, ultimately, permit authorization of the plan and the appropriate delegation for its implementation.
The ED management group should meet at least monthly to review actual performance against the outcomes predicted by the plan. Any variance from the budget in particular should be studied and understood. Remedial action should be taken wherever possible to maintain budget integrity. In many places, the ED management group would meet with the hospital executive at least quarterly to review department performance and to deal with any variation that may have occurred.
27.5 Accreditation, specialist training and recognition in Australasia
James Collier and Allen Yuen
Specialist recognition and registration
Specialist recognition in New Zealand and Australia is handled by the respective medical councils in each country–the Medical Council of New Zealand (MCNZ) and the Australian Medical Council (AMC). In New Zealand, MCNZ handles both specialist recognition (termed vocational registration) and general medical registration. In Australia, the AMC has responsibility for the assessment of International Medical Graduates (IMG) seeking registration to practise medicine in Australia, including specialist recognition of overseas-trained specialists (OTS) and the accreditation of specialist medical colleges. Medical registration (both general and specialist where applicable) is the responsibility of the Medical Board of Australia, which is supported in this role by the Australian Health Practitioner Regulation Agency (AHPRA). Medical registration is required to undertake specialist training. All IMG must be both recognized by the AMC and registered with the Medical Board of Australia. There are three pathways to registration that are available to IMG: Competent Authority Pathway, Specialist Pathway and the Standard Pathway.
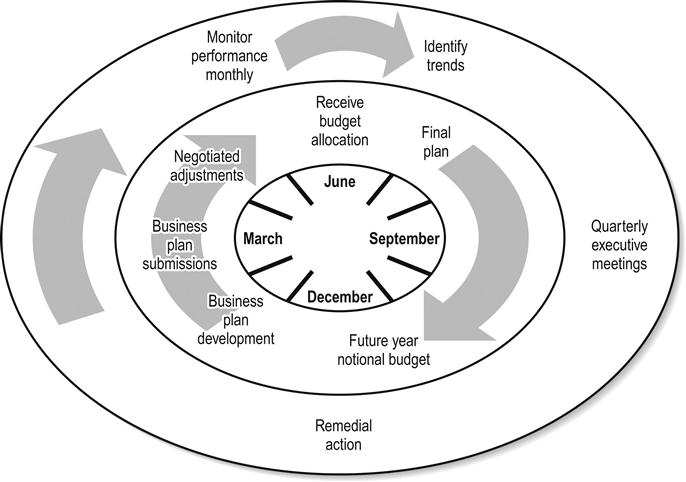
Specialist training in emergency medicine
Specialist medical training is the responsibility of the various specialist medical colleges. Most of these organizations cover both Australia and New Zealand. They are accredited by the AMC. Specialist training in emergency medicine (EM) is covered by the ACEM.
The college provides the framework, standards and supervision for specialist training in EM and successful trainees are granted Fellowship of the ACEM (FACEM).
Training occurs in hospitals and rotations approved by the ACEM for training. Each accredited emergency department (ED) is required to have an appointed Director of Emergency Medicine Training (DEMT). This is the college Fellow with the responsibility of facilitating the delivery of the training programme in that department and hospital. The description below of the training programme reflects the situation in November 2012 [1]. The training programme undergoes regular review and revision.
Basic training
This usually consists of the pre-registration year of practice (internship in Australia or postgraduate year 1 [PGY 1] in New Zealand) and the second year of practice following a doctor’s primary medical degree. It must occur in a variety of clinical rotations and be signed off by the administration of the employing institution.
Provisional training
This usually occurs in the third postgraduate year or beyond. There are three requirements of provisional training:
Advanced training
Advanced training occurs once the trainee has completed all the requirements of provisional training. The ACEM has a detailed curriculum outlining the knowledge and skills required by the completion of advanced training. The main elements are ED training, non-ED training, the minimum paediatric requirement, a research component and completion of the fellowship examination.
ED training
Trainees must complete 30 months of training in accredited EDs. Each accredited ED is allowed to provide training for an individual trainee up to a specified maximum amount of time (6, 12 or 24 months). Training must be in a minimum of 3-month terms. Each term is assessed and signed-off at its completion by the DEMT. As per provisional training, trainee feedback is required at the conclusion of each term.
Hospitals are also assigned a role delineation (major referral, urban district, rural/regional) when they are inspected for training accreditation. Trainees must complete at least 6 months in a major referral hospital and either an urban district or rural/regional hospital.
Non-ED training
Trainees must complete 18 months of training in approved non-ED rotations. These are usually in hospitals accredited for training by the respective college for that specialty. It is required that at least 6 months be spent in critical-care rotations (anaesthesia and/or intensive care). Experience can also be gained in the ACEM accredited special skills terms, such as pre-hospital and retrieval, trauma, toxicology, rural/remote health, ultrasound, research, medical education, simulation, safety and quality and medical administration.
Minimum paediatric requirement
This can be gained by two pathways: completion of a 6-month term in an accredited paediatric emergency department or via completion of a paediatric logbook. With respect to the logbook, this can be utilized during ED and non-ED advanced training involving paediatric (aged 15 years and under) patients. Trainees must log at least 400 substantive encounters with paediatric patients, of which 200 must occur within an ED setting and 100 of these must be from Australasian Triage Scale categories 1, 2 or 3. EDs are given specific accreditation for the use of a paediatric logbook.
Research component
The mandatory learning objectives of the research requirement of training can be met by publishing or presenting a research project to the satisfaction of the ACEM Trainee Research Committee or by successful completion of a minimum of two approved postgraduate subjects from the same course at an Australasian Univeristy.
Fellowship examination
Trainees may attempt the fellowship examination when they are within 1 year of completion of their training. The examination consists of three written sections (multiple choice, short-answer questions and visual aid questions) and three clinical sections (long case, short cases and structured clinical examination). It is run twice a year in various locations across Australia and New Zealand.
Variations to training
Recognition of prior learning can be applied for in line with regulations and upon registration. Up to 2 years of advanced training (up to 1 year of which can be in EM) can be gained overseas, with the prior approval of the ACEM.
Training can also be completed on a part-time basis (at least 50% of the time and conditions of a full-time post) and can be suspended for up to 2 years. All requirements of the training programme must be completed within 12 years of commencement of provisional training.
Dual training
Dual training programmes in paediatric EM (in conjunction with the Royal Australasian College of Physicians) and intensive care medicine (in conjunction with the College of Intensive Care Medicine) are operational.
Recognition of specialist training obtained outside of the ACEM
OTS in EM must apply for specialist recognition from either AMC or MCNZ. In both cases, once the documentation and English language status have been confirmed, the OTS is referred to the ACEM for assessment. The ACEM reviews the applicant’s training, qualifications and experience on paper. If these appear potentially substantially comparable, the ACEM conducts a structured interview for further clarification. The three senior FACEMs on the interview panel review the applicant’s qualifications and experience and determine their level of confidence in the following areas: undergraduate training, basic training, advanced training, postgraduate experience, research and publication profile, education and training experience and administration. Additionally, three topical issues are discussed.
The ACEM then makes a recommendation to the AMC or MCNZ for specialist recognition, further supervision or further training.
The ACEM has a comprehensive website (http://www.acem.org.au) that provides up-to-date information on all aspects of training and other college matters. The AMC (http://www.amc.org.au) and MCNZ (http://www.mcnz.org.nz) also have websites with useful information for overseas-trained doctors wishing to work in either country.
Accreditation
Hospitals seeking accreditation for defined purposes, such as service provision or training, must comply with set standards determined by external institutions which oversee the criteria applicable to such hospitals.
In the case of hospitals overall, the Australian Council on Healthcare Standards (ACHS) determines the service standards of patient care provided by a hospital and its individual departments [2]. The ACHS has included the 10 National Safety and Quality Health Service Standards within its framework and integrated these with standards concerning service delivery, provision of care, workforce planning and management, information management and corporate systems and safety.
The learned colleges, including the ACEM, separately accredit hospitals for their ability to provide postgraduate training, taking the above criteria into account, but placing greater emphasis on the quality of experience, education and supervision for trainees. The items that the ACEM considers and takes into account in any accreditation decision are outlined in the following list from the ACEM guidelines [3]:
 Compliance with the ACEM Continuing Professional Development Programme by the FACEM staff.
Compliance with the ACEM Continuing Professional Development Programme by the FACEM staff.
 Appropriate levels of staffing with respect to medical, nursing, secretarial and other personnel.
Appropriate levels of staffing with respect to medical, nursing, secretarial and other personnel.
 Design and equipment of the department appropriate to the provision of emergency care and training.
Design and equipment of the department appropriate to the provision of emergency care and training.
 An appropriate range and level of support services.
An appropriate range and level of support services.
 The opportunity for trainee research and the infrastructure supporting this.
The opportunity for trainee research and the infrastructure supporting this.
 The ACEM Statement document–Emergency Department Role Delineation.
The ACEM Statement document–Emergency Department Role Delineation.
Accreditation guidelines
Transparent comprehensive ACEM guidelines for mixed and adult EDs seeking training accreditation can be viewed on the ACEM website [3].
The minimum threshold criteria that must be met before an ED can be considered for ACEM training accreditation is 2.5 full time equivalent (FTE) total FACEMs inclusive of the Director and DEMT [3]. The rationale for the minimum threshold relates to the minimum number of specialists required to provide a combination of leadership, mentorship, off-floor training, feedback and assessment and on-floor clinical supervision and feedback.
In addition to this minimum threshold, departments must meet mandatory criteria as outlined below before any level of accreditation can be considered [3]:
 appropriate and acceptable standards of patient care
appropriate and acceptable standards of patient care
 documented management, admission, discharge and referral policies
documented management, admission, discharge and referral policies
 a functional electronic patient information management system
a functional electronic patient information management system
 a formal system of quality management; trainees are expected to participate in these activities
a formal system of quality management; trainees are expected to participate in these activities
 a formal orientation programme for new staff
a formal orientation programme for new staff
 educational programmes for all grades of medical and nursing staff
educational programmes for all grades of medical and nursing staff
 access to advice or information which facilitates trainees seeking mentorship if they wish to do so.
access to advice or information which facilitates trainees seeking mentorship if they wish to do so.
College procedure
The ACEM conducts regular (at least 5-yearly) inspections of ACEM training-accredited EDs, to ensure that standards are maintained and that the various criteria for accreditation are met [4,5,6].
In the intervening period, the Accreditation Committee conducts annual reviews of a department’s aggregated Trainee Feedback Reports. Identified issues require clarification, explanation or resolution by departments.
With respect to an accreditation inspection, the completed hospital information questionnaire, ED criteria checklist and any accompanying documents supplied to the inspection team before the inspection are carefully studied. Interviews with administration, department heads, specialists, trainees, nurse managers and educators contribute significantly to the decisions made.
The ED criteria checklist is a checklist against the minimum threshold, mandatory criteria and a number of specific criteria per level of accreditation currently held or desired in the future. An example of these specific criteria for a 24-month department is illustrated below [3]:
With respect to the level of supervision of trainees, the ED requires:
 Director(s) of Emergency Medicine Training (DEMT). The DEMT will be a FACEM who is required to be employed at a minimum of 0.5 FTE and undertake clinical work within the emergency department. The DEMT should be at least 3 years post-fellowship (within a Co-DEMT model, this is mandatory for at least one of the DEMT). With reference to provisional and advanced trainees within an emergency department roster, the following should be approximated with respect to the amount of clinical support time required within an emergency department for DEMT duties:
Director(s) of Emergency Medicine Training (DEMT). The DEMT will be a FACEM who is required to be employed at a minimum of 0.5 FTE and undertake clinical work within the emergency department. The DEMT should be at least 3 years post-fellowship (within a Co-DEMT model, this is mandatory for at least one of the DEMT). With reference to provisional and advanced trainees within an emergency department roster, the following should be approximated with respect to the amount of clinical support time required within an emergency department for DEMT duties:
 1 hour DEMT clinical support time/trainee/week.
1 hour DEMT clinical support time/trainee/week.
 The presence of a FACEM exclusively rostered to clinical duties for at least 98 hours of every week.
The presence of a FACEM exclusively rostered to clinical duties for at least 98 hours of every week.
 A minimum of 60% of trainee time to be under the direct clinical supervision of a FACEM.
A minimum of 60% of trainee time to be under the direct clinical supervision of a FACEM.
With respect to the structure of the training programme, the ED requires:
These specific criteria are repeated for 6- and 12-month accreditation but the numbers or threshold for each criterion are devised such as to be appropriate to these lower levels of accreditation [3].
Prior to the inspection, the department does a self-assessment on the relevant ED criteria checklist and indicates which criteria it meets, partially meets or does not meet. At the end of an inspection, the inspection team revisits the checklist and performs its own criteria assessment. Any variance between the department’s assessment and the inspectors’ assessment can then be discussed to clarify items of confusion, error or misunderstanding.
Levels of accreditation
There are three levels of accreditation awarded: 6 months, 12 months or 2 years. These periods refer to the amount of accredited time recognized as a part of a trainee’s advanced EM training in that particular ED. The trainee may spend more time in the department, but the extra time will not count towards training requirements. The trainee may spend more time within the same hospital accruing non-ED time in accredited rotations in other specialties relevant to EM.
Since the period of advanced training is 4 years, the above periods of accreditation ensure that trainees rotate through at least two hospitals, benefiting from the particular strengths of each.
Rationale for the accreditation criteria
The Accreditation Committee has discretion on how the criteria are applied. This is for a number of reasons. First, the criteria are not comprehensive and factors not listed in the criteria may weigh positively or negatively on the outcome. Not all criteria necessarily need to be met as great strengths in some criteria may outweigh concerns of not meeting another; however, criteria concerning education, supervision and trainee welfare are a priority. Any criteria that are clearly not met are at least fed back as an issue.
The rationales for the mandatory criteria are fairly self-explanatory. Standards required for acceptable patient care and well-being of staff are paramount. The ACEM would not wish to put a trainee at risk in an environment where this was jeopardized.
Access to a mentoring system is also mandatory and is an AMC requirement of colleges. Trainees need to have the opportunity to seek a mentor, although it is not an obligation of the department to have a mentor for each trainee. Some departments run a supervisor system to aid the DEMT but, as supervisors participate in assessment, these are different from mentor systems.
With regard to specific criteria per level of accreditation, adequate senior staffing with emergency physicians is essential. Trainees must be well supervised, particularly after-hours and during busy evening and weekend periods. As the level of accreditation increases FACEM minimum numbers and the overlap of FACEMs working directly on the floor with trainees increases also. The number of FACEM FTE required increases from 2.5 to 5 to 8, the hours of the week of FACEM clinical presence increases from 50 hours to 80 hours to 98 hours, and the minimum percentage of trainee time under the direct supervision of a FACEM increases from 30% to 40% to 60%; respectively per 6-, 12- and 24-month level of accreditation criteria.
At the same time, trainees need to be given increasing levels of responsibility, including administrative, as they advance in their training, as some may be appointed to director positions at smaller hospitals soon after attaining their specialist qualification [6,7].
Excellent leadership is a requirement for a well-functioning department and training environment, hence the FACEM Director requirement and, as clinical leadership in the ED goes hand in hand with nursing leadership, the nurse unit manager requirement. The ability to utilize a Co-DEM management structure provides larger departments the ability to share an increasing administrative workload and smaller, in particular regional rural departments, the flexibility to use fractional appointees within the role.
Educators are of course an absolute requirement and medical and nursing education should be closely linked. Nurses can be a great source of trainee education and trainees can gain experience by participating in nurse education. Inspectors take note of the interaction between medical and nursing staff education and it becomes easily apparent whether these are well-integrated or separate entities.
The use of a Co-DEMT model is widespread as departments strive to meet the needs of an increasing number of trainees. The use of a DEMT to trainee ratio to determine the clinical support time for DEMT duties within a department applies equally across all levels of accreditation to the benefit of trainees.
Education programmes, particularly for 24-month accredited departments, must show the full spectrum of education. These should include on-floor clinical teaching; fellowship exam-specific programmes; primary exam-specific programmes; and departmental general education sessions. These programmes may be shared between a network of hospitals (ACEM accredited Emergency Medicine Training Network) and trainees must be provided with protected teaching time to allow them to attend education sessions. The culture for education and training can also be demonstrated by the quality and standard of resident and undergraduate education programmes, as well as FACEM university academic appointments. It is expected that the registrars, as advanced trainees, will be involved in student and resident teaching. Access to simulation training is becoming more widespread and available. FACEM commitment to assisting in college exam processes is a requirement for higher levels of accreditation and, again, is a marker of enthusiasm and educational culture.
The ability of a hospital to provide rotations for EM trainees to terms such as medicine, surgery, cardiology, anaesthesia, intensive care, paediatrics and psychiatry enhances a hospital’s chances of attaining accreditation.
Research and quality assurance projects provide a framework for improving performance and the College examines the department’s commitment to research [8]. Smaller 6-month departments may not have significant research infrastructure, but 24-month accredited departments must have at least an individual or a few individuals to assist trainees in their research component.
Case mix and attendance can, of course, ultimately limit or maximize a training experience and this also varies in stipulation per level of accreditation.
Recommendations
Following an accreditation inspection, a detailed report is forwarded to the College’s Accreditation Committee for discussion.
Recommendations are then made regarding level of accreditation, suitability for paediatric logbook status, the number of trainee positions the particular ED can sustain and the role delineation of the hospital. Identified issues are also listed and it is expected the hospital will address these over the course of the next accreditation cycle, with regional Accreditation Committee members reviewing progress annually. Significant concerns require written correspondence to the Chair of Accreditation describing satisfactory resolution of issues. If standards for the level of existing accreditation are not met, departments receive 12-months’ notice that the accreditation status may be reduced to a lower level. A further inspection in 12-months’ time is conducted to determine the outcome. If any hospital at inspection fails to meet the minimum threshold criteria, accreditation is immediately lost without any notice period. The ACEM Board of Education and Council ratify accreditation decisions made by the Committee.
Implications
The accreditation process is comprehensive, fair and important, but it can also be intimidating [9]. Hospitals will retain their accreditation as long as they maintain the desired standards. Inspections by the College can highlight a department’s or hospital’s shortcomings to administrators, so that attention can be paid to correcting the deficiencies.
There has historically been little disagreement from EDs and hospitals with the recommendations made.
Loss of accreditation can occur at any time if departments fall below the minimum threshold. Losing accreditation can have adverse long-term consequences in terms of loss of reputation and lack of good applicants for positions in these departments.
In order to protect the trainees at an institution that loses accreditation, or has a reduction in accreditation status, trainees are allowed to continue having training accredited up to the end point of the current employment contract or change in training year [4].
Success with accreditation ensures a continuation or upgrading of an ED’s reputation and makes that hospital more attractive for prospective trainees and staff specialists. Hospitals therefore have strong incentives to maintain high standards in their EDs.
Accreditation of paediatric-only departments
Accreditation guidelines for paediatric-only departments were jointly developed by the ACEM and the RACP (Royal Australian College of Physicians) through the Joint Training Committee in Paediatric EM. They follow a very similar format and structure to the adult and mixed guidelines but have a paediatric-specific theme.
Accreditation of overseas rotations
ACEM regulations are relatively flexible and trainees are encouraged to work in a variety of hospitals, both in Australia and New Zealand as well as overseas. Overseas terms are preferably in centres with respective college specialist training accreditation and prior approval needs to be sought from the ACEM. So far, most of these overseas accredited terms have been in the UK [10,11].
Accreditation in the future
The Australian Health Ministers’ Advisory Council and the Health Workforce Principal Committee is conducting the Accreditation of Specialist Medical Training Sites Project. In consultation with the learned colleges and jurisdictions, the project is considering opportunities to streamline, improve efficiency and eliminate duplication in regard to accreditation practices across all colleges and disciplines. To date the proposed deliverables of the project are as follows:
 develop overarching accreditation principles
develop overarching accreditation principles
 develop a generic demographic dataset
develop a generic demographic dataset
 develop generic standards with craft specific criteria
develop generic standards with craft specific criteria
 explore the use of other modalities, apart from site visits, in the accreditation process
explore the use of other modalities, apart from site visits, in the accreditation process
 explore the feasibility of an ongoing quality assurance process
explore the feasibility of an ongoing quality assurance process
The criteria that are utilized to determine the role delineation of a hospital are being reviewed within the College and are likely to transition to describe the role delineation of EDs as opposed to hospitals.
In line with these initiatives and the ACEM Curriculum Revision Project (CRP), the ACEM accreditation guidelines are under review. Rising ED attendances, increasing staffing numbers and changing models of care in EDs have seen certain criteria now unable to be used to differentiate across the levels of accreditation. Similarly, the advent of trauma, cardiac and stroke systems across regions has resulted in a narrowing of where trainees can access certain patient cohorts and also blur the historic definition of a ‘tertiary’ facility. With respect to the CRP, the development of learning outcomes for the stages of training and the potential incorporation of specific formative assessment processes within the work place will allow for the creation of more objective criteria concerning the delivery of education within departments. The recent move towards providing options by which departments can meet accreditation criteria (e.g. Co-DEM and Co-DEMT models and formally accrediting training networks) is likely to continue as the College seeks to meet AMC recommendations to explore strategies by which training opportunities can be optimized in smaller facilities, in particular in regional and rural locations.
Overall, the development of a new accreditation framework that meets national requirements, incorporates new criteria from the ACEM CRP and modifies current criteria to reflect better the realities of the modern emergency medicine environment should result in new, more objective accreditation guidelines that focus on education delivery and the associated required resources, clinical supervision and trainee welfare.
27.6 Specialist training and recognition in emergency medicine in the United Kingdom
Kevin Reynard
Introduction
The changing landscape of postgraduate medical training in all specialties in the UK that occurred within the past decade is set to continue. The changes to the structure of training and recruitment have become embedded, during which time large-scale changes to the regulatory systems occurred. The system to fund, control and manage postgraduate medical education is in the process of large-scale change following recent legislation relating to health and social care in England. These systems have developed differently in Scotland, Wales and Northern Ireland.
An understanding of UK training in emergency medicine (EM) requires some knowledge of the regulatory bodies and systems that have been put in place since 2003, relating to the regulation of training, the shape of training and the content of training.
Regulation of training
General Medical Council (GMC)
Anyone who wishes to practise medicine in the UK must be registered with the General Medical Council. The GMC introduced a new registration framework in October 2007. This framework simplifies registration to either ‘full’ or ‘provisional’. Provisional registration allows newly qualified doctors to undertake general clinical training in the UK as a Foundation Year 1 doctor (see below) in posts specifically approved for this purpose. Full registration allows doctors to undertake unsupervised medical practice.
Those new to full registration, or those who have been away from UK practice for 5 years or more, must work for 1 year in an ‘approved practice setting’. A list of these placements can be found on the GMC website. They meet defined standards for training, support and management of doctors.
For either provisional or full registration, non-European Economic Area (EAA) applicants need to demonstrate to the GMC that they:
 hold an acceptable primary medical qualification
hold an acceptable primary medical qualification
 have the requisite knowledge and skills for registration
have the requisite knowledge and skills for registration
 a pass in the PLAB test (Professional and Linguistic Assessments Board)*
a pass in the PLAB test (Professional and Linguistic Assessments Board)*
 sponsorship by a medical royal college (or other approved sponsoring body)
sponsorship by a medical royal college (or other approved sponsoring body)
Doctors applying for full registration must also supply evidence that they have had a period of postgraduate experience equivalent to the general clinical training of the Foundation Year 1.
Detailed guidance is available at www.gmc-uk.org.
The GMC has taken over the role of independent regulator of postgraduate medical education, responsible for approval of curricula, training programmes and certification of completion of training.
Approval of curricula
The GMC has approved the curriculum for training in emergency medicine in the UK. The curriculum includes the syllabus, assessment methodology (including workplace based assessment and examinations) and the required training programme. There is also an approved curriculum for subspeciality training in paediatric emergency medicine. The GMC has approved speciality training programmes in intensive care medicine and pre-hospital emergency medicine, making the training period for those doctors who wish to achieve dual training in EM and one of these specialties longer than previously.
Specialist registration
Doctors who are fully registered with the GMC and who wish to practise as a substantive consultant or GP in the NHS must be on the specialist or GP register. The usual route for registration is to complete a full approved programme of training. Such doctors may then apply via their royal college for a Certificate of Completion of Training (CCT).
A second route, Certification of Eligibility for Specialist Registration (CESR), is available to doctors who have not completed a full approved training programme but who wish their training, qualifications and experience, wherever gained, to be considered for eligibility to be entered on to the specialist or GP register. Application forms, portfolios and other documentary evidence of what the doctor has achieved are sent by GMC to the relevant college for consideration and for a recommendation to be made with regard to registration. It is important to note that GMC is not bound by that recommendation.
If successful, such doctors are issued with a Certificate of Eligibility for Specialist Registration (CESR) which entitles them to apply for inclusion on the UK register but does not confer EEA registration privileges. The process tends to be slow and an application currently costs £1500. Fees to be included on the Medical Register are in addition to this.
Immigration rules
Immigration rules restrict access to UK postgraduate medical education (PGME) for international medical graduates (IMGs). This was driven by the concern that there may be insufficient training opportunities for UK and EEA graduates. A points-based system has been introduced to control immigration. Emergency medicine is currently a ‘shortage occupation’ in the UK. Hence, applicants who meet the requirements for registration with the GMC are highly likely to achieve the points total required under a tier 2 application for a visa for consultant posts or non-training junior doctor posts. It is possible that specialist training posts in emergency medicine will be included on the shortage occupation list. Further details and up to date information is available at www.ukba.homeoffice.gov.uk/visas-immigration.
Medical training initiative (MTI)
EM training in the UK for non-EAA doctors is also available for a period of 6–24 months under the medical training initiative. At the end of this period, trainees must return to their home country. Trainees are sponsored by the College of Emergency Medicine under a Government authorized exchange programme. Successful applicants are exempted from the PLAB test (but are excluded from applying if they have previously failed this test).
To be eligible for sponsorship the doctor must be one of the following:
The individual requirements for the MTI are that the doctor must:
 not (normally) hold EEA citizenship or EEA rights of residency
not (normally) hold EEA citizenship or EEA rights of residency
 hold a primary medical qualification acceptable to the GMC for full registration
hold a primary medical qualification acceptable to the GMC for full registration
 have completed at least 3 years postgraduate training, including an internship
have completed at least 3 years postgraduate training, including an internship
Postgraduate training in the UK
Following graduation, doctors enter a 2-year Foundation programme that delivers general clinical training, a broader experience and the acquisition and verification of generic competencies. Thereafter, those who have successfully completed such programmes and those doctors from other countries who can provide evidence of equivalent experience and competence (and who satisfy immigration rules) can apply for specialist training programmes. These programmes vary in their duration and pattern according to the specialty but lead to the award of a CCT.
Training in EM in the UK
The EM training programme in the UK lasts for 6 years. Acute care common stem (ACCS) training plus a further year in emergency medicine form the first 3 years (core training). During ACCS trainees undertake posts in EM, acute medicine, anaesthesia and intensive care medicine. This is followed by a year working in EM, with a particular focus on gaining paediatric competences and the non-technical skills to be able to lead and supervise others as a registrar. During this period, trainees must pass the diploma of Membership of the College of Emergency Medicine. This is followed by a 3-year specialist training programme leading to fellowship of the CEM to those successful in the exit examination. Transition from core to specialist training is by competition (Fig. 27.6.1).
Specialty training (ST) years 4–6 are spent in a series of EDs. Year-to-year progression is dependent on satisfactory assessment and appraisals, mostly conducted in the workplace. In the final year of training, candidates who are supported by their local programme are eligible to sit for the FCEM examination, successful completion of which is necessary for eligibility for a CCT.
Many higher training posts are unfilled. The reasons for this are widely debated, but include the unsocial nature of the work, the intensity of work, terms and conditions of service compared to elective specialties and primary care, the change in the specialty as a consequence of the emergency care standard (‘4-hour target’) and changes in immigration rules. Currently, these pressures are not adequately compensated for by the rich and rewarding aspects of the work. CEM, in conjunction with other bodies, is striving to correct this imbalance.
It is anticipated that, in the future, trainees will be eligible to move from other training programmes, with recognition of transferable competencies allowing entry at an appropriate point, rather than starting at the beginning of ACCS.
Subspecialty training
Paediatric EM is a recognized CCT subspecialty of both EM and of paediatrics. EM trainees who hold a CCT may undertake additional training in the care of children. The format and content of this training has been agreed by CEM and the Royal College of Paediatrics and Child Health (RCPCH) and lasts for at least 1 year.
Conclusion
The training programme has been through a period of marked transition as a result of forces from within and outside the specialty. There has been a period of stability upon which further refinement, rather than wholesale change, will be likely. ACCS is very popular with trainees with significant competition for places. There is much less competition for higher training posts. Anyone interested in EM training in the UK is advised to make frequent visits to the websites of CEM, GMC and the UK Border Agency.
27.7 Complaints
Peter Garrett
Introduction
Complaints are inevitable in the setting of busy emergency departments (EDs) and high patient expectations. Senior ED staff are well aware of what constitutes optimal care. Unfortunately, EDs are areas where there is little control over the cases presenting or the timing and volume of new arrivals; that combined with a mixture of staff with different levels of experience, long waits and multiple other reasons (Table 27.7.1) means that complaints are common.
Table 27.7.1
Contributing factors and reasons for complaints
Unpredictability of case mix and case load
Variation in attendance rates
Long waiting times
Insufficient staffing for unexpected peaks
Junior staff with variable experience and supervision
Deficiencies in treatment (real or perceived)
Inadequate assessment and missed diagnosis (real or perceived)
Poor attitudes, lack of professionalism
Poor communication, lack of information or consent
Interruptions, multiple concurrent tasks
Delays in investigations, consultations
Access block to inpatient beds
No appropriate follow up
Inappropriate or premature discharge
Unmet expectations
Invasion of privacy
Fees in private hospital EDs
Litigation for compensation
Improvements in clinical care resulting from advances in emergency medicine (EM) and nursing have set new standards with which the public has become familiar through the media. Patients and their relatives have much higher expectations of EDs than previously. They are better informed, more litigious and encouraged by marketing from legal firms. Nevertheless, most patients who may have legitimate cause for complaint do not formally complain. The frequency of complaints is not an accurate gauge of patient satisfaction.
Incidence
Complaint rates about ED care vary from 0.26 to 3.8 complaints/1000 patients [1,2]. Some hospitals only record written complaints, while others also include verbal complaints in their data. Often the complaints refer to more than one issue. More complaints relate to paediatric patients and more are made by the literate.
In a Victorian study of 2419 ED-related complaints from 36 hospitals over 5 years, 37% were made by the patient while 48% were from relatives. Friends accounted for 3% and the rest included GPs, specialists, government representatives and lawyers. ED complaints were 14.3% of the total 16 901 hospital complaints [1].
Reasons
In this study, there were four main categories for complaint: problems relating to care (inadequate treatment, diagnosis or follow up–33%), communication (relaying information, rudeness and discourtesy–31%), access (26%) and administrative deficiencies (incorrect documentation, inability to obtain previous records, lack of privacy or confidentiality and loss of property–7%) [1]. In most other studies, communication is far and away the highest category [2]. In private hospitals, fees are an increasing source of complaint.
The two commonest motivations behind complaints are either the seeking of compensation or threatening litigation due to inadequate clinical care or seeking assurance that corrective measures will be made to ensure that no one else has a similarly unpleasant experience for a variety of reasons [3].
Clinical care
About 50% of complaints claiming inadequate medical assessment and treatment are substantiated [2]. Inadequate physical examination followed by a missed or delayed diagnosis is a frequent complaint and can only be refuted if relevant positives and negatives found at the initial visit are documented accurately.
Medicine is not an exact science and early clinical features may be atypical or overlap with other causes which seem unlikely at initial presentation. Explaining this to the anxious patient who wants a quick diagnosis and symptom relief can pose difficulties for a busy doctor.
Missed fractures are the most frequent ‘misdiagnosis’. Some ‘misdiagnoses’ as perceived by patients result from poor communication, with lack of explanation by the treating doctor of the possible causes or what to do if there is no improvement [2].
Lack of treatment includes insufficient or no analgesia, lack of X-rays, blood tests, urine culture or antibiotics (where an initial presentation, particularly in a child, may have suggested a viral illness with eventual progression to a bacterial infection) and lack of a splint for a ‘soft-tissue injury’, which is subsequently diagnosed as a fracture.
Rough, unskilled or incompetent treatment still occurs despite advances in training of both doctors and nurses. A heavy workload is not an acceptable excuse. With the reduction in allowable weekly labour hours for hospital-employed doctors, EDs may rely to some extent on junior staff and locums under variable levels of senior supervision on some rosters.
Unprofessional conduct and refusal to refer to a specialist or to a previous treating doctor are unacceptable causes of complaint. Cases of sexual misconduct are very rare in EDs and would be referred to a medical board.
Communication
Failures of communication feature prominently in most complaints [4]. Failure of doctors to introduce themselves and to explain the reasons for examination, investigations, treatment, admission or discharge, referrals or delays are all avoidable causes of complaints.
Abruptness, rudeness, discourtesy, insensitivity, absence of caring and other aspects of poor attitude used to be the main reason for complaints but, perhaps as standards in general society have changed, this is no longer the case. However, in EDs, when people are rightfully anxious about their medical condition, such attitudes should not be tolerated. Lack of formality, addressing older patients by their given name, casual dress standards and missing identification have become the accepted norm in many Australasian hospitals, but may still upset some of our senior citizens and immigrants.
Failure to obtain consent in the case of minors or to gain informed consent for procedures and to warn about risks occurs commonly in EDs, where it is assumed that attendance implies consent, but this can be challenged if the patient is brought to hospital by ambulance or other means.
Doctors may miss significant clues if they ignore aspects of a patient’s history which do not fit with a presumptive diagnosis. This may also occur if the history is rushed and overly brief. Incorrect documentation and poor clinical handover is a common source of complaint, particularly when it results in the wrong treatment.
Reliance on referring letters or ambulance sheets without interviewing the patient can result in transcribing incorrect past history, medication charts and allergies. It cannot be assumed that referral details or old case histories are correct. Objective evidence of diagnoses should be sought.
It can be difficult to identify a ‘source of truth’, when people do not have a regular physician. This can be compounded by ‘doctor-shopping’, where patients attend the most convenient bulk-billing family medicine clinic, where their past history is unknown, hoping for a quick cure for acute problems, while reserving attendances at their usual general practitioner for more complicated ongoing illnesses.
Clinical staff in EDs are commonly faced with excessive communication loads. The combination of interruptions and multiple concurrent tasks resulted in 36 communication events an hour in one study and this may produce clinical errors by disrupting memory processes [5].
Delays
Difficulty with access to healthcare is a worldwide problem, even in first world countries, where economic rationalism and changing government policies have resulted in closure of hospital beds, mental health institutions and community resources. Lifestyle and industrial issues have decreased the numbers of medical and nursing staff in hospitals, particularly after hours.
Diminished outpatient services may mean that patients need to be referred to private consultants’ rooms where appointments may not be readily available. Fewer general practices open in the evenings or weekends. Some patients want a one-stop service for their medical consultation, their laboratory tests and their radiology. These social reasons make unnecessary use of scarce resources, despite strategies, such as telephone triage services and hospital-run after hours GP clinics. All the above have contributed somewhat to increased ED attendances.
Delays in triage, time seen by doctor, treatment, investigations, consultations, admission or discharge may therefore occur. Measures to decrease these are only partially successful because there is generally no excess of staff or resources to call upon when there are unexpected peaks in workload. Steps to improve waiting times, increase throughput of short-stay patients and decrease misdiagnosis of fractures have resulted in fewer complaints [6].
Particularly in the case of children and distressed patients, long delays cannot be easily tolerated and a significant number ‘walk out’ without being seen. The majority of these do not generate a complaint, but some progress to increased morbidity [8]. The elderly are less likely to complain, but suffer in silence, such that any pain they have may be unrecognized and untreated until late in the management [9].
Administration
Incorrect documentation by clerical, nursing or medical staff, lack of privacy or confidentiality, loss of valuables, poor cleaning or other environmental issues and queries regarding billing in private hospitals comprise the majority of administrative complaints [1,2].
Errors can be made by doctors in giving advice regarding a patient’s right to claim compensation, since the full circumstances cannot easily be ascertained at the time of consultation. Doctors should not advise patients regarding entitlements to worker’s or traffic accident compensation, but should complete the necessary documentation objectively.
Poor department design, lack of an accessible staff room or little adherence to departmental policy may cause complaints about staff socializing, eating or drinking. Their laughter may be seen by some patients as inappropriate, but by others as a sign of good staff morale.
The Federal Privacy Act 1988 was recently amended and became effective in December 2001 and resulted in removal of prominent whiteboards detailing patient information viewable by other patients and visitors [7,10]. Computers are now used in most departments, but even these may be visible to passers-by.
The Federal Privacy Act gives patients a general right of access to information held about them (see Chapter 25.4 Privacy and confidentiality). While patients have right of access, they must obtain consent from the doctors for further reproduction of the material, as the doctor still has ownership of clinical notes and specialists have legal rights over their reports. Relevant material must be made available to another doctor. Refusal of access must be based on reasonable grounds, such as that access would pose a serious threat to the life or health of any person. Conversely, information held by the doctor on the patient must not be divulged to third parties without patient consent, unless compelled by law, such as with mandatory reporting of child abuse [7].
Unmet expectations
Patient satisfaction surveys have ranked waiting times, symptom relief, a caring and concerned attitude and correct diagnosis as priorities when attending an ED. However, there is a mismatch when compared with staff who agree with the priorities but rank waiting time fourth [11].
Patients expect ED doctors to identify serious or dangerous conditions and to treat these appropriately. Explanation and reassurance are needed. Patients expect investigations and admission as indicated [3].
Responding to a complaint
Effectively responding to a complaint minimizes the likelihood of adversity and escalation. An effective response is early, supportive, open, even-handed and constructive. It should be backed up by a clear, accountable and outcome driven complaints management process that is supported by hospital administration (Table 27.7.2).
Table 27.7.2
Suggested procedure for response to complaints
Accept the complaint
Apologize for the complainant’s dissatisfaction
Defuse any anger
Record the details
Undertake to investigate
Arrange follow up
Investigate
Discuss with staff
Inform administration
Consider legal implications
Follow up with complainant
Resolve complaint
Lessons to be learnt
The immediate response
When a verbal complaint is made, the person to whom it is made has a responsibility to respond at the time as well as notify the appropriate manager of the service. This response should be immediate, genuine and supportive of the complainant’s right to raise issues. The more immediate and active the response the less likely that the complainant will feel alienated or aggrieved and the more likely that anger will be rapidly defused [12]. If a consultation is not going well or there appears to be dissatisfaction brewing, rather than avoid the issue and escape from the situation, it can help to ask if there is anything on the patient’s mind or ask a colleague or senior to assist by consulting. In both the public and private sectors, most unsatisfied patients may not complain immediately, but will spread their disapproval more widely via contacts or media, which can ultimately have an adverse effect on staff morale and future interactions.
Diffusing dissatisfaction and conflict
A genuine empathic response to a complaint will be more likely to lead to a successful outcome [13]. The person should be interviewed in a private place or office away from distractions and listened to in an open and supportive way, without interruption, and avoiding defensive postures and interjections. This is similar to how doctors listen to the medical ‘complaint’ and using the same principles helps. Early excuses, uninformed speculation or a defensive response without appearing to look into the matter will be seen through easily and regarded as dismissive and arrogant. If the person is rude or abusive, it is wise not to mirror this or terminate the meeting prematurely, but state that one still wants to help, understands that they are upset, in the knowledge that showing anger will make it harder to work together to get an appropriate outcome. If an ‘independent’ support person is available, such as a social worker, interpreter (or even a neighbour), for emotional, psychological or other support, this can help both doctor and patient.
Support of the complainant
The person has a right to alert the doctor of their concerns and be heard and to receive reassurance that they will be taken seriously. It helps to let the patient know what the doctor intends to do with their complaint, what the patient’s rights are and that they have alternative routes to raise issues. Some experienced doctors are confident enough to thank the person for their complaint, on the basis that it provides an opportunity to improve services. A person who cares enough to report a problem in a department has great potential later to become a satisfied client. If some complaints may seem trivial, any underlying reasons or causes should be explored, as failure to address their underlying concern may perpetuate the correspondence. It can help to encourage the patient to bring their support person as the presence of a less emotional witness improves recall and can moderate the experience.
Expressing regret
An expression of regret acknowledges the complaint and does not admit error or that the complainant is correct. The more serious the issue being complained about, the more relevant the apology is to establishing empathy and creating an open and honest relationship with the person [15].
Documenting and investigating
As part of receiving the complaint, it is important to document clearly the complainant’s perception of the issues, as well as the name, relationship to patient and correct contact details. At the end of the meeting it is a good exercise to summarize their perception of the issues, outline what actions will be next and the timelines for response.
In the information gathering process it pays to cross-check facts meticulously as any sloppiness in this phase will damage the process later. Take the time to interview involved staff, check medical records and do not be surprised if early assumptions are incorrect.
Determining the issues
Determining what the person wants may not be straightforward, as they may not have crystallized it yet, or be willing to articulate it. People would reasonably expect respect, an understanding of point of view, an immediate investigation of the true facts, early feedback and/or resolution and assurance that the problem will not recur to them or others. These are reasonable and deliverable aspirations and any department should have a system that supports this.
Some complainants want ‘someone’ to be reprimanded or punished (particularly if rudeness or lack of compassion featured) and some may feel they need some financial recompense. The desire for censure can be mitigated by a genuine apology for their experience by the involved staff or by their senior and, if relevant, explanation that contributing systemic issues were involved and will be addressed. If a complaint about unprofessional conduct is upheld, the option of escalating the complaint to a professional body should be available. There may be some scope in private hospitals to renegotiate costs if these contribute to a complaint.
Supporting staff and confidentiality
Most doctors and nurses are devastated when a complaint is made and might feel the need to justify what the patient perceived, disagree with recall and may feel anger towards the complainant. It should be sensitively explained that any complainant is voicing dissatisfaction with a perception and that everyone’s views are being sought to investigate the facts fairly and openly and it may have value in improving the service.
It helps to reassure all that the principles of natural justice will be upheld and confidentiality of the staff and patient will be maintained.
If staff are distressed by the process, support and counselling should be offered, as many doctors and nurses have left the profession as a result of complaints, even though they were not directly responsible for the outcome [14]. Most jurisdictions now operate a ‘systems approach’ to what we used to call ‘human error’ and part of this is accepting personal fallibility (it’s normal to be human) and concentrating on identifying what systems issues require action. Any competence or conduct issue should be addressed by the director of training or supervisors and may form part of a regular ‘performance appraisal’ [15].
Resolution
Once the facts have been established, ideally, corrective actions are identified that will prevent the event that provoked the complaint from recurring. Assess what the most appropriate resolution approach to take is. Facts laid out in a non-judgemental way, any corrective actions proposed and perhaps a repeat of the expression of regret form the basis of the follow-up interview or letter. Address all the issues raised. Rarely, it is advisable to refer to an external investigator or mediator and there should be hospital policy available on this.
In the Victorian study, most complaints (75%) were satisfactorily resolved by explanation of facts and/or apology [1]. Changes in policy occurred in 2% and remedial action took place in 5%. Very few complaints went to the legal system (<1%). The remainder were not upheld, not pursued or found to be frivolous. This is similar to the experience of the state health complaints commissions or ombudsmen where most complaints are resolved by free and open investigation, explanation and conciliation, and very few are seeking censure.
Integrating with risk management
An effective complaints handling process can integrate well with risk management processes, by identifying areas for improvement. A complaint may highlight unusual patterns of practice, deficiencies in protocols and guidelines, areas for further training and even provide the objective evidence needed for development of an ED business case. Complaints and compliments should be included in the risk management discussion of any senior staff meeting.
If the complaint has medicolegal or adverse publicity implications, the Medical Director and/or Executive Officers need to be informed to allow a considered response. Systems might exist that facilitate or enforce this, such as incident monitoring systems, sentinel event monitoring or the formal open disclosure process.
Prevention
System design
A well-equipped ED with adequate numbers of senior medical and nursing staff supervising junior staff, all aware of their scope of practice, will likely have fewer complaints. The department’s design can enhance safety, with good waiting area and resuscitation area visibility, patient privacy maintained, temperature and noise levels comfortable, provide sufficient space, easy access to rest rooms and refreshment and education areas for staff close by [6]. Pain or X-ray protocols should be considered and prioritizing pathology requests.
Verbal and printed information on the frequently complained about areas of triage system, assessment and investigation turn around times, can be provided to waiting patients. High-risk groups that poorly tolerate prolonged waits, like children and psychiatric patients, can be triaged to be seen earlier.
Systems and procedures to follow up abnormal pathology and imaging results should exist and be audited, as 1 in 6 missed diagnoses are related to follow-up processes. Clinical handover, the effective transfer of information and responsibility, is now a major initiative of the Australasian College for Emergency Medicine (ACEM) and Australian Council for Safety and Quality in Health Care (ACHQS) and each department should support a protected and formalized handover process.
People
A polite well-groomed doctor who introduces him- or herself, makes eye contact, shakes hands and uses the person’s title and surname can help to avert complaints. Talking out loud any examination findings as they conduct the examination can minimize accusations of inadequate examination, as stressed patients have poor recall and distorted perception of the interaction.
Adequate documentation of the encounter may provide the only means of refuting or resolving a complaint and while complaint- specific proforma, computerized decision support and discharge instructions can help documentation, preserving time to complete documentation is still important. Records must not be altered after a complaint.
A pro-active approach to complaints handling as part of a wider incident reporting system can result in higher patient and staff satisfaction. Specific training on how to relate to people in the pressured ED environment and how to handle complaints effectively should be incorporated into orientation and undergraduate education for nurses and doctors.
Managing specific aspects
Written formal complaints
Acknowledging the notification as immediately as possible, ideally within 3 days, together with an apology that they have experienced dissatisfaction is an expectation in many jurisdictions. This early response, along with the commitment to investigate and act on any findings may be satisfactory for many complainants. If the matter is clinically significant or may escalate, an early phone call in advance of the written response, perhaps to invite more information or, better, a managed face-to-face meeting. The Australian Council for Safety and Quality in Health Care has published examples of letters and responses [15].
Catastrophic adverse events
If the complaint is about a serious adverse event, such as a deterioration or death, many hospitals advocate the Open Disclosure model, an initiative of the former Australian Council for Safety and Quality in Health Care. The elements of open disclosure are an expression of regret, a factual explanation of what happened, the potential consequences and the steps being taken to manage the event and prevent recurrence. There is an early informal phase where the treating clinician informs the patient of what has occurred and expresses regret for the harm caused or adverse outcome, with follow up in the form of formal open disclosure, which is about facilitating more consistent and effective communication between the patient, the senior clinician and the organization using a trained team in response to the most serious adverse events [15,16].
Grief reactions
Manifestations of grief and the desire to know all the circumstances should be respected but avoiding unverified explanation. Sometimes, a need to blame is part of the grieving process. Again, it is useful to offer support [11] (pastoral care, social worker, external counsellors or psychologists) and some Open Disclosure systems approve financial support to facilitate supportive acts (transport for a family member to come, accommodation close by).
Unreasonable requests or expectations
While the ultimate outcome may be a negative, it can help to start with a positive assertion and try to establish a working relationship: ‘Yes, I can see that this needs to be sorted out. Let me enquire what resources are available to your GP to assist us in this’. A two-way communication allows the complainant to vent and prevents missing any important information. ‘Yes, I can see why you are worried about taking John home. Let’s talk through what the problems are and the early and longer term solutions to this.’
‘Pests’ or persistent complainants
A small number of complainants are unwilling to accept decisions, continue to demand further action, insist on outcomes that are clearly not appropriate or demand things they are not entitled to. They may constantly change the complaints, complain about the process, complain to multiple bodies simultaneously or make inappropriate freedom of information (FOI) requests. While it is tempting to pass them quickly up the chain, this can reinforce their behaviour and create more work. Try to own the complaint, manage their expectations early of what is going to happen and what is possible. Focus your attention on the conduct, not the person and, similarly, separate the conduct from the complaint. Be firm and clear about what is not going to happen, that some complaints have no further avenues and that re-raising the complaint will not be responded to [17].
Delays
Frequent and realistic communication by all staff can help, explaining what delays are occurring, that triage times are revised, why repeated consultations occur, why tests are being done and what the likely outcome of the wait is. It is useful to avoid unrealistic promises like ‘I’ll be back in a minute’ or ‘they said they’d be down from theatre straight away’.
Summary
Complaints are a source of stress and concern for both emergency physicians and their patients. They are inevitable, part of our responsibility and should not be avoided. An understanding of the public’s expectations from their attendance will assist in prevention of complaints [17].
Poor complaints management can damage a department. A good complaints management process can help by saving time, avoiding escalation, restoring the trust and confidence of patients, improving the safety and quality of the service and creating a more satisfactory working environment for staff.
Good complaints management can be easily learnt, but it sometimes requires a change in attitude; the most influential factor in changing attitudes and culture in an organization is senior leadership.
27.8 Patient safety
Peter Sprivulis
Introduction
Patient safety, or the freedom from accidental injury due to medical care or from medical error, is increasingly being recognized as a critical consideration in the delivery of acute and emergency healthcare [1]. Several OECD countries have examined the proportion of acute care admissions during which an adverse event (an unexpected medical problem that happens during treatment with a drug or other therapy) is identifiable using a standard medical chart review. They typically report that 1 in 10 admitted patients experiences an adverse event, of which half are considered preventable with the current state of medical knowledge (i.e. are due to medical error) [1]. Typically, one-third of adverse events leads to moderate or greater disability or death [1]. An important consideration for the emergency care of admitted patients is that the day of greatest risk of an adverse event is usually the first day of admission to hospital. This is when knowledge of the patient’s clinical condition is often incomplete, the clinical condition is least stable and when most patients experience the greatest number of procedures and interventions [2].
Specific emergency department factors that may compromise patient safety
Safe patient care is challenged by several specific emergency department (ED) factors that include:
 Staff factors: ED staffing profiles, particularly in public EDs, typically include a high proportion of junior medical and nursing staff who are still in training. Safety improves with experience. In addition, there is usually a scheduled high turnover of staff, as staff are rotated between alternate training positions. These high levels of rotation can corrode ‘memory’ of safe and desirable processes and systems of care. ED staff are usually rostered to work shifts spanning 24 h a day. Poorly designed rosters may contribute to fatigue [3,4].
Staff factors: ED staffing profiles, particularly in public EDs, typically include a high proportion of junior medical and nursing staff who are still in training. Safety improves with experience. In addition, there is usually a scheduled high turnover of staff, as staff are rotated between alternate training positions. These high levels of rotation can corrode ‘memory’ of safe and desirable processes and systems of care. ED staff are usually rostered to work shifts spanning 24 h a day. Poorly designed rosters may contribute to fatigue [3,4].
 Clinical factors: ED patients have an inherently high severity of illness, placing them at greater risk of serious adverse sequelae if a medical error occurs. In addition, the undifferentiated nature of illness and injuries cared for, often coupled with the incomplete clinical information, creates clinical uncertainty, increasing risk [4,5].
Clinical factors: ED patients have an inherently high severity of illness, placing them at greater risk of serious adverse sequelae if a medical error occurs. In addition, the undifferentiated nature of illness and injuries cared for, often coupled with the incomplete clinical information, creates clinical uncertainty, increasing risk [4,5].
 Physical environment: EDs are noisy, busy work spaces, with frequent intrusions from alarms, pages, telephone calls and personal consultations, all of which create distractions, increasing the risk of error [6].
Physical environment: EDs are noisy, busy work spaces, with frequent intrusions from alarms, pages, telephone calls and personal consultations, all of which create distractions, increasing the risk of error [6].
 Linkages to other care systems: emergency care is reliant upon a complex set of relationships between the ED, referring practitioners, pre-hospital carers, other hospital services and other services responsible for aftercare or following up after discharge from the ED. Poor linkages or communication between the ED and any of these other services can result in errors or omissions in information transfer that compromise patient safety [7].
Linkages to other care systems: emergency care is reliant upon a complex set of relationships between the ED, referring practitioners, pre-hospital carers, other hospital services and other services responsible for aftercare or following up after discharge from the ED. Poor linkages or communication between the ED and any of these other services can result in errors or omissions in information transfer that compromise patient safety [7].
 Overcrowding: EDs have little control over patient attendance and, increasingly, suffer overcrowding as a consequence of poor access to beds downstream of the ED for admitted patients. This is associated with overcrowding and increased mortality, most likely due to a combination of resource effects (incorrect or insufficient resources or attempting procedures or monitoring in inappropriate locations) and delays in time to critical care [4,8].
Overcrowding: EDs have little control over patient attendance and, increasingly, suffer overcrowding as a consequence of poor access to beds downstream of the ED for admitted patients. This is associated with overcrowding and increased mortality, most likely due to a combination of resource effects (incorrect or insufficient resources or attempting procedures or monitoring in inappropriate locations) and delays in time to critical care [4,8].
Common safety problems encountered in emergency departments
The factors described above interact to create a wide range of risks to patients needing emergency care [4]. Some of the errors observed in the emergency setting include:
Improving safety in the emergency department
Specific actions to improve patient safety should be undertaken in the context of a comprehensive organizational framework for clinical governance and quality improvement [1]. The development of a programme of safety improvement for an ED should be undertaken methodically, in accordance with existing Australasian and international standards that usually encompass the following process elements:
 For every thousand prevented or no-harm incidents there may be a hundred of the same type that cause minor to moderate harm, 10 that cause severe harm and 1 that causes death. Therefore, it is important to learn from the prevented or no harm incidents to reduce the chance of the single death incident happening. Often, employees are more willing to report near misses. The importance of including near misses in the incident reporting systems cannot be overemphasized [1].
For every thousand prevented or no-harm incidents there may be a hundred of the same type that cause minor to moderate harm, 10 that cause severe harm and 1 that causes death. Therefore, it is important to learn from the prevented or no harm incidents to reduce the chance of the single death incident happening. Often, employees are more willing to report near misses. The importance of including near misses in the incident reporting systems cannot be overemphasized [1].
 Treat the risks: two common preconceptions that can stand in the way of an effective remedy include the ‘perfection myth’–if we try hard enough we will not make any errors–and the ‘punishment myth’–if we punish people when they make errors they will make fewer of them. In reality, at least 80% of errors may be attributed to poorly designed care systems and processes that fail to account for human fallibility. Unfortunately, the mere publication of a new clinical guideline rarely results in a sustained change in practice. For these reasons, the preferred approach to reducing risk is to use the principles of reliability engineering and process redesign that substitute clumsy, unreliable and dangerous processes or systems with standardized and sustainable processes that make errors more difficult to perform, make the ‘right’ thing to do the easiest thing to do and aid the detection and correction of errors if they do occur (e.g. replacement of vials of similar appearing drugs with well-labelled, prefilled syringes on a resuscitation trolley) [1].
Treat the risks: two common preconceptions that can stand in the way of an effective remedy include the ‘perfection myth’–if we try hard enough we will not make any errors–and the ‘punishment myth’–if we punish people when they make errors they will make fewer of them. In reality, at least 80% of errors may be attributed to poorly designed care systems and processes that fail to account for human fallibility. Unfortunately, the mere publication of a new clinical guideline rarely results in a sustained change in practice. For these reasons, the preferred approach to reducing risk is to use the principles of reliability engineering and process redesign that substitute clumsy, unreliable and dangerous processes or systems with standardized and sustainable processes that make errors more difficult to perform, make the ‘right’ thing to do the easiest thing to do and aid the detection and correction of errors if they do occur (e.g. replacement of vials of similar appearing drugs with well-labelled, prefilled syringes on a resuscitation trolley) [1].
Conclusion
Patients seeking emergency care are at significant risk of harm, in part due to their clinical situation and in part due to the challenges of delivery of emergency care itself. Improving patient safety in the ED requires a systematic approach to risk identification, risk analysis and evaluation and the implementation of safer processes of care. Monitoring is an essential component of patient safety improvement. An open, communicative culture that promotes reporting and minimizes blame supports patient safety improvement.