Procedure 26 Posterior Far Lateral Disk Herniation
Indications
 Intractable radiculopathy resistant to conservative measures
Intractable radiculopathy resistant to conservative measures
 Unilateral, single-level, nerve root compression lateral to the neuroforamen
Unilateral, single-level, nerve root compression lateral to the neuroforamen
 Far lateral disk herniation confirmed by computed tomography (CT) scan or magnetic resonance imaging (MRI): nucleus pulposus herniates beyond the intervertebral foramen, or at least two-thirds lateral to the vertebral pedicle (Papavero and Caspar, 1993).
Far lateral disk herniation confirmed by computed tomography (CT) scan or magnetic resonance imaging (MRI): nucleus pulposus herniates beyond the intervertebral foramen, or at least two-thirds lateral to the vertebral pedicle (Papavero and Caspar, 1993).
 Absence of segmental instability, facet incompetence, or additional pathologies, that is, spinal stenosis or associated central disk herniation
Absence of segmental instability, facet incompetence, or additional pathologies, that is, spinal stenosis or associated central disk herniation
 Radiculopathy correlating with radiographic evidence of far lateral disk herniation (FLDH) compressing the symptomatic exiting nerve root
Radiculopathy correlating with radiographic evidence of far lateral disk herniation (FLDH) compressing the symptomatic exiting nerve root
Indications Controversies
• A far lateral disk herniation (FLDH) associated with adjacent canal stenosis at the level above
• Monoradicular symptoms (denoting isolated far lateral disk herniation) versus multiradicular symptoms (denoting a far lateral disk associated with medially located pathologies, including degenerative changes, canal stenosis, or central disk herniations)
Examination/Imaging
Surgical Anatomy
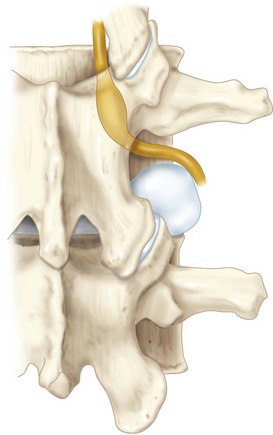
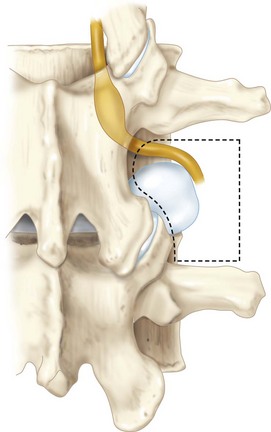
 Anatomic definition: Far lateral, extraforaminal, or extreme lateral disk herniation denotes a disk hernia occurring lateral to the neuroforamen and the facet joint complex (Figure 26-2). The herniated disk fragment usually compresses the exiting nerve root and displaces it superiorly and laterally under tension.
Anatomic definition: Far lateral, extraforaminal, or extreme lateral disk herniation denotes a disk hernia occurring lateral to the neuroforamen and the facet joint complex (Figure 26-2). The herniated disk fragment usually compresses the exiting nerve root and displaces it superiorly and laterally under tension.
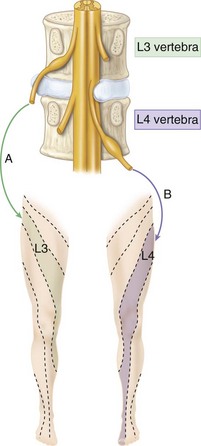
 Because of its anatomic location (Figure 26-3, A), unlike the posterolateral herniated nucleus pulposus (HNP), which affects the traversing nerve root (Figure 26-3, B), FLDH affects the exiting nerve root at the same level.
Because of its anatomic location (Figure 26-3, A), unlike the posterolateral herniated nucleus pulposus (HNP), which affects the traversing nerve root (Figure 26-3, B), FLDH affects the exiting nerve root at the same level.
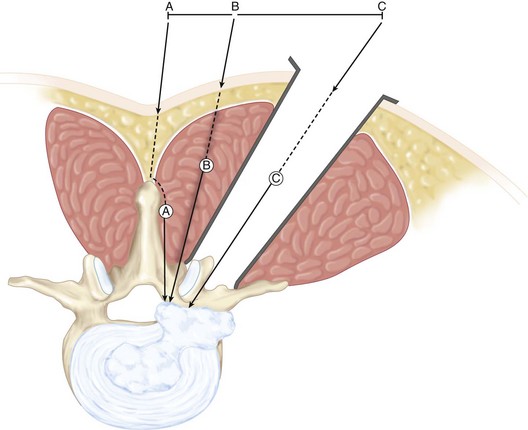
 The anatomic boundaries of the “operative window” or “surgical corridor” for the intertransverse lateral approach (Figure 26-4) are
The anatomic boundaries of the “operative window” or “surgical corridor” for the intertransverse lateral approach (Figure 26-4) are
Positioning
 The prone position with abdomen free hanging is preferred by most surgeons.
The prone position with abdomen free hanging is preferred by most surgeons.
 Although both regional and general anesthesia have been described (Reulen et al, 1996), general anesthesia with endotracheal intubation offers more control of the airway and is preferred by the authors.
Although both regional and general anesthesia have been described (Reulen et al, 1996), general anesthesia with endotracheal intubation offers more control of the airway and is preferred by the authors.
Positioning Pearls
• Positioning the patient on an Andrews frame in a kneeling position allows flexion of the lumbar spine and opening of the intertransverse space, therefore providing a better access to the neural foramen.
• Clearing the abdomen from any compression during positioning prevents intraabdominal pressure–related venous congestion, thereby reducing the risk of bleeding and helping in lumbar flexion.
Portals/Exposures
 Localization and placement of an accurate skin incision is made possible with the use of plain radiographs or C-arm fluoroscopy (anteroposterior and lateral views); following identification of the affected disk level, two horizontal and two vertical lines are marked on the skin.
Localization and placement of an accurate skin incision is made possible with the use of plain radiographs or C-arm fluoroscopy (anteroposterior and lateral views); following identification of the affected disk level, two horizontal and two vertical lines are marked on the skin.
 Horizontally, the upper line marks the inferior border of the transverse process proximal to the affected disk, and the lower line marks the inferior border of the affected disk space.
Horizontally, the upper line marks the inferior border of the transverse process proximal to the affected disk, and the lower line marks the inferior border of the affected disk space.
 Vertically, one line is placed centrally, marking the midline overlying the spinous processes, and a more lateral line (4- to 5-cm paramedian) marks the lateral borders of the pedicles above and below the affected disk level.
Vertically, one line is placed centrally, marking the midline overlying the spinous processes, and a more lateral line (4- to 5-cm paramedian) marks the lateral borders of the pedicles above and below the affected disk level.
 The site of the skin incision (3 to 4 cm in length, and 4- to 5-cm paramedian) is therefore outlined by these horizontal and vertical lines.
The site of the skin incision (3 to 4 cm in length, and 4- to 5-cm paramedian) is therefore outlined by these horizontal and vertical lines.
 Muscle-splitting technique: Following skin incision, the thoracolumbar fascia is identified and incised in line with the skin incision to expose the erector spinae aponeurosis, which is cut longitudinally to expose the multifidus and longissimus muscles. A blunt dissection is carried through the cleavage between the latter muscles and a self-retaining (McCulloch or Gelpi) retractor is placed to expose the “working zone.” This zone is located between the lower surface of the superior transverse process proximally, the superior surface of the inferior transverse process distally, the lateral surface of the pars interarticularis medially, and the tips of the transverse processes laterally (see Figure 26-3).
Muscle-splitting technique: Following skin incision, the thoracolumbar fascia is identified and incised in line with the skin incision to expose the erector spinae aponeurosis, which is cut longitudinally to expose the multifidus and longissimus muscles. A blunt dissection is carried through the cleavage between the latter muscles and a self-retaining (McCulloch or Gelpi) retractor is placed to expose the “working zone.” This zone is located between the lower surface of the superior transverse process proximally, the superior surface of the inferior transverse process distally, the lateral surface of the pars interarticularis medially, and the tips of the transverse processes laterally (see Figure 26-3).
Procedure
Step 1
Step 1 Pearls
• Blunt finger dissection and palpation of bony landmarks (transverse processes and lateral aspect of the pars) can help localize the “operative window.”
• A Kerrison rongeur can be used to remove part of the facet pars laterally, when necessary for adequate exposure.
• The soft tissue can be cleared off the bony landmarks of the working zone and the intertransverse membrane, using a series of angled (3-0) curettes and no. 2 curettes.
Step 1 Instrumentation/Implantation
Step 2
 Exposure of bony landmarks: transverse processes, facet joint, pars, and isthmus
Exposure of bony landmarks: transverse processes, facet joint, pars, and isthmus
 Exposure of the intertransverse muscle
Exposure of the intertransverse muscle
 High-speed burr, or Kerrison rongeur, can be used to partially remove bony overgrowth and improve exposure, as in cases of facet hypertrophy, at L5-S1 level, and around the lateral aspect of the pars.
High-speed burr, or Kerrison rongeur, can be used to partially remove bony overgrowth and improve exposure, as in cases of facet hypertrophy, at L5-S1 level, and around the lateral aspect of the pars.
Step 3
 The “intertransverse membrane” is exposed after incising the medial half of the intertransverse muscle, which is reflected laterally.
The “intertransverse membrane” is exposed after incising the medial half of the intertransverse muscle, which is reflected laterally.
 The posterior primary ramus is then identified, using a microscope as it crosses the medial portion of the intertransverse membrane and before it innervates the paraspinal muscles.
The posterior primary ramus is then identified, using a microscope as it crosses the medial portion of the intertransverse membrane and before it innervates the paraspinal muscles.
 Using the posterior primary ramus as a reference, the dorsal root ganglion and the spinal nerve are then located underneath the intertransverse membrane surrounded by connective tissue and extraforaminal fat.
Using the posterior primary ramus as a reference, the dorsal root ganglion and the spinal nerve are then located underneath the intertransverse membrane surrounded by connective tissue and extraforaminal fat.
 The spinal nerve is then handled very gently to avoid irritation of the dorsal root ganglion.
The spinal nerve is then handled very gently to avoid irritation of the dorsal root ganglion.
 Sweeping a ball-tipped probe beneath the nerve root, the herniated fragment can be identified and removed.
Sweeping a ball-tipped probe beneath the nerve root, the herniated fragment can be identified and removed.
 Identification of the pedicle below offers an alternative option to locate the HNP and the exiting nerve root (dorsal to the pedicle).
Identification of the pedicle below offers an alternative option to locate the HNP and the exiting nerve root (dorsal to the pedicle).
 Underneath the intertransverse membrane, the nerve root/spinal nerve branches are in close proximity to arterial-venous branches (lumbar artery) and herniated disk material. The lumbar artery is a potential source of vigorous bleeding, and should be spared whenever possible. Meticulous hemostasis using bipolar cautery helps exposing the extruded disk herniation, if obscured by venous bundles.
Underneath the intertransverse membrane, the nerve root/spinal nerve branches are in close proximity to arterial-venous branches (lumbar artery) and herniated disk material. The lumbar artery is a potential source of vigorous bleeding, and should be spared whenever possible. Meticulous hemostasis using bipolar cautery helps exposing the extruded disk herniation, if obscured by venous bundles.
Step 3 Pitfalls
• Postoperative anterior thigh burning sensation and dysesthesia may develop secondary to excessive manipulation of the dorsal ganglion during exposure. However, spontaneous resolution is expected.
• Persistent or recurrent leg pain occurs in 21.7% of operated patients, and development of foraminal stenosis or the presence of double herniation (combination of posterolateral and FLDH) should be considered (Chang et al, 2006).
Step 4
 Neurologic decompression: the extruded disk hernia is removed with a pituitary rongeur, and although, in most cases, this is considered sufficient for symptoms relief, further exploration and probing of the neuroforamen with a blunt probe, searching for any residual sequestered disk material or associated foraminal stenosis (notorious for unfavorable outcomes), may be necessary.
Neurologic decompression: the extruded disk hernia is removed with a pituitary rongeur, and although, in most cases, this is considered sufficient for symptoms relief, further exploration and probing of the neuroforamen with a blunt probe, searching for any residual sequestered disk material or associated foraminal stenosis (notorious for unfavorable outcomes), may be necessary.
 Following nerve root manipulation and probing, some surgeons prefer to place a steroid-soaked Gelfoam pledget at the site.
Following nerve root manipulation and probing, some surgeons prefer to place a steroid-soaked Gelfoam pledget at the site.
Step 5
 A surgical drain is not typically necessary.
A surgical drain is not typically necessary.
 Wound closure in layers: paraspinal muscles are usually reapproximated without sutures, and the fascia/aponeurosis are stitched with absorbable sutures.
Wound closure in layers: paraspinal muscles are usually reapproximated without sutures, and the fascia/aponeurosis are stitched with absorbable sutures.
 Local anesthetics (e.g., Marcaine [bupivicaine] without epinephrine) can be generously infiltrated into the soft tissues for analgesia. Deep injection of the local analgesics risks anesthetizing the exiting nerve root.
Local anesthetics (e.g., Marcaine [bupivicaine] without epinephrine) can be generously infiltrated into the soft tissues for analgesia. Deep injection of the local analgesics risks anesthetizing the exiting nerve root.
Postoperative Care and Expected Outcomes
Postoperative Pitfalls
• Wrong-level surgery mandates revision exploration and is prevented by use of intraoperative C-arm fluoroscopy or plain radiography.
• Spondylodiskitis should be treated with immobilization and organism-specific antibiotic therapy.
• Spinal instability, caused by excessive pars excision, may promote accelerated degeneration.
• Persistent/recurrent leg pain may complicate a battered nerve root syndrome, an inadequate decompression, or wrong diagnosis (20% of cases).
• Facet distress syndrome is leg pain (pseudoradicular) with low back pain, more often complicating an L5-S1 interlaminar decompression. Complication can be significantly prevented (incidence rate decreased by 50%) with use of a muscle-splitting technique instead.
Chang SB, Lee SH, Ahn Y, Kim JM. Risk factor for unsatisfactory outcome after lumbar foraminal and far lateral microdecompression. Spine. 2006;31:1163-1167.
Darden BV2nd, Wade JF, Alexander R, et al. Far lateral disc herniations treated by microscopic fragment excision: techniques and results. Spine. 1995;20:1500-1505.
Fankhauser H, de Tribolet N. Extraforaminal approach for extreme lateral lumbar disc herniation. In: Torrens MJ, Dickinson RA, editors. Operative Spinal Surgery (Practice of Surgery Series). Edinburgh: Churchill Livingstone; 1991:145-160.
Jackson RP, Glah JJ. Foraminal and extraforaminal lumbar disc herniation: diagnosis and treatment. Spine. 1987;12:577-585.
O’Brien MF, Peterson D, Crockard HA. A posterolateral microsurgical approach to extreme-lateral lumbar disc herniation. J Neurosurg. 1995;83:636-640.
O’Hara LJ, Marshall RW. Far lateral lumbar disc herniation: the key to the intertransverse approach. J Bone Joint Surg Br. 1997;79:943-947.
Osborn AG, Hood RS, Sherry RG, Smoker WRK, Harnsberger HR. CT/MRI spectrum of far lateral and anterior lumbosacral disc herniations. AJNR Am J Neuroradiol. 1988;9:775-778.
Papavero L, Caspar W. The lumbar microdiscectomy. Acta Orthop Scand Suppl. 1993;64:34-37.
Pearson AM, Blood EA, Frymoyer JW, et al. SPORT lumbar intervertebral disc herniation and back pain: does treatment, location, or morphology matter? Spine. 2008;33:428-435.
Reulen HJ, Muller A, Ebeling U. Microsurgical anatomy of the lateral approach to extraforaminal lumbar disc herniations. Neurosurgery. 1996;39:345-350. discussion 350-1