Emergency and Medical Systems
Edited by George Jelinek
26.1 Pre-hospital emergency medicine
Stephen A Bernard and Paul A Jennings
Introduction
Ambulance services have the primary role of providing rapid stretcher transport of patients to an emergency department (ED). Increasingly, paramedics are also trained to provide emergency medical care prior to hospital arrival in a wide range of life-threatening illnesses with the expectation that earlier treatment will improve patient outcomes.
Dispatch
Many countries have a single telephone number for immediate access to the ambulance service in cases of emergency, such as 911 in North America, 999 in the United Kingdom and 000 in Australasia. However, the accurate dispatch of the correct ambulance skill set in the optimal time frame is complex. It is inappropriate to dispatch all ambulances on a ‘code 1’ (lights and sirens) response, since this entails some level of risk to the paramedics and other road users. On the other hand, it may be difficult to identify accurately life-threatening illnesses or injuries using information gained from telephone communication alone, especially from bystanders. Also, it may be inappropriate to dispatch paramedics with advanced life-support training to routine cases where these skills are not required since they then become unavailable for a subsequent call.
In order to have consistent, accurate dispatch of the appropriate skill set in the optimal time frame, many ambulance services are now using computer-aided dispatch programs. These computer programs have structured questions for use by call-takers with limited medical training. Pivotal to accurate telephone dispatch is identification of the chief complaint, followed by subsequent structured questions to determine the severity of the illness. The answers to these questions allow the computerized system to recommend the optimal paramedic skill set and priority of response. This computer algorithm is medically determined according to local protocols and practices and provides consistency of dispatch.
Most ambulance services generally have at least four dispatch codes. A code 1 (or local equivalent terminology) is used for conditions that are considered immediately life threatening. For these, emergency warning devices (lights and sirens) are routinely used. The possibility of life-saving therapy arriving as soon as possible is judged as outweighing the potential hazard of a rapid response. In a code 2 (or equivalent) response, the condition is regarded as being urgent and emergency warning devices may be used only when traffic is heavy. In a code 3 response, an attendance by ambulance within an hour is deemed medically appropriate. Finally, a non-emergency or ‘booked’ call is a transport arranged at a designated time negotiated by the caller and the ambulance service.
Despite continuous developments in computer algorithms, accurate telephone identification of life-threatening conditions may be difficult. For example, identification of patients who are deceased (beyond resuscitation) [1], in cardiac arrest [2], or suffering acute coronary syndrome [3] has been shown to lack the very high sensitivity and specificity that might be expected.
The dispatch centre also has a role for telephone instructions on bystander cardiopulmonary resuscitation [4] and first aid. For conditions that are regarded as non-urgent, the dispatch centre may transfer the call to a ‘referral service’ for the provision of a medical response other than an emergency ambulance. This might include dispatch of a district nurse for a home visit or the provision of simple medical advice with instructions to see a family physician or attend an emergency department if symptoms persist.
Clinical skills
Ambulance treatment protocols vary considerably around the world. Since there are few randomized, controlled trials to provide high quality evidence-based guidance for pre-hospital care, there is still much controversy and considerable variation in the ambulance skill set in different ambulance services.
Many ambulance services provide a number of varying levels of skill set, dispatching ambulance officers trained in basic life support (including defibrillation) to non-emergency or urgent cases (ambulance paramedics) and more highly trained officers (designated as advanced life-support paramedics or intensive-care paramedics) to patients with an immediately life-threatening condition for which advanced life-support skills may be appropriate [5]. In addition, ambulance services may co-respond with other emergency services (such as fire fighters) to provide rapid-response defibrillation.
The evidence for some of the more common pre-hospital interventions is outlined in the following sections.
Trauma care
Pre-hospital trauma care may be considered as either basic trauma life support (clearing of the airway, assisted ventilation with a bag/mask, administration of supplemental oxygen, control of external haemorrhage, spinal immobilization, splinting of fractures and the administration of inhaled analgesics) or advanced trauma life support (ATLS) including intubation of the trachea, intravenous (IV) fluid therapy, decompression of tension pneumothorax and the administration of intravenous analgesia.
Basic trauma life support
On arrival at the scene of the patient with suspected major trauma, paramedics are trained to perform an initial ‘DR-ABCDE’ evaluation which is similar to the approach that has been developed for physicians, namely consideration of dangers, response, airway, breathing, circulation, disability and exposure. Of particular importance in the pre-hospital trauma setting are dangers to paramedics from passing traffic, fallen electrical wires and fire from spillage of fuel.
The initial assessment of the airway and breathing includes the application of cervical immobilization in patients who have a mechanism of injury that suggests a risk of spinal column instability. Although decision instruments have been developed to identify patients in the emergency department who require radiographic imaging [6], the accuracy of these guidelines in the pre-hospital setting is uncertain. Spinal immobilization of many patients with minimal risk of spinal cord injury is uncomfortable and may lead to unnecessary radiographic studies [7]. Therefore, the recommendation to immobilize the neck in all cases of suspected spinal-column injury based on mechanism of injury alone is currently being challenged [8]. On the other hand, if spinal cord injury is suspected, patients should be transported with full spine immobilization [9].
Accurate triage of major trauma patients is an important component of trauma care in cities with designated major trauma centres. Triage tools based on vital signs, injuries and modifying factors, such as age, co-morbidities and mechanism of injury, are used [10]. Paramedic judgement may also have a role, although some injuries, such as occult intra-abdominal injuries, are difficult to detect on clinical grounds [11].
Advanced trauma life support
The role of ATLS by paramedics, particularly intubation of the trachea in comatose patients and intravenous cannulation for fluid therapy in hypotensive patients, is controversial. Although these interventions are routinely used in critically injured patients after hospital admission, studies to date indicate that the provision of ATLS provided by paramedics may not improve outcomes [5,12]. On the other hand, few studies conducted to date have been sufficiently rigorous to allow definitive conclusions and many were conducted in an urban setting with predominantly penetrating trauma rather than blunt trauma. Therefore, many ambulance services continue to authorize advanced airway management and intravenous fluid resuscitation in selected trauma patients, particularly those who are injured some distance from a trauma service.
Intubation
Following severe head injury, many unconscious patients have decreased oxygenation and ventilation during pre-hospital care and this secondary brain injury is associated with worse neurological outcome [13]. In addition, a depressed gag or cough reflex may lead to aspiration of vomit and this may cause a pneumonitis, which may be fatal or result in a prolonged stay in an intensive care unit. To prevent these complications of severe head injury, endotracheal intubation may be performed. This facilitates control of oxygen and carbon dioxide, provides airway protection and is routinely performed in patients with Glasgow coma score<9 following severe head injury after hospital arrival [14].
Most patients with severe head injury maintain a gag or cough reflex and successful intubation requires the use of drugs to facilitate laryngoscopy and placement of the endotracheal tube. The usual approach in the emergency department involves rapid sequence intubation (RSI), which is the administration of both a sedative drug and a rapidly acting muscle-relaxant, such as suxamethonium. It is unclear from the literature as to whether RSI should be performed pre-hospital by paramedics or, alternatively, be performed in an emergency department by appropriately trained physicians.
Pre-hospital RSI performed by paramedics has been reported in numerous studies as having a high success rate [15]. However, it is uncertain whether this procedure is associated with improved outcomes [16]. Recently, a prospective, randomized, trial in adult patients with severe traumatic brain injury reported that paramedic RSI increased the rate of favourable neurological outcome at 6 months when compared to intubation in the hospital by physicians [17]. On the other hand, this study also showed a relatively high incidence of cardiac arrest in the patients who underwent paramedic RSI. Therefore, some uncertainty remains as to the efficacy of this procedure.
Intravenous fluid
Intravenous fluid resuscitation has been shown to worsen outcome in patients with penetrating trauma and hypotension [18]. However, most major trauma in Australasia and Europe is blunt rather than penetrating and few patients require urgent surgical control of haemorrhage. Therefore, the issue of pre-hospital IV fluid for the treatment of hypotension remains the subject of debate.
Supporters of pre-hospital IV fluid therapy suggest that this treatment is intuitively beneficial and that any delay of this therapy increases the adverse effects of prolonged hypotension, which may result in end-organ ischaemia, leading to multiorgan system failure and increased morbidity and mortality. On the other hand, opponents of pre-hospital IV fluid therapy suggest that this therapy prior to surgical control in patients with uncontrolled bleeding increases blood loss due to increased blood pressure, dilution coagulopathy and hypothermia from large volumes of unwarmed IV fluid. Any additional blood loss would increase transfusion requirements and could be associated with increased morbidity and mortality.
There is no evidence from clinical trials for benefit of the administration of IV fluid to bleeding patients in the pre-hospital setting. A meta-analysis of the studies to date suggests that pre-hospital IV fluid does not improve outcomes [5]. Nevertheless, if intravenous fluid is given to patients with hypotension and severe head injury, crystalloid rather than colloid should be given, particularly in hypotensive patients with severe traumatic brain injury [19].
Analgesia
The administration of effective analgesia in the pre-hospital setting for traumatic pain remains a difficult issue for ambulance services. Many paramedics are not trained to administer IV therapy and treatment options are, therefore, limited to inhaled therapy.
Inhaled analgesic treatments include methoxyflurane and oxygen/nitrous oxide. However, while the former is reasonably effective [20], there are concerns with the administration of this agent in an enclosed space, such as the rear of an ambulance, because of the perceived risk of repeated exposures of these analgesics to the paramedics.
Alternatively, the training of paramedics in the insertion of an IV cannula and administration of small increments of IV morphine is increasingly regarded as a feasible alternative to inhalation analgesia. Alternative routes of narcotic administration, such as intranasal administration, are the subject of current studies. For example, the use of intranasal fentanyl has been shown to be equivalent to intravenous morphine [21].
An alternative analgesic agent for paramedic use is ketamine. Ketamine, in addition to morphine, has been shown to be superior to morphine alone for traumatic pain. In a randomized, controlled trial, adult patients with moderate to severe traumatic pain were randomized to receive either 5 mg of morphine followed by ketamine, or morphine alone [22]. Those who received morphine and ketamine reported a significant pain score reduction compared to those who received morphine alone. However, the rate of adverse effects, such as nausea and dysphoria, was higher following ketamine compared with morphine.
Cardiac care
Cardiac arrest
In 1966, external defibrillation was introduced into pre-hospital care and this led to the development of ‘mobile coronary care units’ in many countries for the delivery of advanced cardiac care for the patient with suspected myocardial ischaemia [23]. This approach was subsequently extended to rapid response for defibrillation of patients in cardiac arrest. Protocols for the management of pre-hospital cardiac arrest are based on the concept of the ‘chain of survival’, which includes an immediate call to the ambulance service, the initiation of bystander CPR, early defibrillation and advanced cardiac life support (intubation and drug therapy).
The patient in cardiac arrest represents the most time-critical patient attended by ambulance services. For the patient with ventricular fibrillation, each minute increase from time of collapse to defibrillation is associated with an increase in mortality of approximately 10%. However, most ambulance services have urban response times that average 8–9 minutes. Since there may be 2 minutes between collapse and dispatch and 1 minute between arrival at the scene to delivery of the first defibrillation, total time from collapse to defibrillation would usually be approximately 12 minutes. Therefore, current survival rates for witnessed cardiac arrest in urban areas are low [24] and there are even fewer survivors in rural areas [25].
The most effective strategy to improve outcomes would be to decrease ambulance response times. However, this would require very significant increases in ambulance resources and would be an expensive strategy in terms of cost per life saved. Alternatively, response times to cardiac arrest patients may be reduced with the use of co-response by first responders equipped with defibrillators. Such a first responder programme has been introduced in Melbourne, Australia with promising results [26].
The role of advanced cardiac life support (ACLS) during cardiac arrest remains controversial [27]. For example, in a randomized, controlled trial comparing a basic life-support approach with an advanced life-support approach, the rate of survival to hospital discharge was 10.5% for the ACLS group compared with 9.2% for the no ACLS group (P=0.61) [28]. This finding of a lack of efficacy of ACLS during cardiac arrest remained after adjustment for underlying differences between the groups in the rates of ventricular fibrillation, response interval, witnessed arrest or arrest in a public location.
Therapeutic hypothermia after resuscitation from cardiac arrest is used in many hospitals, particularly when the initial cardiac arrest rhythm is ventricular fibrillation. A number of clinical trials have tested whether therapeutic hypothermia should be initiated by paramedics after resuscitation using a bolus of cold IV fluid [29,30] or intranasal cooling [31]; however, the results of these studies do not currently support this therapy prior to hospital arrival.
Acute coronary syndromes
Most ambulance services have protocols for the management of the patient with chest pain where the cause is suspected as an acute coronary syndrome. These protocols usually include administration of aspirin and sublingual trinitrates followed by rapid transfer to an emergency department for definitive diagnosis and management. In addition, pain relief using intravenous morphine may be given by advanced life-support paramedics. The role of supplemental oxygen in patients with ST segment elevation myocardial ischaemia (STEMI) but without hypoxia remains uncertain [32].
While these interventions may decrease symptoms, more recent strategies to improve overall outcomes involve triage by paramedics of patients with STEMI using 12-lead electrocardiography to centres for interventional cardiology [33]. For patients with STEMI who are greater than 1 hour to a cardiac catheterization laboratory (i.e. rural patients), pre- hospital thrombolysis may be considered. In a recent European trial, patients with STEMI who presented within 3 hours after symptom onset but who were unable to undergo primary percutaneous coronary intervention (PCI) within 1 hour were assigned to undergo either primary PCI or fibrinolytic therapy [34]. The primary endpoint of death, shock, congestive heart failure or reinfarction occurred in 12.4% of patients in the pre-hospital fibrinolysis group and in 14.3% of patients in the primary PCI group (relative risk in the fibrinolysis group, 0.86; 95% confidence interval, 0.68 to 1.09; P=0.21). The rates of intracranial bleeding were similar in the two groups (after the dose of fibrinolysis was halved in the over 75 years patients). These data suggest that pre-hospital thrombolytic therapy is appropriate if there is a delay of greater than 1 hour in transport to a definitive centre for PCI.
Cardiac arrhythmias
Some patients with an acute coronary syndrome develop a cardiac arrhythmia during ambulance care. Pulseless ventricular tachycardia is treated with immediate defibrillation and amiodarone by slow IV infusion is recommended for ventricular tachycardia where a pulse is palpable and the patient is alert [35]. However, the pre-hospital drug treatment of supraventricular tachycardia is more controversial. While the use of verapamil or adenosine appears to be equivalent in efficacy [36], many ambulance services require the patient to be transported for 12-lead electrocardiography and management of the supraventricular tachyarrhythmia in an emergency department.
Pulmonary oedema
During myocardial ischaemia, the patient may develop pulmonary oedema and, in these patients, the use of oxygen and glyceryl trinitrates is regarded as useful [37]. Despite common use of non-invasive ventilation (NIV) in the emergency department for patients with acute pulmonarty oedema, pre-hospital continuous positive airway pressure for this indication has not been widely adopted, since the equipment is expensive and oxygen consumption is high. Nevertheless, there is some evidence that continuous positive airway pressure is feasible in the pre-hospital setting, may reduce the need for intubation and may reduce short-term morbidity [38].
Other medical emergencies
Stroke
Early identification and effective management of stroke aims to promote optimal recovery. The ambulance plays an important role in stroke management by triaging patients with suspected stroke to an appropriate hospital. Use of a validated stroke screen tool has been shown to increase diagnostic accuracy in identifying stoke and thus facilitate transfer to a stroke centre. There are a number of published stroke screening tools for paramedic use such as the Los Angeles Motor Score (LAMS) [39] and the Melbourne Ambulance Stroke Score [40] that have been shown to be effective in accurately identifying stroke. Patients suspected to be suffering from a stroke should be preferentially transported to a facility with stroke expertise.
Hypoglycaemia
The patient with hypoglycaemia due to relative excess of exogenous injected insulin will suffer neurological injury unless the blood glucose level is promptly corrected. Treatment of the conscious patient involves orally administered dextrose. For unconscious patients, intravenous 20% dextrose should be administered. For paramedics who are not trained to insert IV cannulae or where IV access is not possible, the administration of intramuscular glucagon is also effective, although this is associated with an increase in the time to full consciousness [41].
Patients who respond to treatment may refuse transport to hospital since they feel they have recovered. However, patients on oral hypoglycaemic agents may later develop recurrent hypoglycaemia [42]. Therefore, transport to hospital in this patient group is recommended.
Narcotic overdose
Patients who inject narcotic drugs may suffer coma and respiratory depression which is readily reversed by naloxone. However, the administration of IV naloxone by paramedics is somewhat problematic, since IV access may be difficult and the half-life of IV naloxone (approximately 20 minutes) may be shorter than the injected narcotic. If the patient awakens and leaves medical care, there may also be a recurrence of sedation. Therefore, many ambulance services administer naloxone via the intramuscular or subcutaneous route. While the absorption via this route may be slower, overall, the time to return of normal respirations is equivalent. To avoid the use of needles, naloxone may also be administered via the intranasal route and this has an equivalent onset time to intramuscular naloxone [43].
Anaphylaxis
Many patients with known severe anaphylaxis are prescribed adrenaline (epinephrine) by their physician for self-administration. The use of intramuscular adrenaline (epinephrine) by paramedics is a safe and effective pre-hospital therapy [44]. Generally, a dose of adrenaline 0.3 mg IM together with IV fluid therapy is recommended as first-line therapy for anaphylaxis with intravenous adrenaline reserved for patients who become severely hypotensive.
Seizures
Out-of-hospital status epilepticus is also regarded as a time-critical medical emergency. The first-line treatment of status epilepticus is usually a benzodiazepine. For many years, this was provided using the IV or rectal route of administration. More recently, there are supportive data that intramuscular midazolam is equally effective to intravenous benzodiazepine [45]. Many ambulance services therefore now authorize midazolam 0.1 mg/kg in the adult patient with seizure, with a half dose considered in older patients.
26.2 Retrieval
Marcus Kennedy
Retrieval systems
The definition of retrieval varies by jurisdiction, however, it includes the interhospital transfer of critical patients using specialized clinical staff, transport platforms and equipment. In most regions, this definition extends to the pre-hospital environment when medical staff crewing is deployed and, in this setting, is termed primary retrieval. In various systems, staff may include medical, nursing, advanced life support (ALS) paramedic or intensive care paramedic (or equivalents) in a range of combinations or crew-mix. Retrieval generally involves the transfer of patients with critical illness or life-threatening injury: situations where the patient requires the highest levels of clinical care and vigilance. Retrieved patients are often unstable, at the margin of physiological compensation and in need of specialized investigation and intervention. They are often at that phase of an emergency presentation where diagnosis is incomplete, treatment is problem-focused and risk is high. This setting therefore requires special expertise, risk-averse processes and fail-safe systems characterized by anticipation, redundancy, rapid response and reliability.
Retrieval is a coordinated process that provides specialized assessment and management, prior to and during transfer of critically ill patients from situations where resources or services are inadequate, to a destination where definitive care can be provided. It aims to deliver the same or higher level of clinical care as that available at the point of referral, thus ensuring that the patient is not exposed to any reduction in the quality of clinical care, despite the inherent risks of the transport environment.
The need for retrieval is related to the limitations of health facilities and the geography of populations. It is a reasonable premise that rural communities have a right to equitable and timely access to critical care medicine; however, it is recognized that there is often an urban/rural divide in regard to the accessibility of healthcare generally and to specialized critical care in particular. Key clinical ‘gap’ areas exist at both urban and rural and regional levels in regard to trauma, neurosurgery, cardiac and neonatal and paediatric critical care. Advances in medicine and technology are inevitably (at least initially) usually concentrated in major metropolitan centres, thus increasing the need for critical patient transport (e.g. coronary percutaneous procedures, interventional radiology, such as angio-embolization, major trauma centres and paediatric tertiary and quaternary care hospitals. Given that such divides exist and that critical-care transfer is inevitable, retrieval medicine aims to ensure quality of care in transfer in distinction to the somewhat ad hoc approach to irregular critical-care transfers that otherwise may be the case in less systematized approaches.
Retrieval systems are often a product of their geography and some services have evolved due to their unique environment. Examples include Nordic systems and alpine systems that have emerged from the demands of challenging altitude and temperature extremes, urban trauma service (such as HEMS London) and systems driven by the tyranny of distance, such as the Queensland retrieval system.
Retrieval systems vary by state and internationally. There are no uniform system designs or standards and, consequently, services vary in their use of transport platforms and crew types (nurse, paramedic, doctor). Staff may be employed by a health department, ambulance service, by contract with a private provider or a retrieval service may utilize hospital personnel. A state service may incorporate several retrieval service providers with central coordination; alternately, systems exist with local governance and responsibility at a district or area level. Transport platforms are generally state owned and operated or contracted; however, non-government-owned helicopters may be part of a state system (and have historically received both benevolent and state funding). In the past, such services were the mainstay of retrieval practice and were often initiated by passionate volunteers, being funded by community donations, corporate sponsorship and government grants. Governance systems for such services and their coordination and performance responsibilities were typically variable. Consequently, retrieval systems have evolved, leading to increased systematization and corporate and clinical governance, aiming at reduction in variation, greater accountability and increased reliability at the system level.
Most countries have progressively moved towards centralized state systems. These are characterized by central coordination centres that use nurses, paramedics and doctors who work together utilizing their complementary skills and experience. Neonatal, paediatric, perinatal and adult retrieval services may be integrated, co-located or separate; however, the trend of recent years is to co-locate these services with common governance, to allow synergies to be realized in regard to operational processes, infrastructure, management, education, research, response platforms and clinical staff.
Most retrieval services have developed similar systems for management of the generic operational processes of: patient referral, case coordination, response and logistics, clinical intervention, and destination determination (Table 26.2.1). In addition, these are usually supported by a formal array of governance elements (Table 26.2.2).
Table 26.2.1
Elements of operational management of retrieval services
Programme guidelines
Quality reporting
Reporting to Medical Standards Committee
Management guidelines
Data management
Organizational structure
Contracts and memoranda of understanding
Budget and financial system
Annual and strategic planning
Management and data reports
Table 26.2.2
Elements of clinical governance of retrieval services
Guidelines for coordinators
Guidelines for retrieval clinicians
Support staff guidelines
Equipment management systems
Orientation and training
Professional development
Clinical documentation
Case follow up and feedback
Case review and audit
Incident management
Indicator measurement
Credentialling
Performance management
In addition, states may legislate [1] or learned and academic bodies may publish guidelines and standards to promote safe systems of patient transfer, particularly in the critical-care sector [2].
Retrieval processes
Retrieval coordination
Case coordination is at the heart of all retrieval systems. As a process it commences with the initiation of contact from a referral site. It is important for referrers to understand the indications for retrieval and to have clear guidelines (both system and local) to encourage early referral and good decision making. Statewide trauma systems and neonatal paediatric care systems often have well established transfer criteria; however, processes for other clinical groups are often less developed and may be ad hoc. Mature retrieval systems act as a single point of entry for the referrer, preferably providing services by initiation of a single call to a system-wide phone number. Coordination staff are appropriately qualified senior clinicians, with specialized training and knowledge. Case coordination fundamentally answers: what are the needs of the referrer and their patient? Are the needs for clinical advice, for organization of transport and crew or for assistance in obtaining an appropriate destination for a critical patient? The coordinator must determine quickly and efficiently the planning and intervention priorities for each case. These may be for immediate care or advice, immediate response, destination planning or consideration of complex decisions involving logistics, crew or transport platforms. Coordinators need to display leadership while at all times taking a systems perspective and avoiding tunnel vision or task fixation.
Coordination must be provided through high performance organizations and, typically, utilizes sophisticated communication technologies, such as multiparty conference calls, telehealth videoconferencing, case recording and comprehensive data management systems.
Coordination of retrieval also implies an ongoing process of communication and feedback with the referrer of case progress, estimated response times and knowledge of patient status changes. During the response and transfer phase the coordination centre maintains communication with response teams, providing logistic support and mission oversight.
Transport platforms
Retrieval services generally use road, rotary wing (helicopter), or fixed wing aircraft response and transport platforms. For international retrieval missions, commercial larger jet transport is used and, in uncommon settings, aquatic transport platforms may be used. In consideration of platform selection for a mission, clinical factors must be factored first; these will include need for pressurization, need for space for specialized crew or equipment and patient size. Further to these factors, urgency (of response or return leg or both outbound and return components), distance to referral hospital, availability of helipads at referral and destination hospitals and need to minimize the out-of-hospital time for the patient. Heightened risk for patients in transit is experienced during platform transfers (from bed to trolley to ambulance to aircraft stretcher and so on) and, in general terms, in the out-of-hospital setting. Minimization of number of patient transfers and the out-of-hospital time for the critical care retrieval patient are important principles.
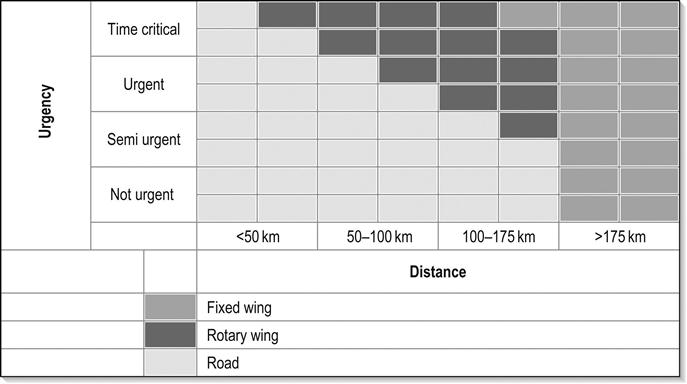
Road transport platforms should be specifically designed and fitted out for retrieval purposes to minimize variation (improving crew performance and safety) and the risk of ad hoc unsecured equipment placement. Use of helicopters (with crews of appropriate skill mix) in retrieval response has been demonstrated to improve patient outcomes [3,4], particularly patients with severe trauma and others with a need for time-critical interventions. In general, helicopter transfer is considered for retrieval of patients approximately 75–175 km from base, with road response used for shorter transfers and fixed wing for longer. These broad recommendations vary depending on road, geography and climatic conditions and on the performance characteristics and landing options for individual aircraft. Fixed wing transfers have the advantage of providing a (usually) pressurized aircraft, greater speed and comfort, more space and a controlled temperature. Rotary wing aircraft have advantages of door-to-door transfer where helipads exist at referral and destination sites, the primary response capability and the potential to avoid road transport legs, and multiple patient transfers. Road transfer offers spatial flexibility, door-to-door transfer and cost efficiency (Fig. 26.2.1).
Crew
Staff selected for roles in retrieval must meet required professional and personal standards. Critical-care capability is essential and medical staff specialist training in a critical-care specialty is desirable. Similarly, nursing and paramedic staff must be trained to intensive care practitioner level. In addition, all staff must have specific training in management of the retrieval environment, clinical care in transport settings and personal and crew behaviours.
The retrieval environment poses particular risk and technical training regarding platforms, procedures, relevant legislation, communication methods, rescue and escape procedures and equipment performance characteristics is needed. Training in clinical care during retrieval needs to ensure capability in management of the complete range of critical care, trauma and intensive care scenarios and an ability to apply depth of clinical knowledge to the relatively compact window of patient care that the retrieval mission represents. Practitioners need to understand in a retrieval setting that an intervention may be possible and ideal while also being inappropriate and inefficient or, that an intervention may be desirable but not be possible or practical. Compromise and pragmatism have a role in pre- and interhospital transfer particularly where priority exists for reaching a definitive care destination. Training in personal and crew behaviours is necessary to optimize the cohesiveness and functionality of the retrieval team – formal exposure to crisis resource management tools is a standard component of aeromedical and road-based retrieval education [5]. In interaction with referring practitioners and primary responders, the retrieval team needs to exhibit empathy, listening skills and professional behaviours – avoiding arrogance, premature conclusions or judgemental behaviour. The training and knowledge base required is significant, therefore training processes must be formalized and must be supported by ongoing professional development and regular credentialling in addition to compliance with relevant regulations.
Crew safety is paramount, so personal protective equipment and clothing which meets aviation and ambulance service standards is mandatory. Safety risk arises also in long and overnight missions and crewing must be adequate to allow sharing of clinical vigilance duties and patient interventions at times of fatigue and to allow for adequate breaks and rest.
Retrieval services play a major role in disaster response and management and generally provide a significant component of the early response to such incidents. Retrieval services and, in particular, their coordination processes are also key to the distribution and reception phase of the disaster response – providing system overview of capability and capacity of health services to receive victims. Retrieval staff must therefore be trained to expert status in this discipline [2,6].
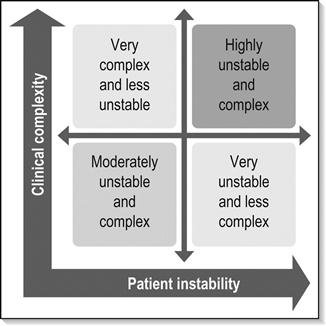
Skill sets
Retrieval medicine and primary response aeromedical settings provide the most challenging of all clinical environments and, therefore, choice of staff skill sets and professional team makeup is fundamental to optimizing clinical outcomes. The central tenets of this clinical environment are that a critical-care retrieval team must consist of (at least) two professionals [6]. They must be trained to critical-care standard and work within their core scope of practice. The skill set they provide must meet the clinical needs of the patient. In most national and international jurisdictions, blended medical practitioner and paramedic or nursing crews satisfy these tenets. Significant literature supports the role of medical practitioners in this environment due to the additional diagnostic capability, procedural range, extent of knowledge and depth of clinical understanding they contribute [7]. Such skills are complemented by the skill set of critical-care-trained nursing staff. Paramedic staff contribute substantial critical-care capability (depending on individual jurisdictional training levels) together with expertise in the transport and pre-hospital scene environments. Crews comprised of paramedic or nursing staff paired in various combinations and without a medical crew member are appropriate for lower risk critical-care transfers, or for non-critical-care retrieval. Skill set needs to match the requirements of the patient in the basic dimensions of clinical complexity and physiological stability; the more unstable and complex patient clearly requiring a higher skill mix in the retrieval team. In rare situations, and where life-saving intervention may be possible, the transport of highly specialized clinical staff to the patient may be appropriate and should be considered, for example, transporting a surgeon to perform an infield amputation on an entrapped patient (Fig. 26.2.2).
Equipment
Within a retrieval service, equipment should be standardized as far as possible. Response kits and platform layouts will then be familiar to all practitioners at all times, including at night and during uncontrolled clinical emergencies. Equipment must meet the needs of the patient population or therapeutic interventions and must consider the operating environment, mission duration, availability of electrical power in transport platforms, oxygen consumption and standard oxygen supplies available in vehicles. Stretchers and equipment bridges must meet aviation engineering standards, as must all electrical equipment that may be used in aircraft.
On all missions, the retrieval practitioner must have access to the complete range of airway management equipment including a difficult airway kit, cardiac monitor defibrillator pacer, multiple infusion pumps appropriate for inotrope infusions, a transport ventilator capable of complex respiratory support, invasive pressure monitoring, temperature monitoring, capnography and oximetry. All equipment must be maintained to the highest level of biomedical support and be fitted with appropriate auditory and visual alert systems. A comprehensive range of drugs is necessary to cover the spectrum of clinical presentations and scenarios encountered in the retrieval setting. These should be maintained in sealed drug kits, with attention paid to expiry dates and to temperature control where relevant. The retrievalist will also require access to antivenoms, thrombolytics, blood and blood products and other specialized agents at times – systems must be in place to ensure timely access to uncommonly used pharmacological agents.
Clinical principles in retrieval and pre-hospital medicine
Preparation for transport
In many cases, the referral of a patient for retrieval is an uncommon event that may occur at one site perhaps once or twice each month and which may involve individual staff members only once or twice per year. Therefore, clear understanding and communication of the needs of the critical-care patient for transfer must be in place. Common dilemmas are faced:
 Does the patient require intubation for transfer?
Does the patient require intubation for transfer?
 What IV access does the patient require? CVC? Arterial line?
What IV access does the patient require? CVC? Arterial line?
Airway management is perhaps the greatest risk in the critical-care retrieval setting. The need for intubation for transfer should be discussed between the retrieval coordinator, referring staff and the retrieval team. In general terms, the patient should be intubated if needed for respiratory failure or, if significantly aggressive, agitated or obtunded, or if their clinical condition makes it likely that they will deteriorate en route, e.g. large intracranial haemorrhage, complete cervical cord injury, or if they have threatened airway obstruction, e.g. burns, epiglottitis which would present a high risk in-transit intubation.
The general principles that should be applied systematically in the preparation of patients for retrieval are given in Box 26.2.1.
Monitoring
Monitoring equipment used in transport should be in accordance with recommended jurisdictional standards. Most patients require at least continuous ECG, pulse oximetry and blood pressure monitoring. In addition, capnography, invasive pressure monitoring, temperature, ventilation and other monitoring may be required. Equipment must be selected carefully and, where possible, be integrated. Sophisticated light, transport-specific, multimodal monitoring units are now available which include the above components plus defibrillation and external pacing capability. Display screens must be visible in daylight and battery life must be appropriate for duration of transport. Equipment alarms must be clearly visible as auditory alarms are difficult or impossible to hear in moving vehicles, especially aircraft. A major component of any monitoring system is the observer and, in the retrieval setting, the need for vigilance is paramount; at all times at least one of the retrieval crew members must be absolutely focused on the patient and monitors, continually scanning measured parameters and clinical status (including temperature, peripheral circulation, urine output, conscious state and respiratory oscillation).
Environmental impacts
Transport environments are usually confined and limited in space, which may present hazards for all staff, the patient and equipment. Care, deliberate planned actions and vigilance are important as is the need to ensure all equipment is secured (and equipment that is needed is accessible). Planned exercise, movement, nourishment, breaks and fatigue avoidance must be considered, depending on the mission characteristics. Aircraft retrieval presents particular challenges [8]. Altitude results in reduction in barometric pressure and associated reduction in partial pressure of oxygen and expansion of gas within enclosed spaces. Expansion of gas (such as in an undrained pneumothorax or in a distended bowel) may result in pain or significant worsening of underlying pathology. In a normal person with sea level SpO2 of 98% and without supplemental oxygen, SpO2 decreases to about 90% at 3000 m altitude (10 000 ft). Most passenger jet aircraft are routinely pressurized to around 8000 ft; however, some aeromedical platforms may be able to be pressurized to sea level, while some (including most helicopters) cannot be pressurized at all. In patients with respiratory and cardiac disease, impacts are felt at lower altitudes. During descent, trapped gas will occupy less space causing contraction of flexible tissues, such as membranes and mucosal surfaces – this may cause pain, for example when middle ear or sinus space pressures cannot be equalized with the rising external atmospheric pressure. Air transport of patients with decompression sickness requires particular planning and care, since the condition may be significantly worsened at altitude as gas solubility in blood decreases with altitude (due to reduced barometric pressure) and dissolved gas comes out of solution in the circulation, forming nitrogen bubbles with devastating consequences.
Other impacts of flight include those due to noise, vibration, humidity, gravity, acceleration and deceleration, third space effects (swelling) and fatigue.
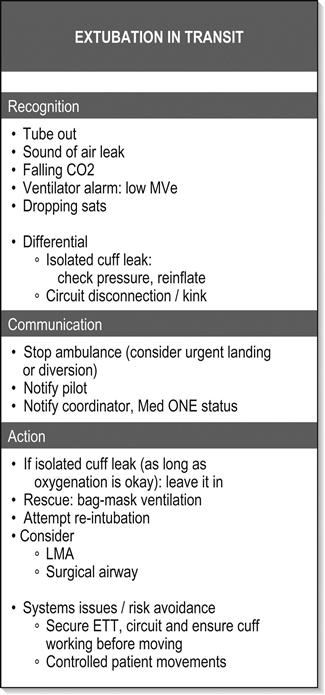
Critical incidents
It is likely that the most complex patients receiving the highest levels of support are also most likely to be exposed to in-transit critical incidents or equipment failure. A component of clinical practice in this setting is therefore the anticipation of such events, vigilance to detect them and rehearsed and standardized problem-solving algorithms to rectify them (Fig. 26.2.3). Examples include ventilator failure, unexpected hypoxia, high airway pressures, cardiac arrest in flight, etc. Such approaches are routine in the aviation industry, from which retrieval and pre-hospital medicine draws much at a cultural level, and have been applied commonly in anaesthesia [9].
Respiratory support
Provision of appropriate oxygen therapy via correct delivery systems will be required for most retrieval patients. Oxygen supplies vary on different patient transport platforms and these must be checked prior to transport. Assisted ventilation is a frequent intervention in critical-care retrieval and must be approached with discipline. A reliable and capable transport ventilator will provide suitable ventilation mode options including intermittent positive pressure ventilation (IPPV), synchronized intermittent mandatory ventilation (SIMV) and pressure support. Non-invasive ventilation (NIV) methods are not commonly utilized in air transport; however, may be valuable in road transfer and in retrieval of patients in whom intubation and assisted ventilation may be undesirable or contraindicated or in patients for whom short-term assisted ventilation is indicated. Ventilators are almost universally power dependent so back-up ventilation systems (manual self-inflating bag/valve system) must be available at all times in the patient cabin to allow management of power, gas or mechanical failure.
Circulatory support and infusions
Intravenous infusions are best delivered using simple and compact syringe drivers. These are available in various sizes and configurations, including banks of multiple syringes. Each retrieval service and, preferably the jurisdiction in which it operates, should maintain standard infusion protocols for preparation, labelling and administration of therapeutic agents and, in particular, inotropes. Use of syringe systems that have error reducing software and programs integrated in them reduces risk of adverse events and patient harm. The retrieval environment is dynamic and attention must be paid to maintenance of infusion rates during transfer and power interruption. Critical patients are often highly dependent on inotropic support and brief periods of interruption of infusions may be associated with catastrophic circulatory collapse. Adequate fluid volumes and spare syringes which are pre-prepared for longer transfers must be planned for, as must the availability of blood and blood products which may need significant coordination.
Infectious risk
The proximity of the retrieval environment means that patients with infectious diseases may present hazards to medical crew, flight crew including pilots and other patients or passengers. Clearly, the application of universal precautions against infectious diseases is applicable as in all clinical settings; however, other measures may be important, such as use of ventilator expiratory filters, avoidance of use of nebulizers which may, for instance, aerosolize influenza, use of prophylactic medications, such as rifampicin, after prolonged exposure to meningococcal disease, barrier precautions in patients with vancomycin-resistant enterococci (VRE) and so on.
Highly-specialized retrieval
Neonatal, obstetric and paediatric specialized retrieval systems have been a part of many health systems for decades. While the clinical demands of these systems require particular sets of knowledge, the retrieval frameworks required are complementary and intersect with the larger and higher volume world of adult retrieval and pre-hospital care. Consequently, blending, collocating or integrating retrieval services is seen as a sustainable model and has become more common. Technical advances in critical care, such as increased use of extracorporeal membrane oxygenation (ECMO) support in severe respiratory failure for example in influenza, have promoted the development of specialized retrieval systems to manage these highly fragile patients [10]. Interestingly, in response to these needs, technology has evolved rapidly to offer lighter, smaller, less invasive and simpler ECMO systems.
26.3 Medical issues in disasters
Richard J Brennan, David A Bradt and Jonathan Abrahams
Introduction
Disaster management involves a complex, multidisciplinary process of which emergency medicine comprises one component. Domestically, fire fighters, law enforcement, ambulance services, civil defence, State Emergency Services, Red Cross national society, defence forces and other aid organizations commonly play major roles. Internationally, governmental and non-governmental organizations, International Federation of the Red Cross and Red Crescent Societies and United Nations agencies are frequently involved. The health and medical management of disasters can also cut across healthcare disciplines, requiring contributions from emergency medicine, public health, primary care, surgery, anaesthetics and intensive care.
From the health perspective, certain types of disasters are usually associated with well-described patterns of morbidity and mortality. The clinical and public health needs of an affected community therefore also vary according to the type and extent of disaster. Emergency physicians should understand the public health and medical consequences of the various types of disasters in order to determine their own roles in preparedness and response. In practice, emergency physicians are most actively involved in the response to an acute-onset disaster that involves multiple casualties, such as a transportation incident. Several other types of disasters, including floods and cyclones, are generally associated with few, if any, casualties. The health and medical needs in these settings usually involve augmenting public health and primary care services.
Emergency physicians should be familiar with disaster epidemiology and disaster management arrangements and understand the medical response to a disaster involving multiple casualties.
The differential effects of disasters on communities in all countries are associated with risk factors which make some communities and subpopulations more vulnerable and less capable of dealing with the risks than others. Apart from health and medical issues, the impact of disasters is often widespread and long term. Disasters can cause significant social, economic and environmental losses that may have devastating effects on the general well-being of the affected community. They may set back years of development progress in poorer countries, including disruption of health systems, such as the Pakistan floods of 2010. Their effects may be felt well beyond the borders of the first affected country. Epidemics, for example, may be prone to widespread international spread, with a broad range economic and sociopolitical consequences, for example, the H1N1 pandemic of 2009.
Definitions and classification
There is no internationally agreed definition of disaster or disaster classification. There are increasingly consistent uses of disaster terms among stakeholder organizations. Common to most definitions is the concept that, following a disaster, the capacity of the impacted community to respond is exceeded and there is, therefore, a need for external assistance.
The United Nations Office for Disaster Risk Reduction (UNISDR), defines a disaster as: ‘a serious disruption of the functioning of a community or a society causing widespread human, material, economic or environmental losses which exceed the ability of the affected community or society to cope using its own resources’ [1]. This definition is also one of several recognized by the World Health Organization (WHO).
The Australian Emergency Management Glossary defines disaster as: ‘a serious disruption to community life which threatens or causes death or injury in that community and/or damage to property which is beyond the day-to-day capacity of the prescribed statutory authorities and which requires special mobilization and organization of resources other than those normally available to those authorities’ [2].
The Center for Research on the Epidemiology of Disasters (CRED), which compiles the data behind the annual World Disasters Report of the International Federation of Red Cross and Red Crescent Societies, stipulates a quantitative surveillance definition involving one of the following: 10 or more people killed; 100 or more people affected; declaration of state of emergency; or an appeal for international assistance [3].
Disaster risk management is the range of activities designed to establish and maintain control over disaster and emergency situations and to provide a framework for helping at-risk populations avoid or recover from the impact of a disaster. It addresses a much broader array of issues than health alone, including a multisectoral approach to hazard identification, vulnerability analysis, risk assessment, risk evaluation and risk treatments [4].
Disaster medicine can be defined as the study and application of clinical care, public health, mental health and disaster management to the prevention, preparedness, response and recovery from the health problems arising from disasters [5]. This must be achieved in cooperation with other agencies and disciplines involved in comprehensive disaster management. In practice, emergency medicine and public health are the two specialties most intimately involved in disaster medicine.
A mass casualty incident is an event causing illness or injury among multiple patients simultaneously through a similar mechanism, such as a major vehicular crash, structural collapse, explosion or exposure to a hazardous material. A complex disaster is a disaster complicated by civil conflict, government instability, macroeconomic collapse, population migration and an elusive political solution.
Disasters are commonly classified as natural versus technological/human-generated (Box 26.3.1) [3]. Disasters may also be classified according to other characteristics, including sudden versus slow onset, short versus long duration, unifocal versus multifocal distribution and primary versus secondary. Classifications of disaster magnitude exist for selected natural hazards, such as earthquakes and hurricanes/cyclones; however, there is currently no standard classification of severity of disaster impact.
Epidemiology
Globally, the types of disasters associated with the greatest numbers of deaths are complex emergencies (CEs). These are crises characterized by political instability, armed conflict, large population displacements, food shortages and collapse of public health infrastructure. Because of insecurity and poor access to the affected population, aggregate epidemiological data for CEs are somewhat limited. However, between 1998 and 2007 in the Democratic Republic of Congo, it is estimated that 5.4 million people lost their lives due to the consequences of the major humanitarian crisis afflicting that country [6]. This was four times the UNISDR estimate of deaths globally due to natural and technological disasters during the 20 years between 1992 and 2012.
According to information compiled by the International Federation of the Red Cross, there has been a significant increase in the total number of natural and technological disasters worldwide during the past 50 years. From 1960 to 2010, the annual number of disasters rose from 50 per year to approximately 700 per year peaking at 810 in 2005. While the total number of people killed by natural and technological disasters is currently approximately 150 000 per year, there is a wide annual range (17 660 in 2009 to 304 476 in 2010 due to the Haiti earthquake and the Russian heatwave). Moreover, the total number affected has almost quadrupled over the past three decades. It is estimated that approximately 200 million people are directly affected on an annual basis. Selected data are presented in Figures 26.3.1 and 26.3.2[3].
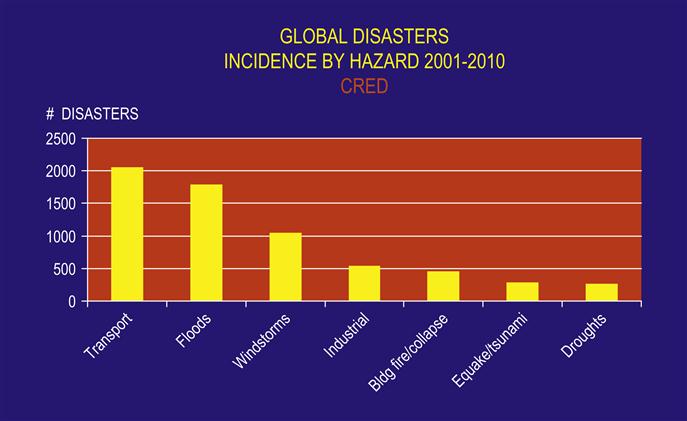
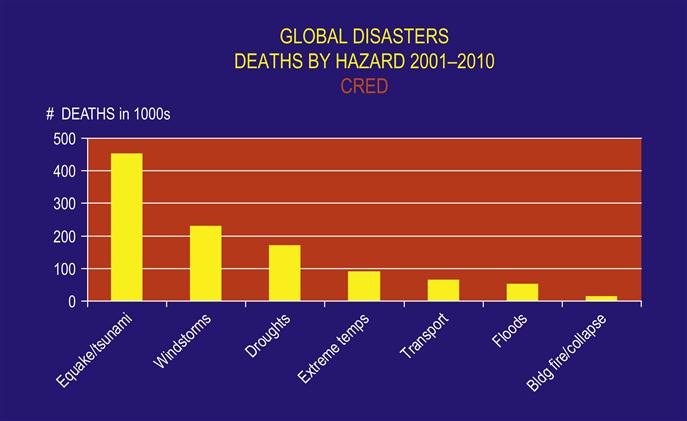
The commonest types of disasters across the globe are: transportation incidents, floods, windstorms, industrial incidents, building collapses, droughts, and earthquakes/tsunamis (see Fig. 26.3.1). Asia is the region of the world most prone to natural and technological disasters, recording 41% of such incidents between 2001 and 2010. It is followed by Africa (24%), the Americas (19%), Europe (14%) and Oceania (2%). Compared with other regions of the world, Australasia and Oceania have a relatively low incidence of disasters. Nonetheless, the World Risk Index (WRI) Report of 2012 included Vanuatu, Tonga and the Solomon Islands among the 10 countries most at risk to natural hazards [7].
Over the past 10 years, the commonest causes of disasters in Australia have been severe storms, including hail, transportation events and bushfires. Historically, the leading cause of death from natural disasters in Australia have been heatwaves (438 killed in 1939, 404 killed in 2009), followed by cyclone and bushfire. Human-generated disasters resulting in multiple casualties have occurred more frequently in Australia in recent years. The commonest causes of mass casualty incidents have been bus crashes, structural fires, mining incidents, aviation incidents and train crashes.
The impact of disasters has been less in New Zealand, where only 75 lives were lost among 307 000 persons affected over the period 2001–2010. However, 2011 brought the Christchurch earthquake with 185 deaths surpassing the death toll of the previous decade. The incidence of disasters also differs, with the commonest major events being transportation disasters, industrial disasters and earthquakes. Data reporting on the incidence of armed conflict is complicated by varying and changing definitions and political motivations of the reporting agencies. The Uppsala Conflict Database Program identified 37 on-going conflicts on five continents in 2011 [8].
The regions recording the highest number of terrorist attacks over the past decade have been Afghanistan and Iraq. Excluding those countries, the number of terrorist attacks worldwide resulting in the death of at least 10 persons, has ranged between 193 and 353 events per year [9]. Overall, this is just a very small fraction of the total number deaths attributed to natural and technological disasters and complex emergencies.
Disaster epidemiology globally, including the Australasian region, is being affected by climate change. Global warming has already been associated with an increase in the frequency, severity, and unpredictability of weather-related disasters, such as heatwaves, floods and droughts. Rising temperatures have been implicated in the spread of infectious disease, such as malaria and dengue, through increases in vector populations, such as mosquitoes. Other important diseases are also sensitive to changing temperatures and rainfall, including malnutrition and diarrhoea. The health-related and other impacts of climate change will not be evenly distributed. Disasters associated with global warming are particularly likely to threaten the lives and livelihoods of coastal communities, those living in low-lying islands (e.g. due to rising sea levels) and in arid and high mountain zones.
Socioeconomic impact
Disasters have the potential for major socioeconomic impact of direct damages plus economic losses, costing the host countries and international community billions of dollars annually. In developing countries, years of development work and investment can be devastated by a single disaster. During the decade 2000–2010, disasters caused a global average of approximately $US107 billion damage per year. Windstorms were the costliest disaster over the decade accounting for 49% of disaster-associated costs led by Hurricane Katrina with over $200 billion in damage. Terrorist attacks on major financial centres, such as the World Trade Center in New York, have demonstrated the potential for tens of billions of direct economic impact, enormous social consequences and political repercussions. These figures may be overshadowed by pandemic disease, such as from avian influenza, for which economic cost estimates range to upwards of $US1 trillion [10].
In Australia over the past 30 years, floods, storms, then cyclones have caused the greatest disaster-related economic losses with an average of approximately $AUS1 billion annually. The most economically costly disaster was the 2010–2011 Queensland floods exceeding $A7 billion in damages and losses.
Economic estimates, of course, are unable to reflect the true scale of human suffering associated with disasters. While we can often document the mortality, morbidity and financial losses associated with disasters, it is impossible to quantify the associated personal, psychological, social, cultural and political losses.
Disaster management/emergency management
As emergency physicians play a vital role in the medical aspects of disaster management, they should be familiar with the underlying concepts on which these arrangements are based [11].
Integrated approach
The basis for the Australian system for managing disasters is a partnership between the Commonwealth, State/Territory local governments, the private sector and the community. Under legislation, State and Territory governments have the primary responsibility for coordinating disaster-management activities and maintain government and statutory agencies that provide emergency services to the community. Local governments play an active role in risk assessments, land-use planning, public education and awareness, local emergency planning and providing local resources in emergency relief and recovery. The major roles of the Australian Federal Government are to support State and Territory governments in coordinating national strategic policy, to assist with disaster information and knowledge management (e.g. meteorological and geological data to support risk assessments and early warnings), to provide financial resources on a cost-sharing basis with States and Territories and to provide operational support in the event that a disaster exceeds the affected State or Territory’s response capability [12]. Federal assistance in the area of health would most likely be medical resources provided by the Australian Defence Force (ADF). The ADF also has special expertise in the management of incidents involving chemical and biological agents.
Comprehensive approach
The comprehensive approach to disaster management encompasses prevention, preparedness, response and recovery. The traditional view is that health and medical professionals contribute most significantly to disaster preparedness and response. A broader appreciation of the factors that enable communities to be more disaster resilient would further recognize the role of the health sector in prevention and mitigation – specifically, by improving overall health, immunization rates and nutritional status of individuals, as measures to reduce vulnerabilities and strengthen resilience. The disaster equivalent of primary prevention activities includes regulatory and physical measures that prevent or mitigate the effects of hazards and to reduce community exposure to these hazards. Preparedness involves arrangements to ensure that resources and services that may be needed can be rapidly mobilized and deployed. Response activities are those actions taken during and immediately after impact to ensure that the disaster’s effects are minimized. Recovery involves strategies and services that support affected communities in reconstructing their physical infrastructure and restoration of their social, economic, physical and emotional well-being.
All-hazards approach
Different types of disasters can cause similar problems. Therefore, disaster management plans are based on a core set of arrangements and measures that can be applied to all hazards. Many risks, however, including acts of terrorism, also require specific prevention, preparedness, response and recovery measures.
The prepared community
The prepared community is the foundation of Australia’s disaster management arrangements. Local governments, voluntary organizations and individuals all play a critical role in this area. Individuals can reduce their own risks by being aware of the local hazards and taking appropriate precautions. Experience has demonstrated that individual and community self-help can often provide the most immediate, decisive and effective relief following a disaster, as it cannot be assumed that assistance from external sources always arrives promptly, particularly in remote area communities.
Risk management
From 1996, following the endorsement of the National Emergency Management Committee, the principles and processes of the joint Australian and New Zealand Standard for Risk Management have been adopted by the Australian emergency management community. The risk management methodology embraces the key approaches identified above and ensures a greater focus on reducing vulnerability of communities, as well as hazard prevention, emergency response and recovery measures [13].
Disaster resilience
Against the background of disasters, climate change and a myriad of social, economic and environmental factors, the Council of Australian Governments adopted the National Strategy for Disaster Resilience in 2011. The Strategy emphasizes the shared responsibility of individuals, households, community organizations, businesses and governments to enhance Australia’s capacity to prepare for, withstand and recover from disasters. According to the Strategy, a disaster-resilient community has the characteristics of: functioning well while under stress, successful adaptation, self-reliance and social capacity. The Strategy provides high-level direction and guidance on how to achieve disaster-resilient communities through a long-term commitment to a broad range of measures including understanding risks, communicating and educating about risks, reducing risks and supporting capacities for resilience [14].
Disaster response planning
Disaster response planning is the process by which a community develops a comprehensive strategy effectively to manage and respond to disasters. It is a collaborative effort that requires cooperation among government agencies, community services and private organizations. The objectives of the planning process include identification of the main hazards facing the community; clarification of the capabilities, roles and responsibilities of responding agencies; and the strengthening of emergency networks. Other operational issues, such as emergency communications and public warning systems, should also be addressed.
All-hazards planning for response and recovery remains fundamental to disaster preparedness. To that end, disaster experience to date reveals a generic set of issues that disaster planners must address in the management of any hazard. These include risk assessment, incident management, on-scene and overall disaster command, control and coordination, relief operations, risk communication and media management, reconstruction, and community recovery. By contrast, the nature of the hazard imposes specific implications for epidemiology, search and rescue, medical care and consequences of contamination and communicable diseases. To this end, governments have elaborated all hazards disaster response planning including hazard-specific disaster subplans (e.g. mass casualty management for burns).
Finally, the circumstances of time, place, climate, geography, politics and security are unique for each disaster and challenge disaster planners to anticipate the issues arising from those specific circumstances.
Several high-profile terrorist events (e.g. World Trade Center attack in New York City) and important gatherings (e.g. London Olympic Games) have highlighted the need for specific planning for terrorist events. Such planning frequently involves collaboration with relevant military, security and intelligence agencies and a consideration of the tactics used by terrorists. The majority of terrorist attacks have employed conventional weapons, including explosives and small arms. Other terrorist tactics include assassinations, hijacking and kidnapping. Unconventional attacks, including those using jet airliners as weapons of mass destruction, or chemical, biological and radiological weapons have constituted only a tiny fraction of international terrorist attacks.
Disaster exercises must be conducted regularly to test the response and recovery aspects of the plan. Exercises range from desktop simulations to realistic scenarios with moulaged patients in the field. If conducted appropriately, they demonstrate strengths and weaknesses of the plan and highlight any need for an updating of response procedures. They are also considered to provide the most practice-based form of disaster response training. Disaster planning is a continuous process and plans need to be regularly reviewed and updated.
Planning and responding for international disasters has become more relevant for Australasian health professionals in light of the terrorist attacks in Bali (2002 and 2005), the Indian Ocean tsunami (2004), the earthquake in Pakistan and India (2005) and the Pakistan floods (2010), including through the deployment of Australian medical response teams (AusMATs) [15]. Such planning and response can be advised by the internationally-recognized Sphere Minimum Standards in Disaster Response [16] and in collaboration with important international agencies, such as the United Nation’s Office for Coordination of Humanitarian Affairs. Sphere specifies standards in six sectors of disaster response: water and sanitation, food security, food aid, nutrition, shelter and health services. These standards are relevant for all disasters and represent an extremely useful reference to guide planning and response for domestic incidents as well.
A major reform of the international humanitarian system was initiated at the end of 2011 under the leadership of the UN’s Office for Coordination of Humanitarian Assistance (OCHA) and involving all major relief agencies through the UN’s Inter-agency Standing Committee (IASC). This reform process, known as the IASC Transformative Agenda, includes a broad range of policy and procedural measures to improve the leadership, coordination, predictability and effectiveness of international disaster response. It also aims to increase the accountability of responding agencies, especially to the affected populations.
Domestic disaster response activities
Disaster management is increasingly seen as a cardinal sign of good governance in civil society. Healthcare systems have become mandated to undertake a range of health emergency and disaster risk management actions, with a focus on disaster preparedness, including disaster planning, training and exercises and response. Specific to emergency medicine, mass casualty management is the subject of well-developed training packages, such as Emergotrain, Major Incident Medical Management and Support (MIMMS), Basic Disaster Life Support (BDLS) and Advanced Disaster Life Support (ADLS).
Incident management
Scene assessment and stabilization
The initial scene assessment is conducted by first responders, such as police, fire or ambulance personnel. It is important for the first medical responder, generally an ambulance officer, rapidly to report findings to the Ambulance Communications Centre. An accurate, timely assessment is critical to initiating an appropriate and effective response. Key information that should be relayed from the scene includes the nature and magnitude of the disaster, the presence of ongoing hazards, the estimated number of deaths and injuries, the need for further assistance and the most appropriate routes of access to the scene. In large-scale disasters that affect entire populations, such as cyclone or earthquake, a rapid multisectoral assessment followed by broader epidemiological assessments is required, including an evaluation of the impact on the health infrastructure, health services, public utilities and shelter.
Site security and safety procedures must be observed to ensure that rescuers and bystanders do not become victims. This is particularly relevant in chemical and radiological incidents or when a terrorist incident is suspected, because of the threats posed by a secondary attack on responders or the potential use of weapons of mass destruction. The police should establish a perimeter around the scene of a multiple casualty incident and allow access only to authorized personnel. If a hazardous material is involved, rescuers may be required to wear specialized personal protective equipment (PPE) to protect their airways, eyes and skin. Electrical hazards, fires, explosions, leaking gases and unstable structures may all pose significant threats to rescue personnel. These hazards must be eliminated or controlled prior to initiating rescue operations.
Hazard-specific issues
While the all-hazards approach remains fundamental to disaster management, a unifying approach for undifferentiated hazards has been developed for the management of incidents involving chemical, biological or radiological agents. Basic principles of awareness include: recognition of potential terrorist events; avoidance of the affected area; isolation of the affected area; and notification of proper authorities. Basic principles for first responders include the four don’ts: don’t become a victim, don’t rush in, don’t TEST (taste, eat, smell, touch) anything, and don’t assume anything. Only properly trained and equipped hazardous material personnel should be in contaminated areas.
Site arrangements
Regardless of the nature of the incident, a Forward Command Post should be set up at or near the disaster site at the beginning of the emergency operation. The Command Post has representatives from the major responding services and reports back to the regional or State Emergency Operations Centre. The function of the Command Post is to coordinate the activities of the various services during the rescue operations. It also provides a central point for the submission of requests for assistance by each of the responding services. Medical and ambulance commanders are located at the Command Post to direct and coordinate medical care to victims at the scene, patient transportation, hospital communications, provision of medical supplies and medical air operations.
Communications
Good communications are vital to ensure appropriate command, control and coordination during a disaster. Communication problems are often cited as a major cause of suboptimal disaster response. There are many factors that may contribute to poor communications at the scene. Damaged equipment and overloaded telephone systems indicate the need for back-up systems, including reserved cellular phone lines. The use of different radio frequencies by different agencies may lead to poor coordination and an inability to communicate vital information. Compatible frequencies need to be identified and utilized. Megaphones may be required to overcome noise at the scene due to heavy extrication equipment, helicopters and general rescue activities. Information overload may also hamper the rescue effort. Radio and telephone reports should be kept brief, relevant and succinct. Professional jargon is frequently misunderstood or misinterpreted by other agencies and is best avoided.
Hospitals must also have reliable communications systems. Designated phone lines, cellular phones and back-up radio networks may augment the existing system during a disaster. It is essential for hospitals to remain in regular contact with the incident medical director, to provide information regarding medical capabilities, bed capacity and bed availability.
Medical management
Personnel
Provider roles in disasters continue to evolve. Dedicated disaster medical response teams have been extensively studied [17]. These teams form an integral part of national response plans in many developed countries notwithstanding lack of data attesting to any reduction in disaster-associated mortality associated with their deployments [18]. At international level, standards and procedures for foreign medical teams are currently being developed, after the poor experiences with many clinical teams following the Haiti earthquake in 2010.
Emergency responders generally respond best when their disaster roles are similar to their daily professional practice. Medical and nursing personnel are best suited to staffing emergency rooms and hospitals, where they have the advantage of working in a familiar, more stable environment. Ambulance personnel have more experience in pre-hospital settings and are usually responsible for conducting the initial on-site medical assessment and triage. In situations where there are multiple casualties, it may be appropriate to send a hospital team to the scene of a disaster, where their main functions are to perform primary and secondary triage and to provide medical care at the Patient Treatment Post. The science and practice of disaster medicine has progressed substantially. Therefore, only doctors and nurses specifically trained to work in the field environment and familiar with the relevant best practices and standards should be deployed to the disaster scene, as inexperienced personnel may well hinder the medical response.
Pre-hospital mass casualty management
Disaster epidemiology has refined the expectations of casualty flow plans. Current epidemiological evidence indicates that 50–80% of people acutely injured in a mass casualty disaster arrive at the closest medical facilities generally within 90 minutes after the event [19]. Moreover, the vast majority of disaster- affected patients self-evacuate without benefit of pre-hospital triage, transport or decontamination. A casualty-flow plan remains crucial to optimize patient care and transportation of those remaining at the scene.
A Casualty Collection Area should be established at a site that is close enough to the disaster scene to allow easy access, but far enough away to ensure protection from potential hazards. Patients are assembled and triaged here prior to transfer to a nearby Patient Treatment Post, where they are once again triaged and basic medical care provided. An Ambulance Loading Point and Ambulance Holding Point also need to be clearly marked so that patient transportation is conducted efficiently and to ensure that scene convergence and congestion is minimized. Landing zones for helicopters are established away from the incident site for safety reasons, to limit noise and to reduce down-wash from rotor blades. A temporary morgue may need to be established in a nearby area when many fatalities have occurred.
Triage
The aim of triage is to allocate medical resources, including personnel, supplies and facilities, in a manner that provides the greatest good to the greatest number of patients. The emphasis is not on providing optimal care to each individual patient, but rather on directing limited medical resources to those who are most likely to benefit. Triage is the single most important medical activity at the disaster site. It is a dynamic, ongoing process that occurs at every stage of patient management, from the disaster site, to the Casualty Collection Area, Patient Treatment Post and again at the hospital. Patients are rapidly assessed and categorized according to priority of treatment and transport. The condition of patients frequently changes and repeated examinations are required so that patients may be moved up or down in the order of priority. Triage is a learned skill and should be conducted by the most experienced medical or ambulance officer at the scene.
Different triage systems have emerged in different parts of the world. In British and Australasian health systems, ‘sieve and sort’ triage processes have become the preferred approach through MIMMS training courses [20]. In North America, ‘start and save’ triage processes have become incorporated into the National Disaster Medical System [21]. More recently, a National Disaster Life Support Consortium in the USA has promulgated a triage approach based on ‘move, assess, sort and send’ [22]. These different systems rely on different assessment approaches with different vital sign thresholds to assign triage priority.
In general, most systems recognize that there are categories of patients who require immediate care, delayed care, minimal care and those that are expectant or unsalvageable. Patients requiring immediate care are individuals in critical condition, but to whom simple life-saving procedures may be successfully applied, such as the manual clearing of the airway. Patients classified as requiring delayed care may have significant injuries, such as major fractures, but are likely to survive if treatment is postponed for several hours. Minimal care patients are generally ambulatory and their treatment may be delayed until other patients have been appropriately treated. Expectant or unsalvageable patients are those that have acutely life-threatening injuries requiring advanced resuscitation, or those that have non-survivable injuries, such as massive head trauma. Advanced life support measures, such as cardiopulmonary resuscitation, are rarely indicated at a scene with multiple casualties. Instead, these patients generally receive palliative care, but only after patients in the immediate category have received appropriate treatment.
Stabilization
Following triage of the affected patients, rapid stabilization of airway, breathing and circulation is provided to those with the greatest potential for survival. Definitive care is not generally provided at the scene. On-scene medical care concentrates on securing the airway, administration of oxygen, external pressure to control haemorrhage and insertion of intravenous catheters for volume expansion prior to hospital transportation. Medical care should generally be provided at the Patient Treatment Post but, during prolonged rescues, resuscitative procedures may be required prior to extrication. Appropriate use of analgesia, including parenteral narcotics and regional nerve blocks, may assist with the extrication of trapped individuals. Special on-scene procedures are sometimes required for those with crush injury, blast injury, burns or hypothermia. Amputation of a mangled limb, although rarely indicated, may be a life-saving procedure for an entrapped patient.
Decontamination
Chemical, biological, radiological and nuclear (CBRN) agents have the potential to contaminate individuals, property and the general environment. In practice, industrial accidents represent by far the most common cause of exposure to hazardous materials that may require decontamination. A small number of high-profile chemical–biological terrorist incidents over the past 20 years have also prompted medical as well as lay attention to this potential threat. Regardless of the cause, the principles guiding the process of decontamination remain consistent.
Decontamination is the process of removing or neutralizing a hazard from the victim or environment. Detailed management protocols exist for these hazards [23–25]. Fundamental principles involve:
 staff and site preparation with establishment of hot/warm/cold zones
staff and site preparation with establishment of hot/warm/cold zones
 casualty, staff and crowd protection
casualty, staff and crowd protection
 clinical treatment of contaminated patients and transport to definitive care
clinical treatment of contaminated patients and transport to definitive care
Removal of contaminated clothes should be conducted as a matter of urgency. Rapid decontamination of the skin is especially necessary following exposure to the liquid or aerosolized form of an agent. It is most useful when conducted within 1 minute of exposure but, in practice, this is rarely possible. When indicated, decontamination should be conducted close to the scene (i.e. in the ‘warm zone’) and, ideally, prior to transportation. Commonly used agents for decontamination include soap and water and hypochlorite (household bleach) in concentrations of 0.5–2.0%. Steps must be taken to ensure that emergency responders, health personnel and other patients are not at risk of secondary exposure to the chemical agent. Decontamination after exposure to a biological agent is less important, as most biological agents are not dermally active. But decontamination may be an effective way to limit the spread of the agent from potential secondary aerosolization.
Transportation
Efficient and rational transportation of patients to appropriate health facilities is dependent on good communications between hospitals and the incident Transport Officer. Capabilities of the affected community’s hospitals should be identified and documented in the regional disaster plan. Hospitals are required regularly to update the Incident Commander and Transport Officer of their bed availability status. The closest hospitals may be flooded by ‘walking wounded’ who have made their own way from the scene and by victims transported by well-meaning civilians. This has the potential of overwhelming local emergency departments and the Transport Officer must take this into consideration when determining the appropriate distribution of patients. It is essential that the disaster scene not be relocated to the nearest hospitals.
A number of factors need to be considered when determining the most appropriate hospital for a particular patient, including the patient’s triage category, the hospital’s capabilities (e.g. trauma, burns), transportation times, distance from the scene and the available transportation modalities. Medical helicopters may be able to transport patients to more distant hospitals, to relieve pressure on nearby facilities.
Health facility management
Guidance on hospital planning for disaster management has become widely available from the World Health Organization [26] as well as domestic stakeholders [27]. Emergency physicians are expected to be familiar with their own hospital disaster plan and have contributed significantly to its development. The plan should address both internal and external disasters. Surge strategies for hospitals and emergency departments have become well elaborated [28].
The emergency department needs to be cleared of non-critical patients and steps taken to expedite appropriate discharge of stable ward patients, so that bed capacity may be optimized. The emergency department should be well stocked with supplies and have arrangements with suppliers for rapid replenishment. A recall system for additional medical and nursing staff mobilized in a disaster needs to be incorporated into the plan. Extra security staff should be on standby to assist with the management of patients, families, friends, onlookers and the media.
Patients require re-triage by a senior medical officer as they arrive at the emergency department. Those with acutely life-threatening injuries are immediately resuscitated. Less severely injured patients need to be regularly reviewed while awaiting definitive care, to monitor for a potential deterioration in their condition. Expectant, unsalvageable patients are provided appropriate palliative care and their condition clearly explained to their relatives. Documentation is kept succinct and should generally be limited to the essential points about each patient’s condition and treatment. Any forensic investigations are likely to require the cooperation of emergency physicians and other health personnel. Cultural and religious needs associated with the management of dead bodies and in communication with relatives should be respected at all times.
Urban search and rescue
Urban search and rescue (USAR) is the science of locating, reaching, treating and safely extricating survivors who remain trapped following a structural collapse. Search and rescue response capabilities have increased significantly, due to advances in rescue technology and in emergency services.
In the period immediately following a structural collapse, many survivors are rescued by uninjured bystanders. Those who remain trapped generally require the assistance of specially trained and equipped units from fire, ambulance or police services in order to be safely extricated. Medical members of search and rescue teams are tasked to provide medical care to the victims and medical support to the rescuers. They are not usually involved in the actual extrication process. Potential hazards to victims and rescuers are numerous and scene safety is of critical importance. The identification and extrication of victims following a major structural collapse is one of the most physically and emotionally challenging tasks of any rescue operation. The shock of dealing with scenes of carnage and mutilation may render some rescue personnel ineffective. These teams must therefore be trained and prepared to deal with the emotional strains of working in such a demanding environment.
Mental health
It is easy to overlook the mental health needs of affected individuals during the emergency response, when rescue and life-saving interventions receive top priority. Emergency physicians should be aware of the significant psychological impact of disasters on victims, families and rescue personnel. Psychological support is recommended as first-level assistance to disaster-affected communities and personnel [29]. Mental health consequences, such as depression, anxiety states and post-traumatic stress syndrome, are well described following disasters and need to be considered when developing the disaster plan. Crisis counselling may play an important role in the overall medical care provided to patients following a disaster. In addition, rescue personnel may well suffer psychological consequences from their own involvement in the disaster response and should therefore be provided with access to appropriate support and services.
Mass gatherings
Social and cultural events can result in the gathering of many people in one place at a particular time, sometimes over several days. Common examples include religious events, music festivals, sporting events, fairs and parades. The organization of medical services for mass gatherings is generally designed to address minor medical needs, but must also take into consideration medical emergencies, such as cardiac arrests, and disaster planning, for incidents such as extreme weather, fire, structural collapse or terrorism. Medical services developed for the mass gathering must be linked to local emergency medical systems. Public health and occupational health regulations, including food safety and environmental health measures, must be observed.
Public health issues in disasters
Public health professionals are involved in all phases of disaster risk management and it is important for emergency physicians to understand the role of public health in disaster medicine and disaster risk management. Epidemiological studies that have identified risk factors for illness and injury following disasters have contributed greatly to disaster risk assessments, prevention, mitigation, preparedness (including planning), response and recovery. These investigations have been central to the development of the science of disaster medicine. They have led to key strategies that have been effective in reducing disaster-related morbidity and mortality.
Public health interventions become high priorities following disasters that disrupt the social infrastructure (for instance, cyclone, flooding, earthquake) and disasters that result in significant population displacement (such as complex emergencies). Priorities for the affected population include the provision of adequate water quantity and quality, sanitation, food, shelter, infectious disease control and disease surveillance. The role of public health following a mass casualty incident includes injury control, occupational health and safety measures for responders and injury surveillance.
The interface between emergency medicine and public health becomes increasingly important following technological disasters or terrorist events involving biological, chemical or nuclear agents. The terrorist attacks with anthrax in the USA during 2001 and their aftermath demonstrated the vital importance of key public health tools, such as disease surveillance and outbreak investigation and control. Following incidents with chemical or radiological agents, public health officials may be required to provide guidance on issues, such as evacuation of the public, mass decontamination and the mass distribution of iodine. Emergency physicians should become more familiar with the skills, roles and responsibilities of their public health colleagues, especially as they relate to disaster management and infectious disease control.
Conclusion
State-of-the-art in contemporary disaster management emerges from interdisciplinary, interagency and international best practices. Curative medical skills and public health skills are both fundamental to the comprehensive management of a community affected by a disaster. Emergency physicians contribute most significantly to the preparedness and response aspects of disaster management. Emergency physicians should plan and build capacities for disasters based on an assessment of the major risks that their communities face and those which are most likely to result in multiple casualties. These include the risks associated with natural, technological, biological and societal hazards. The increased risks posed by climate change and terrorists require the continuing review and revision of disaster risk-assessment processes and disaster planning. Disasters associated with multiple casualties provide unique challenges to the health and medical communities. Short courses in disaster management are widely available and should be part of every emergency physician’s training.
Likely developments
26.4 Triage
Drew Richardson
Introduction
Provision of high-availability quality medical care is expensive and has been traditionally limited to the very wealthy or to situations of great demand, such as the military in battle. Even today, well-organized emergency medical systems are concentrated in societies sufficiently affluent to spend 5% or more of GDP on health. Some form of rationing is required whenever an expensive resource is coupled with fluctuating demand. Price, queuing and denial are all used in different areas of medicine. Simple application of any of these methods in emergency medicine would not be efficient nor equitable, so the majority of emergency medical systems use a triage process to sort patients into a number of queues.
Triage, the sorting of patients on the basis of urgency, is an ongoing process that nevertheless requires formal structures at different points within the continuum of care. In the emergency department (ED) setting there is considerable evidence that urgency can be assigned reliably and distinctly on a five level scale and that this categorization is applicable and useful beyond the concept of ‘urgency’ into other aspects of hospital care.
Origins of triage
The word ‘triage’, arising from the French ‘trier’ meaning ‘to sort’ has its origins in Latin. It has entered English at least three times: from the 18th century wood industry, the 19th century coffee industry and from 20th century emergency medicine. The process understood today as triage was first described by Baron Dominique Jean-Larrey (1766–1842) [1], the surgeon to Napoleon, who also developed the ambulance volante, the first field ambulance. This delivered large numbers of injured but salvageable cases to medical units, mandating a more efficient system than treatment in order of military rank. Jean-Larrey’s ‘order of dressing and arrangement’ by urgency was also in keeping with the egalitarian spirit of the French revolution, although there is no evidence that he actually used the word triage. His concept was embraced and refined by military surgeons over the next 150 years, usually with the primary intent of returning soldiers to battle in the most efficient manner.
Civilian triage developments
There was certainly some sorting of patients from the moment ‘casual wards’ opened in 19th century hospitals, but the first systematic description in civilian medicine was by E. Richard Weinerman in Baltimore in 1966 [2]. Since that time, there has been a huge growth in emergency medicine as a specialty and a number of workers have undertaken formal investigation of triage, particularly in Australasia. The Australasian experience formed the basis of ED triage development in Canada and the UK, while some other jurisdictions have developed systems independently.
Process of triage
The underlying principles of triage are those of equity (or justice) and efficiency. EDs experience potentially overwhelming demand from patients with an enormous range of conditions. Equity demands that the distribution of resources for treatment is fair in the broadest sense. The concept of urgency is well understood by the population who generally accept that it is fair to treat those in the greatest need ahead of those who arrived before them. Efficiency demands that best use is made of available resources. In the setting of ED, cost and resource pressures prevent all demand being satisfied simultaneously. The overall philosophy of ‘doing the greatest good for the greatest number’ requires resource allocation on the basis of need which, in turn, requires a process to identify and prioritize the needs of the presenting population.
In the ED, urgency is distinct from severity, prognosis, complexity and case mix, although a correlation exists. Some urgent problems (for example, upper airway obstruction) have a poor outcome without rapid intervention but are not severe in the sense of requiring long-term care, other severe problems (for example, life-threatening malignancy) may not require any treatment in the ED time frame. Complexity is reflected in the number of interventions, such as investigations or consultations required, whereas case mix is an indication of the resources required to provide care.
Triage is an ongoing process that may change in response to alterations in patient status and resource availability, but it is efficient to undertake a formal process once, early in the patient’s encounter, and then review only as necessary. ED triage is normally undertaken by trained nursing staff at the time of arrival and the assigned urgency is then used to guide treatment order. ‘Triage’, used as a noun, is now regarded as the first point of patient contact in EDs.
The overall efficiency and effectiveness of such a system depends not only on the allocated priority but also on the treatment strategy, that is, the way in which the next patient is chosen from the different queues. A more urgent case should wait less time than a less urgent case but, when resources become available to treat the next patient, choice may still be required between a new arrival and a slightly less urgent patient who has already been waiting for some time. It may also be a more efficient strategy in terms of both waiting time and patient care time to ‘stream’ particular patients to particular providers, for example uncomplicated muscular injuries to a physiotherapist.
Australasian triage development
The first Australasian description was of the Box Hill Triage Scale by Pink and Brentnall in 1977 [3]. They used verbal descriptions without time consideration and classified patients into five categories: immediate, urgent, prompt, non-urgent and routine. Fitzgerald modified this scale in 1989 [4], to produce the Ipswich Triage Scale. This used five colours to categorize patients according to the question: ‘This patient should under optimal circumstances be seen within…’. The five categories were seconds, minutes, an hour, hours and days. Fitzgerald found his triage scale to have good interobserver reliability on formal testing and to be a practical predictor of ED outcome and length of ICU stay, but a relatively poor predictor of outcome at hospital discharge.
Jelinek [5] investigated the relationship between the Ipswich Triage Scale and case mix, observing a strong correlation between triage categorization and overall use of resources in the ED and validated possible funding models. He proposed two possible case mix classifications: urgency and disposition groups (UDGs – 12 groups) and urgency related groups (URGs – 73 groups) based on urgency, disposition and diagnosis. After trimming for outliers, these were found to account for 47% and 58% of the cost variance in large hospitals.
In 1994, the Australasian College for Emergency Medicine formalized the National Triage Scale [6], derived from the Ipswich Triage Scale. This used colours, names or numerical categories to represent five groups, based on the answer to the question ‘This patient should wait for medical care no longer than…’. The categories were: immediate, 10 minutes, 30 minutes, 1 hour and 2 hours. The definition document also proposed Jelinek’s concept [5] of performance indicators based on the proportion of patients whose care fell within the desired time threshold and audit by means of admission rates and sentinel diagnoses. It influenced treatment strategies by indicating the need to achieve performance indicators in a high proportion of patients in every category (higher in the more urgent) and it clearly established the need for EDs to employ systematic, accountable and audited triage processes.
Over the next few years, the National Triage Scale was widely accepted and recognized by all Australian State Governments as an appropriate measure of access to emergency care. It was also adopted in the performance indicators promulgated by the Australian Council on Healthcare Standards [7]. Research repeated the findings of Fitzgerald and Jelinek with reference to the new 5-point scale and investigated many more of the subtleties of triage scale use.
The Australasian Triage Scale
The Australasian Triage Scale (ATS) [8] is the current refinement of the National Triage Scale (NTS). It has been jointly developed by the Australasian College for Emergency Medicine, emergency nursing organizations and other interested parties. For practical purposes, the scale concept itself is unchanged, but the ATS uses numeric classification only, better defines waiting time and includes associated implementation guidelines and educational material, partly derived from work on the NTS in areas such as mental health triage [9]. Further training packages have subsequently been developed [10], secondary to concerns about variation in triage training [11].
The ATS categorizes patients presenting to EDs in response to the question: ‘This patient should wait for medical assessment and treatment no longer than…’ (Table 26.4.1)
Table 26.4.1
The ATS categorization of patients presenting to EDs
| ATS category | Treatment acuity (maximum waiting time) |
| ATS 1 | Immediate |
| ATS 2 | 10 minutes |
| ATS 3 | 30 minutes |
| ATS 4 | 60 minutes |
| ATS 5 | 120 minutes |
Other triage scales
The concept of desirable waiting time must include some subjective component but has, nevertheless, been found to be reliable and reproducible. Achievement of ATS waiting times has proven to be a useful performance indicator, but remains a measure of process rather than ED outcome. Concerns have been expressed in some jurisdictions about the medicolegal implications of a time-based threshold which will not always be met and other systems have taken different approaches in development of their own ED triage systems. Nevertheless, most have developed five-level triage systems along the Australasian model. Major validated triage scales include:
 the Canadian Emergency Department Triage and Acuity Scale (CTAS) [12]: derived from the ATS but using a 15-minute threshold in category 2
the Canadian Emergency Department Triage and Acuity Scale (CTAS) [12]: derived from the ATS but using a 15-minute threshold in category 2
 the Manchester Triage Scale [13]: uses an algorithmic approach to the UK Triage scale, similar to the ATS but with longer thresholds in the lower acuity categories
the Manchester Triage Scale [13]: uses an algorithmic approach to the UK Triage scale, similar to the ATS but with longer thresholds in the lower acuity categories
 the ESI Triage Algorithm [14]: developed in the USA without any time thresholds, but using a simple approach to classifying urgency.
the ESI Triage Algorithm [14]: developed in the USA without any time thresholds, but using a simple approach to classifying urgency.
Use beyond waiting time
Triage is based on a brief assessment and an individual triage categorization can reflect only the probability of certain outcomes. Large populations of triaged patients, however, exhibit predictable patterns. There is a very strong, almost linear relationship between triage category and total rate of admission, transfer or death, ranging from 80–100% in ATS 1 to 0–20% in ATS 5 [15]. This pattern is repeated across hospitals of different size and different patient mix. Admission rates by triage category follow the pattern of overall admission rates in relation to age, giving a flattened ‘U-shaped’ distribution. The inter-rater reliability studies performed using the Ipswich Triage Scale have been repeated using the NTS/ATS, which has been found to be slightly better [16]. Further, admission rates by triage category have been shown to be constant over time in individual institutions [17].
The NTS/ATS has been extensively studied as a case-mix tool. ED outcome (admission/transfer/death versus discharge) accounts for the largest variance in cost, but triage categorization comes a close second, with age third. The mean cost of care for a category 1 patient is approximately 10 times that of a category 5 patient. Urgency and Disposition Groups (UDGs), described by Jelinek using the Ipswich Triage Scale, have been validated using the National Triage Scale on large samples [18]. Age has been included to derive urgency, disposition and age groups (UDAGs – 32 groups), which account for 51% of the cost variance and are not susceptible to different diagnostic approaches [19]. The relativities derived in these studies should no longer be considered valid in the era of overcrowding and access block, because staff costs for admitted patients reflect length of time in the ED, which may now be driven by outside factors. Further, the costs for discharged patients are becoming skewed by increased pressure to keep complex patients out of hospital.
Triage categorization is a very strong predictor of ED outcome and a good predictor of utilization of critical care resources. However, it is a relatively poor predictor of outcome at hospital discharge [20,21]. Many patients with chronic or subacute conditions that frequently cause death are triaged to less urgent categories because there is no benefit from earlier treatment within the time scales available in the ED.
Attainment of performance indicators for patients seen within triage thresholds has been shown to be a measure of resource allocation within the ED. A longitudinal comparative study has demonstrated a significant improvement with an increase in ED staff and funding [22].
Triage staff are well able to assess complexity [23] and so initial triage is also the appropriate point to start streaming decisions, for example to a ‘fast track’ area for low-complexity patients [24]. Although streaming can be seen as decreasing equity because the less urgent patients achieve shorter waiting times than more urgent, in practice, this is compensated by the gain in overall efficiency [25–27]. Like the triage process itself, changes to the treatment strategy, such as streaming, can and should be ongoing, reflecting not the urgency of the patients, but the best distribution of the resources available at that moment.
Structure and function of a triage system
The exact requirements for triage vary with the role, location and size of the hospital, but effective systems share a number of important features, mostly derived from experience:
Pre-hospital triage
The principle of making best use of available resources to maximize patient outcome remains the basis of triage in any setting. Relatively less therapeutic options are available to pre-hospital providers and patient disposition is generally limited to transport and sometimes choice of hospitals. The initial pre-hospital phase, the travel to the patient, must be undertaken on the basis of minimal information. Most pre-hospital systems are strongly protocol driven and tend towards three or four level assessment: rapid response (lights and sirens), immediate response, routine response or no transport. Once the patient is assessed in the field, there is patient benefit in triaging to the most appropriate hospital for tertiary-level conditions, such as major trauma [28] or ST-elevation myocardial infarction [29].
Military and disaster triage
In situations of overwhelming imbalance between resources and demand, triage remains critical in ensuring that available resources are used to achieve the greatest good. The principles of rapid assessment, documentation and multiple queues for care remain the same, but competing demands on resources may mean triaging cases to receive minimal or no care or treating first those who can return to work or duty. The need for both human and physical resources for more important tasks may profoundly limit individual patient care.
Military and disaster triage require seniority and experience (which by definition is rarely available), the ability to make and defend rapid decisions and a successful liaison with other players outside the medical or nursing hierarchy. Senior personnel with significant experience and preferably with additional training should be chosen for this role if possible. Formal triage and documentation must be brief and will use different scales from those appropriate in the ED.