History
Current Medications
Current Symptoms
Physical Examination
Laboratory Data
Electrocardiogram
Findings
Chest Radiograph
Findings
Echocardiogram
Findings
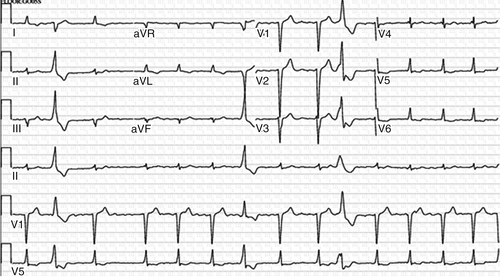
FIGURE 25-1
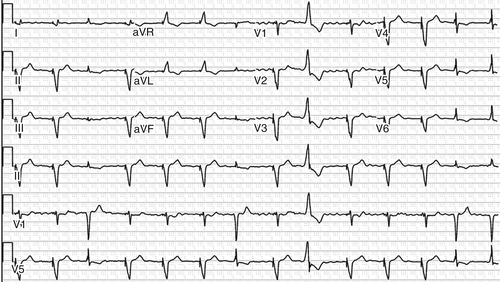
FIGURE 25-2
Physiologic Tracings
Findings
Before Device Implantation
After Atrioventricular Node Ablation and Device Implantation
Computed Tomography
Findings
Focused Clinical Questions and Discussion Points
Question
Discussion
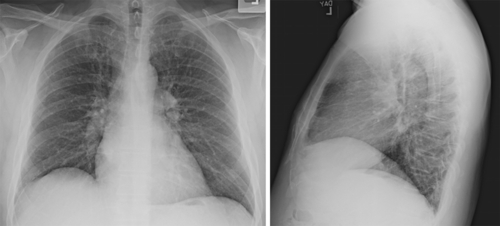
FIGURE 25-3
Question
Discussion
Question
Discussion
Final Diagnosis
Plan of Action
Intervention
Findings
Selected References
1. Bogun F., Crawford T., Reich S. et al. Radiofrequency ablation of frequent, idiopathic premature ventricular complexes: comparison with a control group without intervention. Heart Rhythm. 2007;4:863–867.
2. Ganesan A.N., Brooks A.G., Roberts-Thomson K.C. et al. Role of AV nodal ablation in cardiac resynchronization: in patients with coexistent atrial fibrillation and heart failure a systematic review. J Am Coll Cardiol. 2012;59:719–726.
3. Grogan M., Smith H.C., Gersh B.J. et al. Left ventricular dysfunction due to atrial fibrillation in patients initially believed to have idiopathic dilated cardiomyopathy. Am J Cardiol. 1992;69:1570–1573.
4. Hayes D.L., Boehmer J.P., Day J.D. et al. Cardiac resynchronization therapy and the relationship of percent biventricular pacing to symptoms and survival. Heart Rhythm. 2011;8:1469–1475.
5. Lakkireddy D., Di Biase L., Ryschon K. et al. Radiofrequency ablation of premature ventricular ectopy improves the efficacy of cardiac resynchronization therapy in nonresponders. J Am Coll Cardiol. 2012;60:1531–1539.
6. Stulak J.M., Dearani J.A., Daly R.C. et al. Left ventricular dysfunction in atrial fibrillation: restoration of sinus rhythm by the Cox-maze procedure significantly improves systolic function and functional status. Ann Thorac Surg. 2006;82:494–500 discussion 500-491.
7. Yarlagadda R.K., Iwai S., Stein K.M. et al. Reversal of cardiomyopathy in patients with repetitive monomorphic ventricular ectopy originating from the right ventricular outflow tract. Circulation. 2005;112:1092–1097.





