Needle Thoracostomy (Perform)
Needle Thoracostomy (Perform)
PREREQUISITE NURSING KNOWLEDGE
• Anatomy and physiology of the pulmonary system should be understood.
• The thoracic cavity, in normal conditions, is a closed air space. Any disruption results in the loss of negative pressure within the intrapleural space. Air or fluid that enters the space competes with the lung, which results in collapse of the lung. Associated conditions are the result of disease, injury, surgery, or iatrogenic causes.
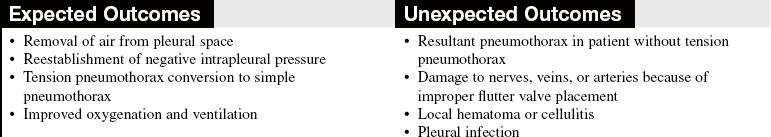
• A pneumothorax is classified as an open, closed, or tension pneumothorax. In patients with tension pneumothorax, air leaks into the pleural space through a tear in the lung and, with no means to escape from the pleural cavity, creates a one-way valve effect. With each breath the patient takes, air accumulates, pressure within the pleural space increases, and the lung collapses. As a result, the mediastinal structures (i.e., heart, great vessels, and trachea) shift to the opposite or unaffected side of the chest. Venous return and cardiac output are impeded, and the possibility of collapse of the unaffected lung exists.1–5
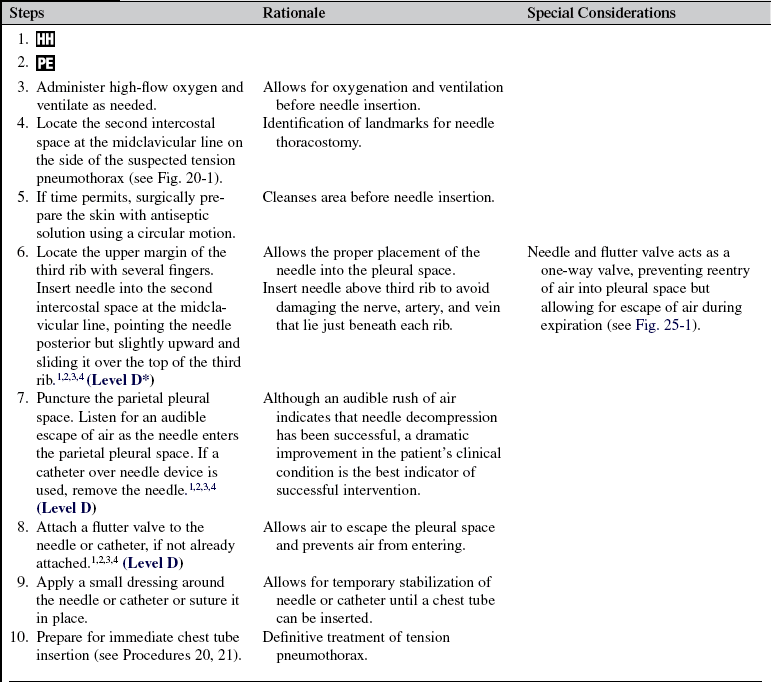
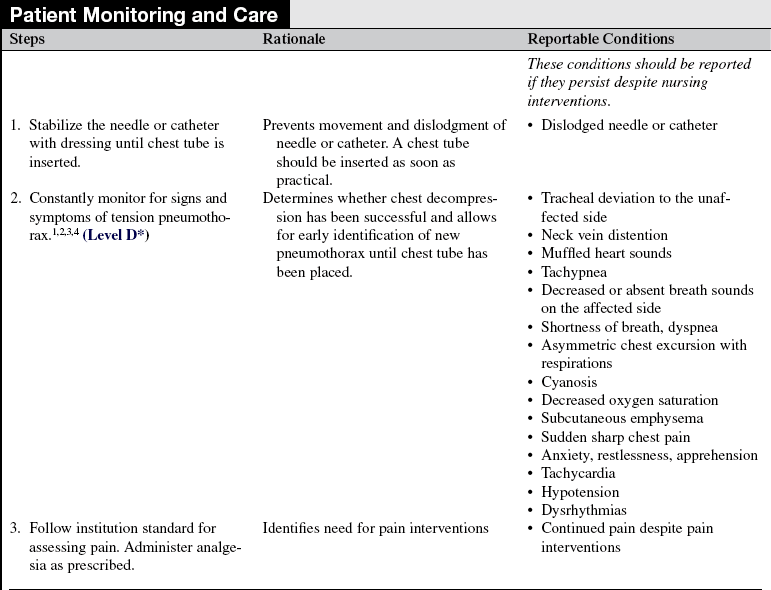
• Tension pneumothorax is a medical emergency that necessitates immediate intervention. Accurate assessment of signs and symptoms allows for prompt recognition and treatment:
 Tracheal deviation to the unaffected side
Tracheal deviation to the unaffected side
 Decreased or absent breath sounds on the affected side
Decreased or absent breath sounds on the affected side
 Asymmetric chest excursion with respirations
Asymmetric chest excursion with respirations
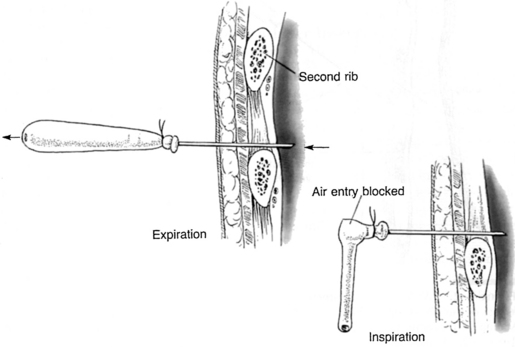
• Needle thoracostomy is performed with placement of a needle into the pleural space to remove air and reestablish negative pressure in a patient with an unstable condition with tension pneumothorax (Fig. 25-1).
EQUIPMENT
• Personal protective equipment
• 14- to 16-gauge hollow needle or catheter with one-way valve attached or commercially available (Heimlich) flutter valve
Additional equipment to have available as needed includes the following:
The listed equipment can be used to create an emergency one-way valve:
Cut a finger off the glove and attach it to the needle with the rubber band.1
PATIENT AND FAMILY EDUCATION
• Explain the procedure and reason for needle thoracostomy.  Rationale: This communication identifies patient and family knowledge deficits concerning the patient’s condition, expected benefits, and potential risks and allows time for questions to clarify information and to voice concerns. Explanations decrease patient and family’s anxiety and enhance cooperation.
Rationale: This communication identifies patient and family knowledge deficits concerning the patient’s condition, expected benefits, and potential risks and allows time for questions to clarify information and to voice concerns. Explanations decrease patient and family’s anxiety and enhance cooperation.
• If indicated, explain the patient’s role in assisting with needle thoracostomy.  Rationale: Eliciting the patient’s cooperation assists with insertion of a needle and flutter valve.
Rationale: Eliciting the patient’s cooperation assists with insertion of a needle and flutter valve.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Signs and symptoms consistent with tension pneumothorax, as noted previously.  Rationale: Accurate assessment of signs and symptoms allows for prompt recognition and treatment. Baseline assessment provides comparison data for evaluation of changes and outcomes of treatment. Tension pneumothorax is a medical emergency that necessitates immediate intervention.
Rationale: Accurate assessment of signs and symptoms allows for prompt recognition and treatment. Baseline assessment provides comparison data for evaluation of changes and outcomes of treatment. Tension pneumothorax is a medical emergency that necessitates immediate intervention.
Patient Preparation
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Ensure that the patient and family understand the emergency nature of the procedure and preprocedural teachings, if appropriate. Answer questions as they arise, and reinforce information as needed.  Rationale: This communication evaluates and reinforces understanding of previously taught information.
Rationale: This communication evaluates and reinforces understanding of previously taught information.
• Position patient in supine position with the head of the bed flat.  Rationale: This positioning allows for identification of landmarks for proper placement of needle and flutter valve.
Rationale: This positioning allows for identification of landmarks for proper placement of needle and flutter valve.
• Perform a pre-procedure verification and time out, if non-emergent.  Rationale: Ensures patient safety.
Rationale: Ensures patient safety.
References
![]() 1. American College of Surgeons Committee on Trauma. Advanced trauma life support manual, ed 7. Chicago: American College of Surgeons; 2004.
1. American College of Surgeons Committee on Trauma. Advanced trauma life support manual, ed 7. Chicago: American College of Surgeons; 2004.
2. Emergency Nurses Association, Trauma nursing core course. provider manual. ed 6. Emergency Nurses Association, Des Plaines, IL, 2007.
![]() 3. Holleran, RS, Air and surface patient transport. principles and practice. ed 3. Mosby, St Louis, 2003.
3. Holleran, RS, Air and surface patient transport. principles and practice. ed 3. Mosby, St Louis, 2003.
![]() 4. National Association of Emergency Technicians, PHTLS. basic and advanced prehospital trauma life support. ed 5. Mosby, St Louis, 2003.
4. National Association of Emergency Technicians, PHTLS. basic and advanced prehospital trauma life support. ed 5. Mosby, St Louis, 2003.
![]() 5. Roberts, JR, Hedges, JR, Clinical procedures in emergency medicine. ed 4. Saunders, Philadelphia, 2004.
5. Roberts, JR, Hedges, JR, Clinical procedures in emergency medicine. ed 4. Saunders, Philadelphia, 2004.