Emergency Medicine and the Law
Edited by George Jelinek
25.1 Mental health and the law: the Australasian and UK perspectives
Georgina Phillips, Suzanne Mason and Simon Baston
Introduction
The emergency department (ED) is frequently the interface between the community and the mental health system. In recent years, changes in health policy have resulted in ‘mainstreaming’ of mental health services, so that stand-alone psychiatric services are less common and services are more likely to be provided in a general hospital setting. Linked to this has been a move away from managing long-term psychiatric patients in institutional settings, so that many of these former patients are now living in the community with or without support from mental health services.
Traditionally, by virtue of their accessibility, EDs have been a point of access to mental health services for persons with acute psychiatric illness, whether this be self- or family referral or by referral from ambulance, police or outside medical practitioners. An important function of an ED is to differentiate between those who require psychiatric care for a psychiatric illness and those who present with a psychiatric manifestation of a physical illness and who require medical care. Admission of a patient with a psychiatric manifestation of a physical illness to a psychiatric unit may result in further harm to or death of the patient.
In the UK and Australasia, doctors in general are empowered by legislation to detain a mentally ill person who is in need of treatment. Mental illness, particularly its manifestation as self-harm, is a common ED presentation (in the UK, making up around 1–2% of new patient attendances and up to 5% of attendances in Australasia) and emergency physicians require not only the clinical skills to distinguish between those who require psychiatric or medical intervention, but also a sound working knowledge of the mental health legislation and services relevant to the state where they practise. This ensures that patients with psychiatric illness are managed in the most appropriate way, with optimal utilization of mental health resources and with the best interests and rights of the patient and the community taken into consideration.
While there are variations in mental health legislation between the UK, Australia and New Zealand, all legislation recognizes fundamental common principles that respect individual autonomy and employ least restrictive management practices. The World Health Organization (WHO) advises 10 basic principles of mental healthcare law, including enshrining geographical, cultural and economic equity of access to mental health care, acceptable standards of clinical assessment, facilitating self-determination, minimizing restrictive treatment and enshrining regular and impartial decision making and review of care [1]. These themes are all present in Australasian and UK law and awareness of such principles aids the clinician in delivering humane and ethical treatment for mentally unwell patients who seek emergency care.
Variations in practice
Mental health legislation in England and Wales
The National Service Framework for Mental Health
The National Service Framework for Mental Health produced by the Department of Health in the UK (1999) is aimed at improving quality and addresses the mental health needs of working age adults up to 65 years. It states as one of its standards that:
Any individual with a common mental health problem should be able to make contact round the clock with the local services necessary to meet their needs and receive adequate care.
Although EDs do not provide the ideal environment for a mental health assessment, they are likely to continue to provide an entry point for people with mental health problems. Easy access to the ED can lead to individuals with acute mental health problems seeking help directly, making up to perhaps 5% of ED attenders.
Two pieces of legislation cover the care and treatment of patients with disorders of the brain or mind. The Mental Health Act (1983) deals with compulsory assessment and treatment of people with mental illnesses, while the Mental Capacity Act (2005) deals with people who are unable to make decisions about their medical treatment for themselves for various reasons.
Mental Health Act
Definition of mentally ill or mental illness
According to the 1983 Mental Health Act, mental illness is undefined. However, in practice it includes conditions such as schizophrenia, bipolar disorder, depression, psychosis and organic brain syndromes. Mental impairment is defined as: ‘a state of arrested or incomplete development of mind which includes significant impairment of intelligence and social functioning and is associated with abnormally aggressive or seriously irresponsible conduct on the part of the person concerned’. A psychopathic disorder is defined as ‘a persistent disorder or disability of mind which results in abnormally aggressive or seriously irresponsible conduct on the part of the person concerned’. The Act does not cover promiscuity or other immoral conduct or sexual deviancy which, in the past, could result in incarceration in psychiatric hospitals or dependence on drugs or alcohol.
Detention of patients with mental illness
The Mental Health Act 1983 provides legislation with regard to the management of patients with a mental illness unwilling to be admitted or detained in hospital voluntarily, where this would be in the best interests of the health and safety of patients and others. For the purposes of the Act, patients in the ED are not considered inpatients until they are admitted to a ward. In order for legislation to be imposed, it is necessary for two conditions to be satisfied: the patient must be suffering from a mental illness and emergency hospital admission is required because the patient is considered to be a danger to themselves or others.
Detention under the Mental Health Act does not permit treatment for psychiatric or physical illness. Treatment can be given under common law where the patient is considered to pose a serious threat to themselves or others. Otherwise all treatment must be with the patient’s consent.
Section 2 of the Mental Health Act facilitates compulsory admission to hospital for assessment and treatment for up to 28 days. The application is usually made by an approved social worker or the patient’s nearest relative and requires two medical recommendations, usually from the patient’s general practitioner and the duty senior psychiatrist (who is approved under Section 12 of the Mental Health Act). In the ED, the responsibility for coordinating the procedure often lies with the emergency physician.
Section 3 of the Mental Health Act covers compulsory admission for treatment. Once again, recommendations must be made by two doctors, one of whom is usually the general practitioner and the other a psychiatrist approved under Section 12 of the Act. The application is usually made by an approved social worker or the patient’s nearest relative. Detention is for up to 6 months but can be renewed.
Section 4 of the Mental Health Act covers emergency admission for assessment and attempts to avoid delay in emergency situations when obtaining a second recommendation could be dangerous. It requires the recommendation of only one doctor, who may be any registered medical practitioner who must have seen the patient within the previous 24 h. The order lasts for 72 h. Application can be made by the patient’s nearest relative or an approved social worker. In practice, the application of Section 4 of the Mental Health Act rarely happens. Usually Section 2 or 3 is the preferred option.
Section 5(2) – doctors holding power and Section 5(4) – nurses holding power of the Act allow the detention of patients who are already admitted to hospital until a more formal Mental Health Act assessment can take place. Unfortunately, presence in the ED is not considered to constitute admission to hospital and this section is, therefore, not applicable to the ED.
A new draft Mental Health Bill, published in 2002, was opposed by professional and patient groups alike. It aimed to introduce a new legal framework for the compulsory treatment of people with mental disorders in hospitals and the community. The new procedure involved a single pathway in three stages: a preliminary examination, a period of formal assessment lasting up to 28 days and treatment under a Mental Health Act order. In order for the compulsory process to be used, four conditions needed to be satisfied: the patient must have a mental disorder, the disorder must warrant medical treatment, treatment must be necessary for the health and safety of the patient or others, and an appropriate treatment for the disorder must be available. The draft Bill made provision for treatment without consent as it is justified under the European Convention on Human Rights Article 8(2) in the interests of public safety or to protect health or moral standards.
The resulting debate saw much of the draft Bill being scrapped in favour of amendments being made to the existing Mental Health Act. This included the creation of community treatment orders and a broader definition of mental disorder.
Police powers
Section 136 of the Act authorizes the police to remove patients who are believed to be mentally disordered and causing a public disturbance to a place of safety. The place of safety referred to in the Act is defined in Section 135 as ‘residential accommodation provided by a local authority under Part III of the National Assistance Act 1948, or under Paragraph 2, Schedule 8 of the National Health Service Act 1977, a hospital as defined by this Act, a police station, a mental nursing home or residential home for mentally disordered persons or any other suitable place, the occupier of which is willing temporarily to receive the patient’. In practice, the police often transport these patients to local EDs. The patient must be assessed by an approved social worker and a registered doctor. The order lasts for 72 h.
Section 135 allows the police to enter premises to remove a patient believed to be suffering from a mental disorder to a place of safety for up to 72 h. The patient is then assessed as above.
Mental Capacity Act
The Mental Capacity Act relates to decision making, for those whose mental capacity is in doubt, on any issue from what to wear to the more difficult issues of medical treatment, personal finance and housing.
Lack of capacity can occur in two distinct ways. First, that capacity is never achieved – for example someone with a severe learning difficulty. Secondly, capacity can be lost either as a result of long-term conditions, such as dementia, or for a short period because of a temporary factor, such as intoxication, shock, pain or emotional distress.
It is also important that decision making is task specific. An individual may be able to make decisions about simple matters, such as what to eat or wear, but may be unable to make more complex decisions, for example about medical care.
Assessment of capacity
To have capacity about a decision, the patient should be able to comply with the following four steps:
 understand the information relevant to the decision
understand the information relevant to the decision
 retain the information for the period of decision making
retain the information for the period of decision making
 use or weigh that information as part of the process of making a decision
use or weigh that information as part of the process of making a decision
Every effort needs to be made to enable people to make their own decisions.
The Act points out that people should be allowed to make ‘eccentric’ or ‘unwise’ decisions, as it is their ability to decide that is the issue not the decision itself.
Advance directives
The Act makes provision for advance directives to be made at a time when the patient has capacity. These directives need to make specific reference to the medical treatments involved and include the statement ‘even if life is at risk’. The validity of any advance decision needs to be clearly documented.
Advocates
Although family and friends have no legal powers (unless specified in advance) to make decisions for the incapacitated patient, the Act recognizes their role in acting as an advocate. An independent mental capacity advocate is available to represent those with no close family or friends.
Emergency treatment
Treatment can be given to patients who lack capacity but several factors need to be considered:
Use of sedation or physical restraint
This is covered in detail elsewhere (Chapters 20.6 and 21.5). From the perspective of the mental health legislation, there are occasions where physical or pharmacological restraint is needed. Sedation or restraint must be the minimum that is necessary to prevent the patient from self-harming or harming others. Generally, a patient committed involuntarily is subject to treatment necessary for their care and control and this may reasonably include the administration of sedative or antipsychotic medication as emergency treatment. Transporting these patients to a mental health service should be done by suitably trained medical or ambulance staff and not delegated to police officers or other persons acting alone.
Mental health legislation in Australasia
In Australia, mental health legislation is a state jurisdiction and, among the various states and territories, there is considerable variation in the scope of mental health acts and between definitions and applications of the various sections. Since the National Mental Health Strategy in 1992, there has been an effort in Australia to adopt a consistent approach between jurisdictions, with an emphasis on ensuring legislated review mechanisms and a broad spectrum of treatment modalities [2]. In 2009, this national strategic approach was reaffirmed by all the States and Territories of Australia with the release of a National Mental Health Plan, focusing on promoting mental health and preventing mental disorders, minimizing the impact of mental illness across the whole community and protecting the rights of people with mental illness.
Several Australian states and territories have recently initiated mental health law reform, all within a human rights framework. Generally, there is an increased recognition of autonomous and supported decision making with a particular focus on enhancing informed consent through advance directives or involving a nominated support person. Increased transparency of and limitations around restrictive practices will affect activities within EDs. Community visitors and mental health tribunals are introduced to ensure frequent independent oversight and review and it is now mandatory in several jurisdictions to give patients and carers written copies of involuntary orders made about them, as well as a statement of their rights. Despite these common themes, key differences apply between mental health acts and therefore specific issues should be referred to the Act relevant to the emergency physician’s practice location.
The Australian and New Zealand mental health acts and related documents referred to in this chapter are the following:
ACT – Mental Health (Treatment and Care) Act 1994, amendments 2007 and current review documents 2012
Queensland – Mental Health Act 2000
Tasmania – Mental Health Act 1996 and the new Mental Health Bill introduced 2012
Sections of the various mental health acts relevant to emergency medicine include those dealing with:
 the definition of mentally ill
the definition of mentally ill
 indigenous and cultural acknowledgement
indigenous and cultural acknowledgement
 the effects of drugs or alcohol
the effects of drugs or alcohol
 criteria for detention and admission as an involuntary patient
criteria for detention and admission as an involuntary patient
 persons unable to recommend a patient for involuntary admission
persons unable to recommend a patient for involuntary admission
 physical restraint and sedation
physical restraint and sedation
 offences in relation to documents
offences in relation to documents
Definition of mentally ill or mental illness
For the purposes of their respective mental health acts, New Zealand and all the Australian states and territories define mental illness or disorder as follows.
Australian Capital Territory
The Australian Capital Territory (ACT) Act defines a psychiatric illness as a condition that seriously impairs (either temporarily or permanently) the mental functioning of a person and is characterized by the presence in the person of any of the following symptoms: delusions, hallucinations, serious disorder of thought form, a severe disturbance of mood or sustained or repeated irrational behaviour indicating the presence of these symptoms.
The ACT Mental Health Act also defines ‘mental dysfunction’ as a ‘disturbance or defect, to a substantially disabling degree, of perceptual interpretation, comprehension, reasoning, learning, judgement, memory, motivation or emotion’.
New South Wales
The New South Wales Act defines mental illness in the same way as the ACT but, in addition, distinguishes between a mentally ill person and a mentally disordered person, chiefly for the purposes of determining need for involuntary admission and treatment.
A person (whether or not the person is suffering from mental illness) is mentally disordered if the person’s behaviour for the time being is so irrational as to justify conclusion on reasonable grounds that temporary care, treatment or control of the person is necessary for the person’s own protection from serious physical harm or for the protection of others from serious physical harm.
New Zealand
In New Zealand, the Mental Health Act defines a mentally disordered person as possessing an abnormal state of mind, whether continuous or intermittent, characterized by delusions or by disorders of mood, perception, volition or cognition to such a degree that it poses a danger to the health or safety of the person or others, or seriously diminishes the capacity of the person to take care of themselves.
Northern Territory
In the Northern Territory, mental illness means a condition that seriously impairs, either temporarily or permanently, the mental functioning of a person in one or more of the areas of thought, mood, volition, perception, orientation or memory and is characterized by the presence of at least one of the following symptoms: delusions, hallucinations, serious disorders of the stream of thought, serious disorders of thought form or serious disturbances of mood. A mental illness is also characterized by sustained or repeated irrational behaviour that may be taken to indicate the presence of at least one of the symptoms mentioned above. The Northern Territory Act goes further to specify that the determination of mental illness is only to be made in accordance with internationally accepted clinical standards.
Similar to the New South Wales Act, there is a provision in the Northern Territory for those who are ‘mentally disturbed’, which means behaviour of a person that is so irrational as to justify the person being temporarily detained under the Act. The Northern Territory also has provisions for people with complex cognitive impairment who require involuntary treatment.
Queensland
The Queensland Act defines mental illness in a similar way to Victoria, in that it is a condition characterized by a clinically significant disturbance of thought, mood, perception or memory, in accordance with internationally acceptable standards.
South Australia
In the South Australian Act, mental illness means any illness or disorder of the mind.
Tasmania
A person is taken to have a mental illness if they experience temporarily, repeatedly or continuously, a serious impairment of thought (which may include delusions) or a serious impairment of mood, volition, perception or cognition.
Victoria
A person is mentally ill if they have a mental illness, being a medical condition characterized by a significant disturbance of thought, mood, perception or memory.
Western Australia
Persons have a mental illness if they suffer from a disturbance of thought, mood, volition, perception, orientation or memory that impairs judgement or behaviour to a significant extent.
Indigenous and cultural acknowledgement
Cultural differences in the understanding and experiences of mental illness can impact greatly on the ability to provide adequate care. While there are some cursory references to acknowledging special cultural and linguistic needs when interpreting the various mental health acts, only the Northern Territory and South Australia in Australia and the New Zealand Mental Health Acts make specific mention of indigenous people, who are known to be a particularly vulnerable group [3]. Recent legislative reform in some Australian states incorporates recognition of the needs of Aboriginal and Torres Strait Islander and other culturally diverse peoples within a general statement of principles.
The Northern Territory Act states that there are fundamental principles to be taken into account when caring for Aborigines and Torres Strait Islanders. Treatment and care needs to be appropriate to the cultural beliefs and practices of the person, their family and community and involuntary treatment for an Aborigine is to be provided in collaboration with an Aboriginal health worker.
New Zealand stipulates that powers are to be exercised in relation to the Mental Health Act with proper respect for cultural identity and personal beliefs and with proper recognition of the importance and significance to the persons of their ties with family, whanau, hapu, iwi and family group. Interpreters are to be provided if the first or preferred language is not English, with special mention of Maori and New Zealand Sign Language.
Safeguards against prejudice
New Zealand and all Australian states include a number of criteria that, alone, cannot be used to determine that a person has a mental illness and requires involuntary admission. These generally include the expression of or refusal to express particular religious, political and philosophical beliefs; cultural or racial origin; sexual promiscuity or preference; intellectual disability; drug or alcohol taking; economic or social status; immoral or indecent conduct; illegal conduct; and antisocial behaviour. The Northern Territory, Western Australia and Queensland also include past treatment for mental illness and past involuntary admission under these criteria.
Effects of drugs or alcohol
In most Australian states and New Zealand, the taking of drugs or alcohol cannot, of itself, be taken as an indication of mental illness. However, the mental health acts of New South Wales, South Australia, Tasmania, Western Australia and Victoria specify that this does not prevent the serious temporary or permanent physiological, biochemical or psychological effects of alcohol or drug taking from being regarded as an indication that a person is mentally ill. The Queensland Act acknowledges that a person may have a mental illness caused by taking drugs or alcohol.
The remaining states do not specifically exclude the temporary or permanent effects of drugs or alcohol but use definitions of mental or psychiatric illness that are broad enough to cover this. Generally, when a person is so mentally and behaviourally disordered as a result of drug or alcohol use that adequate assessment is impossible and risk of harm to self or others is high, then detaining them for the purposes of assessment and treatment is possible under all Australian and New Zealand mental health acts.
Criteria for admission and detention as an involuntary patient
All states require that an involuntary patient has a mental illness that requires urgent treatment while detained in an inpatient setting for the health (mental or physical) and safety of that patient or for the protection of others. Most states also require that the patient has refused or is unable to consent to voluntary admission. It is also emphasized that appropriate treatment must be available and cannot be given in a less restrictive setting. In New South Wales, the effects of chronicity and the likely deterioration of the person’s condition should be taken into account when determining need for involuntary admission.
Western Australia includes the protection of the patient from self-inflicted harm to the patient’s reputation, relationships or finances as grounds for involuntary admission, although future legislation is likely to remove this criterion.
In New Zealand, the doctor must have reasonable grounds for believing that the person may be mentally disordered and that it is desirable, in the interests of the person, or of any other person or of the public, that assessment, examination and treatment of the person are conducted as a matter of urgency.
Involuntary admission
The process of involuntary admission varies quite markedly across the states. It is variously known as recommendation, certification or committal. All jurisdictions require doctors to examine patients and carefully document on prescribed forms the date and time of examination as well as the particular reasons why the doctor believes that the person has a mental illness that requires involuntary treatment. In addition, patients or their advocates are to be informed of the decisions made about them and their rights under the law at all stages of the involuntary admission process. Increasingly, clinicians are required to give copies of formal orders and printed information about their rights to patients and guardians.
ACT
In the ACT, a medical or police officer is able to apprehend a mentally ill person who requires involuntary admission and is able to use reasonable force and enter premises in order to do so. The officer is required, as soon as possible, to provide a written statement to the person in charge of the mental health facility giving patient details and the reasons for taking the action.
A doctor employed by the mental health facility must examine the patient within 4 h of arrival and may authorize detention for up to 3 days. The doctor must inform the Community Advocate and Mental Health Tribunal of the patient’s admission within 12 h and the patient must receive a physical and psychiatric examination within 24 h of detention.
New South Wales
The Mental Health Act in New South Wales allows for a patient requiring involuntary admission to be detained in a declared mental health facility (which includes EDs) on the certificate of a doctor (or trained ‘accredited person’) who has personally examined the patient immediately or shortly before completing the certificate.
For a mentally ill patient, the certificate is valid for 5 days from the time of writing, whereas for a mentally disordered patient, the certificate is valid for 1 day. Mentally disordered patients cannot be detained on the grounds of being mentally disordered on more than three occasions in any 1 month.
Part of the certificate, if completed, directs the police to apprehend and bring the patient to hospital and also enables them to enter premises without a warrant.
An involuntary patient must be examined by an authorized medical officer (including emergency doctors) as soon as practicable, but within 12 h of admission. The patient cannot be detained unless further certified mentally ill or disordered. This doctor cannot be the same doctor who requested admission or certified the patient. After their own examination, the medical officer must arrange for a second examination as soon as practicable, this time by a psychiatrist. If neither doctor thinks that the person is mentally ill or disordered, then the person must be released from the hospital.
A patient who has been certified as mentally disordered, but not subsequently found to be mentally ill, cannot be detained for more than 3 days and must be examined by an authorized medical officer at least once every 24 h and discharged if no longer mentally ill or disordered or if appropriate and less restrictive care is available. New South Wales legislation involves several checks and balances, including timely and regular Mental Health Review Tribunal assessment for all patients recommended for involuntary care.
New Zealand
In New Zealand, a person aged 18 years or over may request an assessment by the area mental health service if it has seen the person within the last 3 days and believes the person to be suffering from a mental disorder. The request may be accompanied by a certificate from a doctor who has examined the ‘proposed patient’ within the preceding 3 days and who believes that the person requires compulsory assessment and treatment. The medical certificate must state the reasons for the opinion and that the patient is not a relative. The area mental health service must then arrange an assessment examination by a psychiatrist or other suitable person forthwith. If the assessing doctor considers that the patient requires compulsory treatment, the patient may be detained in the ‘first period’ for up to 5 days. Subsequent assessment may result in detention for a ‘second period’ of up to 14 more days, after which a ‘compulsory treatment order’ must be issued by a family court judge.
Northern Territory
Any person with a genuine interest in or concern for the welfare of another person may request an assessment by any medical practitioner to determine if that person is in need of treatment under the Northern Territory Mental Health Act. The assessment must then occur as soon as practicable and a subsequent recommendation for psychiatric examination made if the doctor believes that the person fulfils the criteria for involuntary admission on the grounds of mental illness or mental disturbance. The person may then be detained by police, ambulance officers or the doctor making the recommendation and taken to an approved treatment facility, where the person may be held for up to 12 h. The Northern Territory Act acknowledges that delays in this process are likely and enshrines a process to account for this, including the use of interactive video conferencing. A psychiatrist must examine and assess the recommended person at the approved treatment facility and must either admit as an involuntary patient or release the patient if the criteria for involuntary admission are not fulfilled.
A patient admitted on the grounds of mental illness may be detained for 24 h or 7 days if the recommending doctor was also a psychiatrist. Patients admitted on the grounds of mental disturbance may be detained for 72 h or have that extended by 7 days if two examining psychiatrists believe that the person still requires involuntary treatment and cannot or will not consent. Frequent psychiatric reassessment of detained and admitted patients is required to either extend admission or release patients who do not fulfil involuntary criteria.
Queensland
In Queensland, the recommendation for involuntary assessment of a patient must be made by a doctor who has personally examined the patient within the preceding 3 days and is valid for 7 days from the time the recommendation was made. The recommendation needs to be accompanied by an ‘application’ for assessment made by a person over the age of 18 years who has seen the patient within 3 days. The person making the application cannot be the doctor making the recommendation or be a relative or employee of the doctor. The recommendation enables the health practitioner, ambulance officer or police, if necessary, to take the patient to a mental health service or public hospital for assessment. Once there, or if the recommendation was made at a hospital, the assessment period lasts for no longer than 24 h.
The patient must be assessed by a psychiatrist (who cannot be the recommending doctor) as soon as practicable and, if the treatment criteria apply, will have the involuntary status upheld through an involuntary treatment order. The assessment period can be extended up to 72 h by the psychiatrist after regular review.
South Australia
In South Australia, a doctor or trained authorized health professional (who may be a nurse, allied or aboriginal health worker) who considers that a patient requires involuntary admission authorizes a Level 1 Detention and Treatment Order, which is valid for 7 days. A psychiatrist or authorized medical practitioner (senior psychiatry registrar) must examine the person within 24 h or as soon as practicable.
In recognition of the difficulties in accessing appropriate care for people in remote and rural environments, the South Australian Mental Health Act allows for audiovisual conferencing and a range of community and inpatient based treatment orders. A wider range of health professionals can authorize treatment orders so that early access to care in the least restrictive environment can occur.
Tasmania
In Tasmania, an application for involuntary admission of a person may be made by a close relative or guardians or an ‘authorized officer.’ A medical practitioner must then assess the person and, if satisfied that the criteria are met, make an order for admission and detention as an involuntary patient in an approved hospital. This initial ‘assessment order’ is valid for 72 h and gives authority for the patient to be taken to the hospital and detained, whereupon a psychiatric assessment must be carried out within 24 h and the assessment order extended for up to 72 h or discharged. A ‘treatment order’ for the continuing detention of a person as an involuntary patient can only be made by application (including an individualized treatment plan) through an independent tribunal.
Victoria
A person may be admitted to and detained in an approved mental health service once the ‘request’ and the ‘recommendation’ have been completed. The request can be completed by any person over 18 years of age, including relatives of the patient, but cannot be completed by the recommending doctor. The recommendation is valid for 3 days after completion and the recommending doctor must have personally examined or observed the patient.
The request and recommendation are sufficient authority for the medical practitioner, police officer or ambulance officer to take the person to a mental health service or to enter premises without a warrant and to use reasonable force or restraint in order to take the person to a mental health service. Prescribed medical practitioners (psychiatrists, forensic physicians, doctors employed by a mental health service, the head of an ED of a general hospital or the regular treating doctor in a remote area) are also enabled to use sedation or restraint to enable a person to be taken safely to a mental health service.
Once admitted, the patient must be seen by a medical practitioner employed by the mental health service as soon as possible, but must be seen by a registered psychiatrist within 24 h of admission. The admitting doctor must make an involuntary treatment order, which allows for the detention of the patient until psychiatrist review and the urgent administration of medication if needed. The psychiatrist can then either authorize further detention, a community treatment order or discharge the patient.
Western Australia
In Western Australia, a person who requires involuntary admission is referred, in writing, for examination by a psychiatrist in an authorized hospital. The referring doctor or authorized mental health practitioner must have personally examined the person within the previous 48 h and may also make a detention and/or transport order which allows safe transport involving the police or ambulance personnel if required. These orders are valid for up to 72 h, although there are provisions for time extensions outside the metropolitan area.
The referral for assessment is valid for 72 h (although this can also be extended); however, the patient must be examined by a psychiatrist within 24 h of admission and cannot be detained further if not examined. The patient can be detained for further assessment for up to 72 h after initial admission on the order of the psychiatrist, after which time the patient is formally admitted as an involuntary patient, discharged on a community treatment order or released.
Persons unable to recommend a patient for involuntary admission
New Zealand and most states, except for the ACT, specify that certain relationships prevent a doctor from requesting or recommending a patient for involuntary admission.
The recommending doctor cannot be a relative (by blood or marriage) or guardian of the patient and, in addition, in the Northern Territory, Queensland, Tasmania and Western Australia, the doctor cannot be a business partner or assistant of the patient. In Queensland and Tasmania, the recommending doctor cannot be in receipt of payments for the maintenance of the patient.
In New South Wales, the doctor must declare, on the schedule, any direct or indirect pecuniary interest, or those of their relatives, partners or assistants, in a private mental health facility. In Western Australia, the doctor cannot hold a licence from or have a family or financial relationship with the licence holder of a private hospital in which the patient will be treated, nor can the doctor be a board member of a public hospital treating the patient.
Use of sedation or physical restraint
From time to time a patient may need to be sedated or even restrained. The various mental health acts vary considerably in dealing with this issue and accepted clinical practice has evolved differently in each jurisdiction and does not necessarily reflect subtleties within the legislation.
Generally, patients committed involuntarily are subject to treatment necessary for their care and control and this may reasonably include the administration of sedative or antipsychotic medication as emergency treatment. In general, sedation or restraint must be the minimum that is necessary to prevent the patient from self-harming or harming others and careful documentation of the reasons for restraint and the types of restraint is required. While restrained, access to clothing, sustenance, toilet facilities and other basic comforts must be assured.
Patients who are physically or pharmacologically restrained must be closely supervised and not left alone or in the care of persons not trained or equipped to deal with the potential complications of these procedures. Transporting these patients to a mental health service should be done by suitably trained medical or ambulance staff and not delegated to police officers or other persons acting alone.
The ACT specifies that sedation may be used to prevent harm, whereas Western Australia specifies that sedation can be used for emergency treatment without consent and that the details must be recorded in a report to the Mental Health Review Board. Queensland allows a doctor to administer medication for recommended patients without consent to ensure safety during transport to a health facility.
Victoria specifically permits the administration of sedative medication by a ‘prescribed medical practitioner’ to allow for the safe transport of a patient to a mental health service. There is a schedule to complete if this is undertaken. The South Australian law stipulates that medication can only be used for therapeutic purposes and that chemical, physical restraint and seclusion is to be used as a last resort for safety reasons and not as a punishment or for the convenience of others.
The legislation is more specific with regard to the use of physical restraint or seclusion. In the ACT, this can be done to prevent an immediate and substantial risk of harm to the patient or others or to keep the patient in custody.
Queensland requires that restraint used for the protection of the patient or others can only be done on an ‘order’ but is permissible for the purposes of treatment if it is clinically appropriate. Victoria permits the restraint of involuntary patients for the purposes of medical treatment and the prevention of injury or persistent property destruction. Victoria also allows the use of restraint by ambulance officers, police or doctors in order to safely transport the patient to a mental health service, but this must be documented in the recommendation schedule. Tasmania differentiates between chemical restraint and chemical treatment and allows for both chemical and physical restraint as emergency short-term interventions to prevent harm, damage or interference, break up an affray or facilitate transport. The Chief Civil Psychiatrist is required to develop standing orders for clinical use regarding these issues.
Both the Northern Territory and Western Australia permit the use of restraint for the purposes of medical treatment and for the protection of the patient, other persons or property. In Western Australia, this authorization must be in writing and must be notified to the senior psychiatrist as soon as possible, while in the Northern Territory, it must be approved by a psychiatrist or the senior nurse on duty in the case of an emergency.
The New Zealand Mental Health Act makes minimal specific reference to restraint or sedation but enables any urgent treatment to protect the patient or others and allows hospitals and police to take all reasonable steps to detain patients for assessment and treatment. Authority is given to administer sedative drugs if necessary, but the Act mandates a record of this for the area mental health service.
New South Wales has a Reference Guide specifically for mental health issues in the ED which covers sedation and restraint issues. The law permits the use of involuntary sedation for acute behavioural disturbance in an emergency situation in order to prevent individual death or serious danger to the health of others under the common law principle of ‘Duty of Care’. The same applies for children, although consent should be sought from both children or adolescents and their parents or guardians. For the use of physical restraints, although acknowledged as a clinical decision, four pre-conditions must be met:
Emergency treatment and surgery
On occasions, involuntary patients may require emergency medical or surgical treatment. New Zealand and most states, except for Queensland, make provision for this in their legislation, in that patients can undergo emergency treatment without consent, but usually only with the approval of the relevant mental health authorities or treating psychiatrist. In New Zealand, treatment that is immediately necessary to save life, prevent serious damage to health or prevent injury to the person or others can be undertaken without consent.
Victoria has the most specific reference to this treatment by making special allowance for a patient requiring treatment that is life sustaining or preventing serious physical deterioration to be admitted as an involuntary patient to a general hospital or ED for the purposes of receiving treatment. The patient is deemed to be on leave from the mental health service and all the other provisions of the Act apply.
Apprehension of absent involuntary patients
Involuntary patients who escape from custody or who fail to return from ‘leave’ are considered in most state mental health acts to be ‘absent without leave’ (AWOL) or ‘unlawfully at large’. Authorized persons, including ambulance officers, mental health workers and police, have the same powers of entry and apprehension as for other persons to whom a recommendation or certificate relates.
In New Zealand, any compulsory patient who becomes AWOL may be ‘retaken’ by any person and taken to any hospital within 3 months of becoming absent. If not returned after 3 months the patient is deemed to be released from compulsory status.
Powers of the police
The police in all states and New Zealand have powers in relation to mentally ill persons who may or may not have been assessed by a doctor. For someone who is not already an involuntary patient and who is reasonably believed to be mentally ill, a risk to self or others and requiring care, police are able to enter premises and apprehend, without a warrant, and to use reasonable force if necessary, in order to remove the person to a ‘place of safety’. Generally, this means taking the person to a medical practitioner or a mental health service for examination without undue delay.
South Australia and Queensland specifically include ambulance or other authorized officers within this legislation and acknowledge that they often work together with police to detain and transport people for mental health assessment. In Tasmania, people may only be held in protective custody for the purposes of medical assessment for no longer than 4 h and then released if no involuntary assessment order has been made. The ACT law is moving towards replacing police with ambulance paramedics in the role of emergency apprehension and transport to hospital for assessment.
Some states (ACT, New South Wales and Victoria) make special mention of a threatened or actual suicide attempt as justification for police apprehension and transfer to a health facility. New South Wales allows police discretion after a person who appears mentally disordered has committed an offence (including attempted murder), to determine whether it is beneficial to their welfare to be detained under the mental health act rather than under other criminal law. The Victorian and South Australian Acts, in contrast, acknowledge that police do not need clinical judgement about mental illness but may exercise their powers based on their own perception of a person’s appearance and behaviour that may be suggestive of mental illness.
In New Zealand, detention by police is limited to 6 h, by which time a medical examination should have taken place. Ideally, police should not enter premises without a warrant, if it is reasonably practicable to obtain one.
The same powers apply to involuntary patients who abscond or are absent without leave, although some states have specific schedules or orders to complete for this to be done. In general, once police become aware of the patient they are obliged to make attempts to find and return them to what can be viewed as lawful custody.
Prisoners with mental illness
Mental illness among people in prison is extremely prevalent, either as a cause or as a result of incarceration. New Zealand and most Australian states and territories include provisions for prisoners with mental illness within their mental health legislation. While the healthcare of prisoners is generally managed within regional forensic systems, EDs in rural and less-well-resourced areas can become a site of care for prisoners with acute psychiatric illness.
The New Zealand Act states that prisoners with mental illness who require acute care can be transferred to a general hospital for involuntary psychiatric treatment if the prison is unable to provide that care. Australian Acts in New South Wales, the Northern Territory and Victoria all include similar specific provisions for mentally ill prisoners to be able to access involuntary care in public hospitals if needed. New South Wales has separate legislation specifically dealing with mental illness in the forensic setting (NSW Mental Health [Forensic Provisions] Act 1990), while the Tasmanian Act includes a large section involving the admission, custody, treatment and management of forensic patients within secure mental health units. The Victorian Act has some detail in this matter although, in practice, rarely relies on public hospitals due to the development of a stand alone forensic psychiatric hospital. Both Queensland and Western Australia enshrine the same principle of allowing prisoners access to general psychiatric treatment, although their legislation is less specific, while the South Australian Act does not mention prisoners at all. The ACT will incorporate care for prisoners with mental illness in their new Act, emphasizing concern for the community who may be affected by prisoners with mental illness, improving communication between forensic and health services and allowing prisoners with mental illness access to appropriate healthcare. In all jurisdictions, there is significant overlap with other laws such as Crimes and Prisons Acts, which also mention health needs of prisoners.
Offences in relation to certificates
Most states and New Zealand specify in their respective mental health acts that it is an offence to make wilfully a false or misleading statement in regard to the certification of an involuntary patient.
Some states (New South Wales, South Australia, the Northern Territory and Victoria), except in certain circumstances, also regard failure personally to examine or observe the patient as an offence.
Protection from suit or liability
New Zealand and all Australian states specify in their Mental Health Acts that legal proceedings cannot be brought against doctors acting in good faith and with reasonable care within the provisions of the Mental Health Act relevant to their practice.
Information and patient transfer between jurisdictions
All Australian states and territories include special provisions for the apprehension, treatment and transfer of mentally ill patients from other jurisdictions. State governments can enter into agreements to recognize warrants or orders made under ‘corresponding law’ in other states or territories, as long as appropriate conditions are met within their own law. Thus, a patient under an involuntary detention or community treatment order in another state can be apprehended and treated under the corresponding law in a different jurisdiction. Authority is given to police and doctors to detain such patients and information to facilitate assessment and treatment can be shared between states.
Deaths
Involuntary patients should be considered to be held in lawful custody, whether in an ED, as an inpatient in a general hospital or psychiatric hospital or as an AWOL. As such, the death of such a patient must be referred for a coroner’s investigation.
25.2 The coroner: the Australasian and UK perspectives
Robyn Parker and Jane Terris
Australasia
Introduction
The function of the coroner is to investigate and report the circumstances surrounding a person’s death. A coronial inquest is a public inquiry into one or more deaths conducted by a coroner within a court of law. Legislation in each Australian state and territory defines the powers of this office and the obligations of medical practitioners and the public towards it. The process effectively puts details concerning a death on the public record and is being increasingly used to provide information and recommendations for future injury prevention.
As many people die each year either in an emergency department (ED) or having attended an ED during their last illness, it is almost inevitable that emergency physicians will become involved in the coronial process at some stage during their career. Such involvement may be brief, such as the discharge of a legal obligation by reporting a death, or may extend further to providing statements to the coroner regarding deaths of which they have some direct knowledge. Later, the coroner may require them to appear at an inquest to give evidence regarding the facts of the case and, possibly, their opinion. Occasionally, the coroner requires a suitably experienced emergency physician to provide an expert opinion regarding aspects of a patient’s emergency care.
Although the inquisitorial nature of the coronial process is sometimes threatening to medical practitioners, their involvement is a valuable community service. In addition, they may obtain important information regarding aspects of a patient’s clinical diagnoses and emergency care which may improve the provision of emergency care to future patients.
Legislation
The office of the coroner and its functions, procedures and powers is created by state and territory legislation. The legislation also creates obligations on medical practitioners to notify the coroner of reportable deaths and to cooperate with the coroner by providing certain information in the course of an inquiry. The normal constraints of obtaining consent for the provision of clinical information to a third party do not apply in these circumstances.
The coroner is vested with wide-ranging powers to assist in obtaining information. In practice, the police are most commonly used to conduct the investigation. Under the various Coroners Acts they have the power to enter and inspect buildings or places, take possession of and copy documents or other articles, take statements and subpoena people to appear in court. The coroner has control of a body whose death has been reported and may direct that an autopsy be performed.
As each Australian state and territory legislation is different, emergency physicians must be familiar with the details in their particular jurisdiction. The current legislation in each state and territory is the following:
Reportable deaths
Most deaths that occur in the community are not reported to a coroner and, consequently, are not investigated. The coroner has no power to initiate an investigation unless a death is reported, but may choose to investigate the death at the request of a next of kin or a person who registers themselves as an interested party. If a medical practitioner is able to issue a medical certificate of the cause of death, the Registrars-General of that state or territory may issue a death certificate and the body of the deceased may be lawfully disposed of without coronial involvement.
In general, to issue a certificate of the cause of death, a doctor must have attended the deceased during the last illness and the death must not be encompassed by that jurisdiction’s definition of a reportable death. It is essential that every medical practitioner has a precise knowledge of what constitutes a reportable death within the jurisdiction.
It is uncommon for a doctor who is working in an ED to have had prior contact with a patient during the last illness. Therefore, even if sure of the reason why the patient died, the doctor is often unable to complete a medical certificate of the cause of death. It is quite permissible, and even desirable, under these circumstances, to contact the patient’s treating doctor to inquire as to whether that doctor is able to complete the certificate. This process reduces the number of deaths that must be reported and assists families who may be distressed about coronial involvement.
All Australian Coroners Acts contain a definition of the deaths that must be reported. Although the precise terminology varies, there are many similarities between them. In general, each Act has provisions for inquiring into deaths that are of unknown cause or that appear to have been caused by violent, unnatural or accidental means. Many acts also refer to deaths that occur in suspicious circumstances and some specifically mention killing, drowning, dependence on non-therapeutic drugs and deaths occurring while under anaesthesia. The Tasmanian Act goes further to specify deaths that occur under sedation.
As an example, the Victorian Coroners Act 2008 defines a reportable death as a death that is unexpected, unnatural or violent or resulting from an accident or injury. The definition has also been widened to include a death during or after a medical procedure where a doctor would not reasonably have expected the person to die. ‘Medical procedure’ is defined broadly to include ‘imaging, internal examination and surgical procedure’. A reportable death under the Act of 2008 is also the death of a person placed in custody, including deaths involving police or prison officers attempting to take a person into custody.
Despite the seemingly straightforward definitions given in the various acts, there are many instances where it may not be clear whether a death is reportable or not. Emergency physicians are often faced with situations where there is a paucity of information regarding the circumstances of an event and where the cause of death may be difficult to deduce. Correlation between the clinical diagnoses recorded on death certificates and subsequent autopsies has been consistently shown to be poor. What exactly constitutes unexpected, unnatural or unknown is open to debate and may require some judgement. In all cases, the coroner expects the doctor to act with common sense and integrity. If at all in doubt it is wise to discuss the circumstances with the coroner or assistant and to seek advice. This conversation and the advice given must be recorded in the medical notes.
The process of reporting a death is generally a matter of speaking to the coroner’s assistants (often referred to as coroner’s clerks), who will record pertinent details and, if necessary, investigate. The report should be made as soon as practicable after the death. A medical practitioner who does not report a reportable death is liable to a penalty.
Even though coroners’ offices and the police work closely together, reporting a death to the coroner is not necessarily equivalent to reporting an event to the police. If it is possible that a person has died or been seriously injured in suspicious circumstances, then it is prudent to ensure that the police are also notified.
A coronial investigation
After a death has been reported, the coroner or designated assistant may initiate an investigation. This is most commonly conducted by the police assisting the coroner, with an autopsy conducted by a forensic pathologist.
The body, once certified dead, becomes part of that investigation and should be left as far as possible in the condition at death. If the body is to be viewed by relatives immediately, it is often necessary to make it presentable. This must be done carefully, so as to not remove or change anything that may be of importance to the coroner. If a resuscitation was attempted all cannulae, endotracheal tubes and catheters should be left in situ. All clothing and objects that were on (or in) the deceased should be collected, bagged and labelled. All medical and nursing notes, radiographs, electrocardiographs and blood tests should accompany the body if it is to be transported to a place as directed by the coroner.
Medical notes taken during or soon after the activity of a busy resuscitation are often incomplete. It is not easy to recall accurately procedures, times and events when the main task is to prevent someone from dying. Similarly, after death there are many urgent tasks, such as talking to relatives, notifying treating or referring doctors and debriefing staff. It is essential, however, that the documentation is completed as accurately and thoroughly as possible. The notes must contain a date and time and clearly specify the identity of the author. If points are recalled after completing the notes, these may be added at the end of the previous notes, again with a time and a date added. Do not under any circumstances change or add to the body of the previous notes.
In addition to completing the medical notes, a medical practitioner may be requested to provide a statement to the coroner regarding the doctor’s involvement with the deceased and an opinion on certain matters. Such a statement should be carefully prepared from the original notes and written in a structured fashion, using non-medical terminology where possible. The statement often gives the opportunity for the medical practitioner to give further information to the coroner regarding medical qualifications and experience, the position fulfilled in the department at the time of the death and a more detailed interpretation of the events. If a statement is requested from junior ED staff, it is strongly advisable for these to be read by someone both clinically and medicolegally experienced.
Providing honest, accurate and expeditious information to relatives when a death occurs assists in preventing misunderstandings and serious issues arising in the course of a coronial investigation. Relatives vary enormously in the quantity and depth of medical information they request or can assimilate after an unexpected death. It is wise not only to talk to the relatives present at the death but also to offer to meet later with selected family members. Clarification with the family of what actually occurred, what diagnoses were entertained and what investigations and procedures were performed is not only good medical practice but can allay concerns regarding management. Such communication, as well as aiding in the grieving process for relatives of the deceased, may avert an unnecessary coronial investigation initiated by relatives seeking answers about the death by contacting the coroner.
If a significant diagnosis was missed or inappropriate or an inadequate treatment given, or a serious complication of an investigation or procedure occurred, assistance and advice from the hospital insurers and medical defence organizations should be sought before talking to the family. However difficult it may be, it is far better that the family is aware of any adverse occurrences before the inquest than for them to harbour suspicions or to get a feeling something is being covered up. Such a conversation should be part of an open disclosure approach to patient care, involving open communication with a patient or family following an adverse or unexpected event. The coroner is far more likely to be sympathetic to a genuine mistake or omission when it has been discussed with the family and the hospital has taken steps to prevent a recurrence.
Expert opinion
Having gathered all the available information regarding a death, the coroner may decide that expert opinion is necessary on one or more points. Commonly, this involves the standard of care afforded to the deceased. It may, however, also include issues such as the seniority of doctors involved, the use of appropriate investigations, the interpretation of investigations and the occurrence of complications of a procedure. The coroner relies heavily on such opinions for the findings and the selection of an appropriate expert is essential.
The person selected by the coroner to give this opinion should possess postgraduate specialist medical qualifications and be broadly experienced in the relevant medical specialty. For events occurring in the ED, a senior emergency physician with over 5 years of experience is usually most appropriate. The specialist medical colleges may be requested to nominate such a person.
The emergency physician requested to give expert opinion must be able to review all of the available relevant information. Such persons must also consider themselves adequately qualified and experienced to provide an opinion and to answer any specific questions the coroner may have requested to be addressed. The doctor must have the time and ability to provide a comprehensive statement and to appear as a witness at the inquest if requested and to act impartially. The doctor should decline involvement if an interest in the outcome of the case could be implied or if there is a close relationship between the expert witness and any doctors or other personnel who are being investigated as part of the coronial process. Because of the close-knit nature of the medical community, an expert witness is often sought from a location remote from where the death occurred, such as interstate.
A coronial inquest
A coronial inquest is a public inquiry into one or more deaths. Deaths may be grouped together if they occurred in the same instance or in apparently similar circumstances. The purpose of the inquest is to put findings on the public record. These may include the identity of the deceased, the circumstances surrounding the death, the medical cause of death and the identity of any person who contributed to the death. The coroner may also make comments and recommendations concerning matters of health and safety. In some jurisdictions these are termed ‘riders’. In addition, as His Honour BR Thorley pointed out, the inquest serves to:
…include the satisfaction of legitimate concerns of relatives, the concern of the public in the proper administration of institutions and matters of public and private interest…
The inquest does not serve to commit people for trial or to provide information for a subsequent criminal investigation.
With broad terms of reference and the ability to admit testimony that may not be allowed in criminal courts, inquests interest many people, not only those who may have been directly involved. They are often highly publicized media events and may provoke political comment, especially where government bodies are involved. A medical practitioner served a subpoena to attend should prepare carefully, both individually and in conjunction with the hospital, and should ensure that he or she has legal representation, either individually or through the hospital insurers. Where the doctor subpoenaed is being provided legal counsel by the hospital, it is vital to ensure that the hospital administrators support the actions of the doctor in relation to the death. It is advised that, in the event of being subpoenaed to a coronial inquest, the doctor seek advice immediately from the appropriate medical defence agency.
Preparation for an inquest begins at the time of the death. Complete and accurate medical notes, together with a carefully considered statement, provide a solid foundation for giving evidence and handling any subsequent issues. Statements containing complex medical terminology, ambiguities or omissions only serve to create confusion. Discuss the case with colleagues who are not directly involved and have the hospital lawyers read the statement before it is submitted.
Appearing at an inquest can be a stressful event, especially if, on a review of the circumstances, a doctor’s actions or judgement may be called into question. Professional peer support, as well as legal advice, should be offered to all medical staff. Simple actions, such as a briefing on court procedures and some advice on how to deal with cross-examination, can be of immense value.
A coroner’s court is conducted with a mix of ‘inquisitorial’ and ‘adversarial’ legal styles. It is inquisitorial in that the coroner may take part in direct proceedings and can question witnesses and appoint court advisers. It is adversarial in that parties with a legitimate interest can be represented in proceedings and can challenge and test witnesses’ evidence, especially where it differs from what they would like presented. Interested parties generally attend court and can ask any questions of the doctor through their own legal representative or through the police counsel to the coroner. The ‘rules of evidence’ are more relaxed in the coroner’s court than in a criminal court. Hearsay evidence – that is, evidence of what someone else said to a witness – is generally admissible. Despite these differences, it is important to remember that it is no less a court than a criminal court and demands the same degree of respect and professional conduct one would accord to the latter.
Coronial findings
At the conclusion of an inquest, the coroner makes a number of findings directed at satisfying the aims of that inquest. These findings are made public and are often of interest to those who are directly involved, as well as to a wider audience.
The findings of an inquest in which the conduct of a particular emergency physician, ED or hospital has been scrutinized will be of particular interest. Although it is always pleasing to have either positive or a lack of negative comment delivered in the finding, criticism of some aspect of the conduct of an individual, department, hospital or the medical system in general is not uncommon. Unfortunately, it is often this criticism that attracts the most public attention and, somewhat unfairly, the public perception of our acute healthcare system is shaped by the media’s attention to coronial findings.
In the recent past, coroners have commented on inadequate training, experience and supervision of junior doctors, inadequate systems of organization within departments and poor communication between doctors and family members.
Although adverse or critical findings have no legal weight or penalties attached to them, they are in many respects a considered community response to a situation in which the wider population has a vested interest. Used constructively, they can be extremely useful in convincing hospital management that a problem exists and beginning a process for effecting positive change within a department or institution.
The UK
Introduction
The investigation into the circumstances surrounding a death is an important part of a civilized society. Accurate recording of the cause of death serves many purposes, including accurate disease surveillance, the detection of secret homicide and the detection of potentially avoidable factors that have contributed to a death. Various death investigation systems exist around the world. The UK uses the coronial system, Scotland the procurator fiscal. By virtue of the patient population encountered by emergency physicians and the types of deaths that are subject to investigation, emergency physicians may expect to find themselves in contact with either the coroner or the procurator fiscal system during their working lives, thus necessitating an understanding of the workings of these systems.
History of the coroner
The history of the coroner’s office is an interesting reflection of events that shaped our civilization and is in constant evolution. The Shipman Inquiry (2003) and the Fundamental review of Death Certification and Investigation (2003) identified problems within the services available to bereaved families and the process of death certification and led to a reform of the system in the UK in the form of the Coroners and Justice Act 2009.
The office of the coroner was established in 1194 and its primary function then was that of protection of the crown’s pecuniary interests in criminal proceedings. The coroner was involved when a death was sudden or unexpected or a body was found in the open; however, aside from the duty to ensure the arrest of anyone involved in homicide, the coroner held a significant role in the collection of the deceased’s chattels and collection of various fines [1].
Introduction of the Births and Deaths Registration Act in 1836, mandated registration of all deaths before burial could legally occur. This may have arisen out of concern regarding accurate statistical information concerning deaths, but also concern about hidden homicide. Another act introduced the same year enabled coroners to order a medical practitioner to attend an inquest and perform an autopsy in equivocal cases. The Coroners Act of 1887 saw a shift of emphasis from protection of financial interests to the emphasis that remains today, namely the medical cause of death and its surrounding circumstances with eventual community benefit in mind.
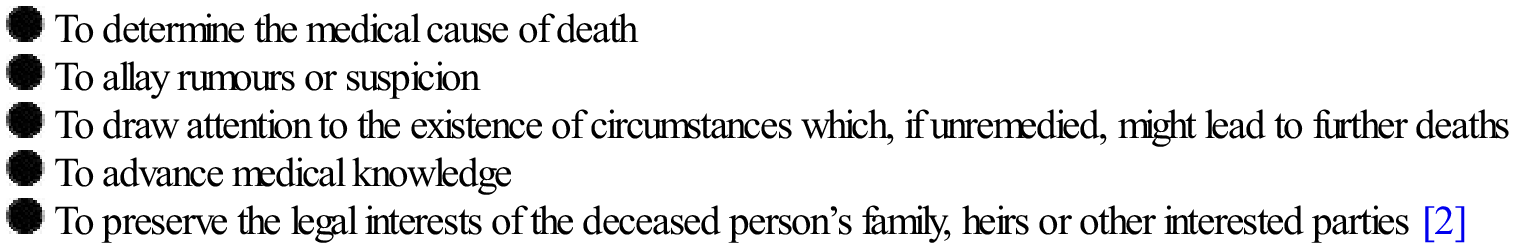
The Broderick committee was appointed in 1965 to review death certification in response to adverse publicity about inquests and pressures to improve death certification. Their report published in 1971 contained 114 recommendations, many of which were enacted. Table 25.2.1 lists the reasons the Broderick Committee considered the purpose of an inquest [2].
Table 25.2.1
Reasons for an inquest (according to the Broderick committee)
The Coroners Act (1988) states that a coroner shall hold an inquest into a death when there is:
…reasonable cause to suspect that the deceased has died a violent or unnatural death, has died a sudden death of which the cause is unknown, or has died in prison or in such a place or circumstances as to require an inquest under any Act [3].
The Coroners and Justice Act 2009 introduced changes to the structure and appointment system for coroners, more flexibility between working areas of coroners and the mandate for all coroners to have held a legal qualification for 5 years, which was intended to standardize practice and ensure sufficient legal understanding for coroners. The new appointment of a chief coroner, with a senior legal background, and with annual reporting to the government, was recommended to be responsible for establishing national training and governance standards and developing a charter for improving services to bereaved families. The death certification system under the Act was modified to provide consistency whether the body is buried or cremated and to ensure that adequate scrutiny of the circumstances around the death happens and is documented. The introduction of a medical examiner attached to a primary care trust to scrutinize all death certificates prior to burial or cremation replaced the previously medically unqualified registrar.
Structure of the coroner system in the UK
Coroners are independent judicial officers who have a legal background, including having been a qualified barrister or solicitor for at least 5 years and, in addition, some may also have a medical background. They are responsible to the Chief Coroner, a senior legal practitioner who must have previously held the position of high court or circuit judge and, ultimately, is responsible to the Crown through the Lord Chancellor. They must work within the laws and regulations that apply to them: The Coroners and Justice Act 2009 replaced the previous framework as described in The Coroners Act 1988, Coroners Rules 1984 and the Model Coroners Charter. There are approximately 148 coroner’s districts throughout England and Wales and each district has a coroner and a deputy and possibly several assistant deputy coroners. Coroners are assisted in their duties by coroner’s officers, who are frequently police officers or ex-police officers and whose work is dedicated solely to coronial matters. This follows long-established practice and has probably arisen because of the significant proportion of cases in which police are the notifying agent. The nature of a coronial investigation requires a person to possess knowledge about legal matters and skill in information gathering. From a practical viewpoint, the coroner’s assistants may be responsible for performing such duties as attending the scene of a death, arranging transport of the body to the mortuary, notification of the next of kin and obtaining statements from relevant parties. Clearly, variation in the structure of the service between regions is inevitable and reflects the size, composition and workload within the district [4].
The 2009 reforms to the coronial process
The UK coronial system underwent fundamental changes following the Coroners and Justice Act 2009, which constituted the first major reforms of the existing system for over 100 years. It included changes to the investigation process for certain deaths previously governed by the Coroners Act 1988.There were also reforms of the certification and registration of deaths. The need for reform was galvanized by several landmark cases including the Shipman Inquiry (2003), in which the system had not identified and isolated a pattern of criminal activities spanning years by the UK GP Dr Harold Shipman, and the Fundamental Review of death Certification and Investigation (2003) which revealed a number of problems and inconsistencies in the process of death certification and the services available to bereaved relatives. Other findings prompting reforms included a lack of leadership and training for coroners and a perceived deficiency of medical knowledge within the system. The structure, training and appointment systems for coroners were changed to include a Chief Coroner, improved training and guidance for coroners, who have to be legally qualified, and powers allowing evidence to be obtained, with search and entry where necessary. Changes to the process for issuing a death certificate include the replacement of a non-medically qualified registrar with a Medical Examiner, reporting to a Chief Medical examiner, who scrutinizes and, if necessary, recommends investigation, following the issuing of the death certificate.
Outline of the coronial system
Upon notification of a death, the coroner makes initial inquiries and may direct a pathologist, who is generally a specialist forensic pathologist, to perform a post-mortem autopsy. Sometimes it becomes clear at this early point that the death is a natural one and does not fall within the Coroners Act, thus no further investigation is required and a death certificate is issued. In other circumstances, further investigations occur and relevant information is gathered. If the coroner is subsequently satisfied that the death is natural, again no inquest is required. In other cases, or in certain prescribed circumstances, an inquest is held. At the conclusion of an inquest, a finding or verdict is delivered. This verdict must not be framed in a way that implies civil or criminal liability.
Reportable deaths
As opposed to the Australasian situation, there is no statutory obligation in the UK for a doctor or any member of the public to report certain deaths to the coroner, however, an ethical responsibility exists and it is recognized practice to do so in particular circumstances. A 1996 letter from the Deputy Chief Medical Statistician to all doctors outlined these circumstances (Table 25.2.2) [5].
Table 25.2.2
Circumstances in which a death should be reported to the coroner
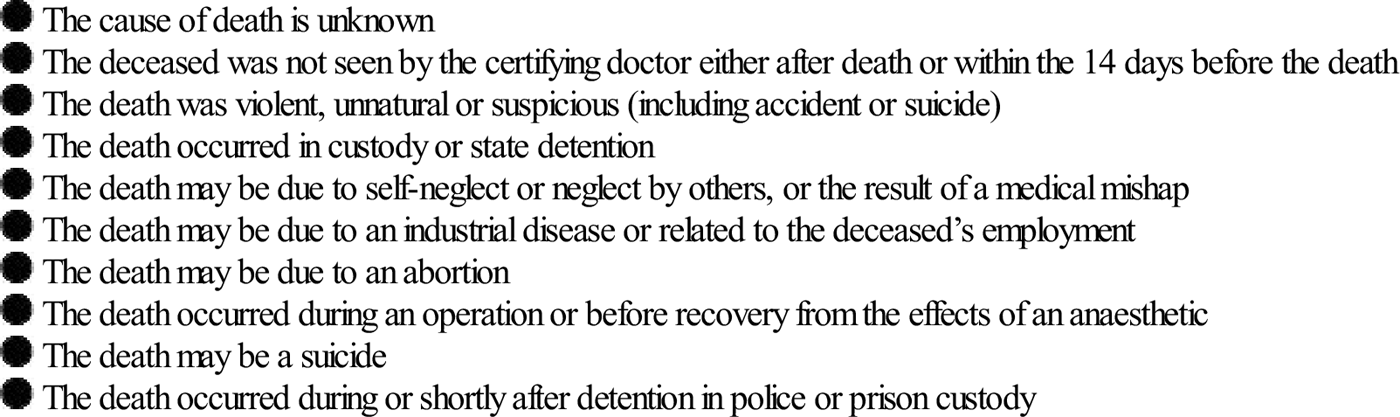
Each booklet of medical death certificates also contains a reminder of the deaths that a coroner needs to consider. The list is not exhaustive.
Scotland
In Scotland, the role of death investigation is undertaken by the procurator fiscal’s office, which is also responsible for the investigation and prosecution of crime and also has responsibility for any treasure found within the district! The registrar of births and deaths in Scotland has a statutory duty to report certain deaths, for example, those due to industrial disease and those occurring during surgery, to the procurator fiscal. The spectrum of deaths investigated is essentially the same as in England and Wales; however, more specific guidelines regarding deaths possibly related to medical mismanagement are provided (Table 25.2.3).
Table 25.2.3
Circumstances in which a death should be reported to the procurator fiscal in Scotland
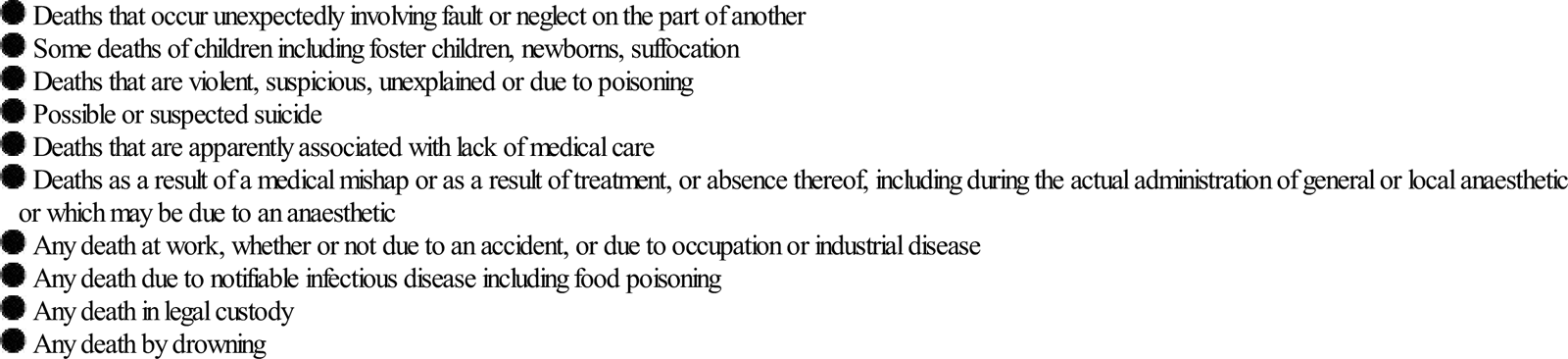
How to report a death
Having determined that a death is reportable, the emergency physician should contact the district coroner’s office and notify the details of the deceased. Where doubt exists about the necessity or otherwise to report a death, a doctor should contact that office to discuss the matter further. The discussion and subsequent decision should be recorded in the patient’s clinical notes. A death certificate should not be written at this stage.
Handling the body
There appear to be no official guidelines in place regarding handling of the body once death has been reported to the coroner; however, this aspect may be an important component of the subsequent investigation. Any therapeutic and monitoring devices, such as endotracheal tubes, intercostal catheters and intravascular catheters, should be left in situ, as determination of their correct placement or otherwise may be relevant to the death investigation. Similarly, it may be important to isolate any equipment (e.g. intravenous infusion pump devices) suspected of being faulty and contributing to the death. In circumstances of suspicious or violent deaths in particular, the body should be not be handled unnecessarily, nor should the body be washed. Important trace evidence that may be crucial for subsequent criminal proceedings could conceivably be lost. For example, in deaths involving firearms, it may be useful for a forensic scientist to swab the deceased’s hands for gunshot residue to help confirm or refute the notion of a self-inflicted injury.
Clothing removed from the deceased during resuscitation efforts should be set aside and preferably placed into individual paper bags. Any remaining clothing on the deceased should be left in situ[6]. Blood taken during resuscitation attempts, regardless of whether it was processed or not, should not be discarded, but kept refrigerated and its existence indicated to the coroner. The examination of ante-mortem blood samples can provide valuable information, particularly with respect to electrolyte and glucose concentrations, drug concentrations and, in deaths possibly attributable to anaphylaxis, tryptase assay [7].
Documentation
The clinical record of the deceased will usually accompany the body to the mortuary and is scrutinized by the pathologist. Clinical information is crucial in consideration of the cause of death and may help direct the pathologist towards an appropriately detailed examination of the relevant system or organ. The guidelines for appropriate documentation in reportable cases are the same as those that apply to medical record-keeping in general. They should be made contemporaneously or as close to as is possible in a resuscitation environment. Each entry should be dated and the time recorded. They must be legible, objective and the sources of information identified. Any errors made should be crossed out, dated and signed. Likewise, if information comes to hand or is recalled at a later date, that entry should be dated and timed. Finally, the author’s name and designation should be clear and all entries signed.
The medical certificate of cause of death (MCCD) is usually written by the medical practitioner who cared for the deceased during their last illness and then passed to a medical examiner attached to the relevant primary care department for scrutiny and investigation if required. The medical examiner may then, if satisfied, authorize burial or cremation or may request further investigation.
Information for families
The 2009 Coroners and Justice Act sought to create a charter of rights for bereaved families in response to perceptions of non-uniform and sometimes inadequate, care and information given to relatives. The next-of-kin of the deceased must be informed that the death has been reported to the coroner and the requirement or reasons for doing so. It is important to inform them that police may be involved in the investigation of the death on behalf of the coroner, but that this does not imply a criminal wrongdoing. Many coroners have a process for meeting with bereaved families to share information and answer questions about the subsequent process. An information leaflet explaining the coroner’s work and rights of the next-of-kin is available from the Home Office [8] and should be available in every ED to pass on to bereaved families. Another useful publication written for bereaved families provides information regarding post-mortems and is available from the Royal College of Pathologists [9].
Post-mortems
The coroner may decide upon the initial report of a death that a post-mortem is necessary in order to determine the cause of death or resolve an issue relevant to a coronial inquiry. In 2010, post-mortem examinations were conducted in approximately 22% of cases by the coroner or procurator fiscal, which may still be a relatively high number but represents a steady downward trend in the proportion of post-mortems conducted [10]. Having decided upon the necessity for a post-mortem, the coroner directs a pathologist to conduct a post-mortem. The Coroners Act states that, in fact, the coroner may ‘direct any legally qualified medical practitioner’ to conduct the post-mortem; however, the Coroners Rules 1984 direct that they should be performed ‘whenever practicable by a pathologist with suitable qualifications and experience’ and, in practice, most are conducted by Home Office accredited forensic pathologists. Clearly, if the standard of medical care provided by the hospital in which the death occurred is in question, it is inappropriate for a pathologist employed by that hospital to conduct the post-mortem.
Consent from relatives to conduct the post-mortem is not required in coroner’s cases. In the event that relatives object to the post-mortem examination, the coroner may delay it to allow them time to obtain legal advice. The adjunct, and sometimes alternative, to autopsy of post-mortem imaging may be seen as more acceptable if the refusal for autopsy is made on religious grounds; however, if the death does fall within the coroner’s jurisdiction and a post-mortem is deemed to be necessary, their objection would be over-ridden. Relatives may request a second post-mortem, although this seldom occurs in practice.
The coroner must, in theory, notify certain persons, including the usual medical attendant of the deceased or the hospital in which the death occurred, of the time and date of the post-mortem (Rule 7, The Coroners Rules 1984). In practice, this tends to occur when a desire to be represented at the examination has been expressed to the coroner and, in that instance, a nominated, medically qualified representative (not a doctor whose practice may be in question) may be present to observe the post-mortem.
The issue of tissue retention at autopsy has received worldwide attention. The Human Tissue Act 2004 laid down guidelines around the process of tissue and organ removal and the need for informed consent by relatives. Guidelines issued by The Royal College of Pathologists [11] recommend that, in coroner’s cases, clear protocols between the coroner and the pathologist should exist and retention of tissues outside of the above-mentioned context should occur with the agreement of both the relatives of the deceased and the coroner.
Preparing a statement for the coroner
The coroner may request a statement from a doctor involved in the care of the deceased and, while there is no obligation to comply with this request, it is generally in the doctor’s interest to do so. The coroner, otherwise, has no option but to compel the doctor to attend court and answer questions. A statement, therefore, that has been carefully prepared with due thought to any issues identified may, indeed, avert the need for an inquest or at least can act as a solid base upon which the examination in court will occur. It is important that the doctor writing the statement understands the circumstances of the death; thus, access to the post-mortem report is often vital and is allowable under Rule 57 of the Coroners Rules. It is generally advisable, except perhaps in circumstances where it is clear that simple, factual background information only is required, to seek legal advice early when requested to provide a statement or attend an inquest.
The statement should be typewritten and contain the author’s qualifications, work experience and current employment post. The sources from which the report is prepared, including clinical notes and pathology reports, should be acknowledged and it should be set out in a logical manner, in chronological order. Technical terms should be qualified with an explanation readily understood by a layperson. It is advisable to have a senior colleague review the statement before submission to the legal representative for final review. The final statement should be dated and signed and a copy kept for future reference.
Inquest
An inquest is a public hearing at which the identity of the deceased and how, when and where the deceased came by his/her death are to be determined. In 2010, only around 10% of reported deaths proceeded to inquest, the remainder being examined ‘in chambers’. Inquests (or fatal accident inquiries in Scotland) are mandatory in certain prescribed circumstances, including deaths in prison or police custody and deaths resulting from workplace incidents. In certain unusual circumstances, inquests are held with a jury that is responsible for the final verdict.
The inquest is inquisitorial in nature, where the truth surrounding the circumstances of the death is sought, rather than adversarial, where two or more parties have a particular claim to prove. As with the preparation of a statement for the coroner, it is wise for a medical witness to seek legal advice and possibly representation prior to attendance at an inquest. The legal arena in which they are held is unfamiliar territory to most doctors and they frequently attract intense media scrutiny; thus, involvement in an inquest may be a daunting and stressful experience requiring support from colleagues and friends.
25.3 Consent and competence – the Australasian and UK perspectives
Jane Terris and Edward Brentnall
Introduction
Consent is necessary for any clinical intervention performed on a patient and the higher standard of informed consent has become accepted.
Consent is an essential basis for any medical intervention and has ethical, legal and administrative elements [1].
Historically, the need for consent may have been applied more variably than today. The American physician, Oliver Wendell Jones said in 1871 to his students: ‘your patient has no more right to all the truth than he has to all the medicine in your saddle bags and should get only so much as is good for him’ [2]. Self-determination was addressed in 1914 by Justice Cardozo who said: ‘every human being of adult years and sound mind has a right to determine what shall be done with his own body’ [3]. The pendulum has recently swung in the direction of patient autonomy and informed choice to the extent that clinicians now need to go to extensive efforts to ensure that enough specific information is given to the patient prior to consent being obtained and the threat of successful litigation, although rare, serves as a potent stimulus to this.
Respect for patient autonomy is enshrined within consent law and to impose care or treatment on patients without respecting their wishes is illegal and unethical.
Consent serves to protect the patient from assault and battery, namely unwanted medical interventions. The more exacting standard of informed consent requires that the patient be given and understand adequate and appropriate information specific to the procedure or intervention to be performed. There is debate around what defines reasonable consent practice in different clinical circumstances. There is also debate around the ethical and legal interpretations of the principles underpinning informed consent, which may vary according to local jurisdiction, subjective interpretation and may, in practice, deviate from the theoretical ideal.
Legally, informed consent protects the patient from assault and protects the clinician from an allegation of assault. On an ethical level, the clinician should aim to facilitate autonomous decision making around treatment goals as jointly agreed with the patient. From an administrative point of view, consent documentation serves as proof of a systematic check that the patient received information concerning, and agreed to, the procedure undertaken. The consent form is only the documentation of consent having been obtained and should not be seen as equivalent to or a substitute for the consent process.
Consent
All medical treatment is based on legal and ethical principles. The four basic ethical principles in medicine are:
 Beneficence: the duty to do the best for the patient.
Beneficence: the duty to do the best for the patient.
 Non-maleficence: the duty to do no harm to the patient.
Non-maleficence: the duty to do no harm to the patient.
Resources may need to be rationed to ensure fair and equitable distribution and no patient has the right to demand treatment not felt to be indicated by the treating clinician.
There is a requirement that patients consent to the specific interventions proposed, provided they have sufficient information to make an informed choice and are competent to do so. It is the job of the emergency physician to ensure that the patient is sufficiently well informed to make the choices that best meet their own needs in the context of patient-centred care. Legal judgements have centred around the nature of the relevant material risks disclosed and whether the patient was actually given sufficient specific information to make an informed choice, in addition to the determination of whether a particular patient has competence in a specific situation.
The term ‘informed decision making’ is preferred by some to informed consent as it reflects consideration of patient autonomy [4]. Consent should be considered as a two-way process in emergency medicine, with an exchange of adequate and relevant knowledge between a patient and the emergency physician, or nurse in some circumstances, and the end goal should be to share the aims of treatment, although it has been suggested that the means of getting to the shared end could reasonably be guided by the clinician, if acting in the patient’s best interests. Failure to obtain informed consent can lead to prosecution. The risk of litigation is related to patient dissatisfaction due to perceived lack of clinician communication or rapport [5], therefore this should serve to build in good communication skills as an essential part of the consent process.
Consent requires the clinician to take an active role in giving information and choice, while respecting the patient’s wishes [6]. The concepts of competence, provision of adequate information and the voluntariness with which consent is given are crucial in the consideration of obtaining valid consent or seeking an informed decision. Treatment without consent may be considered an assault, although the law is generally pragmatic if the clinician is able to demonstrate that they gave the information that most reasonable patients would wish to know and acted in the best interests of the patient, in a manner that most reasonable professionals of similar clinical background and seniority would have done. Judgements may take into account whether the treatment was carried out in an emergency rather than an elective situation and documentation should aim to demonstrate the circumstances under which the decision was taken at the time. There has been debate in both Australian and UK law around what constitutes the reasonable standard of care around consent practices and whether the standard should be that which is thought to be reasonable by a responsible body of professional opinion, known as the Bolam standard [7]. The Bolam ruling was challenged in the Bolitho case [8] which ruled that even expert clinical opinion may be challenged if it was felt to be illogical and not to stand up to analysis. Legal discussion has also centred around precisely what information most patients in a particular situation would want or need to know in order to be considered adequately informed. This principle was the deciding factor in Rogers vs Whittaker [9], in which consent given by the patient was held to be invalid on the grounds of a ruling that insufficiently detailed disclosure by the surgeon did not allow the consent to be informed. Judgements are likely to be subject to location specific jurisprudence and to consideration of the urgency of the situation; however, it should be emphasized that there is a strong need to demonstrate, and to document, that the decision around gaining consent was taken in good faith, with the available evidence at the time, in the patient’s best interests.
The patient has the right to self-determination. Consent lies at the heart of the medical contract between the clinician and the patient. Medical investigation and treatment are essentially voluntary acts, which the patient consents to the clinician performing.
Consent may be given in several ways: implied, verbal or written. If the patient voluntarily presents to the emergency department then some degree of consent is implied, although consent must be specific to the intervention proposed. Simply presenting to the emergency department (ED) with a severe headache does not automatically imply consent to lumbar puncture, for example. Such a procedure would usually need sufficient explanation in order that the patient understood what was to be done and the potential consequences of not doing the procedure, before the consent was given. If a doctor says ‘put your arm out straight because I need to take some blood for a test’ then this may be taken as implied consent for venesection. Written consent is generally sought before more invasive, potentially complex or prolonged procedures, such as procedural sedation for hip relocation in ED and surgery under general anaesthetic. Written consent is not more valid than verbal consent that is documented, but is easier to prove.
Adjuncts to written consent may serve to strengthen both the patient’s understanding of the procedure and to protect the clinician. These may include procedure-specific consent forms and patient information leaflets detailing what to expect after local anaesthetic or recovery from procedural sedation.
Consent must be sought after full and relevant explanation of what is to be done and the expected results, risks and the consequences if it is not done. The explanation should, as much as possible, be balanced and realistic in describing the advantages and disadvantages of each option. To present only a one-sided option may be seen as a form of coercion. There is, however, much potential for debate on ethical and legal points of what defines full, relevant and expected. This is not surprising as the literature around informed consent comes from multiple disciplines including clinical, legal and ethical cases and judgements are open to unique interpretation.
In some ways, written consent is the most difficult to establish. It is impossible to cover every outcome and to establish statistical likelihood of those outcomes occurring in every patient. The difficulties lie with the sometimes discordant medical and legal definitions of being specific and of the patient being adequately informed. For simpler procedures, it may be better to have implied or verbal consent, rather than written consent, although every effort must be taken to record in writing details of the discussion surrounding implied and verbal consent. Consent must be informed, specific and freely given and must cover that which is actually done. Informed consent or decision making requires that clear, accurate and relevant information must be given to the patient. Legal judgements have defined the importance of considering what may be material or significant to that particular individual when disclosing information. Essentially, the patient should be provided with information regarding: (1) treatment options; (2) the foreseeable consequences and side effects of any proposed treatment or intervention; and (3) the consequences of not proceeding with the advised treatment. This information should be conveyed in unambiguous terms and in a manner that is likely to be understood by the patient. Language and other communication needs must be met and there must be an opportunity for the patient to ask questions and to reflect on the information given.
The information should be given by the clinician responsible for the intervention or a delegate who is suitably qualified and has sufficient knowledge of the proposed intervention. It is appropriate for a doctor to give advice as to the best clinical options and for the reasons for this professional opinion. Such an opinion is frequently expected and desired by patients and cannot be considered as coercive unless the information has been presented in a manipulative fashion in order to elicit a particular choice. It is important to avoid subtle forms of information bias, for instance, presenting the patient with only the benefits of having a fracture reduced on an operative list under general anaesthetic in order to minimize workflow disruption in ED, without the relevant statistics of complications of general anaesthetic versus those of procedural sedation in the ED.
In Australia, it is common practice for hospitals to assist staff in making their communications contextual and understanding the unique needs and preferences of indigenous patients.
In New Zealand, the Treaty of Waitangi [10] creates a particular specification in relation to Maori, whereupon doctors may be expected to include the extended family in decision making and to allow the family to be present with the patient. There are other cultures that may have similar expectations within the multicultural environments of both Australasia and the UK.
Competence
The terms ‘competence’ and ‘capacity’ are often used interchangeably in the context of informed consent. The patient must be competent to give the consent or to refuse.
For consent to be valid, it must be given by a person who has the capacity to make that decision which, generally, will be the patient. The default assumption should be that the adult patient has capacity unless clinical assessment clearly finds otherwise [11]. Indicators that the patient may not have intact capacity and may need a more detailed assessment of capacity, include decisions at odds with the treatment advice without a rational explanation, decisions that change with no clear justification and decisions taken on the background of failure to understand the discussion around treatment options for any reason. Capacity may fluctuate in either direction, for instance, in a patient with altered cognition due to alcohol or recreational drugs, and it may be necessary to reassess capacity prior to performing the procedure. The assessment of the competence or capacity of adults to make decisions on their own behalf is a functional one that requires more than cognitive testing with a tool such as the mini-mental status examination, although this should be performed and documented as part of the assessment process. Assessment of competence should be sought and conducted by the doctor proposing the treatment or investigation and should not be delegated to other colleagues, although in complex situations of impaired capacity, a psychiatric opinion may be helpful and legally advisable.
The essential elements required to demonstrate competence are:
 the ability to maintain and communicate a choice
the ability to maintain and communicate a choice
 the ability to understand the relevant information
the ability to understand the relevant information
 the ability to appreciate the situation and its consequences
the ability to appreciate the situation and its consequences
Questions that may be of assistance in assessing capacity are listed in Table 25.3.1. Third parties, such as relatives, are unable legally to provide consent, although it is frequently assumed that they are; however, it is a long-established practice and frequently a useful exercise to involve relatives in the process of determining what the patient would have wanted in a particular circumstance. They may also provide valuable information during the process of competence assessment regarding a person’s set of values and beliefs, cultural considerations and usual behaviour.
Table 25.3.1
Questions for determining competence
| Parameter | Questions |
| Comprehension | What is your present condition? What treatment choices have been suggested? |
| Belief | What do you think is wrong with you? |
| Do you believe that you need treatment? | |
| What do you think the treatment will achieve? | |
| What do you think will happen if you have no treatment? | |
| Why has the doctor recommended this particular treatment for you? | |
| Weighing | How did you reach the treatment decision that you have chosen and what factors helped you make that decision? |
| Choice | Have you decided whether to accept the treatment choice that was recommended for you? Have you made any other decision about your treatment? |
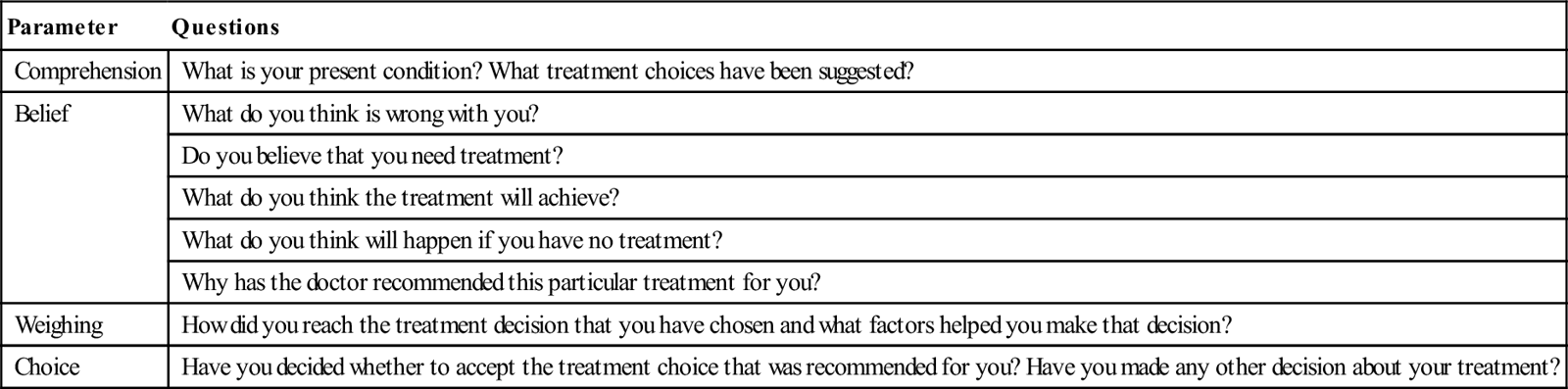
Patients may make an advance statement or living will detailing their wishes for medical treatment should they become incapacitated at a later date in the form of a written document or witnessed oral statement. This is legally binding provided the patient is an adult and was competent at the time made and the statement can be proven to be legally valid and applicable to the current circumstances. This is often difficult to validate in an emergency situation and, if doubt exists about validity, a court ruling should be sought.
Patients who may be incompetent to consent (Table 25.3.2)
Children and adolescents
The legal age of consent in Australasia has changed in the last quarter of a century from 21 to 18 years and, in some circumstances, to 16 years or less. This has occurred against a background of differing ages at which persons may vote, buy tobacco or alcohol, drive cars or engage in sexual activity. There is ongoing debate in both Australia and the UK around the age at which a child may be considered competent to consent, as tested in the cases of Gillick [12] in the UK and Marion’s case [13] in Australia (Table 25.3.3). In the UK, the principle of decision making by a proxy grants a parent or guardian, or a designated person or local authority, the right to give consent. If the proxy is unavailable in an emergency, the principle of necessity justifies treatment provided it can be demonstrated that any decision is taken in the best interests of the patient.
Table 25.3.2
Examples of patients who may not be able to give consent and who may consent for them
| Patient | Proxy consent |
| Children | Parent, guardian, guardianship board, local authority |
| Serious mental illness | Parent, guardian, guardianship board |
| Toxic impairment (drugs and alcohol) | Patient when competent, guardianship board, medical director |
| Intellectual impairment | Guardian, guardianship board, local authority |
| Emergency situations | Patient, guardian, medical director, local authority |
Table 25.3.3
Examples of relevant landmark legal rulings
| Case | Australia | UK |
| Bolam, 1957 Patient undergoing ECT was not given any muscle relaxant and sustained fractures. Not warned of this risk by psychiatrist |
Ruling that the psychiatrist acted in accordance with a reasonable body of psychiatric opinion in not disclosing small risks of injury. Concept became known as the Bolam test of what a reasonable professional opinion would do or say. | |
| Bolitho, 1997 Case of whether a 2-year-old boy with respiratory problems who died should have been intubated |
Bolam test challenged. Ruling that decisions had to stand up to logical scrutiny, whether or not other similar professionals would have taken that decision | |
| Gillick, 1986 Mother of five girls brought case in UK to prevent contraceptive advice being given to under 16s without parental knowledge |
Principles of Gillick case were accepted as part of common law in Australia | Some forms of medical treatment (contraceptives in original case) could be prescribed to under 16s without parental consent or knowledge if the child had sufficient maturity and understanding. Ambiguity around what sufficient meant |
| Marion’s case, 1992 Request for sterilization of a girl with intellectual impairment |
Recognition of the requirement to respect the autonomy and bodily integrity of the individual | |
| Rogers vs Whittaker, 1992 | Consent deemed invalid on grounds that surgeon had given insufficient detail to inform. View that courts rather than medical professionals, should determine the relevant standard of care. Overturned Bolam standard |
The most important factor to be considered is the competence of the patient to understand what is wrong and what the treatment entails. This has more to do with intellectual and emotional maturity than chronological age. It would be reasonable for a 14-year-old girl to consent to appendicectomy, but quite unreasonable to expect the same person to understand the consequences of hysterectomy. In a genuine emergency, the care of the patient is the most important factor and the absence of a parent or guardian is not a bar to an emergency procedure. Should treatment of a minor be required and valid consent not obtainable, the steps taken to obtain consent and the reason why the treatment must be carried out must be clearly documented. If at all possible, the opinion of a second equally or more senior clinician should be documented. Many hospitals require that, in such circumstances, the hospital medical director or delegate give approval. This is simply a means of ensuring that the hospital is aware of the situation and accepts responsibility.
A special situation occurs for children whose parents hold religious beliefs that proscribe the administration of blood products. This creates a situation where the child is incompetent and the parents do not consent. There is now almost standard legislation that allows the attending doctors to certify that blood transfusion is required to sustain life and to then administer the treatment despite opposition from the parents in the best interests of the patient.
Intellectually impaired
For consent to be valid, the patient must be able to understand the nature of the condition, the options available and the treatment being recommended, plus the material risks and the possible outcome of any potential treatments.
The mildly intellectually impaired patient may be able to satisfy these criteria, but the more severely disabled will not be in a position to give valid consent. In the latter situation, in Australia, the guardian or regional Guardianship Board would have to be involved in all but the most urgent cases and there is legislation that covers the protection and administration of incompetent patients. The Board is available to give timely help and has the authority to conduct hearings, receive evidence and make decisions on behalf of incompetent persons. This provides protection for the patient and the doctor. Emergency physicians should ensure that they are aware of how to contact their local Board, both in and out of working hours.
Mentally ill
A diagnosis of mental illness does not automatically preclude a patient from giving consent. The attending doctor must decide on the competence of the patient to consent. The attending psychiatrist may be in a position to assist. If the patient is not competent then the relevant mental health legislation must be considered. Within Australia, the regional Guardianship Boards should be consulted. In the UK, The Mental Capacity Act Deprivation of Liberty Safeguards protects patients in hospitals or care homes from harm.
In an emergency where life or quality of life is seriously threatened and time is of the essence, the facts should be recorded and treatment commenced. A sound knowledge of the mental health and guardianship legislation relevant to the region is essential.
Patient disabled by drugs or alcohol
When a patient is temporarily disabled by drugs or alcohol, the situation is less clear. Legal and medical opinions do not always agree, especially in respect of capacity and blood alcohol readings. The absolute legal position is unclear as to whether an intoxicated person can give consent, but there is no doubt that any clinician who acts in the best interest of the patient will always be on solid ground in the event of legal challenge.
Restraint may be justified in order to prevent patients taking their own discharge with adverse consequences. In these complex situations, it is worth considering whether it is better to be sued for assault and wrongful imprisonment or to be sued for the damage that followed to a patient who was allowed to leave. It may be possible to ask the regional Guardianship Board for help in Australia and the hospital medical director for advice in both Australia and the UK, but there will be occasions in which immediate decisions must be taken and the best rule is to do whatever would be the best for the patient in the longer term. Again, documentation at the time and the signatures of witnesses will help if the court is involved.
The emergency patient
There has been little written about the patient who requires emergency care but is temporarily incapable of providing consent. The overriding principle, however, is one of the duty of care owed by the clinician to the patient. There is also an obligation to explain to the patient what has been done as early as is reasonable in the recovery phase.
The emergency physician must know the essentials of consent and the differences between implied, verbal and written consent. A sound knowledge of regional mental health and guardianship legislation is required. There must be adequate and contemporaneous documentation of decisions. If it is clear that the clinician was acting in the best interests of the patient and that the processes followed were deemed to have been logical and necessary in an emergency situation, it increases the chance that the law will be applied pragmatically.
Emergency physicians work in an environment of multiple simultaneous demands. With respect to critically ill and injured patients, detailed information regarding presentation, past history, cultural considerations and usual level of functioning is often lacking and may, in fact, be wrong. A clinician may have little time to make a detailed assessment before a treatment decision is required. Similarly, the information available at a point in time may be lacking or may change later. Emergency physicians often make complex decisions at short notice with little background information. In situations where decisions have been made on behalf of a patient who is felt to be incompetent, it is important to document carefully the information available at the time and the differential diagnosis and reasons for the course taken. It is good practice also to seek the assistance and advice of a senior colleague where the competence of a patient is in doubt and significant interventions are deemed necessary.
The informed consent process should be driven by the desire to enable and support an appropriate treatment choice by a patient, rather than the fear of litigation and is a core skill within emergency medicine.
25.4 Privacy and confidentiality
Allen Yuen and Biswadev Mitra
Introduction
An individual’s right to privacy and confidentiality has gained increasing recognition over the past decade. In an emergency setting, where patients are more vulnerable because of illness or injury, staff are often provided with confidential family and legal information, which would otherwise not be divulged, trusting that this will only be used to assist in the care of the patient. The law preserving confidentiality in public and private hospitals, day procedure centres and community health centres (called ‘relevant health services’ in the Act) is to be found in the relevant sections of individual state and territory Health Services Acts [1–3]. The section applies to the health service itself, the board of the service or a person who is or was a member of the board, a delegate to a board, a proprietor of such a service or engaged or employed in a service or performing work for it. These people are generally prohibited from disclosing information that could directly or indirectly identify a patient. In addition, the individual state or territory’s health records act and the Privacy Act 1988 (Commonwealth) confer statutory privacy rights on patients, whether they are treated in a public or private facility. Both Acts set up complaint procedures for patients who believe confidential information about them has been unlawfully disclosed to a third party. New Zealand has similar legislation [4].
Physical privacy
Emergency departments (EDs) are necessarily designed in an open plan to increase efficiency, observation and communication, but these requirements do intrude on privacy, particularly if cubicles are separated by curtains rather than solid walls. Consultations may be overheard during history taking and when discussing patients with other medical staff or specialists, either directly or by telephone.
Patient privacy incidents occur frequently in an ED, risk factors being length of stay and absence of a walled cubicle. Patients who have their conversations overheard are more likely to withhold information and less likely to have their expectations of privacy met [5]. Privacy and confidentiality are challenged by physical design, crowding, visitors, film crews, communication and other factors [6].
Prior permission should be obtained from the patient to allow students, nurses, other medical officers to be present during history taking, examination and procedures. This applies both in public and private hospitals. Some aspects of privacy in healthcare in the ED relate to confidentiality while being assessed (being overheard, being seen, being exposed and being embarrassed), which relate to ED design, staff awareness, sensitivity and care. ED staff may be unaware how their routine behaviour may infringe on patient privacy [7].
Staff bays are now often enclosed by glass screens to prevent others from hearing details on a patient’s history or to prevent patients from becoming unnecessarily alarmed by discussion of serious differential diagnoses, which may need to be excluded. Inappropriate or unprofessional comments by staff may also be heard [8].
When the patient is an adolescent, privacy needs may exclude communication with a parent. An understanding of the relevant informed consent law relating to minors is required [9]. The federal Privacy Act does not specify an age at which a child is considered of sufficient maturity to make his or her own privacy decisions. Doctors need to address each case individually, having regard to the child’s maturity, degree of autonomy, understanding of the circumstances and the sensitivity of the information being sought [3].
It is only within the last 5 years that the almost universal ‘whiteboard’ has virtually disappeared. This was a popular and useful management tool in EDs, displaying the patients’ names, working diagnoses, locations and management plans. They were easily visible to anyone who came into the department. To preserve privacy and confidentiality, it was inevitable that they were withdrawn despite strong opposition from ED staff, claiming that this would lead to disruptions in patient care, coordination and flow. These problems did occur during the change-over period, but staff adapted well and the advent of patient-tracking computer systems means that each monitor now provides more clinical information than the whiteboard ever did.
Well-known people (VIPs, politicians, media personalities and sports stars) need even more privacy than others, since they may be accompanied by support staff and, perhaps, a bevy of reporters who may be difficult to control, armed with video cameras and portable recorders. They cannot be restricted until the patient is actually inside the hospital building, after which security is in charge. Even when outside the building, most will accept advice to remain in a provided access zone where they may use their cameras or microphones without intruding on the privacy of other patients or their subject of interest. Hospital staff involved in the care of such patients may also wish to have their own privacy protected. Most hospitals now have media relations officers to take on the role of providing regular updated bulletins.
Healthcare providers
There is also the important matter of privacy for health providers. Whether full names should be displayed on identity badges is debatable. Details of contact numbers and home addresses of consultants, medical staff and nurses must be kept confidential, as there are cases of disgruntled or psychotic patients harassing and stalking clinical staff. Even if the request for contact details is innocent, it is an invasion of a healthcare worker’s privacy for that information to be released without consent. In addition to the statutory offences of breaching confidentiality, doctors and other healthcare providers may be sued at common law if they divulge confidential information without a patient’s consent. The patient may sue for breach of contract or because the doctor has been negligent in disclosing the information. It should be noted that it is lawful for a health professional to disclose information if:
Mandatory reporting
Mandatory reporting overrides privacy laws where they are for the purpose of protection of the health of individuals or communities. Examples are:
 reporting a reportable death or a reviewable death to the coroner
reporting a reportable death or a reviewable death to the coroner
This becomes more difficult when there is merely a suspicion, but doctors are protected if they report on this basis only. The laws vary between jurisdictions.
Police
Assistance must be given to the police when a criminal offence has been committed. In such cases, patient name, date of birth, address, nature of incident, description of injuries and conscious state may be released. An opinion of causation must not be stated.
If an injured patient is suspected of being a crime victim or perpetrator and may be a danger to that patient’s or another’s life, it is the doctor’s civic duty to inform police of the circumstances [11].
If a police enquiry is made by telephone, record the name, station, contact number and request and advise that the information will be obtained and provided. The given contact number must be checked to ensure if it is genuine before providing information, heeding the principles of confidentiality.
With police statements, the doctor should state credentials and experience before giving details of alleged history and physical findings. It is important to be objective and to avoid venturing opinions outside a doctor’s area of expertise. It is preferable for all police statements to be written by the ED director, so that a confidential record is kept of all statements issued.
Assistance is also given to help police identify missing or deceased persons.
Blood samples may need to be collected by law for drug or alcohol screening for patients involved in motor vehicle accidents. These are provided to police for testing.
Forensic issues
All deaths from unknown, unexpected, unnatural, accidental, violent or suspicious causes must be reported to the state coroner. This also includes cases of unknown identity, during or after surgery, in custody, a ward of the state, requested by next of kin or where unable to issue a death certificate.
Patient health information
Legislation
Confidentiality of health information has been the focus of legislation over recent years.
The Privacy Act 1988 [1] applied only to the Australian Commonwealth public sector, but steps were taken early on to introduce it to the private sector, resulting in the Privacy Amendment (Private Sector) Act 2000 becoming law to cover the private (and public) health sector in December 2001 [2]. Patients who have been treated in public hospitals are able to gain access to their medical records by means of the relevant state or territory freedom of information act, e.g. Freedom of Information Act 1982 (Vic). Patients treated in a private hospital, by a private doctor or other private health professional, have a right to gain access under the relevant state or territory health records act, e.g. Health Records Act 2001 (Vic) and also under the Privacy Act 1988 (Commonwealth).
In New Zealand, the Privacy Act was enacted in 1993 and was used to develop the Health Network Code of Practice and Health Information Privacy Code 1994, which was further modified by the Health Information Standards Organization in 2005 [5].
Australian privacy principles [12]
The 13 Australian Privacy Principles (APPs) replace the National Privacy Principles (NPPs) for organizations from 12 March 2014. The APPs are found in the Privacy Amendment (Enhancing Privacy Protection) Act 2012 (Commonwealth). The amendments to the Privacy Act introduce the concept of a ‘permitted general situation’ and a ‘permitted health situation’. The existence of a permitted general situation or permitted health situation is an exception to various obligations in the APPs. A new section 16A outlines seven permitted general situations, where the collection, use or disclosure of personal information about an individual, or of a government-related identifier, will not be a breach of certain APP obligations.
New section 16B outlines five permitted health situations, where the collection, use or disclosure of certain health information or genetic information, will not be a breach of certain APP obligations.
APP1
APP1 requires hospitals or healthcare agencies to have ongoing practices and policies in place to ensure that they manage personal information in an open and transparent way. APP1 introduces a new requirement for agencies to have a clearly expressed and up-to-date policy about the management of personal information by the agency. APP1 specifies the minimum information that should be included in the agency’s APP privacy policy. An agency needs to take reasonable steps to make its APP privacy policy available free of charge and in an appropriate form. The agency must take reasonable steps to provide the policy in a particular form if requested by an individual or body. APP1 also requires an agency to take reasonable steps to implement practices, procedures and systems that will ensure compliance with the APPs and any registered APP codes and enable the agency to deal with inquiries and complaints by individuals.
APP2
APP2 deals with anonymity and pseudonymity and allows individuals to interact with agencies while not identifying themselves or by using a pseudonym. Both requirements are subject to certain limited exceptions, including where it is impracticable for the agency to deal with individuals who have not identified themselves or where the law or a court/tribunal order requires or authorizes the agency to deal with individuals who have identified themselves.
APP3
APP3 outlines when and how an agency may collect personal and sensitive information that it solicits from an individual or another entity. An agency must not collect personal information (other than sensitive information) unless the information is reasonably necessary for, or directly related to, one or more of the agency’s functions or activities. The APPs impose obligations on agencies regarding sensitive information for the first time. APP3 deals with the collection of sensitive information by agencies, which is not permissible unless certain exceptions apply. An agency must only collect personal information from the individual, unless an exception applies. In EDs, it is sometimes difficult to obtain an accurate history, due to the patients’ anxiety about their presenting symptoms. More accurate information may become available after they have had a chance to collect their thoughts, or to affirm areas of their history with family or other witnesses. It is useful to recheck details that may not fit a working diagnosis.
Medication histories are often also inaccurate, since the patient may not be responsible for self-administration or may obtain tablets from a prepackaged dispensing system. Computerized GP letters often have all medications ever prescribed for that patient by the GP practice and, to be accurate, every medication should be checked with the patient or carer to ensure their currency. Patients are not obliged to give their reason for requesting access. Patients do not have immediate right to investigation results. The doctor ordering the tests must be given the opportunity to assess and discuss the results; otherwise there is the risk of misinterpretation.
APP4
APP4 introduces new obligations for agencies in relation to unsolicited personal information. Where an agency receives unsolicited personal information, it must determine whether it would have been permitted to collect the information under APP3. If so, APPs 5 to 13 will apply to that information. If the information could not have been collected under APP3 and the information is not contained in a Commonwealth record, the agency must destroy or de-identify that information as soon as practicable, but only if it is lawful and reasonable to do so.
Computerized patient data must only be accessible to authorized personnel by password-protected access [10].
APP5
APP5 specifies certain matters about which an agency must generally make an individual aware at the time of, or as soon as practicable after, the agency collects their personal information. Patients do have a right to access opinion as well as factual material, including a specialist’s report, whether or not the report states that it is not to be shown to the patient without the patient’s consent [3].
APP6
APP6 outlines the circumstances in which an agency may use or disclose the personal information that it holds about an individual. If an agency collected personal information for a particular purpose, it must not use that information for any other purpose unless:
 the individual has consented to the use for another purpose
the individual has consented to the use for another purpose
 the purpose is directly related to the purpose for which the information was obtained.
the purpose is directly related to the purpose for which the information was obtained.
APP7
APP7 regulates the use and disclosure of personal information by organizations for the purpose of direct marketing.
APP8
APP8 introduces an accountability approach in relation to an agency’s cross-border disclosures of personal information. Before an agency discloses personal information to an overseas recipient, the agency must take reasonable steps to ensure that the overseas recipient does not breach the APPs (other than APP1) in relation to that information. In some circumstances, an act done, or a practice engaged in, by the overseas recipient that would breach the APPs, is taken to be a breach of the APPs by the agency. Hospitals may transfer health information to countries where similar privacy laws exist. Consent needs to be obtained from the patient when in doubt or when sending to countries where no such protection exists.
APP9
APP9 prohibits an organization from adopting, using or disclosing a government-related identifier unless an exception applies. In some settings, such as counselling in HIV/AIDS or sexual health, there are instances where anonymity is requested and granted. In the case of public or private hospital EDs, for providing a safe health service and for billing and rebate purposes, doctors are required to record the identity of the patient [3].
APP10
Under APP10, an agency must take reasonable steps to ensure that the personal information it collects is accurate, up-to-date and complete. An agency must also ensure that the personal information that it uses or discloses is accurate, up-to-date and complete and relevant, having regard to the purpose of the use or disclosure.
APP11
APP11 requires an agency to take reasonable steps to protect the personal information it holds from interference, in addition to misuse and loss and unauthorized access, modification and disclosure. APP11 imposes a new requirement on agencies to take reasonable steps to destroy or de-identify information if the agency no longer needs the information for any authorized purpose, unless:
APP12
APP12 requires an agency to give an individual access to the personal information that it holds about that individual, unless the agency is required or authorized to refuse to give access by or under the Freedom of Information Act 1982 or any other Commonwealth or Norfolk Island legislation that provides for access by persons to documents. Agencies must respond to requests for access within 30 days. Agencies must give access in the manner requested by the individual if it is reasonable and practicable to do so and must not charge for this access.
APP13
APP13 requires an agency to take reasonable steps to correct personal information to ensure that, having regard to a purpose for which it is held, it is accurate, up-to-date, complete, relevant and not misleading.
New Zealand
New Zealand implemented its Privacy Act in 1993, with 12 principles that are similar to the Australian NPPs [4]. The Privacy Act has 12 information privacy principles:
Principles 1–4 govern the collection of personal information. This includes the reasons why personal information may be collected, where it may be collected from and how it is collected.
Principle 5 governs the way personal information is stored. It is designed to protect personal information from unauthorized use or disclosure.
Principle 6 gives individuals the right to access information about themselves.
Principle 7 gives individuals the right to correct information about themselves.
Principles 8–11 place restrictions on how people and organizations can use or disclose personal information. These include ensuring information is accurate and up to date and that it is not improperly disclosed.
Principle 12 governs how ‘unique identifiers’ (such as IRD numbers, bank client numbers, driver’s licence and passport numbers) can be used.
In 2005, the Ministry of Health released the Health Information Strategy for New Zealand [4], with an emphasis on security of electronic data and maintenance of trust in and integrity of, communication. They developed a Privacy, Authentication and Security (PAS) guide, which brought all the existing relevant documents together [15].
Implementation
Most hospitals now provide brochures to patients on arrival outlining these privacy issues. These are important whether the hospital is public or private [16,17]. ED staff must be aware that some patients will require more detailed explanation before they are prepared to reveal all relevant information and a sensitive approach is needed. Complaints about alleged breaches of privacy may be made and, if necessary, may be referred to the state health ombudsman or the state or federal privacy commissioner.
Communications
In this electronic era, sending information by facsimile, e-mail or telephone messaging can breach security and ED staff need to take great care to ensure that there is a responsible person receiving the data or that with telephone messages, only the caller’s contact details are left. Health details should only be discussed directly with the patient, or parent in the case of a minor.
Medicolegal reports
Medical reports can be provided to lawyers or police officers acting on behalf of a prosecution or defending lawyer, after written consent is obtained from the patient. Such reports are the intellectual property of the doctor writing the report. While a patient has a right to view them, there is no right for a copy to be supplied, unless an appropriate fee for preparation of the report is paid.
Where a lawyer requests copies of medical records, rather than a report, the doctor must check the records to ensure that information collected is not sensitive information and does not contain information about others. Payment may be requested for the costs of reviewing and photocopying.
Research and quality assurance
Patients must be asked for consent before participating in research or quality assurance studies and must be de-identified in any reports. They must be fully informed of the reasons for and the possible side effects of the study.
Complaints and non-compliance
Doctors are advised to obtain their own independent legal advice and notify their medical indemnity/insurance company if they are investigated by the privacy commissioner as the result of a complaint that privacy may have been breached. Monetary fines or imprisonment may result from non-compliance [18].
25.5 Ethics in emergency medicine
Mike W Ardagh
Introduction
To be ethical in emergency medicine is to do the right thing for the patient. However, this can be challenging in the context of urgency, uncertainty and impaired patient competence.
How do we know if we should let the intoxicated head-injured patient leave the emergency department (ED) without being fully assessed? How do we decide if the decision of the elderly lady with the fractured neck of femur not to have surgery should be honoured? How could we possibly know what the unconscious cardiac arrest patient wants?
Briefly, decisions about such cases can be guided by a number of tools for clinicians who work among the ethical complexities of emergency medicine. This approach is based on current, popular bioethics. Although it is reasonably generic, there will be places and times when it fits less well. In emergency medicine, standardized processes are popular and the toolkit below suggests a standardized approach to ethics. However, in practice, ethics must be individualized to the patient in front of us. Good clinicians need to superimpose their own morality and understanding of the patient and the patient’s context. This involves a unique interaction with the person the patient is. Ultimately, the aim is to facilitate a process whereby the patient’s true autonomous wishes are honoured. The nature of emergency medicine makes this challenging, but not impossible.
Ethics and law
The ethics methodology described here is a relatively simple approach, to be applied in specific cases, taking into account the peculiarities of the patient’s medical condition and the patient’s ‘world view’. However, this methodology, and ethics in general, struggle to arrive at an indisputable, definitive answer. The law, however, intends to arrive at a definitive answer so that a determination can be made regarding the lawfulness of what was done. The law uses a combination of statute (written law) and precedents (previous interpretation of written law in specific cases) to come to this determination. It is a complex methodology which is best applied retrospectively once all the facts are known. In emergency medicine, ethics is an easier model to use as it can be applied prospectively while there is still uncertainty. However, it is the law which is called upon, from time to time, to determine the ‘rightness’ of medical decision making. Good ethics, well documented, should see the law get behind the medical decision making. However, the decisions of emergency physicians need to be consistent with local law. In reality, this places the emergency physician in a difficult situation, being required to act in keeping with the law, yet with an incomplete knowledge of the law and, at the time of decision making, dealing with many unknowns. Generally, the law is sufficiently consistent to apply ethics with confidence but there are some local differences, particularly regarding how consent might be obtained and who might give it (particularly the acceptance of proxy consent – that is consent from relatives), which should be well known in relevant emergency departments.
Ethical decision making – influences and processes
The words ‘ethics’ and ‘morals’ have origins in different languages but their origins have similar meanings – ‘the done thing’ or ‘the right thing to do’. The use of the words in the English language generally has morals or morality as qualities of an individual and ethics as a description or study of those qualities. However, they both relate to ‘doing the right thing’.
What encourages us to do the right thing?
An individual’s morality is a manifestation of the interactions of many influences, including belief, upbringing, culture, societal influences and professional obligations. Some of these are internal drivers of behaviour (for example, religious or other beliefs), others are ‘internalized’ (for example, societal codes of conduct which are learnt and become habit) and some are ‘external’ (for example laws and professional codes which are obeyed for fear of the consequences if not). The relative contribution of these influences varies from person to person and from context to context. Whatever that mix in an individual doctor, it is a prerequisite for ethical practice that the doctor is of good moral character.
The method of decision making we employ might be ‘utilitarian’ or ‘deontological’ [1]. A utilitarian approach considers the outcomes of actions and values the positive balance of good over bad (or benefit over harm) that ensues. A deontological approach values actions that adhere to overriding moral principles.
Considering the influences on morality and the methods of decision making we might, for example, be nice to our patients because we are nice people (internal morality), we have learnt that being nice is the right thing to do (internalized morality), the code of ethics of our professional body instructs us to be nice (external morality), we believe that being nice is a governing principle of behaviour (deontology) or we think that being nice means patients are less likely to complain about us (utilitarianism). Of course, these are not mutually exclusive and, in practice, there is a mix of all of these influencing our behaviour.
In addition to the clinician’s mix of morality and decision-making methodologies, patients’ choices will be influenced by their own morality and ‘world view’. Some individuals are influenced considerably by spirituality or religion and some cultures have a predominance of such individuals. A deontological approach has appeal in this context. Some individuals have no such influence and instead are influenced by a rational consideration of utility. Some cultures champion the individual’s freedom to determine his or her own destiny. Other cultures consider a group, often a family group, as appropriate to make decisions on behalf of the individual. In some cultures, there is a relatively high level of respect for authority (power differential), so there might be a reluctance to question those of perceived authority, such as doctors. In other cultures, there is less of a barrier to questioning authority, potentially allowing a better exchange of information.
These three dimensions help define the context in which the patient considers ethical decisions: ‘belief’ versus ‘rationality’; ‘individualism’ versus ‘collectivism’; and ‘high power differential’ versus ‘low power differential’. Popular medical ethics of this time tends to come from a Western context of rationality, individualism and relatively low power differential. It is appreciated that this context is not applicable to all. Of most importance, the individual patients we manage have varying positions on each of these three dimensions. Just as one model does not fit all contexts, in the same ED, one model does not fit all patients. One of the challenges we face is to welcome the patient’s perspective (context, values, world view) into the process of decision making.
The contributions to our morality and our processes of ethical decision making are a complex and variable mix, but that does not mean we cannot employ a standardized process for decision making. A song varies in sound depending on who sings it – the music does not change, it is the quality of the voice that makes the difference. So, with the ‘tools’ that follow – it is the quality of the individual’s morality that makes these tools work to best effect.
An ethics toolkit for the emergency department
In emergency medicine there are many aspects of ethics relevant to our practice, including research ethics, professional ethics, ethical issues in resource allocation and so on which, although relevant, are not peculiar to the ED. However, there are two dilemmas which are common in EDs:
The following ‘tools’ in ethical deliberation provide a structure for decisions in these two areas (Box 25.5.1).
Tool 1: the four principles (Box 25.5.2)
Beauchamp and Childress [2] combined the traditional principles of Hippocrates (try to help and try not to harm) with a consideration of the rights of the individual to determine their own destiny and the rights of others who might be affected. In so doing, they described four principles that offer a pragmatic structure for deliberation. Although the ‘Principlism’ of Beauchamp and Childress has attracted criticism, it remains a popular and useful starting point.
Autonomy describes the patient’s right to determine his or her own destiny. However, there are occasions in emergency medicine when respecting autonomy is difficult because the patient’s competence is impaired or there are other influences undermining his or her autonomy.
Beneficence is the principle of acting in a way that benefits the patient. Non-maleficence, or the principle of avoiding harm, is attributed to Hippocrates. All medical interventions have the capacity to harm and it is unrealistic to expect to ‘do no harm’. Instead, we proceed if the benefit/harm balance is acceptable to the patient. When the benefits and harms are determined by the doctor without due consideration of, or in contradiction to, the patient’s perception of benefits and harms, the action is termed ‘paternalistic’ (as a father might treat a child), although ‘parentalistic’ might be a more appropriate, less sexist term.
Ideally, the benefits and harms of our interventions are reasonably clear before we proceed. For example, the performance of gastric lavage on a non-consenting patient after a trivial overdose several hours earlier is ethically unjustifiable, as there is insufficient benefit to override the principles of respect for autonomy and non-maleficence. Research is an ethical necessity to provide the evidence of benefit and harm, upon which to base decisions.
Justice, or the concept of fairness, is best addressed by questioning whether there are others who might be adversely affected by a particular action. Usually, it does not offer much to the deliberations when considering interventions for an individual in an emergency, but there are exceptions. For example, in a mass casualty incident, the performance of a hopeless resuscitation might be unjust, in addition to harming the patient, if it deprives another person with a greater chance of survival. Or, if the intoxicated head-injured young man were to leave the ED with car keys in his hand and an intention to drive, then there is a potential injustice to other road users, possibly sufficient to override his intention to leave.
In addition, there might be questions about the cost of life-sustaining and other emergency care in comparison to other care, such as hip replacements or immunizations. Although such considerations of ‘distributive justice’ are important, it is not appropriate for the clinician managing an individual patient to be influenced by such concerns at that time. However, it is very appropriate for clinicians to contribute to debate regarding healthcare funding and policy, but in a meeting room rather than a resuscitation room.
In applying this tool, it is necessary to discuss with the patient the clinical utility (the beneficence and maleficence, benefits and harms, pros and cons) of the therapeutic options and identify the preferred option or options. The patient is allowed the opportunity, as circumstances permit, to deliberate, discuss with others and then express a decision. Urgency and impaired patient competence might limit how much information can be provided to the patient but these barriers should not be used as a reason not to try. Patients should receive the maximum information circumstances allow. In many cases in EDs, the urgency is related to pressures of work rather than real clinical urgency.
Allowing, even encouraging, a discussion with an interchange of questions and answers will enhance the opportunity for the patient to understand what is available. For the patient, the belief that he or she has been able to maintain control, to take time, to say what he or she thinks and to be listened to, is immensely fulfilling. Independent of the clinical outcome, this belief enhances patient satisfaction.
It is inevitable, and appropriate, that clinicians have a preferred option, based on their understanding of the utility of the interventions and their experience of what the average patient in similar circumstances, and the average clinician in similar circumstances, would choose.
The clinicians’ preferred option should not be stated ‘up front’, but may be offered during conversation. The patient might ask what the clinician thinks is best or the clinician may offer it if the patient appears to be struggling to make a decision (‘would you like me to tell you what I think would be best?’).
If the decision the patient has made is concordant with the clinician’s preferred option, then it is appropriate to proceed with that option. If the patient has been given the best chance possible to make a considered, free and informed choice and that choice is the same as the clinicians’ preferred option, then it is reasonable to assume a true autonomous choice has been made and to get on with it. If the decision the patient has made is discordant with the clinician’s preferred option (as might be the case with the elderly lady who refused surgery for her fractured neck of femur), then it is sensible to proceed to the next tool.
Some would argue that accepting a decision because it is concordant with the clinician’s is a thinly veiled parentalism. However, it is unlikely a concordant decision is a wrong one, it is likely that such a decision will lead to ongoing treatment (thereby keeping the options open) and the practicalities of emergency clinicians in an emergency context unravelling the complexity of such a scenario relegate this concern to fine print.
Although a discordant patient choice may well be a true autonomous choice and, therefore, should be honoured, the discordance with the preferred choice is a trigger for a higher degree of scrutiny. The higher degree of scrutiny continues with the next tool.
However, prior to proceeding to that tool it is important to explore (as part of the continuing interaction started above) the reasons for the patient’s decision. There might be ‘cons’ or ‘harms’ of the preferred choice which can be addressed to the patient’s satisfaction, thereby allowing the patient a chance to choose again with a new perception of pros and cons. The clinician should not be coercive in content nor in manner, however, if there are possibilities which would influence the patient’s decision, they should be offered. An interaction such as this is permissive, not coercive; ‘That’s OK and we will respect your decision, but is there any particular reason you are against the operation?’ ‘OK, I see what you mean. Is there anything we can do so that this is less of an issue for you?’
For example, if it transpires that the elderly woman’s main reason for declining surgery for her fractured neck of femur is an intense concept of privacy, with anticipated unbearable embarrassment associated with being in a multibed room, having to use a bed pan and being examined by multiple people, then offering a single room and enforcing a rule of no medical or other students may give her a new balance of pros and cons which changes her decision.
Tool 2: respecting autonomy (Box 25.5.3)
We have arrived at Tool 2, because at Tool 1 the patient’s expressed choice was discordant with the preferred option of the clinicians. The expressed choice of the elderly lady who refuses to consent to surgery is explicit. The expressed choice of the drunk young man taking his own discharge is not articulated as clearly, but his violent and offensive behaviour and his self-initiated discharge represents a ‘discordance’ with the choice of the clinicians.
As part of Tool 1, the reasons for the patient’s decision have been explored (as opportunity allowed) and any possibilities of mitigating the ‘cons’ of the preferred option have been explored and the options reconsidered. The patient’s decision remains discordant.
There are two questions for the clinicians to consider at this point:
If the answer to this question is ‘no’ then the next question is:
If the answer to this question is ‘yes’, then respecting the patient’s autonomy means disregarding the expressed wish of the patient and honouring the truly autonomous wish. It is an important concept that overriding the expressed wishes of a patient (which on the surface appears parentalistic) is done to honour the truly autonomous wishes of the patient (which have not been expressed due to influences undermining autonomy).
To answer the first question (‘is this decision a truly autonomous decision?’), it is necessary to consider the elements of autonomy – information, competence and freedom – by asking three questions. See Table 25.5.3, which describes Tool 2. Respecting Autonomy.
The first component of an autonomous decision is sufficient information to make the decision. A patient is at liberty to decline to be informed and to make a decision based on whatever information they consider sufficient. However, if a lack of information is clearly leading to a decision the patient would not make if sufficiently informed then the decision is non-autonomous.
The second component of an autonomous decision is the ability to deliberate and express a decision. Some refer to this as competence, or decision-making capacity (although both of these terms may have wider definitions). For this chapter, the term competence is used. Is the patient cognitively impaired, thus impairing his or her competence and, if he or she were competent, is it likely he or she would make a different decision? Determining the patient’s competence is challenging and is covered more fully in Chapter 25.3. However, a simple approach is outlined in Tool 3.
Are there coercive influences leading the patient to make a decision he or she would not make if free from the influence? In the ED, the most common coercive influence is suicidal ideation secondary to depression. Occasionally, other influences, from family or friends, may be present. The presumption in the ED is that someone who has attempted suicide has a depressive illness which is reversible and that their true autonomous wish (if the coercive influence of depression were reversed) would be to receive treatment to preserve their life. This presumption is not always correct as some suicides might be considered to be ‘rational,’ ‘autonomous’ decisions (for instance, the patient with advanced incurable neurological disease). Determining that the patient’s choice is free from a reversible coercive influence is very difficult for an emergency department clinician, in the emergency department and in a hurry. In this context, the most senior and qualified assessment should be called upon (the emergency physician or the psychiatrist, for example). However, if unavailable or still uncertain, then it is appropriate to default to the presumption that the patient’s suicidality is reversible and that the truly autonomous wish would be to receive treatment to preserve life. This default keeps options open and allows further specialist assessment of psychiatric illness. As such, it is the lesser of two possible errors.
Tool 3: assessing competence (Box 25.5.4)
Tool 3 comes into play because it is believed that the patient’s discordant decision might not be their truly autonomous one and the reason relates to possible impaired competence.
The initial test of competence in this step might or might not be definitive. If it is clear the patient ‘knows what they are doing,’ or it is clear they do not, decision making might be finished at this point. Otherwise, and if there is any doubt, reassurance might be required, as discussed in Tool 4.
Competence mostly is about understanding. An initial assessment of competence can be made by asking if the patient displays understanding of three things. See Table 25.5.4 which describes Tool 3. Assessing Competence.
Does the patient display understanding of the illness or injury, the therapeutic options and the perceived or estimated benefits and harms of the various therapeutic options? If it is clear that they do, then competence can be assumed. If it is clear they do not, then competence can be assumed to be absent. If it is unclear if they understand or not, reassurance can be gained as described below.
Tool 4: reassurance about competence (Box 25.5.5)
Competence mostly is about understanding, but there will be supporting information concerning the patient’s capacity to understand, which this tool explores.
Observations regarding the Glasgow coma scale (GCS) and intoxication are important, as they provide ‘hard data’ in the clinical notes (and should be recorded there). However, they are not absolute as they indicate capacity to understand and not actual understanding. A GCS of less than 9 (indicating the patient is not interacting with his or her environment, except non-communicative responses to painful stimuli) will clearly indicate impaired competence as no decision can be made nor expressed. However, a GCS of 14 out of 15 (or even 13 or 12) does not necessarily mean the patient does not understand. The head-injured man who wishes to take his own discharge might be drunk with an initial GCS of 14. This suggests competence might be impaired but does not define incompetence. Incompetence must be proven by a determination that understanding is impaired, by reapplying Tool 3.
Similarly, an early, humane and judicious dose of intravenous morphine for a painful condition (such as for the elderly lady with a fractured neck of femur) does not necessarily render the patient incompetent. If she still indicates understanding then competence should be assumed.
Perseveration is common in mild/moderate head injuries, often manifesting as repeating the same questions over and over (‘Hey doc, what happened to me?’ ‘Why am I here?’ etc.). If new information is not being stored, then competence to make important treatment decisions is unlikely to be present.
If the decision the patient makes is discordant with the preferred option, then we have already challenged his or her understanding: ‘OK, we well respect your decision but can I please, for my own reassurance, ask you a few questions so that I am sure you understand the decision you are making? Can you tell me what you understand about what has happened to you? Can you tell me what you understand about the operation? Can you tell me what you understand about what will happen if you do not have the operation?’ Then, the first part of Tool 4 has asked us to note some potential indicators of impaired capacity to understand. Now, the second part of Tool 4 asks about ‘reason’, as an indicator of the capacity to understand. Reason (I am making this decision because…) is a powerful indicator of a competent decision. The intoxicated head-injured patient might be asked why he wants to leave. He might answer ‘I left my girlfriend at the nightclub with a bloke she fancies. I’m worried about what she’s up to.’
Although we might challenge his reason (and counsel him that, if his girlfriend is cavorting while he is in hospital she’s not the girl for him), he has displayed reason and it is not our place to challenge ‘what makes people tick’ (their context, their values, their world view). Instead, we have the task of ensuring patients are making the right choice for them – their truly autonomous choice. Reason in a decision suggests the choice is a competent one and, consequently, probably an autonomous one.
Tool 5: confirmation the decision is the right one (Boxes 25.5.6 and 25.5.7)
At this stage, one of two possible decisions about the patient’s discordant decision has been made. A final confirmation for each of these decisions follows.
Box 25.5.6 describes Tool 5a. Respecting the patient’s refusal of care. It is important to emphasize that any of these three prove the case. In other words, the presence of any of these three disallows the clinician overriding of the patient’s refusal of care.
Box 25.5.8 describes Tool 5b. Overruling the patient’s refusal of treatment. It is important to emphasize that all three are needed to justify treating a patient against expressed wishes. In this case, the truly autonomous wishes of the patient (to be treated) are being honoured.
In the case of the elderly lady who refused an operation for her fractured neck of femur, discussion might reveal that she had understanding of the consequences of her (discordant) decision. Further discussion might confirm the reasons (intense sense of privacy). Both understanding and reason refute any allegation that she has impaired competence. Her decision is a truly autonomous one and should be honoured. However, there is the possibility of mitigating her reasons (redefining the pros and cons) by arranging greater privacy as suggested earlier. Then her truly autonomous choice and the preferred option of the clinicians may become concordant.
The drunk young man became offensive and disruptive and then left the department. Was his refusal of care a truly autonomous one? If not, would his truly autonomous decision be to accept care? Applying Tool 1, there might be concern that his worsening aggression in the context of a violent blow to the side of his head, represents a deterioration consistent with an expanding extradural haematoma needing urgent attention (beneficence and non-maleficence) and that his discordant decision may be non-autonomous. Applying Tool 2, there might be concern that he ‘wasn’t thinking enough’ (had impaired patient competence). Applying Tools 3 and 4 might reveal that he didn’t know what day it was, he seemed to need reorientation about where he was and what had happened and, when asked if he understood how serious his injury might be and why he was refusing to cooperate with treatment, he was irrational and incoherent. A decision is made that his refusal of care should be overruled and if reassurance, persuasion, bargaining and threats do not allow treatment to proceed, then the clinical staff should consider the use of drugs and restraint to provide treatment. Tool 5 is used for confirmation that this decision is the right one. Finally, and of great importance, the clinicians must document carefully their reasons for intervention (beneficence and non-maleficence) and how they respected his autonomy (the evidence of incompetence and a belief that his true autonomous wish would be to receive treatment).
Tool 6: stopping resuscitation (Box 25.5.8)
When considering whether to stop a resuscitation, the tools listed above are relevant. But, if the patient is unconscious, there is no expressed indication of his or her autonomous wishes. Respect for autonomy and consent may appear irrelevant, but consent should be obtained for resuscitation, like all other medical interventions.
There is an assumption that resuscitation offers hope of a good outcome (which is true), but does not cause harm (which is false). Resuscitation is often provided with this ‘no harm in trying’ belief, but without due consideration of the harms of resuscitation nor how the patient would percieve the balance of benefits and harms. The benefits of resuscitation include the avoidance of death and the restoration of good health. However, resuscitation can cause unnecessary discomfort, indignity, false hope, a lingering death, financial and opportunity costs and survival with a poor quality of life [3]. If patients undergoing resuscitation were able to consider the potential benefits and harms of the resuscitation intervention recieved in a calm and rational state, just as a patient might when consenting for elective surgery, then it would not be suprising to find a number declining consent.
Consent, in relation to resuscitation, attempts to determine what the patient would want if able to consider the benefits and harms of resuscitation. Informed consent, as is appropriate for elective surgery, might be inappropriate during resuscitation owing to the urgency of the treatment and impaired competence of the patient. However, if informed consent is not relevant, other forms of consent still are [4]. The two most common forms of consent used in resuscitation scenarios, where there is both urgency and impaired patient competence, are presumed consent and proxy consent.
Presumed consent uses the concept that a reasonable patient under similar circumstances – or this patient if he or she were able to – would consent to the resuscitation endeavours proposed. This form of consent has merit and is commonly employed but, occasionally, attracts criticism as being a form of medical parentalism, in that it may be perceived to be respecting the principle of beneficence, as the resuscitators perceive it rather than as the patient would perceive it.
Proxy consent involves obtaining consent for resuscitation from a family member or other person, who is perceived to be able to speak on behalf of the patient. Proxy consent avoids the criticism of medical parentalism as the decision is taken out of the physician’s hands, but it suffers as a model as the decision maker may be unable adequately to receive information, understand it and deliberate during a hurried and rapidly evolving resuscitation.
In addition, the proxy might not reflect the views of the patient. There might be occasional circumstances where the proxy declines resuscitation because of some financial or other benefit that would accrue from the patient’s death. More commonly, proxies have a tendency to demand more resuscitation than the patient would have wanted [5,6].
A modification of proxy consent that better addresses the issue of respect for patient autonomy is proxy consent with substituted judgement. This involves not asking what the proxy would want done for the patient, but instead what the proxy thinks the patient would want done. In other words, it attempts to see the resuscitation from the patient’s perspective, as the proxy understands it.
Similarly, a modification to presumed consent is presumed consent with professional substituted judgement [7]. In this model, the resuscitators gather as much information about the patient as they possibly can to attempt to understand how the patient would view this decision. This usually involves speaking with the patient’s loved ones. Then, with some knowledge of the likely outcome of the resuscitation proposed, based on previous experience and a knowledge of the medical literature, they can exercise their moral imagination by asking ‘If I could pause the resuscitation, sit the patient up, talk to him and ask if he wants this resuscitation, what would he say?’ In this way, the patient’s autonomy is respected as best it can be under difficult circumstances, by combining a knowledge of the harms and benefits of the resuscitation with an appreciation of this balance from the patient’s perspective, as best the resuscitators can appreciate it.
For example, in a cardiac arrest, the patient’s primary care doctor might relay details of the conversation he had with the patient during which the patient expressed a desire not to be resuscitated from cardiac arrest. With that information known, asking the question above would bring a clear ‘No, I do not want this resuscitation’. With that response, the resuscitators have an obligation to stop.
The resuscitation should not proceed if presumed consent using professional substituted judgement is employed and the answer to the question is ‘No’. To resuscitate without regard for the patient’s explicit or perceived wishes is a harmful disrespect for his or her autonomy.
Often, and appropriately, a decision to proceed will be made on the basis of a perceived balance of benefit over harm and an uncertainty about what this patient would want. In this case, a ‘trial of treatment’ keeps options open (by keeping the patient alive) and it allows time to gather a clearer view of the likely benefits and harms of resuscitation (as the patient responds or not to the resuscitation) and the likely desires of the patient (as information about the patient comes from relatives or others). The question is asked again, (‘If I could pause the resuscitation, sit the patient up, talk to him and ask if he wants this resuscitation, what would he say?’), until a clear ‘Yes’ or ‘No’ is apparent.
The resuscitators should recognize when the balance of benefit and harm becomes unfavourable from the patient’s perspective, by employing professional substituted judgement. When it is clear that the patient would say ‘No’ to ongoing resuscitation, the resuscitators have a moral obligation to withdraw resuscitation as they can no longer presume the patient’s consent.
The consent model used in resuscitation (proxy or presumed, with or without substituted judgement) will be influenced by the moral dimensions above (especially individualism versus collectivism) and by the legal jurisdiction in which the decision is being made (some may favour a stronger role of proxies in decision making). The law, like ethics, has the objective of ensuring the right things are done for the patient. Presumed consent using professional substituted judgement aims to achieve this, but clinicians should ensure the model they use is consistent with local law.
Summary
To be ethical in emergency medicine is to do the right thing for the patient. The right thing is what the patient would choose if given the ideal circumstances to exercise autonomy. The difficulty we have is determining what the right thing is. The clinician’s morality and methods of weighing ethical issues form a platform for this determination. From this platform the clinician can then apply pragmatic tools, including the four principles, the three questions about autonomy and then the three questions about competence. Further consideration can reassure the clinician about competence and about decisions to treat, or not treat, patients without their consent. In the setting of the unconscious patient undergoing resuscitation, a presumption of consent using professional substituted judgement has the greatest potential to reflect the patient’s truly autonomous wishes.
Having made a good ethical decision, the final task is to document it well. Considerations of the benefits and harms of interventions and how the patient’s autonomy was respected should be well documented and should be concordant with the events that transpired.
























































































































