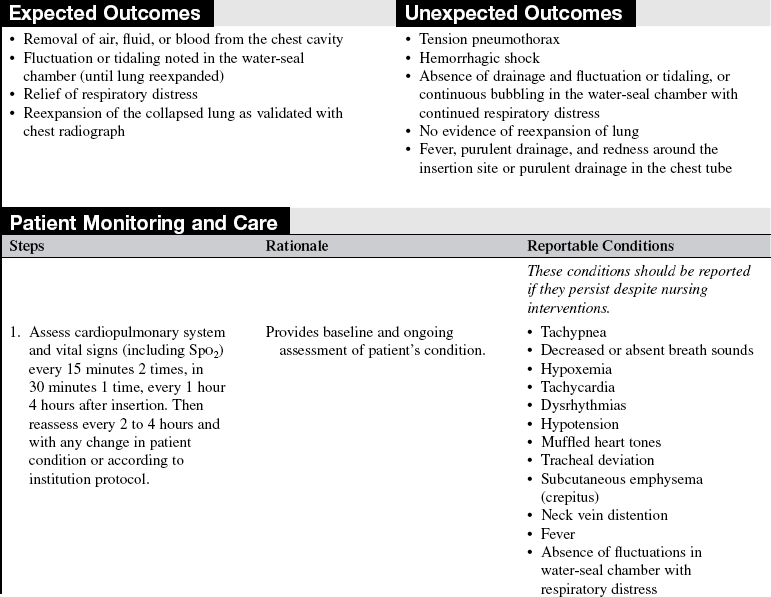
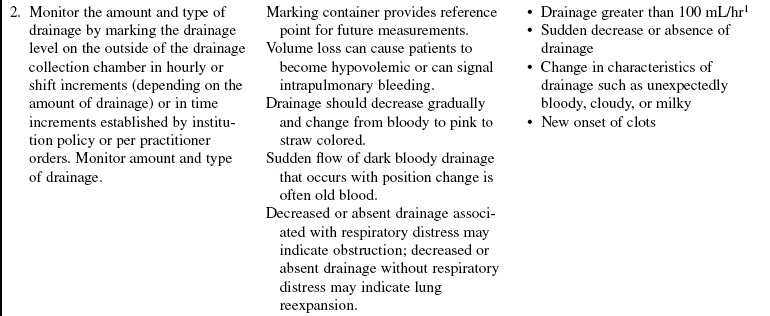
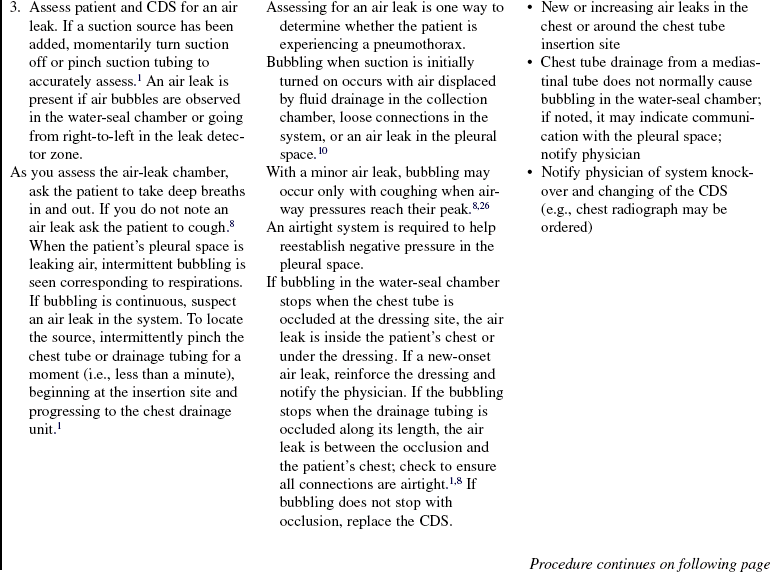
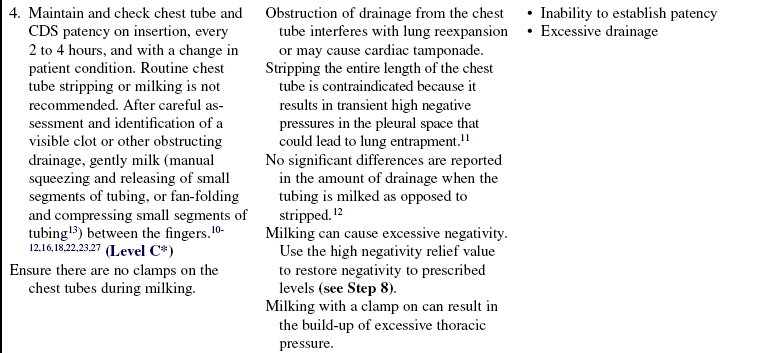
Closed Chest Drainage System
PREREQUISITE NURSING KNOWLEDGE
• Anatomy and physiology of the pulmonary system should be understood.
• Normal intrapleural pressures measure approximately −4 cm H2O during expiration. At end inspiration, pressure decreases to −8 cm H2O.15
• Closed chest drainages systems are used to facilitate the evacuation of fluid, blood, and air from the pleural space, the mediastinum, or both; to restore negative pressure to the pleural space; and to promote reexpansion of a collapsed lung.
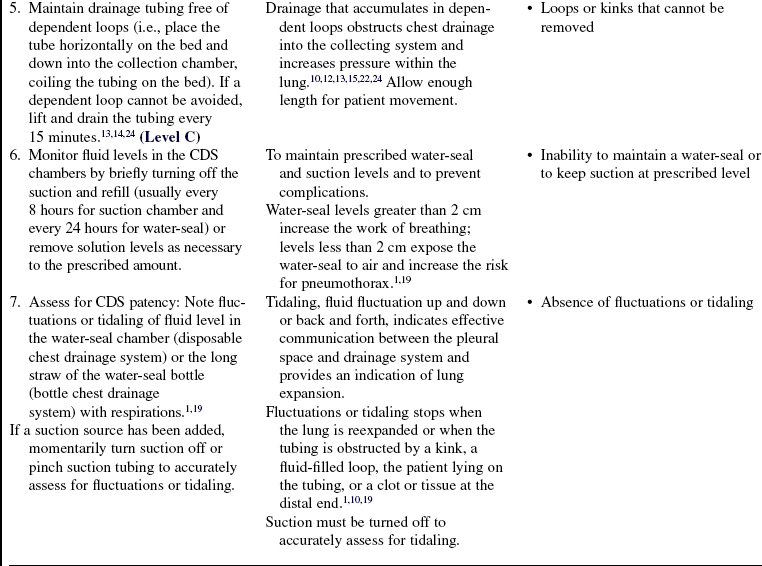
• Closed chest drainage systems (CDSs) include:
 Dry suction with a traditional water-seal; dry suction with a one-way valve; wet suction with a traditional water-seal; and one-bottle, two-bottle, three-bottle, and four-bottle setups
Dry suction with a traditional water-seal; dry suction with a one-way valve; wet suction with a traditional water-seal; and one-bottle, two-bottle, three-bottle, and four-bottle setups
 Gravity, suction, or both to restore negative pressure and remove air, fluid, and blood from the pleural space or the mediastinum
Gravity, suction, or both to restore negative pressure and remove air, fluid, and blood from the pleural space or the mediastinum
 A one-way mechanism created by a water-seal that permits air and fluid to be removed and prevents backflow into the chest
A one-way mechanism created by a water-seal that permits air and fluid to be removed and prevents backflow into the chest
 Greater pressure within the chest than within the system; this requirement is accomplished by keeping the drainage unit at least 1 foot below the chest tube insertion site and the tubing free of dependent loops and obstructions,1,11,13,26 which prevents siphoning of the contents back into the pleural cavity26
Greater pressure within the chest than within the system; this requirement is accomplished by keeping the drainage unit at least 1 foot below the chest tube insertion site and the tubing free of dependent loops and obstructions,1,11,13,26 which prevents siphoning of the contents back into the pleural cavity26
 Differences in flow rates and in accuracy of delivered negative pressures noted in chest drainage systems that were not likely to be clinically important6,7
Differences in flow rates and in accuracy of delivered negative pressures noted in chest drainage systems that were not likely to be clinically important6,7
• Currently, guidelines recommend that a water-seal alone is safe for most patients with a pneumothorax or small air leak.2–5,8,9,20,25 However, if the pneumothorax or air leak is large, expanding, or persistent, suction is recommended.5,8,9
• The most common amount of suction pressure ranges from −10 to −20 cm H2O.1,3,8,14 High suction levels may cause persistent pleural air leaks, air stealing, lung tissue entrapment, and reexpansion pulmonary edema.14,17
• The addition of a suction source can enhance drainage when large volumes of air or fluid must be evacuated.
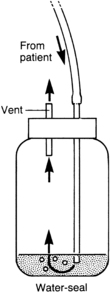
 Some systems and suction devices (e.g., Emerson pump, Cambridge, MA) contain an exit vent from the water-seal chamber that ensures the drainage unit remains vented when the suction device is off. Do not close or occlude the exit vent.19,26 With use of CDSs without an exit vent, the drainage systems should be disconnected from suction before they are turned off.19,26
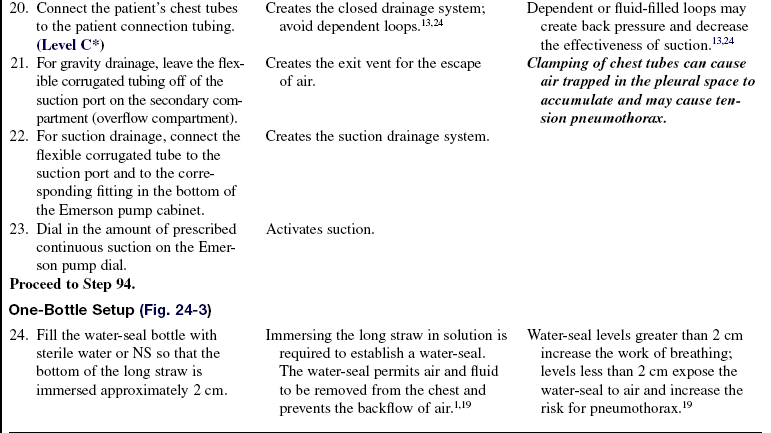
Some systems and suction devices (e.g., Emerson pump, Cambridge, MA) contain an exit vent from the water-seal chamber that ensures the drainage unit remains vented when the suction device is off. Do not close or occlude the exit vent.19,26 With use of CDSs without an exit vent, the drainage systems should be disconnected from suction before they are turned off.19,26
 Some wall-mounted suction devices need control and pressure gauges to regulate and monitor for potential surges in suction levels.15,19,26
Some wall-mounted suction devices need control and pressure gauges to regulate and monitor for potential surges in suction levels.15,19,26
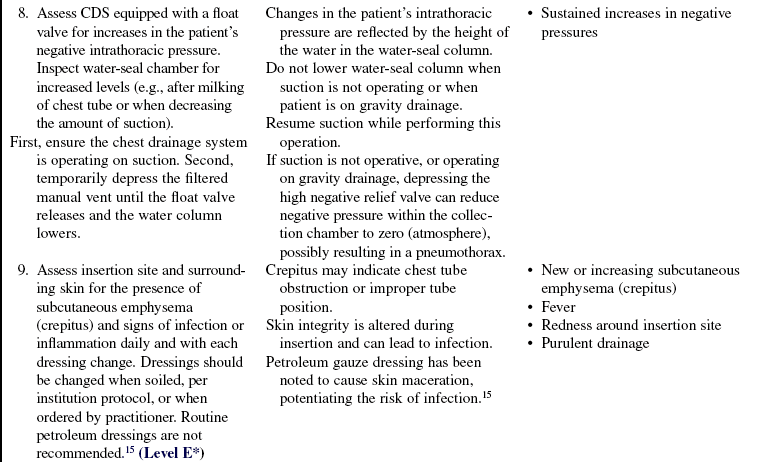
• If clinically desirable, some disposable wet suction with traditional water-seal drainage systems can provide suction levels greater than −25 cm H2O. The suction chamber vent holes can be occluded with nonporous tape or by replacing them with the manufacturer’s special pronged vent plug and connecting directly to wall regulator suction. Suction levels must be converted from prescribed levels of cm H2O suction to mm Hg of wall suction (Table 24-1).
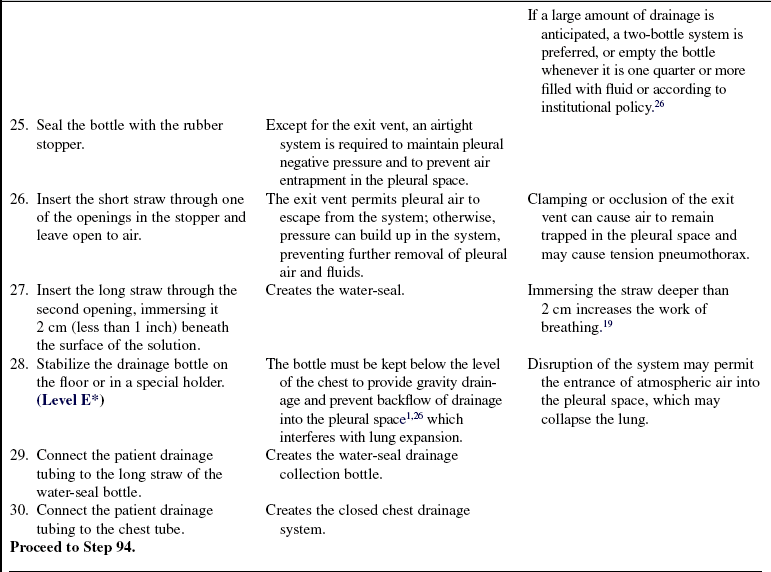
Table 24-1
| cm H2O | mm Hg |
| 20 | 15 |
| 25 | 18 |
| 30 | 22 |
| 35 | 26 |
| 40 | 30 |
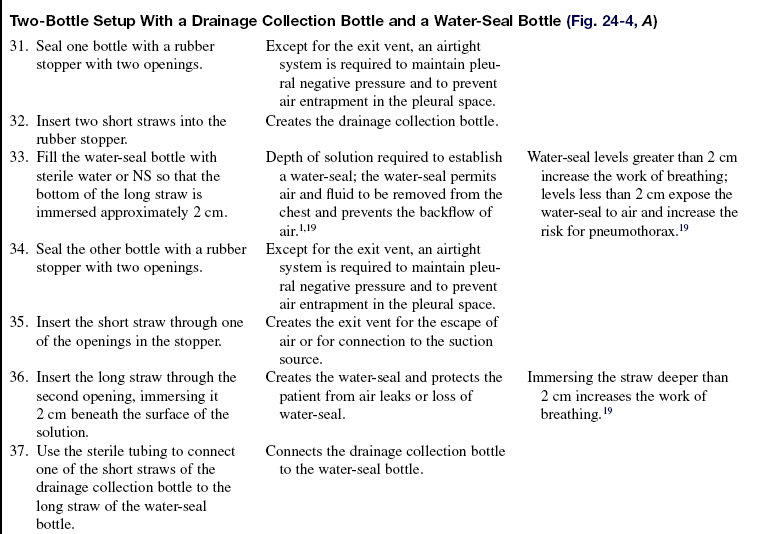
| 45 | 33 |
| 50 | 37 |
| 60 | 44 |
Reprinted with permission of Atrium Medical Corporation, Hudson, NH.
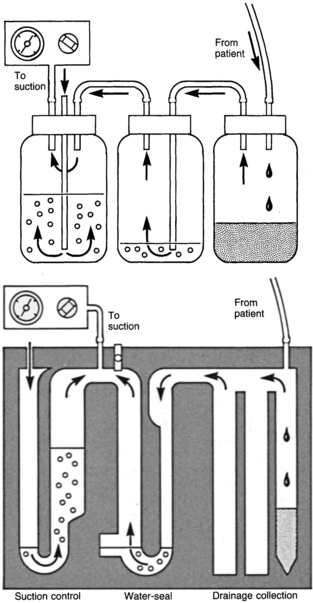
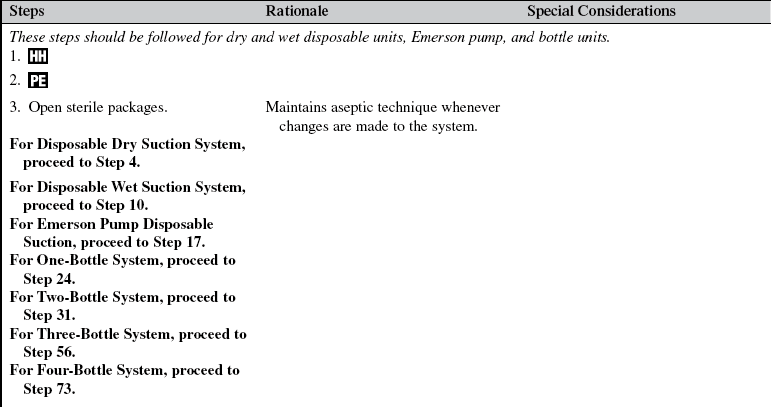
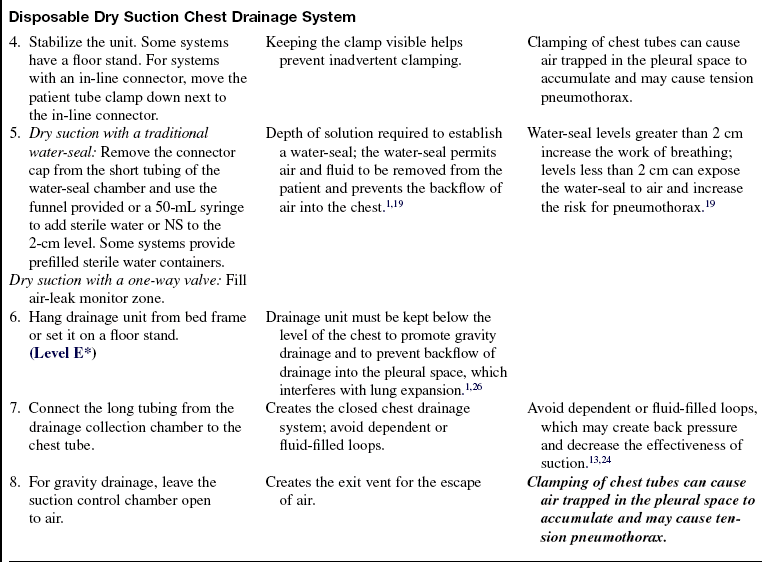
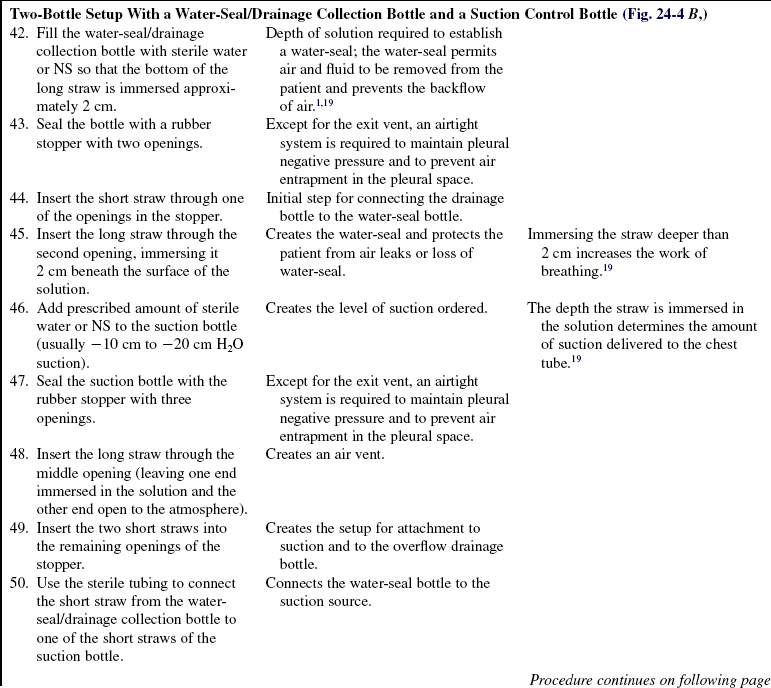
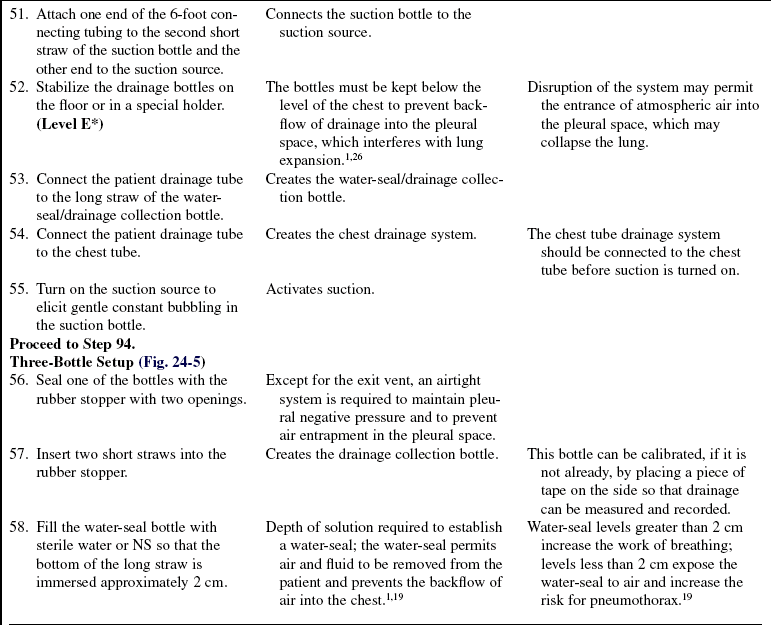
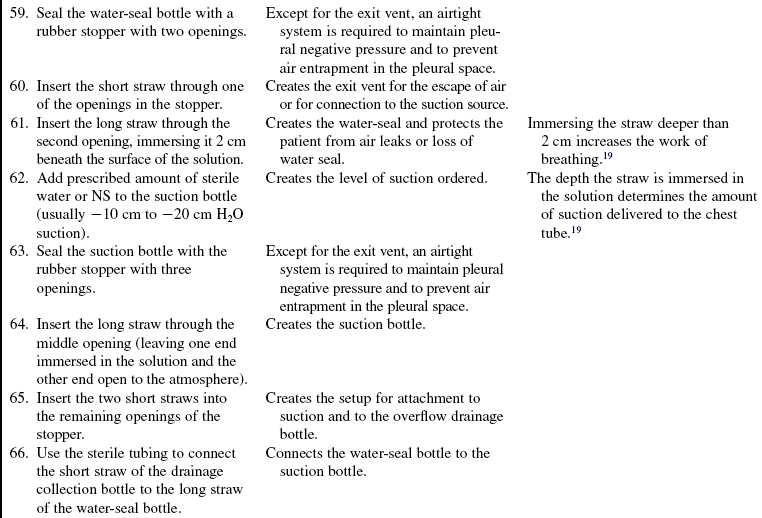
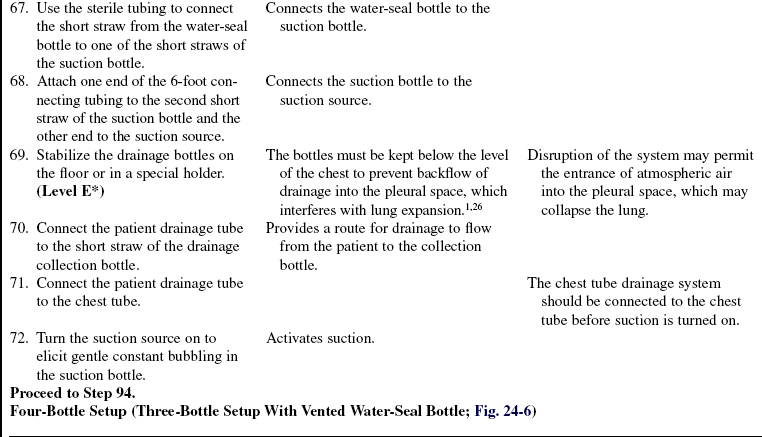
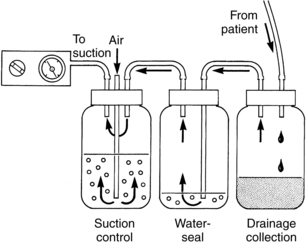
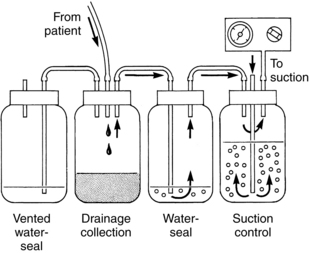
 Correlate to the three-bottle drainage system, with collection, water-seal, and suction control chambers positioned side by side in a molded plastic disposable unit (Fig. 24-1). These include the Pleur-Evac, Thora-Klex, Argyle, and Atrium systems.
Correlate to the three-bottle drainage system, with collection, water-seal, and suction control chambers positioned side by side in a molded plastic disposable unit (Fig. 24-1). These include the Pleur-Evac, Thora-Klex, Argyle, and Atrium systems.
 Are equipped with a positive-pressure relief valve used to prevent a tension pneumothorax if the suction tubing becomes accidentally occluded or if the suction source fails. In addition, automatic and manual pressure relief valves vent excessive negative pressure, such as may occur during deep inspiration or with milking of the chest tube.
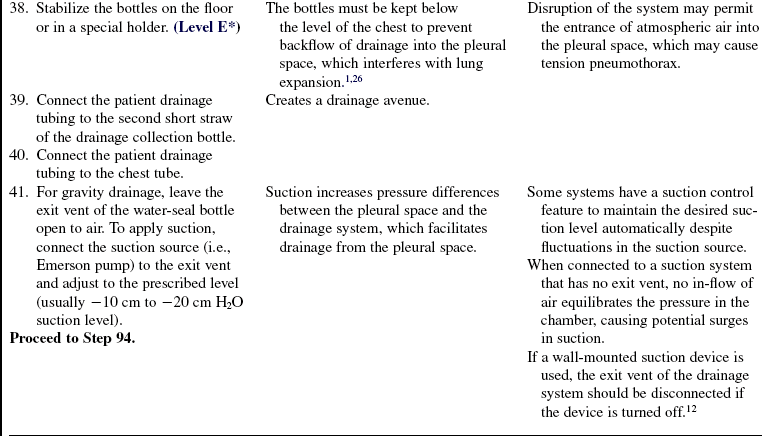
Are equipped with a positive-pressure relief valve used to prevent a tension pneumothorax if the suction tubing becomes accidentally occluded or if the suction source fails. In addition, automatic and manual pressure relief valves vent excessive negative pressure, such as may occur during deep inspiration or with milking of the chest tube.
 May have replaceable collection chambers, which can be removed when filled and replaced with a new one without changing the entire unit.
May have replaceable collection chambers, which can be removed when filled and replaced with a new one without changing the entire unit.
 Have self-sealing ports or collection tubes for aspiration of drainage samples and removal of excess chamber fluid levels.
Have self-sealing ports or collection tubes for aspiration of drainage samples and removal of excess chamber fluid levels.
• Some systems have accessories that may be used to convert them to an autotransfusion unit.
• Some CDSs use dry suction with a traditional water-seal and either a regulator or a restricted orifice mechanism. Although water is added to the water-seal chamber, water does not need to be added to the suction chamber. Instead, the suction source (usually a wall regulator) is increased until an indicator appears.
• Some CDSs are waterless, referred to as dry-dry drains, and have a one-way valve, which eliminates the need to fill any chambers (except an air-leak indicator zone, as needed). A valve opens on expiration and allows patient air to exit, then closes to prevent atmospheric air from entering during inspiration. This one-way valve feature allows the system to be used in the vertical or horizontal position without loss of the seal. These systems are safe if accidentally tipped. The amount of suction delivered is regulated with an adjustable dial.
• Advantages of dry suction are ease of setup; ease of application if higher, more precise levels of suction are needed; and a quiet system.
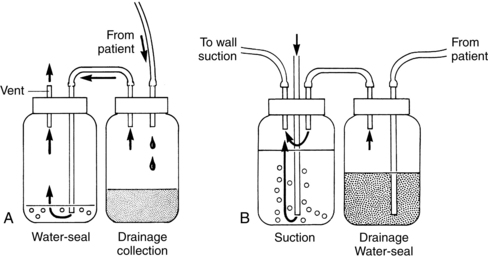
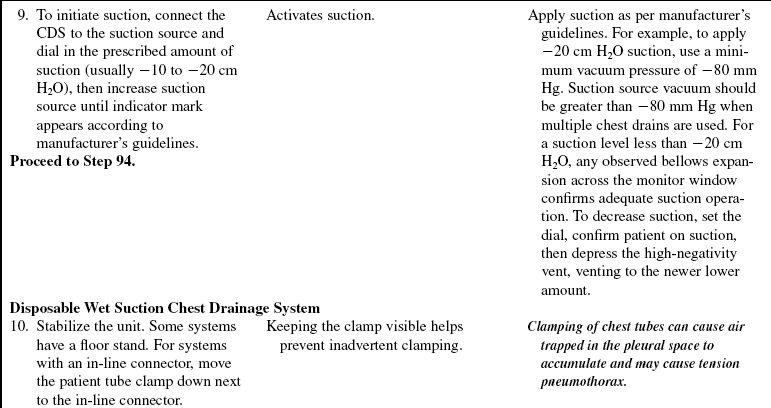
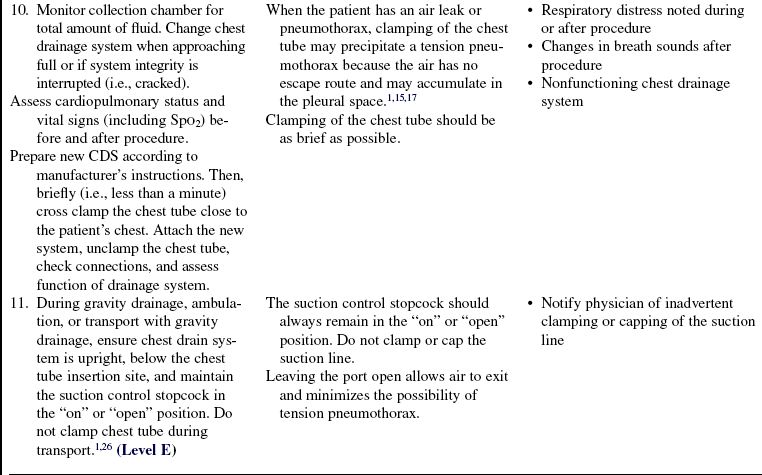
• Some clinicians suggest use of the Emerson pump (Fig. 24-2) for patients with large bronchopleural air leaks because they are high-volume, low-resistance, portable suction devices capable of handling high airflow rates.14,15
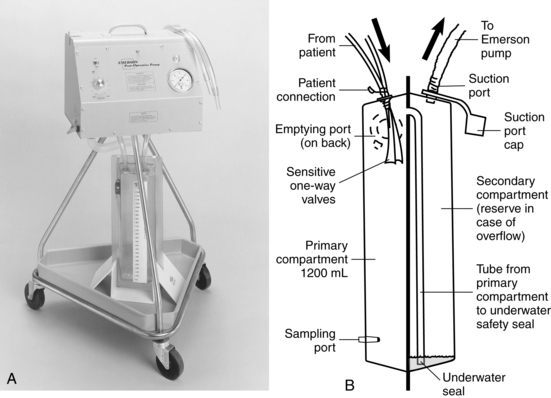
Figure 24-2 A, Emerson pump. B, Emerson disposable chest drain system. (Courtesy J.H. Emerson, Cambridge, MA.)
• Tidaling, fluctuations that occur with inspiration and expiration, provides a continuous manometer of the pressure changes in the pleural space and indicates overall respiratory effort. Absence of fluctuations suggests obstruction of the drainage system from clots, contact with lung tissue, kinks, loss of subatmospheric pressure from fluid-filled dependent loops, or complete reexpansion of the lung.1,10,19
• Except for the exit vent, an airtight system is required to assist in maintaining negative pressure in the pleura and to prevent air entrapment in the pleural space.
• In general, clamping of chest tubes is contraindicated. Clamping a chest tube in a patient with a pleural air leak may cause a tension pneumothorax. The few situations in which chest tubes may be clamped briefly (i.e., less than a minute) include locating the source of an air leak, replacing the chest drainage system, determining whether a patient is ready to have the chest tube removed, and during chest tube removal.1,14,15,21,26
EQUIPMENT
Disposable Setup (Wet and Dry Systems)
Two-Bottle System
PATIENT AND FAMILY EDUCATION
• Explain the procedure, the indication for the chest tube insertion, and how the closed chest drainage system works.  Rationale: This communication identifies patient and family knowledge deficits about the patient’s condition, procedure, expected benefits, and potential risks and allows time for questions to clarify information and to voice concerns. Explanations decrease patient anxiety and enhance cooperation.
Rationale: This communication identifies patient and family knowledge deficits about the patient’s condition, procedure, expected benefits, and potential risks and allows time for questions to clarify information and to voice concerns. Explanations decrease patient anxiety and enhance cooperation.
• After chest tube insertion, instruct the patient to sit in a semi-Fowler’s position (unless contraindicated).  Rationale: Proper positioning facilitates drainage from the lung by allowing air to rise and fluid to settle, enhancing removal via the chest tube. This position also makes breathing easier.
Rationale: Proper positioning facilitates drainage from the lung by allowing air to rise and fluid to settle, enhancing removal via the chest tube. This position also makes breathing easier.
• Instruct the patient to turn and reposition every 2 hours to facilitate drainage. The patient may lie on the side with the chest tube but should keep the tubing free of kinks.  Rationale: Turning and positioning prevents complications related to immobility and retained secretions. Keeping the tubing free of kinks maintains patency of the tube, facilitates drainage, and prevents the accumulation of pressure within the pleural space, which interferes with lung reexpansion.
Rationale: Turning and positioning prevents complications related to immobility and retained secretions. Keeping the tubing free of kinks maintains patency of the tube, facilitates drainage, and prevents the accumulation of pressure within the pleural space, which interferes with lung reexpansion.
• Instruct the patient to cough and deep breathe, with splinting of the affected side or sternum (if mediastinal tube is in place).  Rationale: Coughing and deep breathing increase pressure within the pleural space, facilitating drainage, promoting lung reexpansion, and preventing respiratory complications associated with retained secretions. The application of firm pressure over the chest tube insertion site (e.g., splinting) decreases pain and discomfort.
Rationale: Coughing and deep breathing increase pressure within the pleural space, facilitating drainage, promoting lung reexpansion, and preventing respiratory complications associated with retained secretions. The application of firm pressure over the chest tube insertion site (e.g., splinting) decreases pain and discomfort.
• Encourage active or passive range-of-motion exercises of the arm on the affected side.  Rationale: The patient may limit the movement of the arm on the affected side to decrease the discomfort at the insertion site, which results in joint discomfort and potential joint complications.
Rationale: The patient may limit the movement of the arm on the affected side to decrease the discomfort at the insertion site, which results in joint discomfort and potential joint complications.
• Instruct the patient and family about activity as prescribed while maintaining the drainage system below the level of the chest.  Rationale: The drainage system is maintained below the level of the chest to facilitate gravity drainage and to prevent backflow into the pleural space and potential infectious contamination into the pleural space.
Rationale: The drainage system is maintained below the level of the chest to facilitate gravity drainage and to prevent backflow into the pleural space and potential infectious contamination into the pleural space.
• Instruct the patient and family about the availability of prescribed analgesic medication and other pain relief strategies.  Rationale: Pain relief ensures comfort and facilitates coughing, deep breathing, positioning, and range-of-motion exercises and promotes healing.
Rationale: Pain relief ensures comfort and facilitates coughing, deep breathing, positioning, and range-of-motion exercises and promotes healing.
PATIENT ASSESSMENT AND PREPARATION
Patient Assessment
• Assess significant medical history or injury, including chronic lung disease, spontaneous pneumothorax, pulmonary disease, therapeutic procedures, and mechanism of injury.  Rationale: Medical history or injury may provide the etiologic basis for the occurrence of pneumothorax, hemothorax, empyema, pleural effusion, or chylothorax.
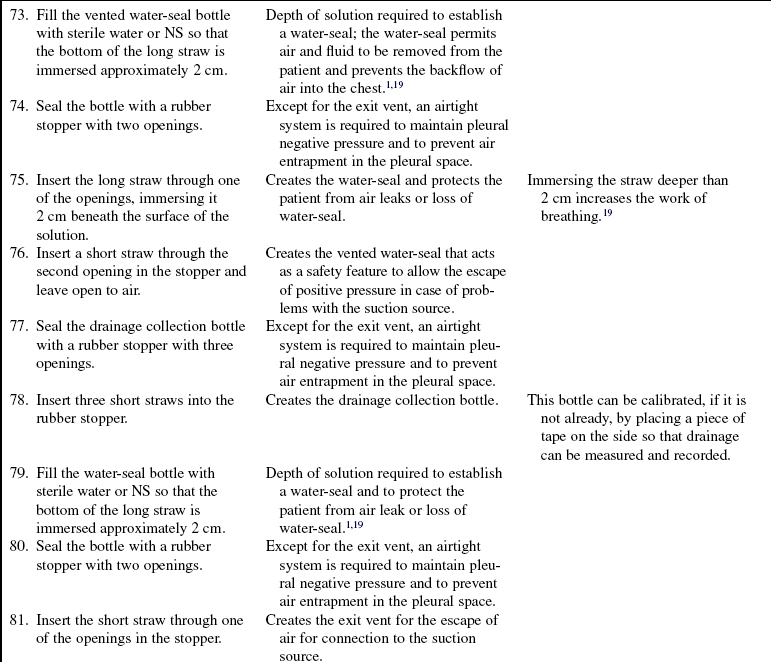
Rationale: Medical history or injury may provide the etiologic basis for the occurrence of pneumothorax, hemothorax, empyema, pleural effusion, or chylothorax.
• Assess baseline cardiopulmonary status, as follows:
 Vital signs (blood pressure, heart rate, respiratory rate)
Vital signs (blood pressure, heart rate, respiratory rate)
 Shortness of breath or dyspnea
Shortness of breath or dyspnea
 Anxiety, restlessness, or apprehension
Anxiety, restlessness, or apprehension
 Decreased oxygen saturation (e.g., pulse oxymetry [SpO2])
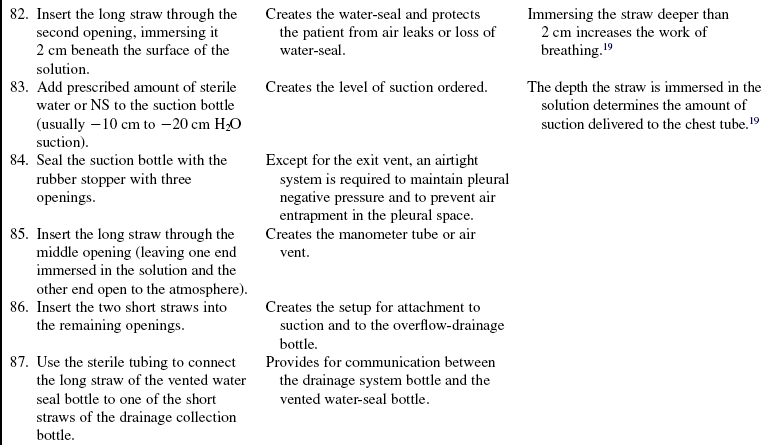
Decreased oxygen saturation (e.g., pulse oxymetry [SpO2])
 Decreased or absent breath sounds on the affected side
Decreased or absent breath sounds on the affected side
 Crackles adjacent to the affected area
Crackles adjacent to the affected area
 Asymmetrical chest excursion with respirations
Asymmetrical chest excursion with respirations
 Hyperresonance with percussion on the affected side (pneumothorax)
Hyperresonance with percussion on the affected side (pneumothorax)
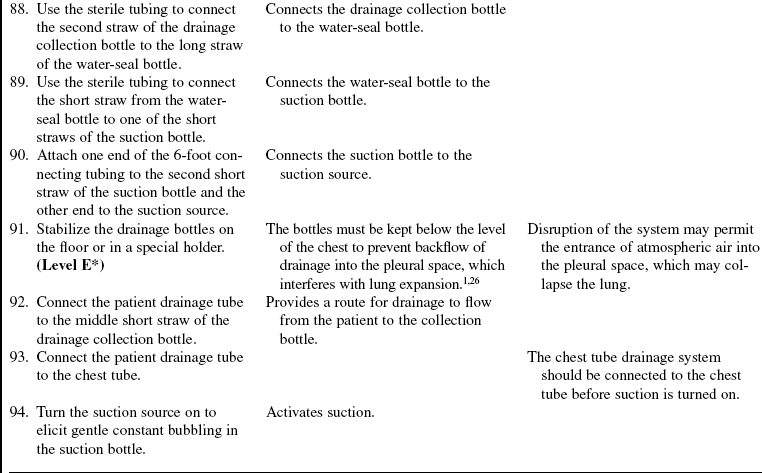
 Dullness or flatness with percussion on the affected side (hemothorax, pleural effusion, empyema, or chylothorax)
Dullness or flatness with percussion on the affected side (hemothorax, pleural effusion, empyema, or chylothorax)
 Subcutaneous emphysema or crepitus (pneumothorax)
Subcutaneous emphysema or crepitus (pneumothorax)
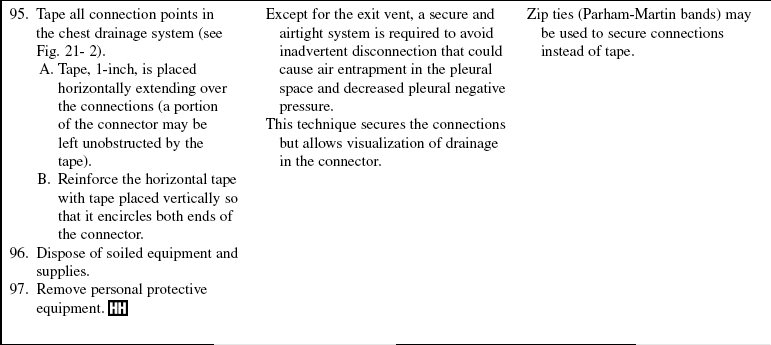
 Tracheal deviation to the unaffected side (tension pneumothorax)
Tracheal deviation to the unaffected side (tension pneumothorax)
•  Rationale: Accurate assessment of signs and symptoms allows for prompt recognition and treatment. Baseline assessment provides comparison data for evaluation of changes and outcomes of treatment.
Rationale: Accurate assessment of signs and symptoms allows for prompt recognition and treatment. Baseline assessment provides comparison data for evaluation of changes and outcomes of treatment.
• Assess diagnostic tests (if patient’s condition does not necessitate immediate intervention):
•  Rationale: Diagnostic testing confirms the presence of air or fluid in the pleural space, a collapsed lung, hypoxemia, and respiratory compromise.
Rationale: Diagnostic testing confirms the presence of air or fluid in the pleural space, a collapsed lung, hypoxemia, and respiratory compromise.
Patient Preparation
• Ensure the patient understands pre-procedural teachings. Answer questions as they arise, and reinforce information as needed.  Rationale: This communication evaluates and reinforces understanding of previously presented information.
Rationale: This communication evaluates and reinforces understanding of previously presented information.
• Verify correct patient with two identifiers.  Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
Rationale: Prior to performing a procedure, the nurse should ensure the correct identification of the patient for the intended intervention.
• Administer prescribed analgesics or sedatives as needed.  Rationale: Analgesics and sedatives reduce the discomfort and anxiety experienced, facilitating patient cooperation and improving outcomes.
Rationale: Analgesics and sedatives reduce the discomfort and anxiety experienced, facilitating patient cooperation and improving outcomes.
References
![]() 1. Allibone, L. Nursing management of chest drains. Nurs Stand. 2003; 17:45–56.
1. Allibone, L. Nursing management of chest drains. Nurs Stand. 2003; 17:45–56.
2. Alphonso, N, et al. A prospective randomized controlled trial of suction versus non-suction to the under-water seal drains following lung resection. Eur J Cardiothorac Surg. 2005; 27:391–394.
![]() 3. Ayed, AK, Suction versus water seal after thoracoscopy for primary spontaneous pneumothorax. prospective randomized study. Ann Thorac Surg 2003; 75:1593–1596.
3. Ayed, AK, Suction versus water seal after thoracoscopy for primary spontaneous pneumothorax. prospective randomized study. Ann Thorac Surg 2003; 75:1593–1596.
4. Baumann, MH. Management of spontaneous pneumothorax. Clin Chest Med. 2006; 27:369–381.
![]() 5. Baumann, MH, Management of spontaneous pneumothorax. an American College of Chest Physicians Delphi -consensus statement. Chest 2001; 119:590–602.
5. Baumann, MH, Management of spontaneous pneumothorax. an American College of Chest Physicians Delphi -consensus statement. Chest 2001; 119:590–602.
![]() 6. Baumann, MH. What size chest tube? What drainage system is ideal? And other chest tube management questions. Curr Opin Pulm Med. 2003; 9:276–281.
6. Baumann, MH. What size chest tube? What drainage system is ideal? And other chest tube management questions. Curr Opin Pulm Med. 2003; 9:276–281.
![]() 7. Baumann, MH, et al. Comparison of function of commercially available pleural drainage units and catheters. Chest. 2003; 123:1878–1886.
7. Baumann, MH, et al. Comparison of function of commercially available pleural drainage units and catheters. Chest. 2003; 123:1878–1886.
8. Cerfolio, RJ. Recent advances in the treatment of air leaks. Curr Opin Pulm Med. 2005; 11:319–323.
9. Cerfolio, RJ, et al. The management of chest tubes in -patients with a pneumothorax and an air leak after -pulmonary resection. Chest. 2005; 128:816–820.
![]() 10. Deshpande, KS, Tortolandi, AJ, Kvetan, V, Troubleshooting chest tube complications. how to prevent—or quickly correct—the major problems. J Crit Ill. 2003; 18(6):275–280.
10. Deshpande, KS, Tortolandi, AJ, Kvetan, V, Troubleshooting chest tube complications. how to prevent—or quickly correct—the major problems. J Crit Ill. 2003; 18(6):275–280.
![]() 11. Duncan, C, Erickson, R. Pressures associated with chest tube stripping. Heart Lung. 1982; 11:71–166.
11. Duncan, C, Erickson, R. Pressures associated with chest tube stripping. Heart Lung. 1982; 11:71–166.
![]() 12. Duncan, C, Erickson, R, Wiegel, RM. Effect of chest tube management on drainage after cardiac surgery. Heart Lung. 1987; 16:1–9.
12. Duncan, C, Erickson, R, Wiegel, RM. Effect of chest tube management on drainage after cardiac surgery. Heart Lung. 1987; 16:1–9.
![]() 13. Gordon, PA, et al, Positioning of chest tubes. effects on pressure and drainage. Am J Crit Care 1997; 6:33–38.
13. Gordon, PA, et al, Positioning of chest tubes. effects on pressure and drainage. Am J Crit Care 1997; 6:33–38.
![]() 14. Gordon, PA, Norton, JM, Merrell, R, Redefining chest tube management. analysis of the state of practice. Dimens Crit Care Nurs 1995; 14:6–13.
14. Gordon, PA, Norton, JM, Merrell, R, Redefining chest tube management. analysis of the state of practice. Dimens Crit Care Nurs 1995; 14:6–13.
![]() 15. Gross, SB. Current challenges, concepts and controversies in chest tube management. AACN Clin Issues Crit Care Nurs. 1993; 4:75–260.
15. Gross, SB. Current challenges, concepts and controversies in chest tube management. AACN Clin Issues Crit Care Nurs. 1993; 4:75–260.
16. Halm, MA. To strip or not to strip? Physiological effects of chest tube manipulation. Am J Crit Care. 2007; 16(6):609–612.
![]() 17. Henry, M, Arnold, T, Harvey, J. British Thoracic Society guidelines for the management of spontaneous pneumothorax. Thorax. 2003; 58:39–52.
17. Henry, M, Arnold, T, Harvey, J. British Thoracic Society guidelines for the management of spontaneous pneumothorax. Thorax. 2003; 58:39–52.
![]() 18. Isaacson, JJ, George, IT, Brewer, MJ. The effect of chest tube manipulation on mediastinal drainage. Heart Lung. 1986; 15(6):601–605.
18. Isaacson, JJ, George, IT, Brewer, MJ. The effect of chest tube manipulation on mediastinal drainage. Heart Lung. 1986; 15(6):601–605.
![]() 19. Kam, AC, O’Brien, M, Kam, PCA. Pleural drainage systems. Anaesthesia. 1993; 48:154–161.
19. Kam, AC, O’Brien, M, Kam, PCA. Pleural drainage systems. Anaesthesia. 1993; 48:154–161.
20. Kelly, AM, Review of management of primary spontaneuos pneumothorax. is the best evidence clearer 15 years on. Emerg Med Aust 2007; 19:303–308.
21. Lehwaldt, D, Timmins, F, Nurses’ knowledge of chest drain care. an exploratory descriptive survey. Nurs Crit Care. 2005; 10(4):192–200.
![]() 22. Lim-Levy, F, et al. Is milking and stripping chest tubes really necessary. Ann Thorac Surg. 1986; 42:77–80.
22. Lim-Levy, F, et al. Is milking and stripping chest tubes really necessary. Ann Thorac Surg. 1986; 42:77–80.
![]() 23. Pierce, J, Piazza, D, Naftel, DC, Effects of two chest tube clearance protocols on drainage in patients after myocardial revascularization surgery. Heart Lung . 1991; 20:125–130.
23. Pierce, J, Piazza, D, Naftel, DC, Effects of two chest tube clearance protocols on drainage in patients after myocardial revascularization surgery. Heart Lung . 1991; 20:125–130.
![]() 24. Schmelz, JO, et al. Effects of position of chest drainage tube on volume drained and pressure. Am J Crit Care. 1999; 8:319–323.
24. Schmelz, JO, et al. Effects of position of chest drainage tube on volume drained and pressure. Am J Crit Care. 1999; 8:319–323.
25. Stolz, AJ, et al. Predictors of prolonged air leak following pulmonary lobectomy. Eur J Cardiothorac Surg. 2005; 334–336.
![]() 26. Tang, AT, Velissaris, TJ, Weeden, DF, An evidence-based approach to drainage of the pleural cavity. evaluation of best practice. J Eval Clin Pract 2002; 8:333–340.
26. Tang, AT, Velissaris, TJ, Weeden, DF, An evidence-based approach to drainage of the pleural cavity. evaluation of best practice. J Eval Clin Pract 2002; 8:333–340.
![]() 27. Wallen, M, et al, Mediastinal chest drain clearance for cardiac surgery. Cochrane Database of Systematic Review 2004;, doi: 10/1002/14651858. CD003042. pub2. [2:Art. No. : CD003042].
27. Wallen, M, et al, Mediastinal chest drain clearance for cardiac surgery. Cochrane Database of Systematic Review 2004;, doi: 10/1002/14651858. CD003042. pub2. [2:Art. No. : CD003042].