Procedure 23 Thoracoplasty for Rib Deformity
Indications
 Adolescent/adult scoliosis: Rib prominence is associated with rigid, rotated, decompensated thoracic and double major curves. In these patients, a convex thoracoplasty may be necessary if it is not possible to fully derotate the curves during posterior instrumented spinal fusion. An example would be a rib hump greater than 4 cm, rib angle greater than 15 degrees, and curve flexibility less than 50%.
Adolescent/adult scoliosis: Rib prominence is associated with rigid, rotated, decompensated thoracic and double major curves. In these patients, a convex thoracoplasty may be necessary if it is not possible to fully derotate the curves during posterior instrumented spinal fusion. An example would be a rib hump greater than 4 cm, rib angle greater than 15 degrees, and curve flexibility less than 50%.
 Rib hump deformity is a common finding in the three-dimensional evolution of adolescent idiopathic scoliosis. Albeit a cosmetic concern, rib hump deformity is a major source of patients’ postoperative dissatisfaction if not corrected to their expectations. The effect of thoracoplasty on pulmonary function has been a topic of interest, with varying reports of clinical significance.
Rib hump deformity is a common finding in the three-dimensional evolution of adolescent idiopathic scoliosis. Albeit a cosmetic concern, rib hump deformity is a major source of patients’ postoperative dissatisfaction if not corrected to their expectations. The effect of thoracoplasty on pulmonary function has been a topic of interest, with varying reports of clinical significance.
 Rib prominence associated with a compensated curve, where posterior spinal fusion is not necessary or a previously fused curve is present: the indication may be poor appearance or discomfort when sitting in a chair or leaning against a wall.
Rib prominence associated with a compensated curve, where posterior spinal fusion is not necessary or a previously fused curve is present: the indication may be poor appearance or discomfort when sitting in a chair or leaning against a wall.
 To increase flexibility of the curve: concave rib osteotomies and elevation of the concavity dorsally out of the chest may be present.
To increase flexibility of the curve: concave rib osteotomies and elevation of the concavity dorsally out of the chest may be present.
Indications Pitfalls
Indications Controversies
Examination/Imaging
 Measurement of angle of thoracic rotation (ATR) by inclinometer
Measurement of angle of thoracic rotation (ATR) by inclinometer
 Radiographs: full-length posteroanterior, lateral, bending, and Stagnara views
Radiographs: full-length posteroanterior, lateral, bending, and Stagnara views
Surgical Anatomy
 Ribs/transverse process: parts of the ribs corresponding to vertebrae in the structural curve are resected.
Ribs/transverse process: parts of the ribs corresponding to vertebrae in the structural curve are resected.
Positioning
 The patient is positioned prone on a Jackson table in the standard manner for a posterior spinal fusion. Preparation and draping with wide lateral margins is advised to better assess and visualize the rib prominence.
The patient is positioned prone on a Jackson table in the standard manner for a posterior spinal fusion. Preparation and draping with wide lateral margins is advised to better assess and visualize the rib prominence.
Positioning Pearls
Portals/Exposures
 For concave rib osteotomies to increase scoliotic curve flexibility, the steps are similar.
For concave rib osteotomies to increase scoliotic curve flexibility, the steps are similar.
Portals/Exposures Pearls
Portals/Exposures Pitfalls
Portals/Exposures Instrumentation
Portals/Exposures Controversies
Procedure
Step 1
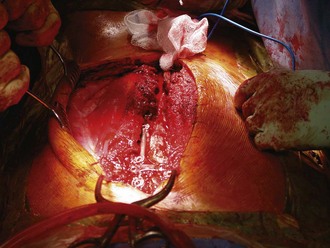
 The ribs that are to be resected are palpated, and a subperiosteal exposure of the rib, 2 to 3 cm lateral to the transverse process, or as close to the apical portion of the rib as possible, is started with Bovie electrocautery in its midline (Figure 23-2).
The ribs that are to be resected are palpated, and a subperiosteal exposure of the rib, 2 to 3 cm lateral to the transverse process, or as close to the apical portion of the rib as possible, is started with Bovie electrocautery in its midline (Figure 23-2).
 A Freer elevator, a small Cobb elevator, or an Alexander elevator is used to subperiosteally expose each rib on its dorsal surface over the entire length of the resection (usually 2 cm is needed).
A Freer elevator, a small Cobb elevator, or an Alexander elevator is used to subperiosteally expose each rib on its dorsal surface over the entire length of the resection (usually 2 cm is needed).
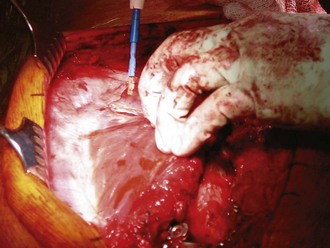
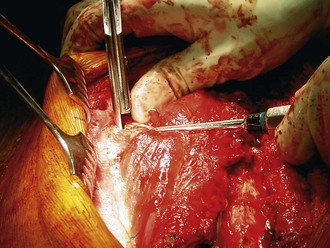
 A small elevator or curved hemostat is gently passed underneath (ventrally) the rib subperiosteally; care is taken to avoid injury to the pleura underneath (Figures 23-3 and 23-4).
A small elevator or curved hemostat is gently passed underneath (ventrally) the rib subperiosteally; care is taken to avoid injury to the pleura underneath (Figures 23-3 and 23-4).
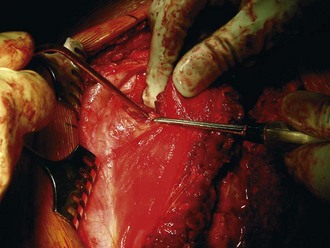
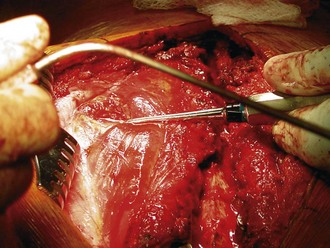
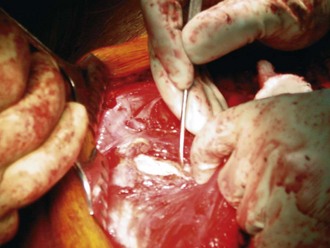
 A Doyen elevator is passed circumferentially and swept both medially and laterally to extend the exposure for a short distance, facilitating confirmation of adequate subperiosteal release of the rib (Figures 23-5 and 23-6).
A Doyen elevator is passed circumferentially and swept both medially and laterally to extend the exposure for a short distance, facilitating confirmation of adequate subperiosteal release of the rib (Figures 23-5 and 23-6).
Step 1 Pearls
Step 1 Instrumentation/Implantation
Step 1 Controversies
Step 2
 Two right-angle retractors are placed on the medial side of the rib, pulling back the paraspinal muscle.
Two right-angle retractors are placed on the medial side of the rib, pulling back the paraspinal muscle.
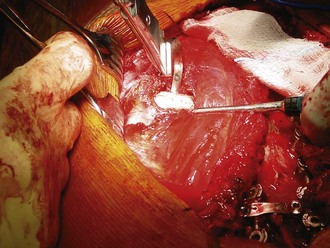
 A Cobb elevator is used to strip the periosteum further to expose the medialmost attachment of the rib to the transverse process (Figure 23-7).
A Cobb elevator is used to strip the periosteum further to expose the medialmost attachment of the rib to the transverse process (Figure 23-7).
 A rib cutter is then passed around the rib and pushed as far medially as possible, up against the transverse process (Figure 23-8). The rib is then cut medially, with the ideal cutting plane being exactly parallel to the floor.
A rib cutter is then passed around the rib and pushed as far medially as possible, up against the transverse process (Figure 23-8). The rib is then cut medially, with the ideal cutting plane being exactly parallel to the floor.
 The rib cutter is moved laterally, and about 2 cm should be initially resected (Figure 23-9). Starting at the apical levels, a symmetric resection of the ribs is made both proximal and distal to the apex. In general, as one goes more proximal and distal, less rib is cut. The most important and challenging aspect of this procedure is achieving ideal visual assessment of the rib deformity, which guides the extent of the resection (Figure 23-10).
The rib cutter is moved laterally, and about 2 cm should be initially resected (Figure 23-9). Starting at the apical levels, a symmetric resection of the ribs is made both proximal and distal to the apex. In general, as one goes more proximal and distal, less rib is cut. The most important and challenging aspect of this procedure is achieving ideal visual assessment of the rib deformity, which guides the extent of the resection (Figure 23-10).
 Bone wax is applied to the ends of the ribs (lightly), and Gelfoam is packed into the periosteal bed to assist with hemostasis (Figure 23-11).
Bone wax is applied to the ends of the ribs (lightly), and Gelfoam is packed into the periosteal bed to assist with hemostasis (Figure 23-11).
Step 2 Pearls
• The rib is held with a towel clip to prevent its sharp edge from plunging through the pleura when it is cut.
• One can always return after the spinal correction and instrumentation portion of the procedure is completed to take more rib out, but it cannot be put back. Taking too much rib and creating a concavity is worse than leaving a residual rib deformity.
• The apex of the curve will translate to the midline of the spine, ultimately leaving a much larger gap than apparent at the time of rib resection.
Step 2 Pitfalls
Step 3
 The portions of the ribs that are resected can be morselized and used for autologous bone graft for fusion.
The portions of the ribs that are resected can be morselized and used for autologous bone graft for fusion.
 After the spinal instrumentation, correction, and bone grafting, the ribs may be brought together with heavy absorbable suture through small drill holes in the rib ends. This provides additional correction of the rib hump and stability of the rib ends to facilitate healing and patient comfort. The rib periosteum is approximated.
After the spinal instrumentation, correction, and bone grafting, the ribs may be brought together with heavy absorbable suture through small drill holes in the rib ends. This provides additional correction of the rib hump and stability of the rib ends to facilitate healing and patient comfort. The rib periosteum is approximated.
 A water test is performed to make absolutely certain the pleura is intact. Using a small pitcher, saline is poured into the wound carefully so as not to create any additional air bubbles. The anesthesiologist performs a Valsalva maneuver three times to look for a leak in the pleura. Any pleural leaks are repaired with 2-0 absorbable suture.
A water test is performed to make absolutely certain the pleura is intact. Using a small pitcher, saline is poured into the wound carefully so as not to create any additional air bubbles. The anesthesiologist performs a Valsalva maneuver three times to look for a leak in the pleura. Any pleural leaks are repaired with 2-0 absorbable suture.
 The intercostal muscle layer is approximated with a suture, and a medium Hemovac drain (Zimmer Inc., Warsaw, Ind.) is placed over the resected rib bed and brought out lateral to the spine. The thoracolumbar fascia is closed with a running long-acting absorbable suture, starting at the distal end of the wound.
The intercostal muscle layer is approximated with a suture, and a medium Hemovac drain (Zimmer Inc., Warsaw, Ind.) is placed over the resected rib bed and brought out lateral to the spine. The thoracolumbar fascia is closed with a running long-acting absorbable suture, starting at the distal end of the wound.
Step 3 Pearls
Postoperative Care and Expected Outcomes
 A small protective shell is applied over the rib resection area if desired. This shell helps avoid a postoperative flail chest and minimizes the motion of the cut ribs over the pleura, and it may decrease the accumulation of a pleural effusion. (This is optional.)
A small protective shell is applied over the rib resection area if desired. This shell helps avoid a postoperative flail chest and minimizes the motion of the cut ribs over the pleura, and it may decrease the accumulation of a pleural effusion. (This is optional.)
 Thoracoplasty may increase pain or mildly prolong the postoperative course following spinal fusion with instrumentation.
Thoracoplasty may increase pain or mildly prolong the postoperative course following spinal fusion with instrumentation.
 To allow mobilization, aggressive pulmonary toileting and chest physiotherapy is necessary, with adequate pain control.
To allow mobilization, aggressive pulmonary toileting and chest physiotherapy is necessary, with adequate pain control.
 Patients with moderate or severe pulmonary symptoms are monitored with semierect radiographs for 2 to 3 days. If a significant amount of pleural fluid accumulates and the patient is symptomatic, a thoracocentesis is performed; if fluid accumulation occurs a second time, a chest tube is considered.
Patients with moderate or severe pulmonary symptoms are monitored with semierect radiographs for 2 to 3 days. If a significant amount of pleural fluid accumulates and the patient is symptomatic, a thoracocentesis is performed; if fluid accumulation occurs a second time, a chest tube is considered.
 For small pleural effusions, oral or intravenous furosemide may be used to diurese the patient.
For small pleural effusions, oral or intravenous furosemide may be used to diurese the patient.
 A consistent decrease in pulmonary function is observed in the early postoperative period, which mandates proper patient selection. A decline of forced vital capacity (FVC) of 22%, forced expiratory volume in 1 second (FEV-1) of 24%, and total lung capacity of 25% were found in the first 6 months. Gradual improvement occurs over the next 3 years. Patients with less than 60% of predicted values should be cautiously approached as candidates for thoracoplasty.
A consistent decrease in pulmonary function is observed in the early postoperative period, which mandates proper patient selection. A decline of forced vital capacity (FVC) of 22%, forced expiratory volume in 1 second (FEV-1) of 24%, and total lung capacity of 25% were found in the first 6 months. Gradual improvement occurs over the next 3 years. Patients with less than 60% of predicted values should be cautiously approached as candidates for thoracoplasty.
 In 2007, Newton and colleagues set out to determine what factors could predict 2-year postoperative pulmonary function tests (PFTs) in patients with adolescent idiopathic scoliosis. In their prospective study, they found thoracoplasty to result in a significant PFT reduction. Their cohort included 107 patients who underwent thoracoplasty, out of 254 total patients. Of these 107, 51 were posterior spinal fusion (PSF) with thoracoplasty, and 56 were anterior approach with thoracoplasty. Fifty-four percent of thoracoplasty patients saw a 15% or greater decrease in their predicted PFTs. The decrease in PFTs was greater in the group who underwent anterior surgery.
In 2007, Newton and colleagues set out to determine what factors could predict 2-year postoperative pulmonary function tests (PFTs) in patients with adolescent idiopathic scoliosis. In their prospective study, they found thoracoplasty to result in a significant PFT reduction. Their cohort included 107 patients who underwent thoracoplasty, out of 254 total patients. Of these 107, 51 were posterior spinal fusion (PSF) with thoracoplasty, and 56 were anterior approach with thoracoplasty. Fifty-four percent of thoracoplasty patients saw a 15% or greater decrease in their predicted PFTs. The decrease in PFTs was greater in the group who underwent anterior surgery.
 In 2008, Suk and associates retrospectively reviewed outcomes of thoracoplasty in the setting of thoracic adolescent idiopathic scoliosis corrected with pedicle screw instrumentation. Three surgical groups were compared, looking specifically at deformity correction, the effects on pulmonary function tests, and complications. The groups were representative of no thoracoplasty, thoracoplasty without direct vertebral rotation, and thoracoplasty with direct vertebral rotation.
In 2008, Suk and associates retrospectively reviewed outcomes of thoracoplasty in the setting of thoracic adolescent idiopathic scoliosis corrected with pedicle screw instrumentation. Three surgical groups were compared, looking specifically at deformity correction, the effects on pulmonary function tests, and complications. The groups were representative of no thoracoplasty, thoracoplasty without direct vertebral rotation, and thoracoplasty with direct vertebral rotation.
 Suk demonstrated a statistically significant difference in the correction of rib hump deformities across the three surgical groups. Thoracoplasty with direct vertebral correction offered the greatest amount of correction. Additionally, there were no statistically significant decreases, nor differences between surgical groups regarding pulmonary function testing at the time of most recent follow-up (specifically measuring FVC and FEV-1). Suk recognized the failure to include a group with direct vertebral rotation alone and states this was because the population numbers were too small to include in statistical analyses.
Suk demonstrated a statistically significant difference in the correction of rib hump deformities across the three surgical groups. Thoracoplasty with direct vertebral correction offered the greatest amount of correction. Additionally, there were no statistically significant decreases, nor differences between surgical groups regarding pulmonary function testing at the time of most recent follow-up (specifically measuring FVC and FEV-1). Suk recognized the failure to include a group with direct vertebral rotation alone and states this was because the population numbers were too small to include in statistical analyses.
 Greggi and colleagues retrospectively reviewed outcomes of patients treated by posterior spinal fusion compared with those who underwent posterior spinal fusion with thoracoplasty. Their cohorts consisted of 40 patients each, with the majority of curves classified as Lenke 1 in both groups.
Greggi and colleagues retrospectively reviewed outcomes of patients treated by posterior spinal fusion compared with those who underwent posterior spinal fusion with thoracoplasty. Their cohorts consisted of 40 patients each, with the majority of curves classified as Lenke 1 in both groups.
 They found that PSF with thoracoplasty resulted in a significantly better main thoracic curve reduction, in addition to the absolute rib hump correction and the percent reduction of rib hump. Scoliosis Research Society scores were used to assess patient satisfaction, and no statistically significant differences were found between the groups, indicating thoracoplasty did not necessarily result in a more satisfactory cosmetic improvement than PSF alone. Regarding PFTs, there were no significant differences between the groups preoperatively and postoperatively. However, within each group, FVC and FEV-1 showed a statistically significant improvement postoperatively at the latest follow-up.
They found that PSF with thoracoplasty resulted in a significantly better main thoracic curve reduction, in addition to the absolute rib hump correction and the percent reduction of rib hump. Scoliosis Research Society scores were used to assess patient satisfaction, and no statistically significant differences were found between the groups, indicating thoracoplasty did not necessarily result in a more satisfactory cosmetic improvement than PSF alone. Regarding PFTs, there were no significant differences between the groups preoperatively and postoperatively. However, within each group, FVC and FEV-1 showed a statistically significant improvement postoperatively at the latest follow-up.
 Newton demonstrated that curves greater than 50 degrees in magnitude had a high risk of restrictive lung disease. None of the patients in the Suk or Greggi study suffered restrictive lung disease preoperatively. Thus the data they have presented demonstrating improvements in pulmonary function postoperatively, although statistically significant, may not be clinically significant.
Newton demonstrated that curves greater than 50 degrees in magnitude had a high risk of restrictive lung disease. None of the patients in the Suk or Greggi study suffered restrictive lung disease preoperatively. Thus the data they have presented demonstrating improvements in pulmonary function postoperatively, although statistically significant, may not be clinically significant.
 In summary, thoracoplasty does improve appearance and patient satisfaction in those patients undergoing surgery for scoliosis but increases operative time, blood loss, and may have a cost to pulmonary function and patient comfort.
In summary, thoracoplasty does improve appearance and patient satisfaction in those patients undergoing surgery for scoliosis but increases operative time, blood loss, and may have a cost to pulmonary function and patient comfort.
Barnes J. Rib resection in infantile idiopathic scoliosis. J Bone Joint Surg Br. 1979;61:31-35.
Barret DS, Maclean JG, Betany J, et al. Costoplasty in adolescent idiopathic scoliosis: objective results in 55 patients. J Bone Joint Surg Br. 1993;75:881-884.
Flinchum D. Rib resection in the treatment of scoliosis. South Med J. 1979;36:1378-1380.
Geissele AE, Ogilvie JW, Cohen M, et al. Thoracoplasty for treatment of rib prominence in thoracic scoliosis. Spine. 1994;19:1636-1639.
Greggi T, Bakaloudis G, Fusaro I, et al. Pulmonary function after thoracoplasty in the surgical treatment of adolescent idiopathic scoliosis. J Spinal Disord Tech. 2010;23:e63-e69.
Harvey JrCJ, Betz RR, Clements DH, Huss GK, Clancy M. Are there indications for partial rib resection in patients with adolescent scoliosis treated with Cotrel-Dubboset instrumentation? Spine. 1993;18:1593-1598.
Manning CW, Prime FJ, Zorab PA. Partial costectomy as a cosmetic operation in scoliosis. J Bone Joint Surg Br. 1973;55:521-527.
Newton PO, Perry A, Bastrom T, et al. Predictors of change in postoperative pulmonary function in adolescent idiopathic scoliosis: a prospective study of 254 patients. Spine. 2007;32:1875-1882.
Owen R, Turner A, Banforth JSG, Taylor JF, Jones RS. Costectomy as the first stage of surgery for scoliosis. J Bone Joint Surg Br. 1986;68:91-95.
Shufflebarger HL, Smiley K, Roth HJ. Internal thoracoplasty: a new procedure. Spine. 1994;19:840-844.
Steel HH. Rib resection and spine fusion in correction of convex deformity in scoliosis. J Bone Joint Surg Am. 1983;65:920-925.
Suk SI, Kim JH, Kim SS, Lee JJ, Han YT. Thoracoplasty in thoracic adolescent idiopathic scoliosis. Spine. 2008;33:1061-1067.
Thulburne T, Gillespie R. The rib hump in idiopathic scoliosis: measurement, analysis and response to treatment. J Bone Joint Surg Br. 1976;56:64-71.
Westgate HD, Moe JH. Pulmonary function in kyphoscoliosis before and after correction by Harrington instrumentation method. J Bone Joint Surg Am. 1969;51:935-946.