CHAPTER 23. Moderate Sedation/Analgesia
Jan Odom-Forren
OBJECTIVES
At the conclusion of this chapter, the reader will be able to:
1. Define moderate sedation, deep sedation, and general anesthesia.
2. Identify the statutory, regulatory, practice guidelines, and promulgated professional standards of care for nurses administering moderate sedation and analgesia.
3. State the components of presedation patient assessment.
4. List sedative and analgesic medications, dosing guidelines, and nursing considerations associated with their administration.
5. Identify required monitoring parameters for the patient receiving moderate sedation and analgesia.
6. State postsedation monitoring requirements for the patient receiving sedation.
7. Identify risk management strategies used to reduce the incidence of complications associated with the delivery of sedative and analgesic medications.
I. SEDATION
A. Definitions
1. Minimal sedation (anxiolysis)
a. Respond normally to verbal commands.
b. Cognitive function and coordination may be impaired.
c. Ventilatory and cardiovascular functions are unaffected.
2. Moderate sedation and analgesia (formerly referred to as “conscious sedation”)
a. A drug-induced depression of consciousness
b. Patients respond purposefully to verbal commands either alone or accompanied by light tactile stimulation.
c. No interventions required to maintain a patent airway
d. Spontaneous ventilation adequate
e. Cardiovascular function usually maintained
3. Deep sedation and analgesia
a. A drug-induced depression of consciousness
b. Patients cannot be easily aroused.
c. Respond purposefully after repeated or painful stimulation.
d. Independent ability to maintain ventilatory function may be impaired.
e. May require assistance in maintaining a patent airway
f. Spontaneous ventilation may be inadequate.
g. Cardiovascular function usually maintained
4. Anesthesia
a. Consists of general anesthesia and spinal or major regional anesthesia
b. Does not include local anesthesia
c. General anesthesia is a drug-induced loss of consciousness.
(1) Patients not arousable, even with painful stimulation
(2) Ability to independently maintain ventilatory function often impaired
d. Often require assistance in maintaining a patent airway
e. Positive pressure ventilation may be required because of:
(1) Depressed spontaneous ventilation
(2) Drug-induced depression of neuromuscular function
f. Cardiovascular function may be impaired.
5. Goals and objectives of moderate sedation and analgesia
a. Maintain adequate sedation with minimal risk.
b. Relieve anxiety.
c. Produce amnesia.
d. Provide relief from pain and other noxious stimuli.
e. Overall goal: to allay patient fear and anxiety with a minimum of medication
f. Altered mood
g. Enhanced patient cooperation
h. Elevation of pain threshold
i. Stable vital signs
j. Intact protective reflexes
k. Rapid recovery
l. Unconsciousness and unresponsiveness are not goals of moderate sedation and analgesia.
6. Indications for moderate sedation and analgesia
a. Diagnostic and therapeutic procedures that require anxiolysis and/or analgesia, widely used throughout health care facilities and physician offices, including, but not limited to:
(1) Burn unit dressing changes
(2) Cardiology, heart station, cardiac catheterization and electrophysiology laboratories
(3) Cosmetic surgery
(4) Gastroenterology
(5) General surgery procedures
(6) Gynecology
(7) Ophthalmology
(8) Oral surgery
(9) Orthopedic procedures
(10) Pulmonary biopsy and bronchoscopy
(11) Radiology, interventional radiology
(12) Urology
(13) Emergency department procedures
B. Legal scope of practice issues
1. Requires:
a. An understanding of definition and levels of sedation
b. Adherence to clinical criteria outlined
2. Nurses required to comply with legal scope of practice issues in many jurisdictions
a. Legal scope of practice issues related to nursing delegated and administered through state boards of nursing
b. Nurses engaged in administration of sedation must ascertain their state board of nursing’s formal position or policy statement delineating their role and responsibility in the delivery of sedation and analgesia.
c. Most states have adopted guidelines, but some states have not taken formal action on the issue or lack statutory authority to enact such legislation.
C. The Joint Commission (TJC)
1. TJC has taken an active role in the development of policies, standards, and intents related to operative or other high-risk procedures and/or the administration of moderate or deep sedation or anesthesia.
a. The standards apply when patients receive in any setting:
(1) Moderate or deep sedation
(2) General anesthesia
(3) Spinal anesthesia
(4) Other major regional anesthesia
2. It is the obligation of each institution to develop institution-wide appropriate protocols for patients receiving sedation.
3. TJC states:
a. Moderate or deep sedation and anesthesia are provided by qualified individuals.
b. Sufficient numbers of qualified personnel are present during procedures using moderate or deep sedation and anesthesia.
c. Presedation and preanesthesia assessment is performed for each patient before beginning:
(1) Moderate or deep sedation
(2) Anesthesia induction
d. Moderate or deep sedation and anesthesia care are planned.
e. Patient’s physiological status is monitored during sedation or anesthesia administration.
f. Patient’s postprocedure status is assessed on admission to and before discharge from the postsedation or postanesthesia recovery area.
D. Professional organizations
1. In July 1991, the Nursing Organizations Liaison Forum in Washington, D.C., endorsed a position statement for the management of patients receiving intravenous sedation for short-term therapeutic, diagnostic, or surgical procedures.
a. This position statement has been adopted by many professional nursing organizations.
2. Professional organizations have developed specialty guidelines for use.
3. Participating professional organizations
a. American Society of PeriAnesthesia Nurses
b. Association of periOperative Registered Nurses
c. American Society of Anesthesiologists
d. American Association of Nurse Anesthetists
e. Society of Gastroenterology Nurses and Associates
f. American Society for Gastrointestinal Endoscopy
4. Professional organization guidelines, TJC standards, and statutory regulations require policy development that prepares the nurse participating in the delivery of sedation to demonstrate:
a. Knowledge of anatomy, physiology, cardiac dysrhythmias, and complications related to the administration of sedative agents
b. Knowledge of pharmacokinetic and pharmacodynamic principles associated with moderate sedation medications
c. Presedation assessment and monitoring of physiologic parameters including:
(1) Respiratory rate and ventilatory function
(2) Oxygen saturation
(3) Blood pressure
(4) Cardiac rate and rhythm
(5) Level of consciousness
d. Understanding of principles of oxygen delivery and the ability to use oxygen delivery devices
e. Ability to rapidly assess, diagnose, and intervene in the event of an untoward reaction associated with administration of moderate sedation
f. Proven skill in airway management
g. Accurate documentation of the procedure and medications administered
h. Competency validation for training and education conducted on a regular basis
II. PRESEDATION ASSESSMENT
A. Presedation assessment goals
1. Identify preexisting pathophysiological disease.
2. Obtain baseline patient information.
3. Take history and perform physical examination.
4. Reduce patient anxiety through education and communication.
5. Prepare a plan for the procedure.
6. Obtain informed consent.
B. Components of presedation assessment
1. General health
a. Height and weight
b. Obesity or recent weight loss
c. Current medications or herbal use
d. Baseline vital signs and temperature
e. History of tobacco or alcohol use
f. Physical handicaps and level of mobility
g. Pain assessment
2. Medical history
a. Cardiac
(1) Angina
(2) Coronary artery disease
(3) Dysrhythmias
(4) Exercise tolerance
(5) Hypertension
(6) Myocardial infarction
(7) Presence of a pacemaker or implantable cardioverter defibrillator
b. Pulmonary
(1) Asthma
(2) Bronchitis, tuberculosis, pneumonia
(3) Dyspnea
(4) Exercise tolerance
(5) Cigarette smoking
(6) Recent cold or flu
(7) Airway assessment
(a) Mallampati assessment or other assessment such as having patient open mouth, stick out tongue, and flex neck (see Figure 23-1)
(b) Craniofacial abnormalities
(8) Sleep apnea
c. Hepatic
(1) Ascites
(2) Cirrhosis
(3) Hepatitis
d. Renal
(1) Dialysis
(2) Renal failure
(3) Renal insufficiency
e. Neurological
(1) Convulsive disorders
(2) Headaches
(3) Level of consciousness
(4) Stroke
(5) Syncope
(6) Cerebrovascular insufficiency
(7) Preexisting neurological deficit
f. Endocrine
(1) Adrenal disease
(2) Diabetes
(3) Thyroid disease
(a) Hyperthyroidism
(b) Hypothyroidism
g. Gastrointestinal
(1) Hiatal hernia
(2) Predisposition to nausea and vomiting
(3) Chronic diarrhea or constipation
h. Hematology
(1) Anemia
(2) Aspirin, nonsteroidal anti-inflammatory drug use
(3) Excessive bleeding
i. Musculoskeletal
(1) Arthritis
(2) Back pain
(3) Joint pain
3. Nothing by mouth (NPO) status
a. Guidelines for Preoperative Fasting (American Society of Anesthesiologists) include:
| Ingested Materials | Minimum Fasting Period† (h) |
|---|---|
| Clear liquids‡ | 2 |
| Breast milk | 4 |
| Infant formula | 6 |
| Nonhuman milk§ | 6 |
| Light meal¶ | 6 |
| These recommendations apply to healthy patients who are undergoing elective procedures. They are not intended for women in labor. Following the guidelines does not guarantee a complete gastric emptying has occurred. | |
| †The fasting periods apply to all ages. |
|
| ‡Examples of clear liquids include water, fruit juices without pulp, carbonated beverages, clear tea, and black coffee. |
|
| §Since nonhuman milk is similar to solids in gastric emptying time, the amount ingested must be considered when determining an appropriate fasting period. |
|
| ¶A light meal typically consists of toast and clear liquids. Meals that include fried or fatty foods or meat may prolong gastric emptying time. Both the amount and type of foods must be considered when determining an appropriate fasting period. |
|
b. Emergent procedures require consideration of:
(1) NPO status
(2) Risk of gastric acid aspiration
c. Histamine-blocking and gastrokinetic agents may be used to decrease gastric acidity and decrease gastric volume.
III. PROCEDURAL CARE
A. Monitoring
1. Monitoring process during the procedure includes:
a. Observation and vigilance
b. Interpretation of data
c. Initiation of corrective action when required
2. Electrocardiogram (ECG)
a. ECG monitoring during sedation procedures is required to detect:
(1) Dysrhythmias
(2) Myocardial ischemia
(3) Electrolyte disturbance
(4) Pacemaker function
b. Cardiac rhythm and dysrhythmias that may be encountered include:
(1) Sinus tachycardia
(2) Sinus bradycardia
(3) Sinus arrhythmia
(4) Premature atrial contractions
(5) Supraventricular tachycardia
(6) Atrial flutter
(7) Atrial fibrillation
(8) Junctional rhythm
(9) Premature ventricular contractions
(10) Ventricular tachycardia
(11) Ventricular fibrillation
c. See Chapter 32 for description, ECG criteria, and treatment protocol for specific dysrhythmias.
3. Noninvasive blood pressure
a. Hypotension
(1) A decrease in systolic arterial blood pressure of 20% to 30% and may be caused by a variety of factors including:
(a) Hypovolemia
(b) Myocardial ischemia
(c) Pharmacological agents
(d) Acidosis
(e) Parasympathetic stimulation (pain, vagal stimulation)
(2) Treatment
(a) Administer oxygen.
(b) Administer a fluid challenge (300-500 mL crystalloid).
(c) Correct acidosis or hypoxemia.
(d) Relieve myocardial ischemia.
(i) Nitrates
(ii) Oxygen
(iii) Analgesia
(e) Titrate sympathomimetic medications.
(f) Titrate inotropic agents.
b. Hypertension
(1) Normal blood pressure should be less than 120/80 mm Hg for an adult.
c. Blood pressure that stays between 120/80 mm Hg and 139/89 mm Hg considered prehypertension
d. Systolic blood pressure greater than 140 mm Hg or a diastolic blood pressure greater than 90 mm Hg considered hypertension
(1) Increases bleeding
(2) Predisposes patient to hemorrhage
(3) May lead to cardiac dysrhythmias
(4) Increases systemic vascular resistance
(5) Increases myocardial oxygen consumption
(6) Treatment
(a) Diuresis for fluid overload
(b) Noxious stimuli require analgesia or discontinuation of stimuli.
(c) Sympathetic nervous stimulation may require alpha and beta blockade.
(d) Myocardial ischemia requires nitrates and analgesia.
4. Ventilatory function
a. Assessed using auscultation and having patients take deep breaths
b. Pulse oximetry
(1) Required with sedation to monitor oxygenation status of patient
(2) Provides a noninvasive, continuous monitoring parameter to assess the percentage of hemoglobin combined with oxygen
(3) Pulse oximetry technology allows two light-emitting diodes to measure the intensity of transmitted light across the vascular bed.
(4) Early indication of developing hypoxemia
c. Capnography
(1) Consider using to monitor ventilatory status (end-tidal carbon dioxide levels)
(2) Provides a graphic representation of exhaled carbon dioxide levels with a tracing (capnogram)
(3) Best monitor for measuring adequacy of ventilation
(4) Must use to monitor ventilatory function during deep sedation
5. Level of sedation scoring system
a. Ramsey Sedation Scale (Table 23-1)
| Score | Responsiveness |
|---|---|
| 1 | Patient is anxious and agitated or restless, or both. |
| 2 | Patient is cooperative, oriented, and tranquil. |
| 3 | Patient responds to commands only. |
| 4 | Patient exhibits brisk response to light glabellar tap or loud auditory stimulus. |
| 5 | Patient exhibits a sluggish response to light glabellar tap or loud auditory stimulus. |
| 6 | Patient exhibits no response. |
b. Modified Observer’s Assessment of Alertness/Sedation Scale (Table 23-2)
| Responsiveness | Score |
|---|---|
| Agitated | 6 |
| Responds readily to name spoken in normal tone (alert) | 5 |
| Lethargic response to name spoken in normal tone | 4 |
| Responds only after name is called loudly and/or repeatedly | 3 |
| Responds only after mild prodding or shaking | 2 |
| Does not respond to mild prodding or shaking | 1 |
| Does not respond to deep stimulus | 0 |
c. Sedation Visual Analogue Scale (0-100 mm)
d. Sedation Scale by M. McCaffery and C. Pasero (Box 23-1)
BOX 23-1
SEDATION SCALE
S = Sleep, easy to arouse
1 = Awake and alert
2 = Slightly drowsy, easily aroused
3 = Frequently drowsy, arousable, drifts off to sleep during conversation
4 = Somnolent, minimal or no response to physical stimulation
From McCaffery M, Pasero C: Pain: Clinical manual, ed 2, St Louis, 1999, Mosby.
B. Procedural considerations
1. All syringes labeled
2. Emergency medications and equipment immediately available
3. Adequate intravenous access established before the procedure
4. “Time out” immediately before procedure
5. Turn alarms on and keep them on.
6. Documentation of care every 5 minutes during procedure and at least every 15 minutes during phase I recovery
a. Vital signs
b. Oxygen saturation
c. Level of sedation
IV. AIRWAY MANAGEMENT AND MANAGEMENT OF RESPIRATORY COMPLICATIONS
A. Evaluation of airway
1. Oral cavity inspection
a. Loose, chipped, capped teeth
b. Dental anomalies
(1) Crowns
(2) Bridges
(3) Dentures
c. Obstruction to airflow
(1) Tumors
(2) Edema
(3) Inflammatory processes
2. Temporomandibular joint examination
a. Conducted with patient’s mouth opened wide
(1) Normal distance between upper and lower central incisors is 4 to 6 cm.
b. Indications of reduced temporomandibular joint mobility
(1) Clicking sound when mouth opened
(2) Pain associated with opening mouth
(3) Reduced ability to open mouth
3. Physical characteristics
a. The following physical characteristics may indicate potential for difficult airway management:
(1) Recessed jaw
(2) Protruding jaw (hypognathous)
(3) Deviated trachea
(4) Large tongue
(5) Short, thick neck
(6) Protruding teeth
(7) High, arched palate
4. Mallampati airway classification system (Figure 23-1)
a. Initially described in 1983
b. Offers clinician a grading system for anticipation of difficult intubation
c. Examination conducted while patient’s head is maintained in a neutral position and mouth is opened 50 to 60 mm
d. Classes I to IV are based on anatomic areas visualized.
(1) Class I: uvula, tonsillar pillars, soft and hard palate visualized
(2) Class II: uvula, hard and soft palate visualized
(3) Class III: portion of uvula and hard palate visualized
(4) Class IV: portion of hard palate visualized
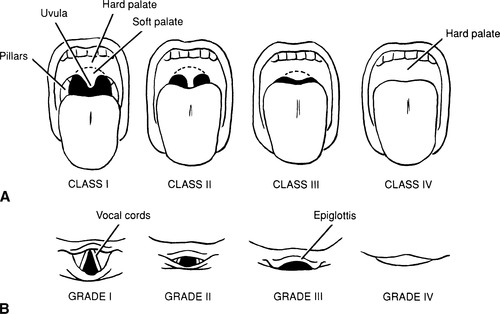 |
| FIGURE 23-1 ▪
Mallampati airway classification.
(From Mallampati SR: Clinical signs to predict difficult tracheal intubation [hypothesis]. Can Anaesth Soc J 30:316, 1983.)
|
5. Anesthesia provider should be consulted for any patient determined at risk for airway management.
B. Complications
1. Potent synergistic effect when following medications used together
a. Sedative
b. Hypnotic
c. Analgesic
2. Decreased oropharyngeal muscle tone predisposes patient to airway obstruction, leading to apnea and hypoxemia.
3. Steps for restoration of airflow
a. Lateral head tilt
b. Chin lift
c. Jaw thrust
d. Nasal airway insertion
e. Oropharyngeal airway insertion
f. Endotracheal tube insertion
4. Oxygen delivery devices: because of respiratory depressant effects associated with administration of sedative, hypnotic, or opioid medications, it is strongly recommended that supplemental oxygen be administered to all patients receiving sedation and analgesia (see Chapter 31).
V. PHARMACOLOGICAL AGENTS
A. Sedation and analgesia medications
1. Benzodiazepines (see Chapter 22 for general facts, pharmacokinetics, and pharmacodynamics)
a. Midazolam (Versed) sedation
(1) Dosing guidelines are individualized and titrated to effect.
(2) Do not administer by rapid injection.
(3) Titration to effect means administration of drug until:
(a) Somnolence
(b) Nystagmus
(c) Slurred speech
(4) Healthy patients: before the procedure
(a) Small increments (0.5 mg) of midazolam are administered over 2 minutes.
(b) Initial intravenous dose should not exceed 2.5 mg.
(c) Some patients may respond to as little as 0.5 to 1 mg.
(5) Adults 60 years or older: elderly, debilitated, chronically ill patients or patients with reduced pulmonary reserve
(a) Require small, incremental (0.25-0.5 mg) doses administered over 2 minutes
(b) Initial dose should not exceed 1.5 mg.
(c) If additional sedation is required, it is imperative to wait 2-3 minutes to evaluate the pharmacological effect before administering additional sedation.
b. Diazepam sedation
(1) Dosing guidelines: individualized and titrated to effect
(2) Before the planned procedure, 1 to 2 mg of intravenous diazepam is titrated over a minute.
(3) Additional 1-mg increments may be administered over several minutes during the procedure.
(4) Additional time must be allowed to evaluate pharmacological effect in geriatric or debilitated patients or patients with decreased cardiac output.
(5) Do not administer by rapid or single-bolus injection.
(6) Extreme care must be exercised when administering diazepam concurrently with opioids.
c. Benzodiazepine antagonist: flumazenil (Romazicon)
(1) Specific benzodiazepine antagonist
(2) Reverses central nervous system effects of benzodiazepines through competitive inhibition of benzodiazepine receptor sites on the γ-aminobutyric acid (GABA) benzodiazepine receptor complex
(3) Duration and degree of reversal related to total dose administered and plasma benzodiazepine concentration
(4) Dose: 0.2 mg administered intravenously over 15 seconds.
(5) If desired level of consciousness not obtained after waiting an additional 45 seconds, a further dose of 0.2 mg can be injected.
(6) May be repeated at 60-second intervals when necessary (up to a maximum of four additional times) to a maximum total dose of 1 mg
(7) Dosage should be individualized based on patient’s response, with most patients responding to doses of 0.6 to 1 mg.
(8) Onset: 1 to 2 minutes; an 80% response will be achieved within 3 minutes of administration.
(9) Duration: 40 to 80 minutes; monitor (up to 120 minutes) for resedation.
2. Opioids
a. Opioids bind to specific opiate receptor subtypes located within central nervous system.
(1) Mu
(2) Kappa
(3) Delta
(4) Sigma
b. See Chapter 22 for general facts, pharmacokinetics, and pharmacodynamics.
c. Dosing guidelines
(1) Fentanyl: 1 to 2 mcg/kg titrated in 25-mcg increments
(2) Meperidine: 0.5 to 1 mg/kg titrated in 25-mg increments
(3) Morphine: 0.05 to 0.2 mg/kg titrated in 1- to 2-mg increments
3. Sedatives, hypnotics, and dissociative anesthetic agents
a. Sedative, hypnotic, and dissociative medications are added to deepen levels of sedation.
(1) Administration of these medications by registered nurses depends on statutory, regulatory, and recommended standards of care.
(2) Manufacturer recommendations generally advise that these agents be administered by anesthesia providers.
(3) Nurse-administered propofol sedation varies with state board of nursing.
(a) Advantages of using propofol for nurse administration of sedation
(i) Short action of medication
(ii) Rapid recovery
(iii) Lower incidence of postoperative/postprocedure nausea and vomiting
(iv) Faster discharge of patients
(b) Disadvantages of using propofol for nurse administration of sedation
(i) Unpredictability of action
(ii) Demanding airway requirements
(iii) No known reversal
(iv) Package insert with propofol states that it is to be used by individuals trained in administering general anesthesia
(c) Perianesthesia nurses should check the scope of practice in the state employed.
(d) See Box 23-2 for safe use of propofol.
BOX 23-2
SAFE USE OF PROPOFOL
Responsible physician:
▪ Must have education and training to manage complications
▪ Must be proficient in airway management
▪ Have ACLS training
▪ Must understand pharmacology of drugs
Practitioner administering propofol:
▪ Must have education and training to identify and mange airway and cardiovascular changes of patient who enters state of general anesthesia
▪ Must have ability to assist in management of complications
▪ Must be present throughout procedure with no other responsibilities other than monitoring patient
▪ Must monitor patient, assessing level of consciousness, ventilation, oxygen saturation, heart rate, blood pressure with monitoring of exhaled carbon dioxide when possible
▪ Must identify early signs of hypotension, bradycardia, apnea, airway obstruction, oxygen desaturation
▪ Must have age-appropriate equipment immediately available
▪ Must not be involved in conduct of surgical/diagnostic procedure
ACLS, Advanced cardiac life support
From Odom-Forren J: The evolution of nurse-monitored sedation. J Perianesth Nurs 20:395, 2005.
b. See Chapter 22 for general facts, pharmacokinetics, and pharmacodynamics.
B. Techniques of administration
1. Single-dose injection technique uses individual medications titrated slowly to effect.
a. To establish an analgesic base, often opioids are administered before benzodiazepines.
b. Two to three minutes before the procedure, intravenous opioids may be slowly administered to establish analgesia.
c. Benzodiazepines are then added and titrated to patient effect.
(1) Combining medications (opioids, benzodiazepines, and hypnotics)
(a) Reduces total dosage through synergistic action
(b) Assists clinician in maintenance of sedation and analgesia parameters
(c) Provides rapid patient recovery
d. Despite the speed with which a desired plasma concentration can be achieved, risks associated with a bolus technique outweigh potential benefits.
e. Small incremental doses allow therapeutic plasma levels to be reached slowly and produce the desired pharmacological effect with a minimum of medication.
2. Continuous infusion techniques produce a constant medication plasma level.
a. Avoids fluctuations in medication plasma levels associated with bolus technique
b. Popular sedative technique in critical care units for mechanically ventilated or agitated patients
c. Additional benefits of continuous infusion techniques
(1) Shorter recovery time
(2) Reduced medication requirement
(3) Minimized side effects
d. Careful titration based on predetermined clinical endpoints (nystagmus, slurred speech, sedation) allows a rapid return to an alert state after infusion is discontinued at conclusion of procedure.
e. Continuous infusion techniques are extremely difficult to master as a clinician, particularly in establishing a baseline level of sedation.
(1) When establishing baseline sedation levels, patients are predisposed to oversedation as the clinician is attempting to establish a desired level of sedation.
(2) This frequently results in patient’s entering a state of deep sedation or general anesthesia.
VI. POSTSEDATION RECOVERY
A. Monitoring
1. Purpose
a. Ensure return of physiological function.
b. Assess patient.
c. Assess readiness for discharge.
d. Treat complications.
2. Monitoring and discharge policies
a. Required by accrediting bodies
b. Recommended by professional organizations
3. Dependent on:
a. Diagnostic or surgical procedure performed
b. Length of procedure
c. Preprocedure physiological status
d. Intraprocedural complications
e. Medications administered
f. Quantities of medications administered
4. Documentation of recovery parameters
a. Use of a postprocedure objective scoring tool (e.g., Aldrete scoring system) to determine readiness to move from phase I to phase II level of care
b. Objective parameters must assess:
(1) Activity
(2) Respiration
(3) Circulation
(4) Level of consciousness
(5) Oxygenation
c. Upon completion of the procedure, all patients must be monitored until all institution-approved discharge criteria are met.
(1) These discharge criteria must be developed in conjunction with statutory, regulatory, and professional organization standards (see Chapter 30 for more discharge criteria).
(2) One of the following objective scoring tools for outpatient “street fitness” may be used to assess for discharge readiness.
(a) Chung’s Postanesthesia Discharge Scoring System
(b) Modified Postanesthesia Discharge Scoring System
(c) Aldrete’s Modified Postanesthesia Recovery Score (see Box 23-3)
BOX 23-3
DISCHARGE CRITERIA SCORING
| Category | Score = 2 | Score = 1 | Score = 0 |
|---|---|---|---|
| Respirations | Breathes and coughs freely | Dyspnea | Apnea |
| O 2 Saturation | SpO 2 > 92% on R/A | Supplemental O 2 | SpO 2 < 92% on O 2 |
| Circulation | BP +/− 20 mmHg pre-op value | BP +/− 20-50 mmHg pre-op value | BP +/− 50 mmHg pre-op value |
| LOC | Awake and oriented | Wakens with stimulation | Non-responsive |
| Movement | Moves 4 limbs spontaneously | Moves 2 limbs spontaneously | Moves 0 limbs spontaneously |
Postanesthesia Discharge Scoring System (PADSS)
1. Vital signs
2 = Within 20% of preoperative value
1 = 20-40% of preoperative value
0 = 40% of preoperative value
2. Ambulation and mental status
2 = Oriented ×3 and has a steady gait
1 = Oriented ×3 or has a steady gait
0 = Neither
3. Pain or nausea/vomiting
2 = Minimal
1 = Moderate
0 = Severe
4. Surgical bleeding
2 = Minimal
1 = Moderate
0 = Severe
5. Intake and output
2 = Has had PO fluids and voided
1 = Has had PO fluids or voided
0 = Neither
The total score is 10, with patients scoring ≥9 fit for discharge home.
MODIFIED Postanesthetic Discharge Scoring System (MPADSS)
1. Vital Signs
2 = Within 20% of preoperative value
1 = 20-40% of preoperative value
0 = 40% of preoperative value
2. Ambulation
2 = Steady gait/no dizziness
1 = With assistance
0 = None/dizziness
3. Nausea/vomiting
2 = Minimal
1 = Moderate
0 = Severe
4. Pain
2 = Minimal
1 = Moderate
0 = Severe
5. Surgical bleeding
2 = Minimal
1 = Moderate
0 = Severe
The total score is 10, with patients scoring ≥9 fit for discharge home.
*A minimum score of 9/10 (and/or return to similar preop status) is achieved prior to transferring the patient to a Phase II recovery area.
From Chung F: Discharge criteria – a new trend. Can J Anaesth 42(11):1056-1058, 1995.
B. Postsedation
1. Instruction
a. Conduct in presence of a responsible adult assuming care of patient on discharge
b. Written discharge instructions addressing medications, diet, and procedure-specific information must be reviewed with each patient.
c. To protect patient, sedation and analgesia discharge instructions identify:
(1) Medication used
(2) Side effects
(3) Specific postprocedural guidelines
2. Patient criteria for discharge
a. Patients should be alert and oriented or return to baseline status.
b. Parents should be informed that pediatric patients are at risk for airway obstruction if head falls forward while child is secured in a car seat.
c. Vital signs should be stable and within acceptable limits.
d. Outpatients should be discharged in presence of a responsible adults who will accompany them home. (This includes all patients who have received sedation, whether minimal, moderate, or deep.)
3. Sedation and analgesia postsedation follow-up
a. A mechanism to ascertain postprocedure status is recommended for patients discharged on day of procedure.
b. Inpatient information may be gathered by the moderate sedation practitioner after the procedure.
c. Methods of gathering data include the following:
(1) Patient questionnaire
(2) Telephone interview
(3) Satisfaction survey
d. Purpose of postsedation assessment is to evaluate the following:
(1) Incidence of complications related to administration of moderate sedation
(2) Delayed recovery
(3) Procedural complication rate
(4) Return to function
VII. SEDATION RISK MANAGEMENT
A. Strategies
1. Quality: defined as the comprehensive positive outcome of a product
a. Achievement of excellence in health care requires quality care and service evaluation.
2. Quality of sedation services based on:
a. Compliance with prescribed standards
b. Recommended practice guidelines
3. Implementation of a successful moderate sedation program based on:
a. Delivery of highly technical aspects of care
b. Positive outcomes
4. Unexpected events and complications may occur as a result of:
a. Human error
b. Periods of reduced observation
c. Environmental factors
d. Poor communication
e. Haste
f. Poor patient selection
g. Lack of preparation
5. To prevent or reduce the number of adverse events:
a. Implement a risk reduction strategy for all units and personnel engaged in administration of moderate sedation.
b. Individual injury prevention strategies include the following:
(1) Development of a complete sedation plan
(2) Presedation preparation and patient assessment
(3) Application and use of required monitoring equipment
(4) Selection of appropriate pharmacological medications and techniques
(5) Preparation and presence of emergency resuscitation equipment and personnel
(6) Preparation for specific procedures and locations
(7) Postsedation monitoring and discharge planning
6. Management of risks and liability for the moderate sedation practitioner
a. Practice issues: know the state board of nursing’s position on the practice.
b. Policies and procedures: must know sedation policy and procedure for facility and adhere to practices.
c. Education and competence: must be educated in all aspects of practice of sedation and analgesia and show competence in delivery of care.
d. Preprocedure care: assessment is important risk tool to determine whether patient is appropriate for nurse-monitored sedation.
e. Medication administration: know sedation continuum and titrate to moderate sedation.
f. Documentation: all nursing care should be documented to give accurate picture of patient’s care.
g. Wrong-site surgery: implement in all settings to decrease risks of wrong person or wrong procedure.
h. Administration of anesthetic agents: know state board of nursing’s position, organizational statements, support or lack of support from the institution, and personal education and competence to deliver the care.
7. Ideally, individual risk reduction strategies prevent injury before an adverse incident or event takes place.
a. Application of a risk management program
(1) Department or institution basis
(2) Development and implementation of mechanisms aimed at:
(a) Risk
(b) Identification
(c) Analysis
(d) Control
b. Creation of a moderate sedation database program, as depicted in Figure 23-2, is essential.
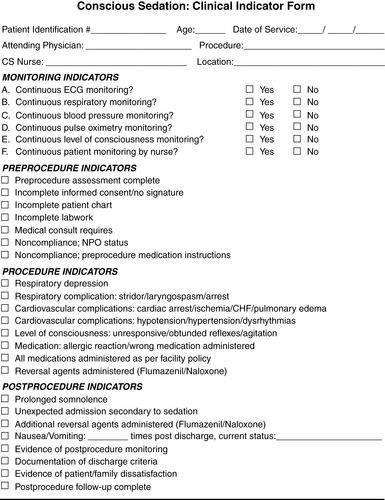 |
| FIGURE 23-2 ▪
Conscious sedation database program.
(From Kost M: Manual of conscious sedation, Philadelphia, 1998, WB Saunders. Copyright 1996, Specialty Health Consultants.)
|
c. Coordinator guides input into moderate sedation database.
d. Once database has been instituted, strategies to implement changes are used.
BIBLIOGRAPHY
1. Aldrete, J., Postanesthesia recovery score revisited, J Clin Anesth 7 (1995) 84.
2. American Heart Association, About high blood pressure. ( November 3, 2008) ; Available at:www.americanheart.org; Accessed.
3. American Nurses Association, Nursing liaison forum: Policy statement on conscious sedation. ( 1991)American Nurses Association, Washington, DC.
4. American Society of Anesthesiologists, Practice guidelines for management of the difficult airway. ( August 13, 2008) ; Available at:www.asahq.org/publica tionsAndServices/Difficult%20Airway.pdf; Accessed.
5. American Society of Anesthesiologists Task Force on Sedation and Analgesia by Non-anesthesiologists, Practice guidelines for sedation and analgesia by non-anesthesiologists, Anesthesiology 96 (4) ( 2002) 1004–1017.
6. Association of periOperating Registered Nurses, Standards, recommended practices and guidelines, AORN J 75 (2002) 642–652.
7. Cohen, L.B.; DeLegge, M.H.; Aisenberg, J.; et al., AGA Institute review of endoscopic sedation, Gastroenterology 133 (2007) 675–701.
8. Foster, F., Conscious sedation…coming to a unit near you. ( 2001)Springhouse Corp, SpringNet, Springhouse, PA.
9. Kost, M., Manual of conscious sedation. ( 1998)WB Saunders, Philadelphia.
10. Kost, M., Moderate sedation/analgesia: Core competences for practice. ed 2 ( 2004)Saunders, Philadelphia.
11. Kost, M.; Brown, D.; DeZayas, B., The administration of conscious sedation by non-anesthesia personnel, Anesth Today 11 (2) ( 2000) 11–15.
12. Lightdale, J.R.; Goldman, D.A.; Feldman, H.A.; et al., Microstream capnography improves patient monitoring during moderate sedation: A randomized, controlled trial, Pediatrics 117 (6) ( 2006) e1170–e1178.
13. Meltzer, B., RNs pushing propofol, Outpatient Surgery 4 (7) ( 2003) 24–37.
14. Moos, D.D.; Cuddeford, J.D., Implications of obstructive sleep apnea syndrome for the perianesthesia nurse, J Perianesth Nurs 21 (2) ( 2006) 103–115.
15. Odom-Forren, J., The evolution of nurse monitored sedation, J Perianesth Nurs 20 (6) ( 2005) 385–398.
16. Odom-Forren, J., The propofol debate continues, J Perianesth Nurs 21 (2) ( 2006) 77–78.
17. Odom-Forren, J., Perioperative patient safety and procedural sedation, Perioperative Nursing Clinics 3 (4) ( 2008) 355–366.
18. Odom-Forren, J.; Watson, D., Practical guide to moderate sedation/analgesia. ( 2005)Saunders, Philadelphia.
19. Ramsay, M.A.; Savege, T.M.; Simpson, B.R.; et al., Controlled sedation with alphaxalone-alph adolone, Br Med J 2 (1974) 656–659.
20. The Joint Commission, Hospital accreditation standards. ( 2008)The Joint Commission, Oakbrook Terrace, IL.
21. Vargo, J.J., Minimizing complications: Sedation and monitoring, Gastrointest Endosc Clin N Am 17 (1) ( 2007) 11–28; v-vi.




